Introduction
Global terrorist attacks, defined as intentional violent acts of significant health impact, have become increasingly more complex, often exploiting unconventional modalities that cause unique traumatic injury patterns, similar to those seen on the battlefield, and requiring a rapid medical response in dangerous and evolving scenarios. Since 2001, the world has witnessed an increase in these asymmetric terrorist attacks on civilian targets, as well as the use of non-conventional weapons including vehicles, homemade bombs, military-grade firearms and ammunition, and chemical weapons like Sarin, Chlorine, and Novichok. This has caused increased demands on health systems and threatened safety of responders and facilities. This editorial argues for the consolidation of the body of experience gathered since 2001 into an initiative called Counter-Terrorism Medicine (CTM), and defining the parameters of CTM within the larger specialty of Disaster Medicine (DM). Reference Levy, Ciottone and Voskanyan1 The time is right to coalesce the varied experiences in these low-frequency, high-acuity events into a commonly accepted strategy to better allow dissemination of best practices and develop evidence-based approaches following the mitigation, preparedness, response, and recovery phases of the disaster cycle.
Counter-Terrorism Medicine: Defining a Sub-Specialty
While the health care system has long been responding to terrorist attacks, little has been done to consolidate research and academic efforts around these events. Following 9/11, the planning and execution of terrorist attacks have become demonstrably more sophisticated, resulting in greater societal impact in terms of lives taken and fear instilled. Reference Smith and Zeigler2 Trends in terrorism-related medical literature demonstrate a steady drop-off following a 9/11/2001 spike, which saw a significant increase in the Western medical literature focused on terrorism and its health care implications, despite no concurrent increase in transnational Western terrorism over that same period, emphasizing the global impact of the 9/11 attacks (Figure 1). Reference Ritchie, Hassel, Appel and Roser3 Despite this, there remains no commonality of understanding or consolidation of this specialism.
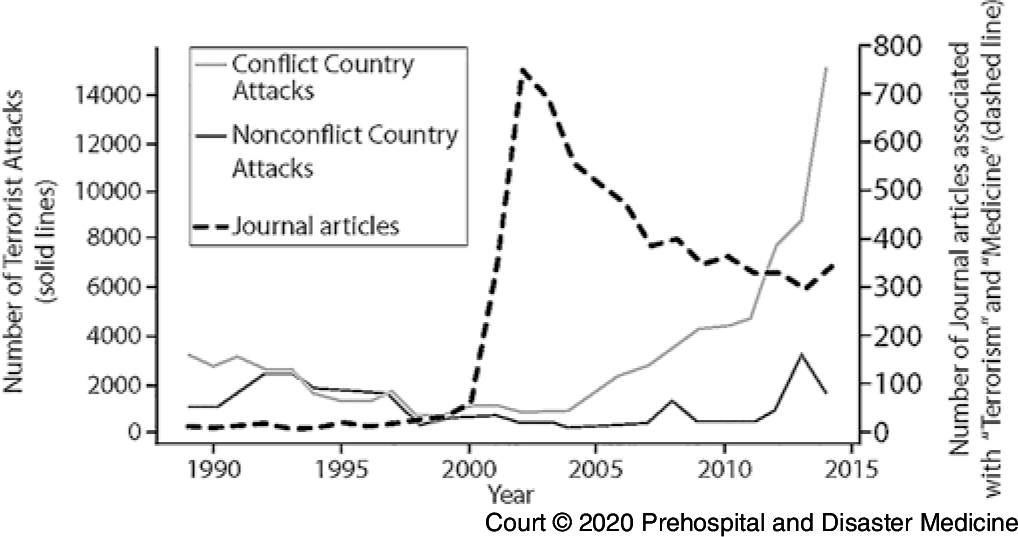
Figure 1. Recorded Terrorist-Related Activity since 1985 with Related Presence of Concurrent National Conflict versus Frequency of Journal Articles in PubMed Associated with MeSH Search Terms “Terrorism” and “Medicine.”Reference Ritchie, Hassel, Appel and Roser3
One of the challenges in allying the medical context with a concept which is fundamentally non-medical is that any discussion on “terrorism” rapidly leads to a concern over the use of the term, in particular around its politicized use. The concept of terrorism versus “freedom fighter” is a well-established dichotomy on the continuum of violence for political gain, but increasingly, terrorism in the midst of conflict and insurgency muddies the water of a definition further. The rise in terrorism focused around national or regional conflict has significant complications in terms of addressing its trends, Reference Smith and Zeigler2 as opposed to terrorism that takes place outside of a direct proximity to conflict.
A myriad of definitions of terrorism have existed, all focusing on a politicized, crisis-centered definition:
The unlawful use of force or violence against persons or property to intimidate or coerce a government, the civilian population, or any segment thereof in furtherance of political or social objective. 4
The World Health Organization (WHO; Geneva, Switzerland) and the Centers for Disease Control and Prevention (CDC; Atlanta, Georgia USA) have both utilized these political definitions to classify terrorism-related casualties in the International Classification of Diseases 10th Edition (ICD-10) criteria. 5 The major limitation of this is that for a death or injury to be classified as relating to terrorism, it requires the federal government to designate an event as “terrorist.” If no designation, then it is not considered terrorism-related. In 2003, a recognition of the requirement for a medical definition of terrorism was proposed that deconstructed the traditional definitions, focusing the optics instead through a health care lens:
The intentional use of violence, real or threatened, against one or more non-combatants and/or those services essential for or protective of their health, resulting in adverse health effects in those immediately affected and their community, ranging from a loss of well-being or security to injury, illness, or death. Reference Arnold, Örtenwall and Birnbaum6
As noted in this seminal paper, “a universal medical/public health definition of terrorism is not merely a theoretical concern, but has important operational implications for health care systems.” We also concur that “the development of effective medical strategies against terrorism requires agreement about what we are dealing with.” Indeed, lack of a medical definition makes consolidating acquired research and knowledge in this field difficult, limiting its presence in the medical literature. We therefore argue for a medical definition of “terrorism,” focused on health care impact, as the basis for the sub-specialty CTM.
The 2017 Las Vegas (Nevada USA) mass-shooting that resulted in 58 dead and 869 injured demonstrates the terminology quagmire. The US Department of Homeland Security (DHS; Washington, DC USA) defines it as a “Targeted Violence” event, 7 while the Global Terrorism Database (GTD) includes it, but states it doesn’t fit the criteria. 8 The popular media uses varied commentary. Reference Dolliver and Kearns9 This is problematic and leads to inconsistency in reporting, resulting in an incomplete academic discussion, despite the event’s clear relevance to the medical community. Using the medical definition of terrorism, we propose a triad that defines the key aspects within CTM, namely: Intent, Violence, and Health Care Impact.
All disasters are indiscriminate, but it is the focused intentionality of terrorist attacks that can convert a routine car accident into a mass-casualty incident from a Vehicle Ramming Attack. Targeting and a desire to have a societal impact also increases the numbers and injury severity of victims of terrorism. These acts are designed to maximize casualties, posing unique medical preparedness and mitigation concerns, particularly at mass-gathering events where hundreds of people can become “soft-targets,” not only in traditional venues such as concerts and sporting contests, but also street festivals, holiday markets, and busy city pedestrian areas, as the recent events in Nice, Berlin, and London have demonstrated.
The use of unique modalities such as military-grade firearms, shrapnel-filled bombs (ball bearings, screws, and nails), and chemical warfare agents also differentiate terrorist attacks from accidental trauma, with the subsequent impact on the health care services required to care for higher acuity patients. Reference Rozenfeld, Givon, Rivkind, Bala and Peleg10 The likelihood of long-term sequelae from both physical and psychological impact is also increased in terrorist events. Reference Ellenberg, Taragin and Ostfeld11,12 Understanding the complexity of victim suffering can change the recovery trajectory for individuals and communities.
The third component of CTM relates to the effect on the health systems in all phases of the disaster cycle, and is not always tied to numbers of casualties. In both the mitigation phase, defined as limiting the direct effect of terrorism on health care services, and the preparedness phase, defined as enhancing the ability to respond to an event, impact is not necessarily related to death toll. The Sarin attacks in Tokyo, the Anthrax attacks in the US, and the cyber-attacks on the National Health System in the United Kingdom all caused a significant amount of disruption to the health care systems, well beyond the actual harm to the population. In Tokyo, the coordinated attacks resulted in the death of 13 people, but caused a global threat concern which resulted in a significant health burden that is now a hallmark of chemical/biological/radiological/nuclear explosion (CBRNE) preparedness.
Global attacks on health care facilities and workers have become increasingly commonplace. 13,Reference Taylor14 While most of these atrocities occur in conflict settings, it remains a global risk 15-18 that can have a significant impact on community preparedness and resiliency. Reference Stith, Panzer and Goldfrank19 Health care facilities and responders are soft targets that can be primarily or secondarily attacked. Reference Ganor and Wernli20-24 The history of health care as a target for terror, the increasing impunity globally to the protected status of health care, and the availability of obvious soft targets with significant potential impact makes mitigation of the threat and health care target-hardening a key tenet of CTM.
Counter-Terrorism Medicine – A Sub-Specialty of Disaster Medicine
Disaster Medicine focuses on a cyclical, revisionist learning model where responses to high-acuity, low-frequency events inform the recovery, preparedness, and mitigation strategies, thus influencing the impact of future “catastrophic” events. Reference Ciottone, Biddinger and Alaska25 As discussed, terrorist attacks cause significant impact on a health care system’s ability to respond. We therefore propose two key recommendations:
-
1. The creation of the CTM initiative: a consolidation of the disparate and connected concepts currently in the academic literature under a new umbrella term, thus increasing the exposure of this important medical niche while highlighting the requirement for interoperability across a multitude of stakeholders. This will promote the advancement of the field through common understanding and propagation of knowledge and best practices.
-
2. Counter-Terrorism Medicine as a sub-specialty of DM (Figure 2): DM utilizes the cycle of mitigation, preparedness, response, and recovery, linking acute response directly to effectiveness and impact on the recovery phase, which then influences mitigation and preparedness. Reference Stith, Panzer and Goldfrank26
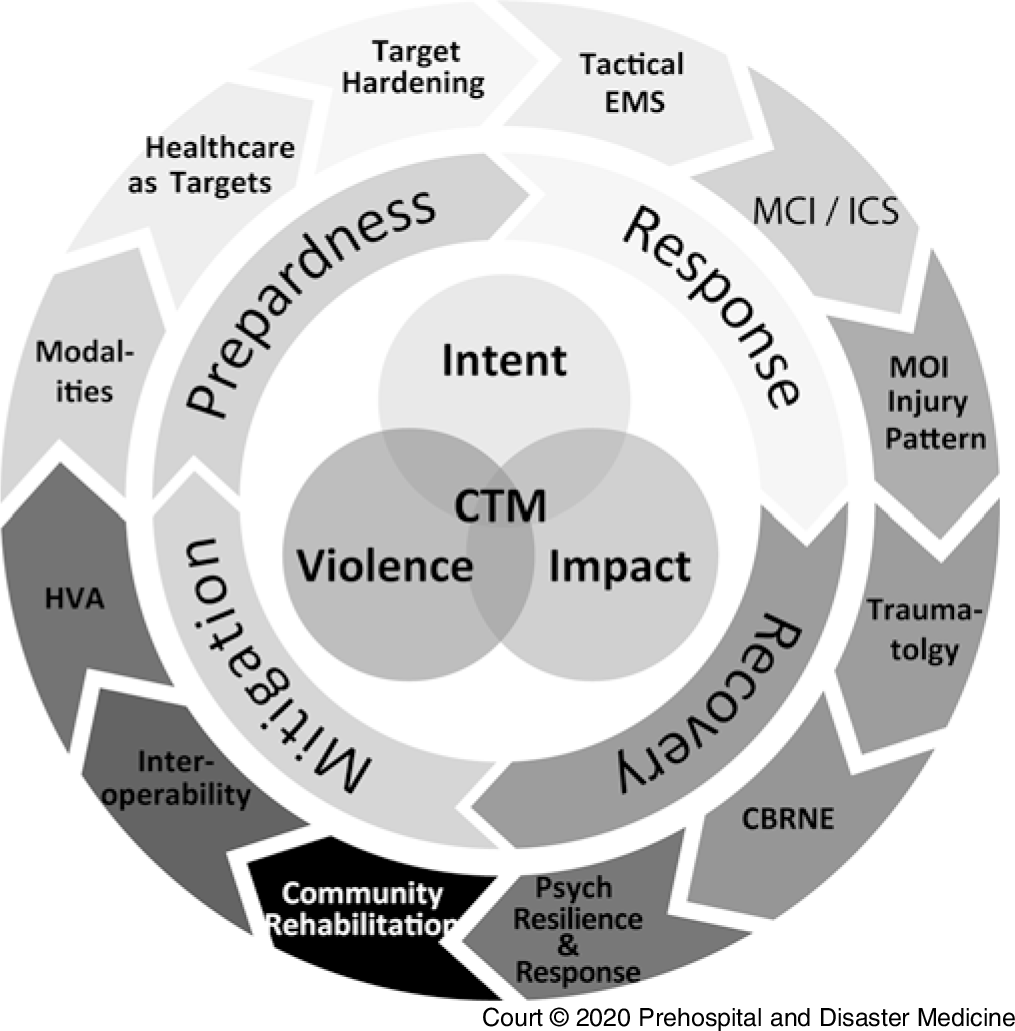
Figure 2. Counter-Terrorism Medicine/Disaster Medicine Cycle – A Pictorial Representation.
We present CTM as a new field, but it would be remiss to not acknowledge those who have laid the foundations for this with previous work. In particular, the work by Shapira and Cole in Essentials of Terror Medicine in 2009. Reference Shapira, Hammond, Cole, Shapira, Hammond and Cole27 We acknowledge the validity and importance of this work, while contending that CTM differs significantly by expanding the scope of practice and placing CTM as a sub-specialty of DM.
Despite the presence in the literature of “terror medicine” as a concept since 2005, Reference Cole28 it has been unable to consolidate opinion into a field. In contrast, we propose utilization of CTM in the literature, a sub-specialty that is health care focused in its definition and framed in the context of the disaster cycle. In doing so, CTM encourages a revisionist approach, allowing “response” to influence future “mitigation” and “preparedness,” thereby reducing risk and impact. We feel CTM, with its focus on “countering” the risks and effects of terrorism on health care, better defines the field as part of the “counter-terrorism” conversation, enabling a more fundamental medical involvement in this area.
Limitations
In many nations, tactical Emergency Medical Services (EMS) integrate prehospital medical providers with law enforcement. While these “SWAT” medical officers may respond to terrorist attacks, they also participate in non-terrorism-related police operations. Tactical EMS is included within the CTM paradigm, as seen in the CTM disaster cycle diagram, but this deserves further exploration outside the scope of this article.
Conclusion
The time has come for a consolidation of the health care response to terrorism. Counter-Terrorism Medicine, as a sub-specialty of DM, accomplishes this by focusing on events that include the triad of Intent, Violence, and Health Care Impact through mitigation, preparedness, response, and recovery activities. It builds on the vital work by a range of academics since 2001 and seeks to consolidate this currently disparate field. We propose CTM should feature in the medical literature search engines and be available for academics as a MeSH term when publishing to help refine the field. Further research on the existing literature based on this concept is warranted to better understand and consolidate this vital discussion.
Conflicts of interest
All authors confirm they have no competing interests.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1049023X2000103X





