Introduction
There is a high prevalence of deaths occurring in non-palliative care units in acute hospital settings such as cardiology, geriatrics, and intensive care; yet, non-palliative care professionals (NPCPs) including physicians, nurses, and social workers often perceive themselves as inadequate in engaging with and caring for critically and terminally ill patients and their families (Holley et al. Reference Holley, Carmody and Moss2003; Lien Foundation 2014). With the onus on NPCPs in their respective non-palliative settings to treat disease and prolong life, poor patient prognosis and death often trigger distress and dilemmas within them and cast doubt upon their clinical competencies (Braun et al. Reference Braun, Ford and Beyth2010; Langley et al. Reference Langley, Kisorio and Schmollgruber2015; Zwicker and Lutz Reference Zwicker and Lutz2018). In the context of Singapore and neighboring Asian regions, this phenomenon is further exacerbated by societal death taboos, lack of involvement in one’s own death preparation, poor communication between patients and family decision-makers, as well as traditional concepts of filial piety and familial obligation that contribute to the pursuit of futile life-sustaining interventions (Chan et al. Reference Chan, Ho and Leung2012; Chan and Yau Reference Chan and Yau2010; Ho and Tan-Ho Reference Ho, Tan-Ho, Vasbinder and Gulyas2016). As such, the impact of failed efforts at curation and stalling death in this instance would be intensified by the strata of not just personal and professional but organizational and societal pressures, resulting in massive stress and consequently burnout (Koh et al. Reference Koh, Chong and Neo2015, Reference Koh, Hum and Khoo2019).
Burnout is a reaction to chronic job-related stress and occurs when individuals become overwhelmed with the emotional, mental, and physical duress associated with their professional work. Defined as “a state of exhaustion in which one is cynical about the value of one’s occupation and doubtful of one’s capacity to perform” (Maslach et al. Reference Maslach, Jackson and Leiter1996), it can translate into a “literal collapse of the human spirit” (Storlie Reference Storlie1979). Burnout has also been found to negatively impact quality of care and expression of empathy among professional care providers (Dewa et al. Reference Dewa, Loong and Bonato2017; Wilkinson et al. Reference Wilkinson, Whittington and Perry2017), while causing increased medical errors among physicians and heightened turnover rates of workers in various health-care institutions (Dill and Cagle Reference Dill and Cagle2010; Shanafelt et al. Reference Shanafelt, Balch and Bechamps2010). A study found that physicians within the health-care clusters of Singapore experience high levels of burnout rates of up to 80.7%, surpassing the burnout rates of physicians in the United States, which ranged between 47% and 70% (Lee et al. Reference Lee, Loh and Sng2018). These figures may very well worsen, bearing in mind the rapidly aging population in Singapore and the consequent proportionate rise in the number of patients who will require end-of-life care outside of palliative care units (See et al. Reference See, Lim and Kua2016).
In order to safeguard NPCPs from burnout and ensure that patients and families receive quality and dignified care, there needs to be a comprehensive understanding of the specific challenges NPCPs face within the health-care ecosystem, before appropriate interventions can be implemented. While a handful of research has explored the experience of NPCPs caring for end-of-life patients, they have focused preliminarily on nurses and physicians of single medical specialties (Gardiner et al. Reference Gardiner, Cobb and Gott2011; Garner et al. Reference Garner, Goodwin and McSweeney2013; Lai et al. Reference Lai, Wong and Ching2018; Oliveira et al. Reference Oliveira, Fothergill-Bourbonnais and Mcpherson2016) and lack a comprehensive representation of all major key stakeholders of multiple medical disciplines that play vital roles in supporting the end-of-life journeys of terminally ill patients. Furthermore, most of these studies were conducted in Western societies, with only one article examining the phenomenon in Asia (Lai et al. Reference Lai, Wong and Ching2018). To address this critical knowledge gap, the current research aims to (a) identify precise challenges of NPCPs caring for end-of-life patients in Singapore, (b) determine how these challenges interact with and influence each other systemically; and (c) further the advancement of theories and practices for supporting NPCPs in the provision of quality end-of-life care beyond the boundaries of palliative medicine.
Methods
Design
This study adopts a constructivist phenomenological qualitative research design with an interpretive-systemic framework (IFS) of inquiry to elicit the lived experiences of NPCPs caring for end-of-life patients outside of palliative care settings in Singapore. The IFS enables a multiple interpretive process for understanding a given phenomenon through the lens of the many contextual systems that it is embedded in, as represented by specific stakeholder groups (Fuenmayor Reference Fuenmayor1991; Ochoa-Arias Reference Ochoa-Arias1998).
Sampling
Guided by the ISF, participants representing the 3 major stakeholder groups of NPCPs including physicians (n = 35), nurses (n = 35), and medical social workers (n = 35), who belong to 9 major medical disciplines of Cardiology, Geriatrics, Intensive Care Medicine, Internal Medicine, Nephrology, Neurology, Oncology, Respiratory Medicine, and Surgery, were recruited through purposive snowball sampling (N = 105). Seven major public hospitals and health-care institutions served as the primary recruitment sites including Khoo Teck Puat Hospital, Tan Tock Seng Hospital, National University Hospital, Changi General Hospital, Sengkang General Hospital, Singapore General Hospital, and the Singapore Cancer Society. The inclusion criteria comprised full-time employed NPCPs who could communicate in English or Mandarin and provide informed consent. NPCPs who were working on a part-time basis with less than 35 hours of work per week, suffering from any mental health conditions, or unable to provide informed consent were excluded from the study. On-site collaborators from the 7 collaborating hospitals including heads of department, nursing managers, and master social workers assisted in participant recruitment. Upon identification of suitable participants through purposive sampling, the on-site collaborator briefly introduced study background and obtained verbal consent for referral to the research team. Successful referrals were contacted via email or telephone by the research team, who explained the background of the study objectives, carried out screening, and scheduled a time for data collection via face-to-face interview. Participants who successfully completed the interview were invited to recruit their coworkers for the study, with the same referral procedures being adopted. The inclusion and exclusion criteria and on-site collaboration ensured that recruited participants were representative of the medical specialities and professions.
Careful ethical considerations were included in every step of research design and implementation – these included the protection of confidentiality, providing a safe environment for participants to share their experiences in an open and honest manner, as well as secure handling of all research data.
In-depth interviews
In-depth semi-structured interviews were conducted to collect rich experiential narratives and multiple interpretations on end-of-life care provision beyond palliative medicine. Participants were asked to reflect and comment on 8 key areas, including (1) their knowledge, attitudes, and perceived values of end-of-life care; (2) work procedures and processes in caring for end-of-life patients; (3) challenges faced when engaging in end-of-life care work; (4) reflection and articulation of a specific care encounter and relationship with an end-of-life patient and their family; (5) their experience with patient death, loss, and grief; (6) the impact of end-of-life care in their professional and personal lives; (7) their end-of-life care work in relation to the larger health-care system; and (8) their education and training needs for competent end-of-care provision. Each interview took 60 to 90 minutes to complete and were recorded and transcribed verbatim. All interviews took place between May and December 2019.
Data analysis
Framework analysis (Ritchie and Spencer Reference Ritchie, Spencer, Bryman and Burgess1993) including both inductive and deductive approaches were adopted to critically examine the data for generating themes that illuminate the lived experiences of NPCPs caring for end-of-life patients. Framework analysis is specifically developed in the context of applied policy research, one that has specific questions, a predesigned sample, and a priori issue and aims to meet specific information needs and provide outcomes or recommendations (Srivastava and Thomson Reference Srivastava and Thomson2009). The analytical supported by the NVIVO software involved several steps of data reduction and reconstruction. First, multiple readings and line-by-line coding were carried out by the first, second, and third authors; written summaries and codes that reflect the a priori of end-of-life care provision challenges were created. Second, axial coding was conducted to develop and refine possible categories of responses; text files containing quotes supplementing the emergent themes and subthemes were also created. Third, the same 3 members of the research team individually reviewed and defined the emergent themes and presented to one another and the larger research team for confirmation; once consensus was reached, operational definitions were created. Finally, themes and subthemes were proposed and mapped with supporting quotes from transcripts. Distribution of theme occurrences and frequency counts were tabulated. To address issues of trustworthiness and credibility, emergent themes were constantly compared within and across groups during regular meetings, and members checking was conducted with selected research participants of all 3 stakeholders groups from the 9 medical disciplines.
Findings
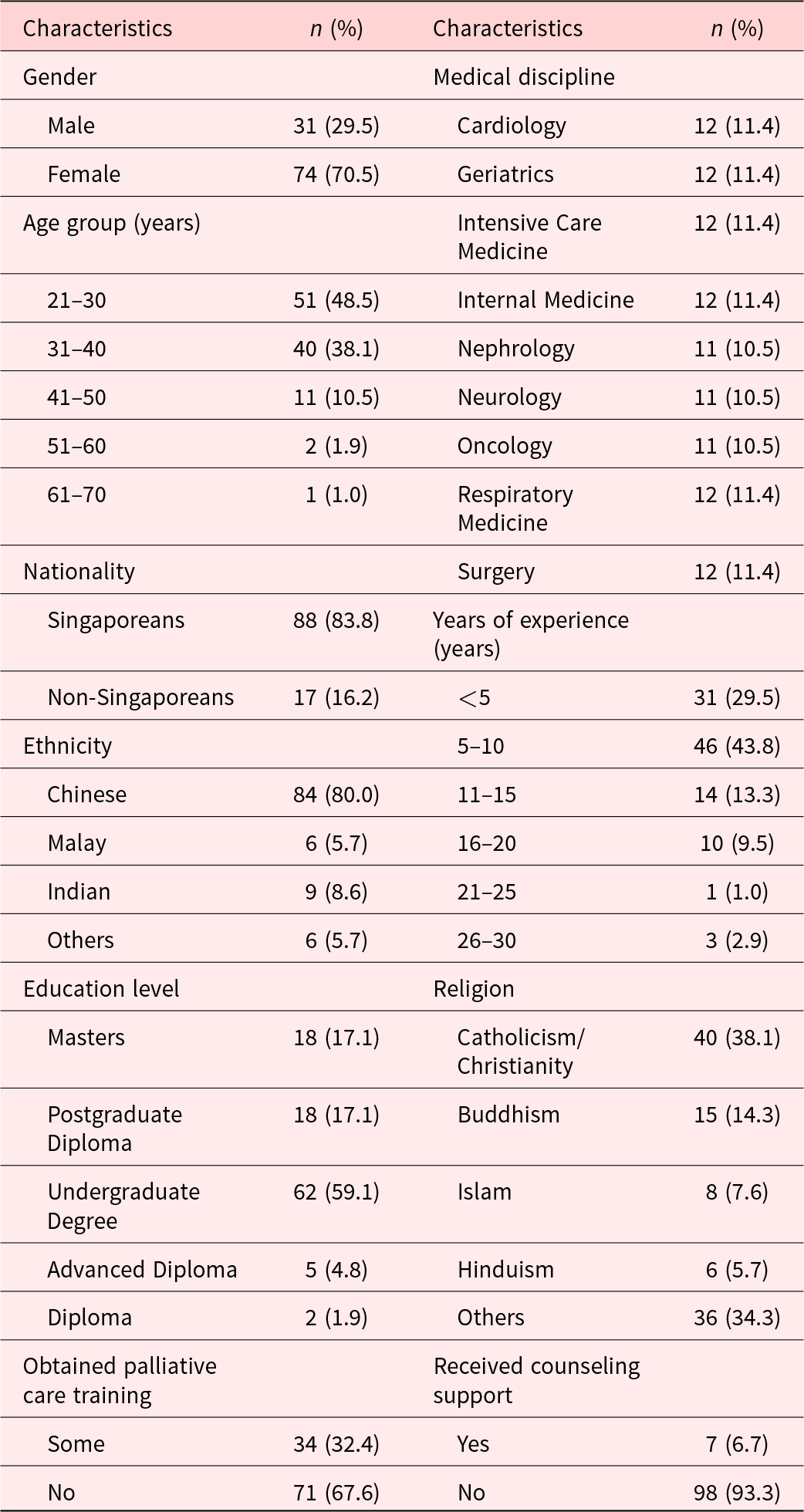
Table 1 presents the background information for research participants. Overall, 70.5% of participants were female with a mean age of 33 years (SD ± 7.5; range = 23–64). About 88% were Singaporeans, 80% were ethnic Chinese, and 28.6% were Catholics. About 91% had at least an undergraduate degree, 43.8% had between 5 and 10 years of working experience, with 29.5% having more than 5 years of experience. About 34.3% had obtained some form of palliative care training. Moreover, participants were also proportionately spread across the 9 medical disciplines of Cardiology (11.4%), Geriatrics (11.4%), Intensive Care Medicine (11.4%), Internal Medicine (11.4%), Nephrology (10.5%), Neurology (10.5%), Oncology (10.5%), Respiratory Medicine (11.4%), and Surgery (11.4%).
Table 1. Overall demographics of research participants (N = 105)
Framework analysis revealed 5 themes and 17 subthemes that illuminate the individual, relational, cultural, institutional, and structural challenges that NPCPs faced in rendering end-of-life care. Each of these themes and subthemes is considered in turn and supported by illustrative quotes.
Individual challenges
Individual challenges (theme 1) faced by NPCPs revolved around the personal emotional strains they experienced in the provision of end-of-life care (Box 1). Unresolved grief (subtheme 1, n = 33) was identified to be the most common emotional strain that NPCPs suffered from – a testament to the significance of deaths and losses within non-palliative care units. Yet, this grief often went undetected and consequently unsupported due to the NPCPs’ lack of awareness in recognizing signs of grief or their desire to avoid confronting those difficult emotions in a fast-paced work environment. Such feelings of grief are exacerbated by NPCPs’ self-imposed mortality gatekeeping (subtheme 2, n = 34) – a longstanding expectation and perception within non-palliative medical units that they must avert death and banish suffering and one that contributes to feelings of stress, helplessness, and self-blame in their work. Conversely, NPCPS also experienced moral distress (subtheme 3, n = 22) when they felt pressured by patients’ families to continue futile and aggressive treatments, especially against the wishes of their patients, for fear of legal implications.
Box 1. Individual challenges
Subtheme 1: Unresolved grief
“I feel a great loss. I feel very sad, because when you keep taking care of the patient … you develop a quite good relation …. So, when they pass away, you feel that one of your relatives or one of your loved ones pass away.” (A03P, Geriatric Physician, 36)
“After having worked too long in the oncology setting, some of us leave. I believe that is because it’s emotionally draining, especially because of our attachment with patients.” (B02N, Oncology Nurse, 42)
Subtheme 2: Mortality gatekeeping
“When he died, I was upset … I felt some guilt that I was part of the medical team that had put him through this procedure, that ultimately caused him to pass away.” (A11P, Intensive Care Unit Physician, 40)
“Whenever I think about the great divide, I think about the divide between me and the patient. They’re on the other side with the pain, and I’m here, no pain. As much as I try to cross over to the other side to alleviate their pain right, I cannot reach them.” (A06N, Surgery Nurse, 26)
Subtheme 3: Moral distress
“We have patients who have clearly said they do not want resuscitation. But when they get sick, a relative counteracts that …. It’s very difficult for a health-care provider to go against that … for your own peace of mind, the family’s peace of mind, but also legally, everyone here is petrified about being sued.” (A11P, Intensive Care Unit Physician, 40)
“The family member’s decision takes the weight. So, we will still go ahead with it… (I’m) not very comfortable with that, because it’s like, ‘I need to do a treatment that I think the patient doesn’t want, and I think it’s not going to help, but I still have to do it.’” (D04N, Neurology Nurse, 27)
Relational challenges
Relational challenges (theme 2) encountered by NPCPs involved barriers to effective care partnerships with patients and their families (Box 2). NPCPs expressed lacking skills and confidence in managing complex patient–family dynamics (subtheme 4, n = 27) during decision-making processes, especially when patients themselves declined participation in these discussions. This challenge stems from the collectivistic Asian culture, in which family members often expect and are given the authority to make treatment and care decisions (Back and Huak Reference Back and Huak2005). NPCPs also faced competency-related apprehension (subtheme 5, n = 15) from patients and families, with their professional capabilities put into question when their prognoses were deemed inaccurate or when they were perceived to be of a junior rank. Such mistrust affected the quality of relationships between NPCPs and patient–families, as well as contributed to more feelings of helplessness and disempowerment in NPCPs.
Box 2. Relational challenges
Subtheme 4: Complex patient–family dynamics
“The most difficult challenge is if the family is huge and if the family is not on talking terms amongst each other, and what matters to the person nearing death is that the family be harmonized or to be in agreement.” (B03S, Geriatric Social Worker, 40)
“The spokesperson is normally the oldest son, and then you can get a little bit of problem there if say the oldest son isn’t the primary caregiver, and the loved one (patient) is actually living with the daughter or something like that.” (A11P, Intensive Care Unit Physician, 40)
Subtheme 5: Competency-related apprehension
“We think (the) patient is dying in the next 1 or 2 days, the patient is hanging in (there), so sometimes the families get upset. They come back to you, ‘Doctor you said 72 hours, (the) patient is still (alive).’” (A02P, Geriatric Physician, 64)
“The resistance comes from the family members because … they will ask about what kind of medications you are giving and when you say morphine, some of them just associate it with giving up or hastening death. They just feel like you are speeding up death.” (B08P, Internal Medicine Physician, 27)
Subtheme 6: Unrealistic expectations
“The family has unrealistic expectations and wants us to bring him [patient] back to life, make him wake up and that kind of thing, and then they want everything. Even though we know that in some situations, it’s quite futile already.” (A14P, Cardiology Physician, 32)
“‘Just give her medicine and (my) mum would get better.’ Even though (her) mum was already palliative, but then you know, her understanding was, ‘She’s in a hospital, why are doctors not treating her?’” (A07S, Respiratory Medicine Social Worker, 29)
Chiefly furthering these difficulties is the challenge of managing unrealistic expectations (subtheme 6, n = 29) from patients and families with regards to treatment efficacy and feasibility of recovery. This occurred when family members held impractical beliefs on what medical teams could do in supporting patients in the final stages of life, with the hope that illness trajectories could be reversed.
Cultural challenges
Cultural challenges (theme 3) that NPCPs were confronted with stemmed from vast inadequacies in death literacy due to the local cultural taboo of death (Box 3). NPCPs reported often receiving requests for collusion (subtheme 7, n = 10), that is, to withhold medical information, diagnosis, and prognosis from the patient; NPCPs who refused to comply risked facing anger, rejection, or complaints from these families. Such requests, and the refusal to participate in end-of-life conversations such as Advance Care Planning are not surprising as simply engaging in death-related discussions can be deemed unlucky in Singapore, with an implied absence of filial piety or familial obligation (Ho and Chan Reference Ho, Chan and Conway2011).
Box 3. Cultural challenges
Subtheme 7: Requests for collusion
“We notice that (when the) family … and patients with metastatic cancer come in, there is collusion. The family has not told the patient, and they don’t want you to tell the patient, so that is a difficult thing to deal with.” (A02P, Geriatric Physician, 64)
“Family members actually want us to collude and say, ‘Don’t tell them about their [patients] medical condition. Don’t tell them about the prognosis.’” (A01S, Neurology Social Worker, 43)
Subtheme 8: Death denial
“We run into all these problems with patients and families because people are just not prepared. They don’t want to talk about death, then you are wasting time in your busy clinic, starting to get them to open up.” (B03P, Nephrology Physician, 35)
“If we were to just strike (up) a conversation like that (randomly), it’s not easy (to get the patients to open up). Yeah, because it’s still a taboo.” (B03N, Oncology Nurse, 38)
Subtheme 9: Death anxiety
“When you are in the hospital, sometimes even (for) me, if I think about death, I’m still scared.” (A12N, Respiratory Medicine Nurse, 44)
“I was quite uncomfortable, because I think the word ‘palliative’ is quite a big word. The word ‘dying’ is – I mean it happens all the time, but it’s still not easy when you first start out.” (B04S, Internal Medicine Social Worker, 25)
NPCPs reported that many patients and families exhibited death denial (subtheme 8, n = 8), refusing to engage in end-of-life conversation because of their reluctance to accept a terminal prognosis, especially when patients’ functional capacities remain temporarily intact. It is important to note that such death anxiety (subtheme 9, n = 17) is not exclusive to patients and families – NPCPs also revealed personal apprehensions about mortality that compounded their difficulty in broaching end-of-life care discussions at work.
Institutional challenges
Institutional challenges (theme 4) that NPCPs faced were found in workplace culture and stigma that hindered professional empowerment and personal and patient well-being (Box 4). Interdisciplinary power disparities (subtheme 10, n = 24) were highlighted by mainly nurses and medical social workers – further evidence to the longstanding perceived authority of physicians over other medical professionals.
Box 4. Institutional challenges
Subtheme 10: Interdisciplinary power disparities
“So I will advocate, but until a point in time where even the consultant turns down (the suggestion), then I will feel that, okay then maybe – I mean like, who am I, am I going to override what the consultant says?” (B01S, Geriatric Social Worker, 31)
“We can suggest (solutions), but how open you are to listen to a nurse’s opinion depends very much on (the) medical team.” (D04N, Neurology Nurse, 27)
Subtheme 11: Misalignment of care goals
“When you say you want to act in the best interest of the patient, especially when the patient doesn’t have decision-making capacity, different people caring for that person may have different approach to the management of EoL.” (B03P, Nephrology Physician, 35)
“The renal doctors don’t want to release the patient to palliative, because they would definitely want the patient to continue with treatment because they are still so young.” (A05S, Nephrology Social Worker, 30)
Subtheme 12: Stigma of vulnerability
“I don’t know whether there is a trust issue? Maybe, you talk to (Institution’s Counselor) and you are seen as weak … not competent, I don’t know … what if whatever I share comes back to disadvantage me in the future?” (A04S, Intensive Care Medicine Social Worker, 29)
“Sometimes there is a lot of stigma because if you go to see a psychologist, some people may judge you for it and things like that.” (B08P, Internal Medicine Physician, 27)
Misalignment of care goals (subtheme 11, n = 9) across various medical disciplines and units were found to cause conflict and delay in end-of-life care processes, an indication that different medical disciplines had contrasting perceptions of end-of-life care. Meanwhile, support programs put in place by the institutions for its staff often went unused due to the stigma of vulnerability (subtheme 12, n = 18) – NPCPs feared judgment and speculations about their competency and suitability to their work that could damage their career. Of note, medical social workers spoke about this concern more than nurses and physicians; while they possessed the most psychosocial knowledge and training among all the stakeholders, they seemed to also hold themselves to expectations of high emotional competence and thus ironically refrained from seeking help.
Structural challenges
Structural challenges (theme 5) that NPCPs had to cope with encompassed fundamental limitations within the larger health-care system and infrastructure that posed predicaments to quality of care (Box 5). One of the most severe problems highlighted by NPCPs was the deficiency in end-of-life care training (subtheme 13, n = 36), which greatly contributed to them feeling ill-equipped in providing adequate and holistic care, timely referral, clear communication with patients and families, as well as aligning care goals with other NPCPs. It is evident that there is a lack of holistic training for medical professionals – NPCPs expressed that they knew little outside of their own medical specialties.
Box 5. Structural challenges
Subtheme 13: End-of-life care training
“For us, (we are not sure of) which time point is a good time to refer to them … We have sometimes difficulty (in predicting) the time (of) end‐stage renal failure.” (A04P, Nephrology Physician, 44)
“I wish I could (refer patients to palliative care), I suppose that would be a kind of like advocacy, but I don’t know what the criteria is for palliative referral, because mostly it’s the doctors who are doing it.” (D04N, Neurology Nurse, 27)
Subtheme 14: Tenuous resources and disjointed infrastructure
“(There are) not enough machines, I need to go and borrow. I need to call the (different ward) levels and see where else I can borrow the machine from, and usually it takes a while.” (D04N, Neurology Nurse, 27)
“To get a bed in the hospital and to wait in the emergency department on the trolley beds, (is) not the most pleasant way to deal with palliative patients who are approaching the later part of their lives.” (A01P, Geriatric Physician, 35)
Subtheme 15: Discontinuity of care
“There are GPs (General Practitioners) but there is no framework. There is no link between hospital and the GP. No link between primary and secondary care, so there is a big gap in the service here.” (A02P, Geriatric Physician, 64)
“AIC requires a lot of input from the doctors, the nurses, the PT, the OT (and), the MSW, (you have to go through) a lot of processes before you can submit that form … sometimes the (additional) barrier will be getting the doctor to write the report for the patient.” (B03N, Oncology Nurse, 38)
Subtheme 16: Excessive red tape
“I have to refer to palliative care, palliative care then has to do it, and sometimes by the time all that’s happened, the patient’s died in hospital. And I think that’s one of the least satisfying parts of working with these patients.” (A11P, Intensive Care Unit Physician, 40)
“Although we can offer help, the process of getting help is difficult. You need to give me a thousand and one documents, you need to explain to me why you have no money … sometimes people really think that it’s very, very intrusive, because it comes to a point where I need to know how you spend your every cent.” (A05S, Nephrology Social Worker, 30)
Subtheme 17: Efficiency over quality
“Although they always focus on person-centric care, but I just feel that sometimes, it is just very goal-oriented, very task-oriented, such that it is just for discharge (of patients).” (D10S, Cardiology Social Worker, 25)
“I guess it’s just the whole setting of an acute hospital, especially when the turnaround time is a lot faster, there’s the demand for decisions and practical steps. It seems to be a lot more important than what patient feels.” (A07S, Respiratory Medicine Social Worker, 29)
A strongly articulated challenge by all stakeholders was the problem of the tenuous resources and disjointed infrastructure (subtheme 14, n = 34) – poor resources and limited manpower often formed the basis of their many challenges, exacerbated by excessive bureaucratic procedures or demands. NPCPs also reported a discontinuity of care (subtheme 15, n = 19), in which inconsistent care teams, poor documentations, and the lack of communication between care agencies had hampered care quality.
Excessive red tape (subtheme 16, n = 17) were identified as hurdles to care referral, efficiency, and quality, with markedly complicated administrative procedures affecting the relationship and rapport between NPCPs and their patients and families. Finally, in the constant pursuit and ingrained culture of fulfilling Key Performance Indexes, NPCPs found themselves being swept up in the demands for quick decisions and practical steps rather than holistic patient care, consequently prioritizing efficiency over quality (subtheme 17, n = 36).
Discussion
The findings of this study have provided a systemic view of the difficulties encountered by NPCPs caring for patients and their families at the end-of-life – namely, Individual, Relational, Cultural, Institutional, and Structural challenges. The following discusses the interactions between and recommendations to mitigate the challenges from our findings.
The Individual challenges faced by NPCPs emphasize the urgent need for psychosocial education and intervention on understanding and coping with grief to be implemented across all medical disciplines on a Structural level. Mindful-compassion art-based therapy that integrate contemplative meditation with arts for nurturing self-understanding and supporting grief work has shown to be highly effective for burnout reduction and resilience building (Ho et al. Reference Ho, Tan-Ho and Ngo2021). On an Institutional level, emotion-focused debriefing for deceased or unexpectedly deteriorating patients should be incorporated into team meetings. Death Rounds, 1-hour sessions dedicated to discussions of emotional reactions to patient death, have been found to be supportive (Smith and Hough Reference Smith and Hough2011). Clear guidelines about potential legal issues should be incorporated into these health-care institutions; NPCPs must be informed of these legal technicalities so that they are able to work and communicate with less fear and uncertainty.
The Relational challenges that NPCPs encountered demonstrate the benefit of NPCPs possessing more comprehensive knowledge about palliative care and dying trajectories – confidence in their expertise would empower them to be open and honest with patients and families, thus eliminating unnecessary confusion and misgivings. This can be done on an Institutional level by ensuring that NPCPs complete necessary palliative care courses, as well as communication skills workshops, to maximize their end-of-life care capabilities and efficacy. Additional curricula for medical students that incorporate attachment and first-hand experience of end-of-life care can serve to prepare them mentally, emotionally, and clinically as future NPCPs (Ratanawongsa et al. Reference Ratanawongsa, Teherani and Hauer2005).
The Cultural challenges that NPCPs face transcend the larger health-care system into society – death anxiety and taboos can be abolished by consistent and determined public education in death awareness. Campaigns pushing for ACP and demonstrating its benefits to familial harmony and patient well-being can minimize the need for collusion (Dutta et al. Reference Dutta, Lall and Car2019; Lall et al. Reference Lall, Dutto and Tan2021). On an Institutional level, NPCPs should receive training in fundamental death education, with an emphasis on reflecting on what death means to them (Ho et al. Reference Ho, Lall and Tan2021).
The Institutional challenges NPCPs struggle with demonstrate pressing need for leveling the hierarchy in health-care by cultivating an institutional ethos of open and respectful interdisciplinary communication and advocacy for patients. At the same time, there must be a shared understanding of patient conditions for end-of-life referral to lessen confusion and dispute. Institutions must also safeguard the well-being of its staff by encouraging and even providing incentives for them to seek regular psychosocial support. The onus must not simply be on staff to speak up or seek help; leaders of health-care organizations can endorse and nourish such behavior by role-modeling their willingness to listen, to accept help and to conduct wellness check-ins for their colleagues (Kim et al. Reference Kim, Appelbaum and Baker2020). All these can only be achieved with inculcation of clear institutional values and guidelines that support the above.
The Structural challenges NPCPs face highlight the need for more focus on and continuity in end-of-life and palliative care within the formal education and subsequent training curricula for all medical professionals. At the same time, the overloaded health-care infrastructure could be eased in 3 aspects – first, technology must continue to be enhanced so that it can effectively attend to tasks that do not necessarily require human manpower, such as monitoring, analyzing, and recording patient vital signs and symptoms (Nwosu et al. Reference Nwosu, Sturgeon and McGlinchey2019). This will free up NPCPs to focus on the context and complexity of treatment and care plans. Second, incentives to join health care such as more scholarships or subsidies in training and education could enhance manpower recruitment. Third, continued and rigorous campaigns, initiatives, and public education on aging healthily would help in lessening the number of people requiring health services in the future.
Strengths and limitations
This is the first known study exploring the systemic challenges of NPCPs spanning 9 major medical disciplines and encompassing 3 professional stakeholders responsible for the care for end-of-life patients, thus ensuring perspective inclusivity across the health-care system. As such, the current findings can provide moderatum generalizability (Williams Reference Williams and May2002) and can proficiently serve as a guide for other Asian regions that share similar social and cultural contexts as Singapore. This is one of the largest qualitative studies that examine the lived experience of health-care workers in Asia and comprises over 100 in-depth interviews. To competently process and accurately analyze such large volume of data poses numerous challenges and complexities. These were addressed by investigator triangulation and members checking to ensure inter-subjectivity in the analytical process, while enhancing trustworthiness in data interpretation. Future research can further contribute to this body of work by exploring the challenges of other non-palliative care medical disciplines such as those of the Accident and Emergency units and paramedics.
Conclusion
This study has identified the challenges of NPCPs caring for end-of-life patients in Singapore and presented these findings through an interrelated and systemic lens. The implications and recommendations in this paper will further the advancement of theories and inform practices for supporting NPCPs in the provision of quality end-of-life care. With the alleviation of challenges that they face in their daily endeavors, NPCPs would be able to focus their efforts and abilities on providing high quality of care to their patients and families, as well as experience positive stimulation in their life’s chosen work. This necessitates intentional, meaningful, and sustainable changes throughout the health-care ecosystem and larger society.
Acknowledgments
We would like to express our appreciation and gratitude to all of our key informants for sharing their vulnerable insights and lived experiences in end-of-life care. All authors were involved in the conceptualizing of the study, in formulating the questions for the interview, and in preparing the manuscript.
Conflicts of interest
The authors declare none.
Ethical approval
Ethical approval for this study is obtained from the Institutional Review Board of Nanyang Technological University (IRB-2019-03-025).




