Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) means that the patients are treated in the hospital for several weeks due to aggressive immunosuppressive chemotherapy and immune system reconstitution, after which they are monitored in outpatient care for many months due to the risk of severe side effects (Gyurkocza et al., Reference Gyurkocza, Rezvani and Storb2010). Even though the goal of allo-HSCT is to cure from a fatal disease, mainly hematological cancer, approximately one-fourth of patients suffer a relapse, the 1-year transplant-related mortality is around 13% and the probability of 3-year survival after allo-HSCT is around 70% (Remberger et al., Reference Remberger, Ackefors and Berglund2011).
During the allo-HSCT trajectory, patients need care and support from their family members, especially when returning home after the long hospital stay, and there are indications that the level and quality of caregiver support influences patients’ transplant experience (Rini et al., Reference Rini, Emmerling and Austin2015). Being a family caregiver in allo-HSCT often includes providing practical and physical care to the patient, as well as emotional support (Bergkvist et al., Reference Bergkvist, Larsen and Johansson2018). Among family caregivers, 50% report anxiety and 74% depressive symptoms pre-transplantation (Sannes et al., Reference Sannes, Simoneau and Mikulich-Gilbertson2019), while caregiver burden appears to be a constant source of stress that adversely affects family caregivers’ quality of life (QoL) up to 1 year after allo-HSCT (Sabo et al., Reference Sabo, McLeod and Couban2013). Family caregivers in allo-HSCT experience a high sense of uncertainty prior to transplantation due to, among other things, the lack of information about the patient's disease and the side effects of treatment (Bergkvist et al., Reference Bergkvist, Winterling and Kisch2020). The unique life situation of family caregivers in allo-HSCT comprising of high responsibility, a great sense of uncertainty about the future and long-term worries, is also explained by the patient's high risk of relapse and that her/his health status can change rapidly, which causes concern about what will happen next (Kuba et al., Reference Kuba, Esser and Scherwath2017; Bergkvist et al., Reference Bergkvist, Larsen and Johansson2018; Kisch et al., Reference Kisch, Bergkvist and Alvariza2020). If family caregivers are prepared for the tasks and demands of the caregiving role prior to allo-HSCT, their situation during the distressing time of the allo-HSCT trajectory might be easier.
Hudson put forward a theoretical model for conceptualizing supportive interventions for family caregivers in end-of-life care, which was underpinned by Folkman's (Reference Folkman1997) adapted stress-coping model. The Hudson model includes several concepts that may be important in family caregivers’ coping process and one of the key concepts is preparedness for caregiving (Hudson, Reference Hudson2003). Preparedness for caregiving is defined as perceived readiness for the multiple domains of the caregiving role, i.e., the tasks and demands of the caregiver role including the provision of practical care and emotional support, but also for managing the stressors related to caregiving (Archbold et al., Reference Archbold, Stewart and Greenlick1990). Preparedness has been shown to be associated with lower levels of caregiver strain among family caregivers to older patients discharged from the hospital (Archbold et al., Reference Archbold, Stewart and Greenlick1990) in palliative cancer care (Henriksson and Arestedt, Reference Henriksson and Arestedt2013), in curative cancer care (Fujinami et al., Reference Fujinami, Sun and Zachariah2015), as well as in allo-HSCT care (Eldredge et al., Reference Eldredge, Nail and Maziarz2006). Furthermore, associations between preparedness and other concepts suggested as important in Hudson's theory have been explored in curative and palliative cancer care. These studies indicate that higher preparedness is associated with lower distress (Fujinami et al., Reference Fujinami, Sun and Zachariah2015), better mood (Schumacher et al., Reference Schumacher, Stewart and Archbold2007), and less anxiety although it was not related to less depression or better general health (Henriksson and Arestedt, Reference Henriksson and Arestedt2013). Moreover, higher preparedness is associated with stronger feelings of hope (Henriksson and Arestedt, Reference Henriksson and Arestedt2013) and reward (Eldredge et al., Reference Eldredge, Nail and Maziarz2006; Henriksson and Arestedt, Reference Henriksson and Arestedt2013). Hudson (Reference Hudson2003) also include the concepts of self-efficacy and competence in his model as important for enabling family caregivers to handle their caregiver situation, but there seems to be a lack of knowledge regarding the associations between preparedness for caregiving and these two concepts. Hudson's model was developed for family caregivers to patients with life-threatening illness who were close to death. The model can also be used when investigating key concepts that might influence how family caregivers handle the caregiving situation in curative cancer care, such as during allo-HSCT. However, to the authors’ knowledge, no associations between preparedness for caregiving and caregiver burden, anxiety/depression, competence, self-efficacy, and general health have been investigated in an allo-HSCT context, with the exception of a study showing a negative association between preparedness and caregiver burden (Eldredge et al., Reference Eldredge, Nail and Maziarz2006).
The experience of caregiving might also be influenced by demographic factors such as age, gender, and socioeconomic status, i.e., education (Hudson, Reference Hudson2003) as well as the nature of the relationship between the patient and the family caregiver, for example, if the caregiver is a spouse, parent, or friend. In cancer care, there are divergent results regarding the importance of age (Papastavrou et al., Reference Papastavrou, Charalambous and Tsangari2009; Li et al., Reference Li, Mak and Loke2013; Akgul and Ozdemir, Reference Akgul and Ozdemir2014) and the relationship with the patient (Papastavrou et al., Reference Papastavrou, Charalambous and Tsangari2009; Langer et al., Reference Langer, Yi and Storer2010; Li et al., Reference Li, Mak and Loke2013), but it has been reported that being female (Li et al., Reference Li, Mak and Loke2013) and having a lower educational level (Papastavrou et al., Reference Papastavrou, Charalambous and Tsangari2009; Langer et al., Reference Langer, Yi and Storer2010; Simoneau et al., Reference Simoneau, Mikulich-Gilbertson and Natvig2013; Akgul and Ozdemir, Reference Akgul and Ozdemir2014) are associated with more negative caregiver outcomes such as caregiver burden, depression, and distress. Only a few studies have explored the relationship between age, gender, relationship, and preparedness. One study showed that being female and living with the patient were associated with higher levels of preparedness for caregiving, while age and being the patient's partner were not (Henriksson and Arestedt, Reference Henriksson and Arestedt2013). In another study, being a partner was associated with higher levels of preparedness, compared to other kinds of relationships (Archbold et al., Reference Archbold, Stewart and Greenlick1990; Schumacher et al., Reference Schumacher, Stewart and Archbold2007).
Although it has been confirmed that preparedness for caregiving improves family caregivers’ well-being in cancer and palliative care, there is still limited knowledge in the allo-HSCT context, where family caregivers live in an uncertain situation and have a high level of responsibility for supporting the patient at home. The aim of this study was to explore whether demographic factors are associated with preparedness for caregiving prior to allo-HSCT and if such preparedness for caregiving is associated with caregiver outcomes in terms of caregiver burden, anxiety/depression, competence, self-efficacy, and general health among family caregivers.
Methods
Design
A correlational, cross-sectional design was used.
Setting, sample, and procedure
Family caregivers 18 years or older who were able to read and speak Swedish were included from two out of the six centers performing allo-HSCT in Sweden from 15 October 2017 to 14 November 2018. During the inclusion period, all 148 adult patients admitted to these centers for allo-HSCT were contacted by a HSCT-coordinator and asked if they would agree to identify one family caregiver prior to their transplant. Three patients stated that they did not have a family caregiver, three refused to allow their family caregiver to be asked to participate, and the family caregivers of 17 patients did not understand Swedish. Thus, 125 family caregivers were eligible for inclusion. They were informed about the study and given the questionnaire before the allo-HSCT started. However, 12 declined participation and 27 failed to return the questionnaire, resulting in a sample of 86 family caregivers (response rate 69%). Participants gave their written informed consent and ethical approval was obtained from the Regional Ethical Review Board in Stockholm (No. 2017/1112-31/4).
Measurements
The self-administered questionnaire included demographic questions about gender, age, marital status, living situation, and education, in addition to validated instruments.
The Preparedness for Caregiving Scale (PCS) measures caregivers’ readiness to provide care (Archbold et al., Reference Archbold, Stewart and Greenlick1990). It consists of eight items rated on a 5-point Likert-type scale ranging from “not at all prepared” (0) to “very well prepared” (4) with a total score from 0 to 32. A higher score indicates higher preparedness (Archbold et al., Reference Archbold, Stewart and Greenlick1990). The PCS has shown good validity and reliability in studies of family caregivers of patients in palliative care (Henriksson et al., Reference Henriksson, Andershed and Benzein2012).
The Caregiver Burden Scale (CBS) measures subjective burden experienced by caregivers (Elmstahl et al., Reference Elmstahl, Malmberg and Annerstedt1996). It consists of 22 items rated on a 4-point Likert-type scale, ranging from 1 to 4. Although the CBS has five subscales, in the present study only the 8-item “general strain” scale (CBS-GS) was used. The item scores are added together and divided by the number of items to obtain a mean score for each person, with a total score ranging from 1 to 4. Higher scores indicate higher caregiver burden. The CBS has shown satisfactory measurement properties in studies of family caregivers of patients with stroke (Elmstahl et al., Reference Elmstahl, Malmberg and Annerstedt1996).
The Hospital Anxiety and Depression Scale (HADS) measures symptoms of anxiety and depression in two 7-item subscales (Zigmond and Snaith, Reference Zigmond and Snaith1983). Each item has four response options, ranging from 0 to 3. The items in each subscale are summed and have a score ranging from 0 to 21, with higher scores indicating more severe symptoms of anxiety and depression. A score of ≥8 is used as the cutoff (Bjelland et al., Reference Bjelland, Dahl and Haug2002). The HADS has well-documented measurement properties in a broad range of groups (Bjelland et al., Reference Bjelland, Dahl and Haug2002).
The Caregiver Competence Scale (CCS) measures caregivers’ perceived adequacy of performance (Pearlin et al., Reference Pearlin, Mullan and Semple1990). It consists of four items rated on a 4-point Likert-type scale ranging from “not at all competent” (0) to “very competent” (3) with a total score from 0 to 12. A higher score indicates higher perceived competence. The CCS has shown good measurement properties in studies of family caregivers of palliative care patients (Henriksson et al., Reference Henriksson, Andershed and Benzein2012).
The General Self-Efficacy Scale (GSE) measures an individual's confidence in her/his ability to cope with critical or unusual situations (Schwarzer and Jerusalem, Reference Schwarzer, Jerusalem, Weinman, Wright and Johnston1995). It consists of 10 items rated on a 4-point Likert-type scale from 1 to 4, with a total score ranging from 10 to 40. A higher score indicates higher levels of self-efficacy. The GSE has shown good measurement properties in general populations (Love et al., Reference Love, Moore and Hensing2012).
General health was assessed using the global question about present health from the SF-36, “How would you rate your overall health” with five response options: excellent (1), very good (2), good (3), fair (4), and poor (5) (Ware and Sherbourne, Reference Ware and Sherbourne1992).
Statistical analysis
Missing data in the PCS, CBS-GS, HADS, CCS, and GSE were replaced if they did not exceed 20% (Downey and King, Reference Downey and King1998) using person-mean imputation (Bell et al., Reference Bell, Fairclough and Fiero2016). Descriptive statistics were applied to describe the characteristics of the participants and the Spearman's rank-order correlation coefficient (r s) was used to explore the association between caregiver burden, anxiety, depression, competence, self-efficacy, and general health.
A multiple linear regression analysis was conducted to explore the association between sociodemographic factors and preparedness for caregiving. The latter was used as the outcome variable and all hypothesized explanatory variables (gender, age, education, and relationship to the patient) were entered simultaneously (forced entry method). Hierarchical linear regression analyses in two blocks were conducted to investigate whether preparedness was associated with caregiver outcomes (caregiver burden, anxiety, depression, competence, self-efficacy, and general health). In the first block (univariate regression), each caregiver outcome was separately regressed on preparedness. In the second block (multiple regression), the regression model was adjusted for all four demographic factors. The regression diagnostics detected no severe violations in the regression models regarding linearity (scatterplots), homoscedasticity (Breusch–Pagan test), multicollinearity (VIF > 2), influential observations (Cooks distance > 4/n), and normally distributed residuals (normal probability plots and D'Agostino test of normality of the standardized residuals). One exception was the regression model with the HADS depression as the outcome in which the residuals deviated somewhat from a normal distribution. To handle this problem, a regression model with robust standard errors was conducted. In addition, we used ordinal logistic regression analysis to investigate whether preparedness was associated with general health (as it has an ordinal outcome). According to the Brant test, the assumption of parallel lines was not violated (χ 2(15) = 16.4, p = 0.36).
The level of statistical significance was set at p < 0.05. The statistical calculations were performed with SPSS 24.0 (IBM Corp., Armonk, NY, USA) and Stata 16.1 (StataCorp LLC, College Station, TX, USA).
Results
The participants
The characteristics of the participants and levels of caregiver outcomes are presented in Table 1. The final sample included 86 family caregivers with a median age of 56 years. About two-thirds were women (n = 65, 76%) and 66% (n = 57) were partners of the patient. Additionally, most of the family caregivers reported excellent/very good (n = 28, 33%) or good (n = 42, 49%) general health and only a few reported fair/poor general health (n = 14, 17%). More than half reported symptoms of anxiety (n = 48, 56%) and about one-third reported symptoms of depression (n = 24, 28%).
Table 1. Characteristics of the participants (n = 86)

Sociodemographic factors associated with preparedness for caregiving
Having a higher education (B = 2.72, p = 0.02) and being the patient's partner (B = 2.81, p = 0.03) were significantly associated with a higher level of preparedness for caregiving. Gender and age were not significantly associated with preparedness. The multiple regression model explained 15% of the total variance in preparedness (Table 2).
Table 2. Associations between demographic factors and preparedness for caregiving (multiple linear regression, forced entry, n = 85)

Dichotomous variables: gender (women/men), education (high/low), and relationship (partner/other).
Associations between preparedness for caregiving and caregiver outcomes
The univariate linear regression models in Block I revealed that higher levels of preparedness were significantly associated with lower symptom levels of depression (B = −0.14, p = 0.02), higher levels of caregiving competence (B = 0.22, p < 0.001), and higher levels of self-efficacy (B = 0.11, p < 0.001). These associations remained after the regression models in Block II were adjusted for gender, age, education, and relationship to the patient. The explanatory variables in the multiple regression models (Block II) explained between 9% and 41% of the total variance in the caregiver outcome variables. Caregiver burden and symptoms of anxiety were not associated with preparedness in either the univariate or multivariate regression models (Table 3). The ordinal logistic regression analyses demonstrated that higher levels of preparedness were significantly associated with higher levels of self-rated general health in both unadjusted (OR = 0.87, p = 0.001) and adjusted models (OR = 0.88, p = 0.00) (Table 4).
Table 3. Associations between preparedness for caregiving and caregiver outcomes (univariate and multiple linear regression, forced entry, n = 83–85)
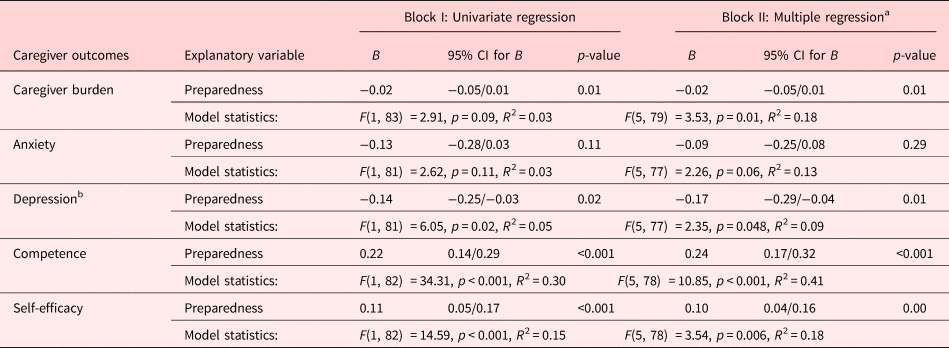
a Adjusted for gender, age, education, and relationship to the patient (not presented in the table).
b Linear regression with robust standard errors.
Table 4. Associations between preparedness for caregiving and general health (univariate and multiple ordinal logistic regression, n = 83)

Pseudo R 2 = McFadden's R 2.
a Adjusted for gender, age, education, and relationship to the patient (not presented in the table).
Associations between caregiver outcomes
No one of the outcomes were significantly associated with all other caregiver outcomes (Table 5). Except for the strong association between anxiety and depression (r s = 0.67, p < 0.001), the strongest associations were shown between depression and caregiver burden (r s = 0.54, p < 0.001), depression and general health (r s = 0.45, p < 0.001), anxiety and caregiver burden (r s = 0.38, p < 0.01), and anxiety and general health (r s = 0.34, p = 0.01) (Table 5).
Table 5. Associations between the caregiver outcomes (Spearman's rank-order correlation coefficient, pairwise deletion, n = 83–85)

* p > 0.05.
** p < 0.01.
*** p < 0.001.
Discussion
In summary, the result of the present study shows that those family caregivers who were more prepared for caregiving had significantly less symptoms of depression, higher competence, and self-efficacy, as well as better general health. However, no associations were found between preparedness for caregiving and anxiety or caregiver burden. Family caregivers who had a higher education and were the patient's partner were significantly more prepared for caregiving, while no associations were found with gender or age.
Family caregivers who were the patient's partner had a significantly higher level of preparedness for caregiving in allo-HSCT compared to non-partners, which is supported by previous findings from the cancer care context (Archbold et al., Reference Archbold, Stewart and Greenlick1990; Schumacher et al., Reference Schumacher, Stewart and Archbold2007; Henriksson and Arestedt, Reference Henriksson and Arestedt2013). It could be that partners have had a chance to prepare by receiving information and support from healthcare professionals prior to allo-HSCT, i.e., many meetings often take place between the patient, family caregivers, and healthcare professionals, which can provide a sense of involvement and security (Bergkvist et al., Reference Bergkvist, Winterling and Kisch2020). During the allo-HSCT recovery phase, family caregivers are often available 24 h a day to manage ongoing physical symptoms, attend multiple outpatient appointments, and navigate medication (Bergkvist et al., Reference Bergkvist, Winterling and Kisch2020). Many HSCT centers acknowledge the crucial role of caregivers in contributing to the effectiveness of care. It needs should be borne in mind that transitioning to a caregiver role is often challenging. For most people, it is a new experience and they may not be equipped to become caregivers and cope with the related responsibilities. This new role can lead to health problems and distress, with some caregivers at greater risk of having unmet support needs. A transition is defined as a passage from one life phase, condition, or status to another and has been described in the nursing literature as involving complex processes, including changes in identities, roles, relationships, abilities, and behavior patterns (Schumacher and Meleis, Reference Schumacher and Meleis1994). There are numerous factors that might influence transition, such as preparedness, knowledge, expectations, social context, and emotional and physical wellbeing (Schumacher and Meleis, Reference Schumacher and Meleis1994). Preparedness facilitates the transition experience and is related to knowledge about what to expect during a transition and what strategies may be helpful in managing it — something that could be supported by nursing interventions (Meleis et al., Reference Meleis, Sawyer and Im2000).
In the present study, family caregivers with a higher education reported greater preparedness for caregiving than those with a lower educational level. No existing studies have investigated this relationship, but our finding was not unexpected as previous studies among family caregivers show that higher levels of education are associated with a more positive caregiver experience (Papastavrou et al., Reference Papastavrou, Charalambous and Tsangari2009; Langer et al., Reference Langer, Yi and Storer2010; Simoneau et al., Reference Simoneau, Mikulich-Gilbertson and Natvig2013; Akgul and Ozdemir, Reference Akgul and Ozdemir2014). This could be due to an adequate level of health literacy. Although health literacy does not only depend on educational level but also on age, ethnicity, income, and multi-morbidity (Berkman et al., Reference Berkman, Davis and McCormack2010), several studies indicate that low health literacy is associated with increased caregiver burden and that when the caregiver plays a major role in self-management support it is of importance for self-management behaviors and use of health services by patients (Yuen et al., Reference Yuen, Knight and Ricciardelli2018). A previous systematic review points out that low health literacy may be improved by increasing knowledge and self-efficacy (Berkman et al., Reference Berkman, Sheridan and Donahue2011). It also seems likely that in a cancer care context, family caregivers with a high level of commitment to being properly informed and trained are more confident in their abilities and cope better with the challenge of managing disease-related problems (Prue et al., Reference Prue, Santin and Porter2015). This is supported by our study, where higher preparedness among family caregivers was significantly positively associated with both competence and self-efficacy. This has not been previously reported in the HSCT context, to the best of our knowledge, elsewhere. Enhancing family caregivers’ competence and self-efficacy for managing caregiving demands during the patients’ illness may be a key factor for reducing their psychological distress, as earlier studies in different groups of family caregivers indicate that higher competence is associated with lower caregiver burden (van der Lee et al., Reference van der Lee, Bakker and Duivenvoorden2014), while higher self-efficacy is linked to better health (Harmell et al., Reference Harmell, Mausbach and Roepke2011; Bevans et al., Reference Bevans, Wehrlen and Castro2014).
In our study, higher levels of preparedness were associated with lower levels of depression and better general health, but not with anxiety. This is in contrast to an earlier study in the palliative context in which higher preparedness was associated with less anxiety but not depression or better general health (Henriksson and Arestedt, Reference Henriksson and Arestedt2013). However, this and other studies indicate that higher levels of preparedness are associated with different dimensions of psychological well-being (Schumacher et al., Reference Schumacher, Stewart and Archbold2007; Henriksson and Arestedt, Reference Henriksson and Arestedt2013; Fujinami et al., Reference Fujinami, Sun and Zachariah2015). Health is a broad concept including physical, emotional, social, and existential aspects, and it is likely that preparedness is more associated with the emotional aspects of health. It is surprising that preparedness was not significantly associated with caregiver burden in the present study, as this has been shown in previous studies of cancer care (Archbold et al., Reference Archbold, Stewart and Greenlick1990; Fujinami et al., Reference Fujinami, Sun and Zachariah2015), and it is assumed that knowledge about what to expect would diminish family caregivers’ level of stress. There might be several explanations for this, e.g., how and when caregiver burden is measured as well as the patient's situation. Although the CBS-GS has been used among lung cancer patients (Borges et al., Reference Borges, Franceschini and Costa2017) and in the palliative context (Holm et al., Reference Holm, Arestedt and Carlander2017), the scale might not accurately capture the most important issues in a curative setting, such as great uncertainty about the future (Bergkvist et al., Reference Bergkvist, Larsen and Johansson2018). It is likely that caregiver burden will increase at a later stage of the transplantation process when the patient's functional status and QoL decrease, as caregiver burden is linked to the patient's functional status (Manskow et al., Reference Manskow, Sigurdardottir and Roe2015) and QoL (Borges et al., Reference Borges, Franceschini and Costa2017). This is strengthened by the fact that the participants in the present study reported lower levels of caregiver burden compared with caregivers in a palliative context (Holm et al., Reference Holm, Arestedt and Carlander2017) and severe traumatic brain injury context (Manskow et al., Reference Manskow, Sigurdardottir and Roe2015), but similar to caregivers of patients with lung cancer in all stages of the disease (Tan et al., Reference Tan, Molassiotis and Lloyd-Williams2018).
A recent review of seven efficacy studies on psychosocial interventions for caregivers in autologous and allogeneic HSCT patients was conducted, but none of these studies included preparedness as an outcome (Bangerter et al., Reference Bangerter, Griffin and Langer2018). Nevertheless, the review revealed that interventions had a positive effect on fatigue and mental health service use, but not on burden or sleep quality, while the effects on depression, anxiety, coping, and QoL were inconsistent (Bangerter et al., Reference Bangerter, Griffin and Langer2018). A newly published study investigated the effectiveness of an individual six-session psychosocial intervention for family caregivers in autologous and allogeneic HSCT care, where improved QoL, self-efficacy, and coping skills reduced caregiving burden, lower anxiety, and depression symptoms in comparison with a group that received standard care were reported (El-Jawahri et al., Reference El-Jawahri, Jacobs and Nelson2020). Coping and self-efficacy have been shown to be essential components of a brief psychosocial intervention that improves QoL and mood for caregivers of HSCT recipients during the acute recovery period (Jacobs et al., Reference Jacobs, Nelson and Traeger2020).
Our findings can be understood in relation to the conceptual model of caregiver support developed by Hudson (Reference Hudson2003). This model describes feelings of being prepared and/or rewarded as resources that influence the way family caregivers cope with the caregiving situation. However, preparedness is probably also influenced by other variables that were not considered in this study, for example, coping strategies, hope, the quality of the relationship, social network, and the patient's health status.
A way of increasing the preparedness for caregiving prior to allo-HSCT is to try to reduce their great uncertainty about the future (Bergkvist et al., Reference Bergkvist, Larsen and Johansson2018) that probably creates the high levels of anxiety and depression (Sannes et al., Reference Sannes, Simoneau and Mikulich-Gilbertson2019). In this situation as in many others information is considered a key element of support (Hudson, Reference Hudson2003). Earlier intervention studies in palliative care have demonstrated that preparedness of caregiving can be influenced by psycho-educational sessions in groups regarding the diagnoses and symptom relief, daily care and nutrition problems, support and existential issues (Henriksson et al., Reference Henriksson, Arestedt and Benzein2013; Holm et al., Reference Holm, Arestedt and Carlander2016). However, a problem when conducting interventions for caregivers is that those who have low levels of preparedness also have the lowest rates of using education and training services (Dionne-Odom et al., Reference Dionne-Odom, Applebaum and Ornstein2018), which is a difficulty when designing interventions that aim to increase preparedness. One way may be to structurally assess and address family caregivers’ preparedness and individual needs prior to allo-HSCT and from there enable them to use tailored individual psycho-educational support so that the family caregivers can better cope with their caregiving role, resulting in more positive experiences throughout the allo-HSCT trajectory.
A limitation in this study is the relatively small sample, explained by the fact that allo-HSCT recipients constitute a limited population, which increases the risk of type II errors. A related limitation is that no a priori power calculation was conducted. Nevertheless, the sample size can be deemed large enough as a univariate linear regression model requires 55 observations to detect a medium effect size (f 2 = 0.15, 1−β = 0.80, α = 0.05). The multiple linear regression analysis with four explanatory variables required 85 observations, which was fulfilled. However, the linear regressions with five explanatory variables required 92 observations and were therefore underpowered, which was also the case for the ordinal logistic regression. Nevertheless, the adjusted regression models confirmed significant associations detected in the univariate regression models. At the same time, despite the fact that the situation prior to the start of the allo-HSCT process is stressful for both patients and family caregivers, the rate of enrollment was good and included family caregivers from two allo-HSCT centers. However, it is possible that family caregivers who declined participation in studies are those with lower preparedness for caregiving, as a previous qualitative study revealed (Bergkvist et al., Reference Bergkvist, Winterling and Kisch2020) that it is more difficult to recruit family caregivers who are experiencing a higher level of burden. Unfortunately, there is no data about the characteristics of those caregivers who did not return the questionnaire, which is a limitation as it means that no drop-out analysis is possible, thus similarities and/or differences between those who returned the questionnaire and those who did not cannot be determined.
Furthermore, almost all of the family caregivers in our study were born in Sweden, and our results might not be relevant to caregivers of other ethnic backgrounds. However, a strength is that 50% of the sample have lower educational levels, which is a group that less often participates in research. Due to the cross-sectional design, no causal conclusions about the associations can be drawn.
In conclusion, this study contributes scientific knowledge about the preparedness of family caregivers in the unique life situation prior to allo-HSCT. By combining factors highlighted in the literature, we have shown that higher preparedness is significantly associated with higher levels of competence and self-efficacy, lower levels of depression, and better general health. These results indicate that it is valuable for family caregivers to be prepared for caregiving prior to allo-HSCT
Acknowledgment
We would like to thank the family caregivers who agreed to participate in this study as well as the staff who helped to recruit them.
Funding
This study was supported by the Swedish Blood Cancer Foundation.
Conflict of interest
There are no conflicts of interest.








