Introduction
Undoubtedly, COVID-19 is the biggest threat of global public health for 2020, since despite its low case fatality ratio (CFR), the easiness in transmission leads to a worldwide pandemic (Heymann and Shindo, Reference Heymann and Shindo2020). The value of R 0 of the disease during the early phase of the pandemic was estimated at 2.24–3.58 (Zhao et al., Reference Zhao, Lin and Ran2020), making the essential use of strict public health measures to set the transmission under control (Guo et al., Reference Guo, Li and Monroe-Wise2020).
Several studies have investigated the impact of COVID-19 on patients with chronic diseases. Through an analysis of 72,314 cases in China, it was found that the CFR was 10.5% for cardiovascular disease patients, 7.3% for diabetes, 6.3% for chronic respiratory syndrome, and 6% for hypertension, while the CFR of the general population was 2.3% (Wu and McGoogan, Reference Wu and McGoogan2020). In addition, even though the original data have not been published so far, it is widely accepted that patients receiving immunosuppressant or immunomodulatory therapy (e.g. those affected by multiple sclerosis) have an increased risk of complications and mortality from COVID-19 (Willis and Robertson, Reference Willis and Robertson2020). Furthermore, the disease outbreak has lead to treatment delays in patients with chronic diseases, such as cancer, which might be disturbing and affect the treatment outcome. For example, delaying therapies for gastrointestinal and lung cancer patients was considered necessary in China during the disease outbreak to prevent the risk of infection (Moujaess et al., Reference Moujaess, Kourie and Ghosn2020). Hence, patients with chronic diseases consist a highly vulnerable group during the COVID-19 outbreak, which has to be further studied.
Quarantine is a must-use measure during a disease outbreak to protect public health (Tognotti, Reference Tognotti2013; Parmet and Sinha, Reference Parmet and Sinha2020). In the current pandemic, this approached has been firstly used in China to set COVID-19 under control and to protect the health of vulnerable populations, such as patients with chronic illness (Guo et al., Reference Guo, Li and Monroe-Wise2020). Nevertheless, it is necessary to investigate the economic, societal, and psychological impact of this policy in order to improve the way it is implemented and to design strategies minimizing the negative effects, since the implementation of quarantine raises several ethical dilemmas (Upshur, Reference Upshur2003; Cetron and Landwirth, Reference Cetron and Landwirth2005).
To date, limited studies have investigated the mental health of people with chronic diseases while implementing quarantine policies. More specifically, in a relevant study in South Korea during the MERS outbreak in 2015, it was found that those with history of physical disease had increased odds for clinically significant anxiety 4–6 months after the quarantine (Jeong et al., Reference Jeong, Yim and Song2016). An additional study in the same country on quarantined hospitalized hemodialysis patients during the MERS outbreak found that 11% and 15.1% met the criteria for clinically significant anxiety and depression, respectively (Lee et al., Reference Lee, Kang and Cho2018). Concerning the outbreak of COVID-19 and related quarantine measures, a recent study in Spain during March 11–15, 2020 found that chronic disease patients had higher levels of stress, anxiety, and depression compared with healthy individuals (Ozamiz-Etxebarria et al., Reference Ozamiz-Etxebarria, Dosil-Santamaria and Picaza-Gorrochategui2020). Thus, chronic disease patients might have increased supportive care needs while placed in quarantine.
To date, no other relevant studies have been published, leading to several literature gaps, especially since the previous studies have not investigated patients with different types of chronic diseases while implementing quarantine policies. In that context, this study investigated mental health parameters of patients with chronic diseases during the COVID-19 outbreak in Greece.
Methods
Aim
The aims of the study were the following: (a) to search for an effect of quarantine duration on anxiety, depression, somatization, and distress of chronic disease patients and (b) to investigate differences between healthy individuals and patients with chronic diseases in anxiety, depression, somatization, and distress during the COVID-19 quarantine.
Study design
This study was part of a wider ongoing research to investigate mental health parameters in the Greek population, which started at December 2018. The research has gained approval by the appropriate Committee of the Medical School of the National and Kapodistrian University of Athens and complies fully with the Declaration of Helsinki. At the present study, all the eligible participants from the dataset completing the assessments between March 30, 2020 and May 4, 2020 were extracted to be further analyzed.
Participants
The inclusion criteria in the present study were the following: (a) age over 18 years old and (b) being able to communicate in Greek. The inclusion and exclusion criteria have not changed at any stage of the data collection process.
Assessments
Sociodemographic data
The sociodemographic data of the participants included gender (male/female), age (18–30/31–45/46–60/over 60), family status (married/unmarried living with a partner/unmarried living alone/divorced or widowed), having children (yes/no), educational level (primary/secondary/tertiary), smoking status (current smoker/occasional smoker/nonsmoker), and occupational status (unemployed/student/private sector worker/public sector worker/freelancer or businessman woman/pensioner/house worker).
The 4-dimensional symptom questionnaire
The 4-Dimensional Symptom Questionnaire (4DSQ) consists a self-reported instrument including 50 items scored on a Likert-type scale (0 = no to 4 = very much or always). This instrument includes four different subscales, measuring distress, anxiety, depression, and somatization (Terluin et al., Reference Terluin, van Marwijk and Adèr2006). The 4DSQ has been previously validated in Greek (Tsourela et al., Reference Tsourela, Mouza and Paschaloudis2013). In this study, the a level was 0.84 for depression, 0.88 for anxiety, 0.91 for distress, and 0.85 for somatization.
Procedures
As mentioned above, this study is part of a wider research investigating mental health parameters in the Greek population. Several posts on social networks containing a link leading to the assessments, also explaining the study purpose, the inclusion criteria, and the anonymity of participation, were used for participant recruitment. The posts were placed on groups with general content to increase the representativeness of the study sample. The participants pressing the link were guided to the assessments, which were completed instantly. The time needed to complete the assessments was estimated at approximately 5 min. The participants analyzed in the present study were those that have completed the assessments from March 30, 2020 till May 3, 2020. The beginning of this time interval was one week after the start of the quarantine, since the recall period of the 4DSQ is one week. Thus, since the quarantine started at March 23, 2020, using participants who completed the assessments prior to March 30, 2020 would lead to recalling symptoms placed before the beginning of the quarantine. The end of this interval refers to the last day of the quarantine in Greece. In the present study, the participants analyzed were those with no chronic disease (N = 943) and those with the following diseases: cardiovascular (N = 27), autoimmune (Ν = 37), chronic respiratory diseases (N = 29), and endocrine disorders (N = 22). These disease groups were included since at least 20 participants were found in the dataset for each of these subgroups. Patients with other diseases (e.g. schizophrenia) and patients with multiple chronic diseases (e.g. asthma and cancer) were analyzed in separate groups (N = 30 and 18, respectively). Thus, the first group consisted of healthy individuals and the other six patients with different types of chronic diseases.
Statistical analysis
The statistical analysis of the present study was carried out by the use of SPSS statistical software version 26 (SPSS, Inc., Chicago, IL). Absolute values and proportions were used for descriptive analysis regarding the demographic characteristics of the study. Since according to the Kolmogorov–Smirnov test the normality of the 4DSQ subscales was not violated, independent sample T-test was applied to investigate differences between healthy individuals and each subgroup with chronic disease. The effect size was calculated by the use of Glass's Δ. Pearson's correlation was used to investigate the relationship between the duration of quarantine and the 4DSQ subscales for the chronic disease and the healthy individuals’ group. The p-value was set at 0.05 for all the analyses.
Results
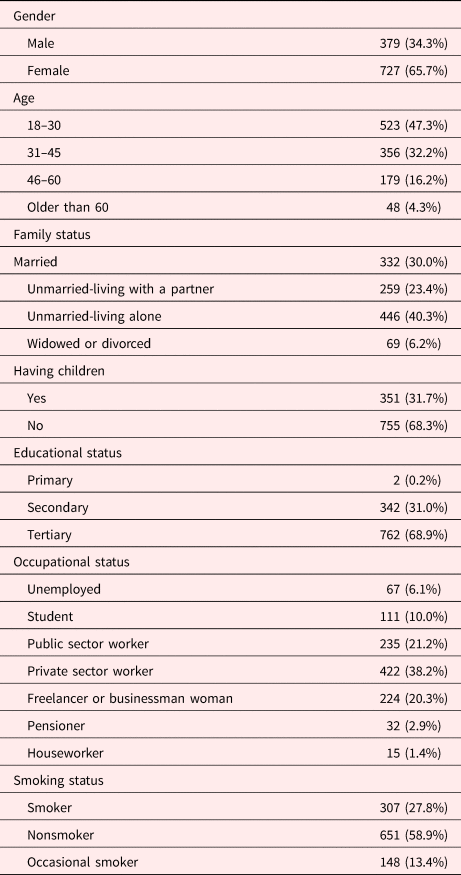
The sociodemographic data of the participants are presented in Table 1. As indicated in the table, the sample consisted mostly be females (65.7%). A considerable proportion of participants was between 18–30 years old (47.3%) and unmarried who lived alone (40.3%). Most of the participants did not have children (68.3%), were nonsmokers (58.9%) and had received tertiary education (68.9%). Private sector workers (39.2%) and public sector workers (21.2%) were the most frequent types of occupational status. Further information is presented in Table 1.
Table 1. The sociodemographic data of the study sample
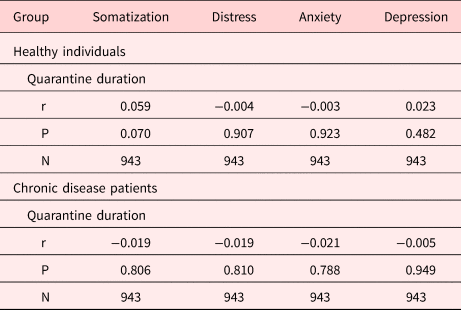
The correlation between quarantine duration and the 4DSQ subscales score is presented in Table 2. As indicated in the table, there was no correlation between quarantine duration and the subscales’ scores both in the healthy individuals and the chronic disease patients group.
Table 2. The correlation between quarantine duration and the 4DSQ subscales in healthy individuals and chronic disease patients
With regard to differences in 4DSQ subscales between healthy individuals and chronic disease patients, the relevant analysis is presented in Table 3. As indicated in the table, chronic disease patients had statistically significant higher scores in somatization (p = 0.000) and distress (p = 0.001). The differences in anxiety and depression were not statistically significant (p = 0.098 and 0.052, respectively).
Table 3. The differences in 4DSQ subscales between healthy individuals and chronic disease patients
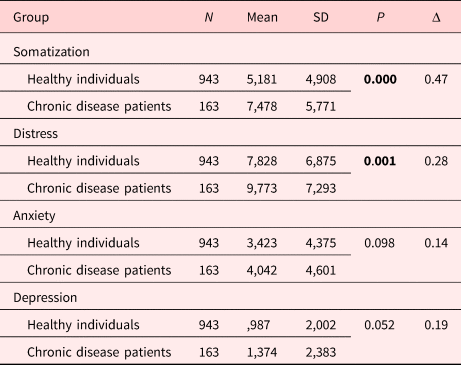
All the statistically significant values have been highlighted in bold.
The mean value of the 4DSQ distress subscale was 7.828 for healthy individuals (SD 6.875). Statistically significant differences were noted only when compared with patients with respiratory diseases (p = 0.028), as shown in Table 4.
Table 4. The differences in distress between healthy individuals and each patient group
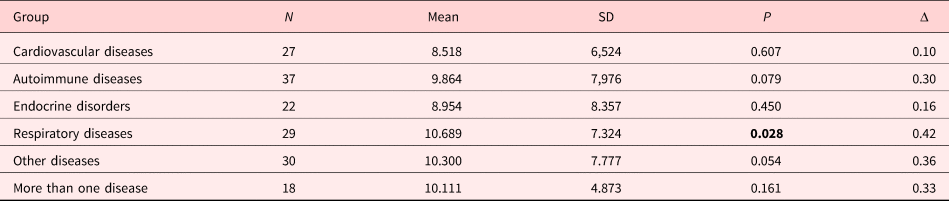
All the statistically significant values have been highlighted in bold.
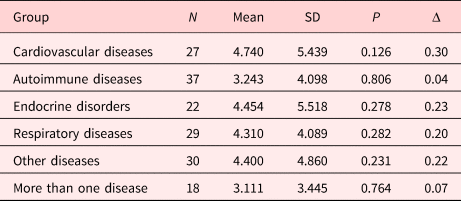
The mean value in the 4DSQ anxiety subscale was 3.423 for healthy individuals (SD 4.375). As indicated in Table 5, there were no statistically significant differences with any of the patient groups.
Table 5. The differences in anxiety between healthy individuals and each patient group
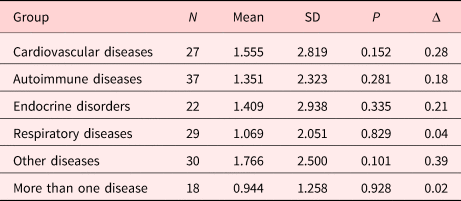
The mean value of 4DSQ depression was 0.987 for the healthy individuals group (SD 2.002). The comparisons with each of the patient groups of the study did not lead to statistically significant differences in depression, as shown in Table 6.
Table 6. The differences in depression between healthy individuals and each patient group
The mean value of the 4DSQ somatization subscale was 5.181 for the healthy individuals group (SD 4.908). Concerning the differences in somatization between healthy individuals and each patient group, the relevant analysis is presented in Table 7. As indicated in the table, most patient subgroups had statistically significant higher scores of somatization.
Table 7. The differences in somatization between healthy individuals and each patient group
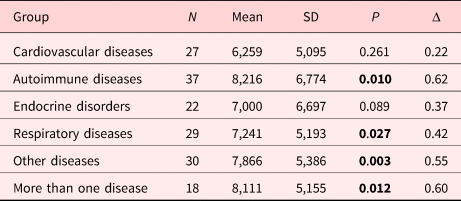
All the statistically significant values have been highlighted in bold.
Discussion
This study aimed to investigate the correlation between time spent on quarantine and the 4DSQ subscales in chronic disease patients in contrast to the relevant correlation in healthy individuals, as well as to search for differences in the scores of these subscales based on the disease status of the participants. The first main finding of the study is that there is no correlation between the 4DSQ subscales and time spent on quarantine neither for the healthy individuals nor for the chronic disease group. The second finding regards the significantly higher levels of distress and somatization in chronic disease patients, while anxiety and depression have no difference compared with healthy individuals. The analyses per disease indicate that endocrine and cardiovascular disease patients are not significantly affected, since they did not differ from healthy individuals in any of the 4DSQ subscales. Autoimmune patients, those affected by more than one disease and patients with other diseases, differ from healthy individuals only in somatization. Patients affected by respiratory diseases have additional supportive care needs, since they differ from healthy individuals in more than one parameter (somatization and distress). Of note, all the analyses indicated a nonsignificant effect on patient depression and anxiety.
The absence of significant associations between the 4DSQ subscales and quarantine duration is in line with previous studies concerning the association between quarantine duration and psychopathological manifestations in the general population. For example, during the COVID-19 massive quarantine in China, it was found that time was unrelated to the intensity of anxiety levels (Hu et al., Reference Hu, Su and Qiao2020), while, in a previous study in Toronto, Canada during the SARS outbreak, it was found that quarantine duration was not significantly related to depressive symptoms, although there was a trend toward a positive association (Hawryluck et al., Reference Hawryluck, Gold and Robinson2004). The results of the present study confirm and expand the current knowledge, since, both in the healthy individuals and in the chronic disease patient group, there was no association between the 4DSQ subscales and time spent in quarantine.
A paradoxical finding of the present study has to do with the absence of higher depressive levels for chronic disease patients during the lockdown, since, according to the previous study in Greece, chronic disease patients have higher levels of depressive symptoms compared with healthy individuals (Gerontoukou et al., Reference Gerontoukou, Michaelidoy and Rekleiti2015). The absence of differences could be attributed to mechanisms activated during societal threat in collective-oriented societies, such as Greece. More specifically, during the 2015 capital controls, a study in breast cancer patients found that depressive symptoms were queerly lower during that period of economic and political destabilization, a finding that could be attributed to an increase of social support toward the vulnerable during the general societal threat (Pelekasis et al., Reference Pelekasis, Kampoli and Ntavatzikos2017). Similar mechanisms could have been activated during the current crisis, leading to higher support toward patients with chronic diseases, and positive effects on depressive levels, leading to the absence of differences from healthy individuals.
Nonetheless, since this study found higher levels of distress and somatization for chronic disease patients, developing and implementing appropriate mental health interventions during quarantine policies is essential. In addition, as indicated from a study during the SARS outbreak, psychopathological manifestations could lead to extra secretion of catecholamine, which causes instability of myocardial electricity and adverse outcomes on cardiovascular disease patients (Pan et al., Reference Pan, Zhang and Li2003). As for patients with autoimmune diseases, such as multiple sclerosis, it is supported that COVID-19-related anxiety could lead to disease exacerbations (Ahadi et al., Reference Ahadi, Sahraian and Rezaeimanesh2020). Thus, developing and applying appropriate interventions for chronic disease patients during a pandemic is essential.
As for the content of those interventions, aiming only at mental health parameters might be somehow restricting, since chronic disease patients might have additional supportive care needs while placed in quarantine. Interestingly, it has been supported that an underrated threat for chronic disease patients, such as cardiovascular, regards the absence of physical activity during quarantine, which could lead to a further risk for adverse outcomes (Mattioli et al., Reference Mattioli, Puviani and Nasi2020). For that reason, it is essential to design appropriate interventions targeting both the improvement of mental health and the adoption of a healthy lifestyle during the quarantine. In Greece, recent studies testing the effectiveness of a relevant culturally oriented intervention entitled "Pythagorean Self-Awareness" indicate a wide range of benefits for mental health and health behaviors of patients with chronic diseases, such as cancer and multiple sclerosis (Darviri et al., Reference Darviri, Zavitsanou and Delikou2016; Anagnostouli et al., Reference Anagnostouli, Babili and Chrousos2019; Charalampopoulou et al., Reference Charalampopoulou, Bacopoulou and Syrigos2020). Thus, developing and applying an internet-based intervention using this content could lead to improvements in mental health and health behaviors of patients with chronic disease during a future COVID-19 quarantine or generally in future pandemics.
A few limitations for this study have to be reported. At first, internet data collection is prone to selection bias, since potential participants with no or low access to the internet have a smaller chance to be included (Bethlehem, Reference Bethlehem2010). Even though carrying out an internet-based data collection process was unavoidable due to the lockdown, this leads to a selection bias that cannot be ignored. The young age of the study participants and the high proportion of those with no children reflect this type of bias. In addition, there could be a sample size bias, since not using a relevant formula to determine the optimal sample size indicates that the results of a study are prone to this type of error (Campbell and Machin, Reference Campbell and Machin1999). Finally, it is unclear if the differences recorded between patients and healthy individuals are similar to those under normal circumstances, since patients with chronic diseases, especially those with advanced illness, have a generally higher risk of psychopathology compared with healthy individuals (Turner and Kelly, Reference Turner and Kelly2000; Tremblay and Breitbart, Reference Tremblay and Breitbart2001; Gerontoukou et al., Reference Gerontoukou, Michaelidoy and Rekleiti2015; Rabiee et al., Reference Rabiee, Nikayin and Hashem2016).
Relevant studies have to be carried out in other countries to understand if the differences reported at the present study account only for Greece or are general. More specifically, Greece is considered as a successful case in COVID-19 outbreak management (Tsiotas and Magafas, Reference Tsiotas and Magafas2020). Hence, studies in other countries more significantly affected by the outbreak (e.g. Italy, Spain, and France) could allow us understand if the effects are similar across different countries or are influenced by the degree that each country was affected by the pandemic.
Conclusions
This study investigated the effect of massive quarantine during COVID-19 in Greece on distress, anxiety, depression, and somatization of patients with chronic diseases. Distress and somatization were increased in chronic disease patients, while anxiety and depression were not. Endocrine and cardiovascular disease patients were not significantly affected, since they did not differ from healthy individuals in any of the 4DSQ subscales. Patients affected by respiratory diseases had additional supportive care needs, since they scored significantly higher from healthy individuals in more than one parameter (somatization and distress). Autoimmune patients, those affected by more than one disease and patients with other diseases differed from healthy individuals only in somatization. Since this study indicates that chronic disease patients have additional supportive care needs, developing and delivering relevant interventional programs during pandemics is essential.
Funding
This research received no specific grants from any funding agency in either the public, commercial, or not-for-profit sector.
Conflict of interest
The authors hereby state that they have no potential conflicts of interest to declare.










