Introduction
The COVID-19 pandemic caused many changes in parent’s lives, including the need to support virtual learning, job loss, and effects of stay-at-home orders (Gassman-Pines et al. Reference Gassman-Pines, Ananat and Fitz-Henley2020). As a result, many parents report significant declines in their well-being, including worse mental health (Bargon et al. Reference Bargon, Batenburg and Van Stam2020; Ciążyńska et al. Reference Ciążyńska, Pabianek and Szczepaniak2020; Wimberly et al. Reference Wimberly, Towry and Caudill2021). Parents of children with cancer may be particularly at-risk for psychological distress during the pandemic given additional financial strain (Carrera et al. Reference Carrera, Kantarjian and Blinder2018), treatment isolation guidelines (Björk et al. Reference Björk, Wiebe and Hallström2009; Henry et al. Reference Henry, Leprince and Garcia Robles2020), transitioning to at-home care (Branowicki et al. Reference Branowicki, Vessey and Temple2016), and barriers to social support (McCubbin et al. Reference McCubbin, Balling and Possin2002). Research suggests managing a child’s cancer diagnosis can cause psychological stress (Cadman et al. Reference Cadman, Rosenbaum and Boyle1991; Pai et al. Reference Pai, Greenly and Lewandowski2007); however, less is known about risks for adverse mental health outcomes during the pandemic for parents of children with cancer.
U.S. adult depression levels increased 3-fold over pre-pandemic levels (Ettman et al. Reference Ettman, Abdalla and Cohen2020). Among parents, approximately half reported stress levels to be an 8 or higher on a 10-point scale (APA 2020). Parents of children with cancer have experienced increased stress from health-care changes and social isolation (Ciążyńska et al. Reference Ciążyńska, Pabianek and Szczepaniak2020; Wimberly et al. Reference Wimberly, Towry and Caudill2021) and heightened anxiety regarding their child’s health (Guido et al. Reference Guido, Marconi and Peruzzi2021). Contrarily, other studies report little change (Auletta et al. Reference Auletta, Adamson and Agin2020; Janssen et al. Reference Janssen, Kullberg and Verkuil2020; van Gorp et al. Reference van Gorp, Maurice‐Stam and Teunissen2021). Understanding unique challenges faced by parents during COVID-19 is particularly important given families already face significant challenges from caring for a child with cancer (Bowman et al. Reference Bowman, Rose and Deimling2006; Nijboer et al. Reference Nijboer, Tempelaar and Sanderman1998).
Parents of children with cancer must navigate the pandemic as well as changes to health care and uncertainties about COVID-19 infection in their immunocompromised child (Wimberly et al. Reference Wimberly, Towry and Caudill2021). COVID-19 suspended randomized control trials, limiting treatment options (Auletta et al. Reference Auletta, Adamson and Agin2020), and imposed increased infection control measures and visitor restrictions at hospitals (Cakiroglu et al. Reference Cakiroglu, Yeltekin and Fisgin2021). Additionally, families of survivors have had reduced access to care (e.g., supportive services, follow-up screening) (Auletta et al. Reference Auletta, Adamson and Agin2020; Kahn et al. Reference Kahn, Schwalm and Wolfson2022). Beyond these health-care changes, financial strain from the pandemic has caused disruption to families’ ability to pay for basic needs and health care, imposing further anxiety (Wimberly et al. Reference Wimberly, Towry and Caudill2021). Given the general mental health risks faced by parents and added risks due to COVID-19 (van Gorp et al. Reference van Gorp, Maurice‐Stam and Teunissen2021), additional research is needed to understand the experiences of parents of children with cancer during the pandemic. Further, qualitative research on this topic remains limited.
The purpose of this paper is to qualitatively describe the experience of parents of children with cancer during the COVID-19 pandemic. Given pre-existing stressors faced by families of children with cancer, we expected parents to report significant impacts to their family and challenges caring for their child with cancer. By hearing parent perspectives, we hope to better inform health-care services and family-based interventions to alleviate parental distress from the pandemic and improve emotional well-being for these families.
Methods
This study received approval from the Institutional Review Board (STUDY00001575). Consent for participation was implied from survey completion. Data come from a larger web-based study examining the impact of COVID-19 on families of children with cancer. Participants were recruited between February and May 2021 using Facebook advertisements (Fig. 1) in partnership with Momcology®, a community-based organization for pediatric cancer caregiver support. Eligible participants were English-speaking parents of children (≤18 years) with a cancer diagnosis. Eligibility was assessed with a short questionnaire at the start of the survey. Participants completed the COVID-19 Exposure and Family Impact Scale (CEFIS) (Kazak et al. Reference Kazak, Alderfer and Enlow2021) followed by an open-ended prompt: “Please tell us about other effects of COVID-19 on your child/ren and your family, both negative and/or positive.”

Figure 1. Facebook Recruitment Advertisement.
Participants
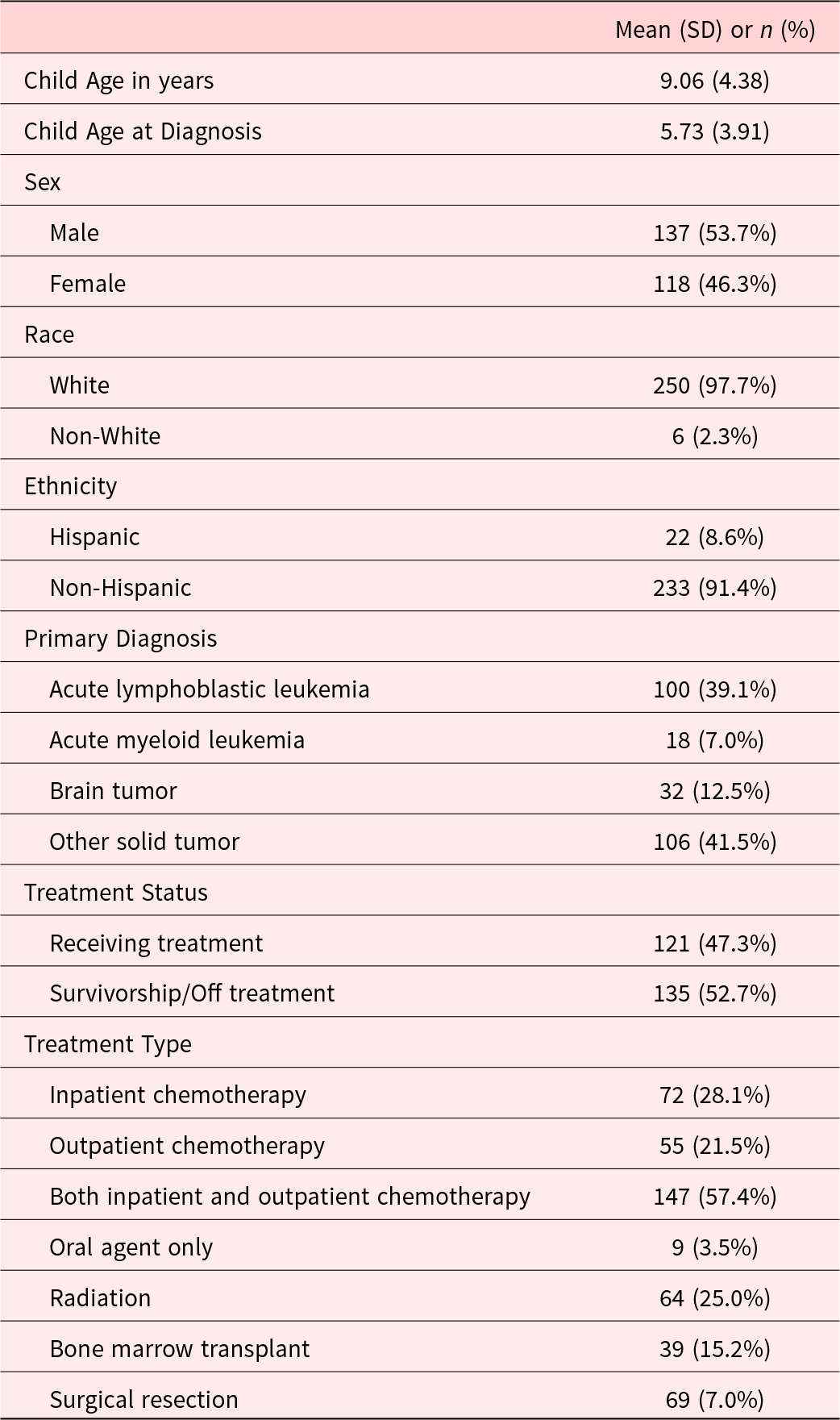
The survey yielded 296 responses to the open-ended question, of which 256 were included for analysis. Forty responses were identified as bots (e.g., duplicate enrollment, automated enrollment by software applications), using a method employed in previous social media research (Pozzar et al. Reference Pozzar, Hammer and Underhill-Blazey2020), and excluded. Thus, the final sample included 256 self-identified parents of children with cancer. Demographic characteristics of parents and children are described in Tables 1 and 2, respectively.
Table 1. Parent characteristics (N = 256)

Table 2. Child characteristics (N = 256)
Analysis
All 256 responses were coded by 2 trained research coordinators (C.J.S and M.S.S). Reponses were qualitatively analyzed via QSR NVivo (Version 11) (Q.I.P. Ltd. 2015) using open coding, in which themes were identified from the data (Khandkar Reference Khandkar2009). A team of 3 researchers (M.A.S, M.S.S, and C.J.S) began the process by reading 20 responses and noting emerging ideas using thematic content analysis (Anderson Reference Anderson2007). First, the 3 researchers read responses, in batches of 20, noting emerging ideas. Second, after 40 responses were read, the team met to generate a list of tentative categories. Third, these categories were organized into a list of themes. Fourth, the research team used the constant comparison method to sort and define themes (Glaser Reference Glaser1965) as they continued to read responses in batches of 50. This iterative process continued in sets of 50 until all responses have been read. Fifth, once it was determined that saturation had been reached, the final list of themes was decided, and definitions were detailed for each theme. The 2 coders used the agreed upon codebook to create frequency counts in NVivo for all themes. All coded responses were additionally coded for sentiment analysis (defined as positive or negative) by both coders individually and then compared to determine reliability. Sixth, the research team identified and discussed participant quotes to represent themes within the descriptive analysis.
Results
Six major themes emerged: (a) family changes, (b) social isolation, (c) emotional impact, (d) school changes, (e) health-care changes, and (f) physical health. Figure 2 illustrates the significant observed overlap between these themes. Many parents focused on the overarching family changes resulting from the pandemic, while others focused on specific changes in their children’s lives. Parents reported that these changes caused feelings of social isolation and emotional impacts.
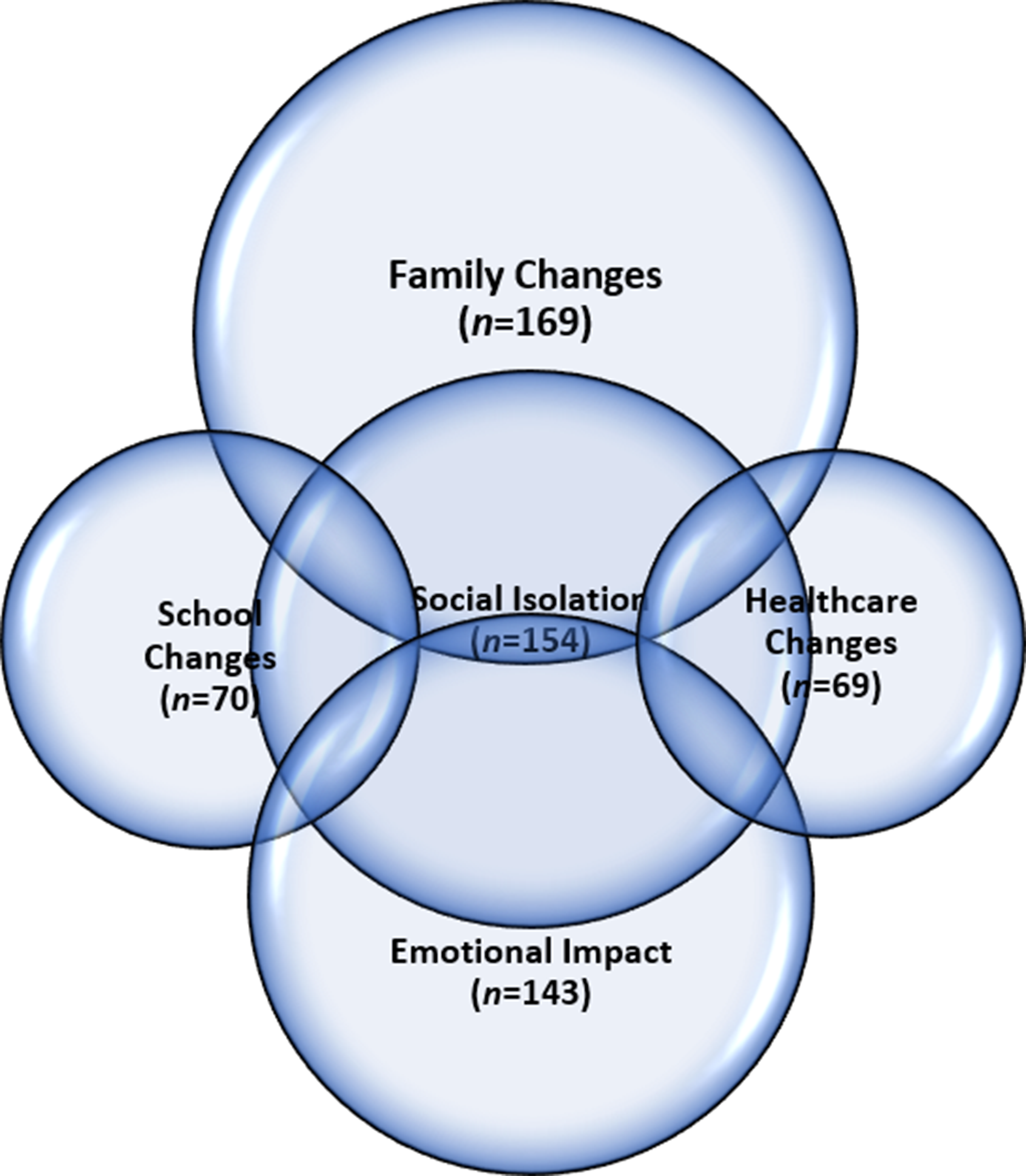
Figure 2. Observed Overlap of Qualitative Themes.
There was a total of 638 coded references from the 256 unique responses. Total number of references will be referred to throughout the results. Overall, the coders had 94% agreement. The average kappa score for the 6 themes was 0.78 for inter-rater reliability. Most references came from themes (a), (b), and (c), of which there were 169 (26%), 154 (24%), and 143 (22%) references, respectively. Sentiment analysis revealed 83% of references across themes were negative; however, family changes contained 39% positive references. Table 3 provides a comprehensive list of sample quotations.
Table 3. Themes and exemplar quotes from parents of children with cancera
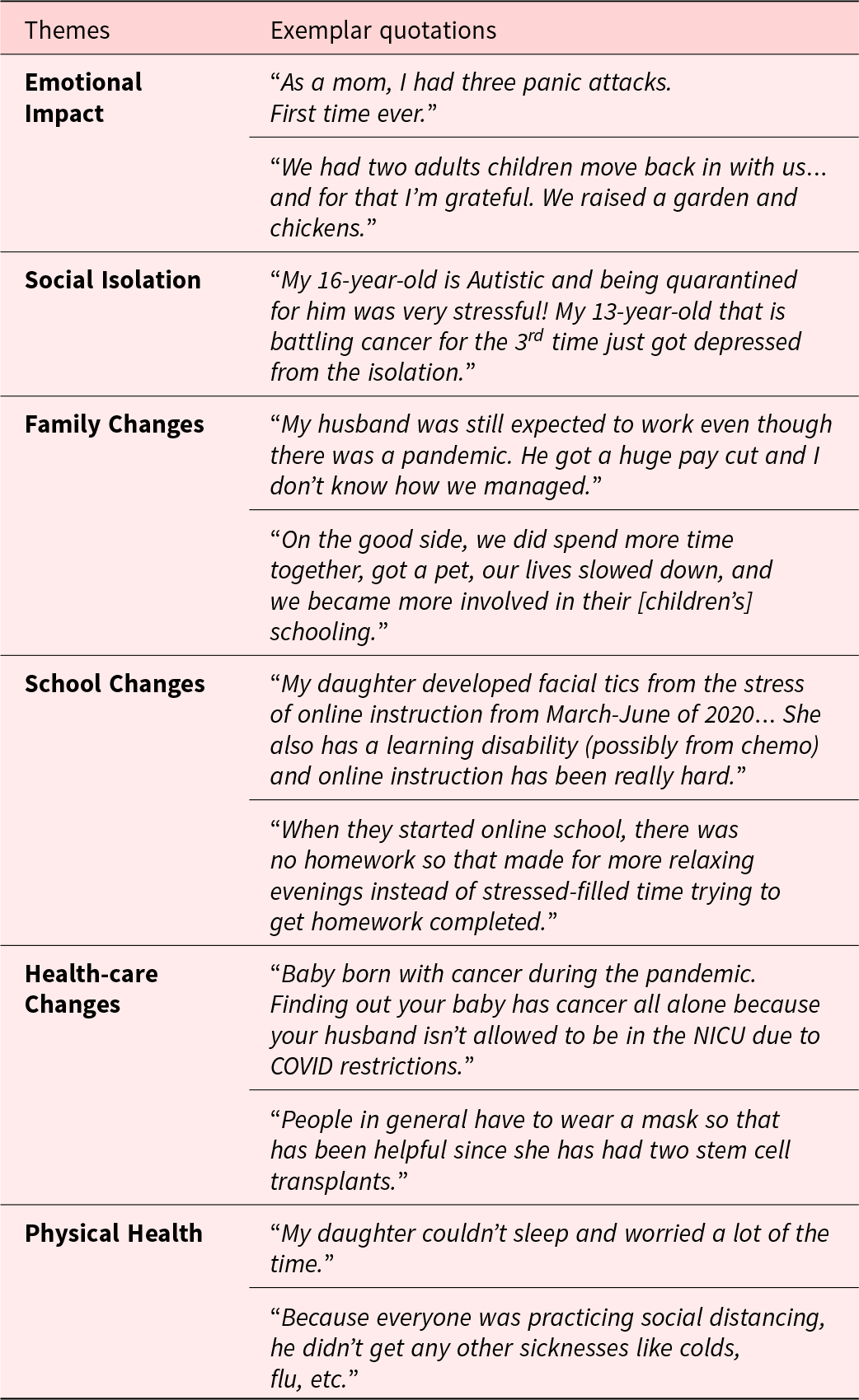
a Gray boxes indicate negative sentiment and white boxes indicate positive sentiment.
Family changes
Family changes resulting from COVID-19 was a prominent overarching theme (n = 169 references, 26% of references) and was expressed in conjunction with many of the other themes; 103 (61%) were negative. Some examples of family changes included financial challenges, changes in family routine and functioning, loss of family members, and time spent together. Out of all themes, family changes contained the highest proportion of positive sentiment (n = 66, 39%). The source of this positive sentiment was often the increased time spent together as a family. Negative sentiment mostly involved challenges balancing work and childcare responsibilities at home.
Negative family changes
Families experienced role changes as parents managed helping their children with virtual learning, working remotely, and their child’s medical care. As a result of job loss or limited capacity to work, parents experienced financial hardships while facing the high costs of medical care.
I’ve taken on a part time job in a warehouse to help make ends meet to keep up with medical bills. (mother of a 4-year-old son with a brain tumor)
Parents also reported changes in family structure during the pandemic:
With a three-year-old in treatment in the hospital and a baby at home, our family was split for a third of the year. I had to quit my nursing job to take care of my kids since my daughter was immunocompromised and we weren’t comfortable asking for help. (mother of a 3-year-old daughter with a brain tumor)
Positive family changes
Despite challenges, a subset of parents reported positive changes (n = 66, 39%). A commonly mentioned change was increased time together.
We have grown together as a family, eaten together more, walked together more, and in general spend more time together. (mother of an 8-year-old child with rhabdomyosarcoma)
Parents also expressed gratitude to be away from the hospital:
The positive was finally being home and having my older son home from college, so we were all together, and just so grateful to be home and out of the hospital. (mother of a 15-year-old son with acute myeloid leukemia (AML))
Remote work provided some parents reprieve while navigating their responsibilities caring for their child with cancer.
I was able to provide her better care since I was able to work from home. (mother of a 10-year-old daughter with rhabdomyosarcoma)
Social isolation
Social isolation (n = 154, 24%) was another overarching theme that affected many facets of families’ lives including work, health care, home environment, and school. All references to social isolation were coded as negative sentiment. Many parents reported feeling isolated due to quarantine and socially distancing from others. Families described the implications of missed activities and the challenges of working remotely.
Unable to celebrate my son’s graduation, unable to celebrate end of treatment, unable to freely visit with friends. (mother of a 15-year-old-daughter with Ewing’s sarcoma)
One parent described concern regarding her son’s friendships:
He was prevented by his school district from participating in classroom activities during treatment and transplant, so he lost all his relationships with his friends. He was just starting to make progress, when the schools were shut down, and he has had no further contact with kids from school. (mother of a 12-year-old son with acute lymphoblastic leukemia (ALL))
Hospital visitor restrictions (both inpatient and outpatient) allowing for only one visitor at a time isolated parents from their children and spouses. These restrictions also led to less interactions for the child with nurses, medical support staff, family, and friends.
Clinic visits were stressful for my daughter. She usually fills her time at the clinic playing in the playroom and walking the halls talking to the nurses. Now she has to spend long clinic days stuck in her room. (mother of a 4-year-old daughter with ALL)
She was not allowed visitors of any kind, except one parent, despite the fact that she had a terminal illness. (mother of a 5-year-old daughter with a brain tumor)
Parents felt isolated from their friends and other support networks. Parents emphasized the impact of losing support from their community that lightened the burden of caring for their child with cancer.
We have not been able to rely on our ‘village’ for emotion support. (mother of an 11-year-old daughter with ALL)
Emotional impact
Many parents described the emotional impact their family experienced during the pandemic (n = 143, 22%). Negative emotional impacts included increased anxious and depressive symptoms, health anxiety, and stress. One common positive emotional impact mentioned was acceptance of socially isolating given previous experience with this from their child’s cancer.
Negative emotional impact
Eighty-nine percent (n = 127) of references to emotional impact expressed negative sentiment. For families off therapy, COVID-19-related public health measures precluded families from experiencing the freedom they expected after remission.
They have given up so much to keep their sister safe after giving up so much during her active treatment. It has brought many PTSD triggers up for all of us. (mother of a 13-year-old daughter with ALL)
Parents in the active treatment phase experienced changes in visitor restrictions and time spent together that caused them and their children to feel exhausted and fearful. Families additionally lost connections to a community of other families of children with cancer. Thus, the changes brought by the pandemic compounded the emotional toll of experiencing active treatment alone.
Being a cancer family, especially at the beginning of the COVID was extremely scary. (mother of a 2-year-old son with ALL)
Parents were emotionally overwhelmed by the burden of caring for their child in the hospital while isolated from their partner or extended family due to visitor restrictions.
The hospital’s guidelines that limited one caregiver to a patient room were TERRIBLE for a caregiver’s mental health. (mother of a 3-year-old daughter with AML)
Families remained at home due to public health restrictions and heightened concerns for their immunocompromised child. The prolonged isolation at home was emotionally exhausting for parents and children alike.
My daughter spent most of the first years of her life kind of in isolation due to her cancer diagnosis… She doesn’t really know a different life, but it’s definitely affected her emotionally. (mother of a 4-year-old daughter with Wilm’s tumor)
Positive emotional impact
Only 16 (11%) of emotional impact references were positive. Some parents expressed how their experience caring for their child with cancer prepared the family for the pandemic.
A positive is that we are not a stranger to being isolated, so it’s a little bit easier on us emotionally and mentally because we’ve already lived through it being isolated from cancer and trying to be safe. (mother of an 11-year-old daughter with neuroblastoma)
School changes
There was a total of 70 (11%) references to school changes. Parents referenced remote learning and school closures during COVID-19. For some families, remote learning had a negative impact on their children’s education, behavior, and overall mood. For other families, remote learning made it easier to balance the many challenges brought by the pandemic.
Negative school changes
The majority (n = 56, 80%) of school changes references were negative. Parents experienced difficulty transitioning their children from in-person schooling to remote schooling and discussed how the structure of in-person school was important for their child’s well-being and academic performance.
Distance learning for a child who was already behind due to cancer only made him more behind. (mother of an 8-year-old son with hepatoblastoma)
Positive school changes
Positive references to school changes comprised 20% (n = 14) of the references. Some families found resiliency in the increased flexibility, time spent together, and slower pace of remote schooling.
My son, the cancer survivor, does better on a hybrid school schedule and can get enough rest – fatigue is an issue for him. He is doing really well. (mother of a 15-year-old son with medulloblastoma)
Health-care changes
In addition to the visitor restrictions, health-care changes included fewer activities at the hospital, challenges with appointment scheduling, and routine COVID-19 testing, masking, and gowning. While children were anxious about the additional protective gear, parents reflected hopefully on an increase in positive health practices from the public.
Negative health-care changes
There was a total of 69 (11%) references to health-care changes; 66 (96%) of these were negative. One example is the obstacle to seek medical care during travel restrictions:
We were medically evacuated to Hawaii from Japan for my son to receive treatment. We were stuck there for 5 months because of travel restrictions. (mother of a 3-year-old son with ALL)
Another parent lamented about the lack of services available during hospital stays:
Cancer isn’t fun for anyone, especially children. But to have to go through cancer treatment and COVID? No child life, no interaction with other children going through the same thing, no special surprises, no extra toys during chemo, no MAW. It’s been miserable. (mother of an 8-year-old son with a brain tumor)
Positive health-care changes
There were only 3 (4%) positive references about health-care changes. These parents found gratitude in the new preventative measures of masking, social distancing, and frequent hand washing.
We were already living with some sort of fear of interaction in the ‘normal’ world. I appreciated that people in general were taking more care (washing hands, wearing masks, limiting hospital contact when not needed). (mother of a 7-year-old son with ALL)
Physical health
A small number of references were made (n = 33, 5%) about the effects of the pandemic on physical health. Parents noted changes in the frequency of illness, weight gain or loss, sleep, and activity levels.
Negative physical health
Most references (n = 24, 73%) about physical health were negative. Some families noticed a decline in their children’s health due to decreased activity levels:
My kids are less active than they once were and stay in their rooms a lot. (mother of an 11-year-old daughter with ALL)
Other parents noticed recognizable changes in their child’s weight:
She is now dealing with significant weight loss. (mother of a 9-year-old daughter with a brain tumor)
Positive physical health
A quarter of references to physical health were coded as positive (n = 9, 27%). Parents were relieved that their children got sick less because of social distancing and public health measures. The increased time at home allowed some survivors time to recover from their treatment.
Our cancer survivor child was able to make huge strides in her recovery from treatment effects. She began walking and eating because we had time to focus on it. (mother of an 11-year-old daughter with a brain tumor)
Discussion
Results from this large national sample of parents of children with cancer suggest the effects of the COVID-19 pandemic have been significant and exacerbated by caring for a child with, or recovering from, cancer. Specifically, the needs of an immunocompromised child contributed to increased anxiety and stress among parents and children due to concerns about viral exposure and social isolation. Some increase in anxiety can be attributed to health anxiety and limited knowledge of childhood cancer patients’ specific vulnerability to COVID-19 (Dai et al. Reference Dai, Liu and Liu2020; Hamdy et al. Reference Hamdy, El-Mahallawy and Ebeid2021; Liang et al. Reference Liang, Guan and Chen2020; Wimberly et al. Reference Wimberly, Towry and Caudill2021). Moreover, parents indicated that the lost social support, which mitigated stress before the pandemic, contributed to psychological distress.
As expected, many parents reported how the pandemic led to family changes. In alignment with previous research, many families reported financial hardship because of pandemic-related policies and disruptions (Jenco Reference Jenco2020). The increased stress parents reported from balancing home schooling with other demands such as remote work and financial burden appears to be common among parents during the pandemic (Hiraoka and Tomoda Reference Hiraoka and Tomoda2020; Verlenden et al. Reference Verlenden, Pampati and Rasberry2021). The transition to remote learning contributed further to the difficulties parents experienced. Some children may have been more vulnerable to school changes as many children with cancer are often absent from school and face neurocognitive deficits due to their treatments (Kurtz and Abrams Reference Kurtz and Abrams2010; Levin Newby et al. Reference Levin Newby, Brown and Pawletko2000). Literature specific to families of children with cancer and schooling during the COVID-19 pandemic remains limited.
Parents reported that social isolation made it more difficult for families to cope with the many other changes brought by COVID-19. Pre-pandemic literature has shown families of children with cancer find resiliency through family cohesiveness and social support from their community to make the treatment process more manageable and meaningful (McCubbin et al. Reference McCubbin, Balling and Possin2002). However, the onset of the COVID-19 pandemic disrupted these supports. For many parents, the combination of health-care changes and social isolation presented additional challenges for them and their child with cancer. Parents commonly described how hospital visitor restrictions caused their children to feel isolated. For those with chronic illnesses, unfulfilled social needs may have detrimental effects on treatment outcomes and quality of life (Heller et al. Reference Heller, Rehm and Parsons2021). Limiting visitors to a single parent for inpatient units also contributed to family stress because parents were not able to relieve each other during long periods of inpatient care. The pandemic stripped many parents of children with cancer of their supports both within the hospital and in their community. Without this support, parents expressed caring for a child with cancer during this crisis had an immense emotional impact. Additional emotional impact came from the relived trauma of staying home to protect their child. These reports of this emotional impact and stress reflect other studies that have found significant psychological impact on parents of children with cancer and their families from the pandemic (Darlington et al. Reference Darlington, Morgan and Wagland2020; Guido et al. Reference Guido, Marconi and Peruzzi2021; Wimberly et al. Reference Wimberly, Towry and Caudill2021).
Despite the overwhelming negative sentiment, many families identified positives from the pandemic. A unique benefit to families of children with cancer was the appreciation of widespread masking and social distancing. Additionally, many parents reported that the pandemic provided an opportunity for family bonding. Existing literature supports this as shared leisure time benefits family functioning and families have been shown to be resilient in the face of shared adversity (Hornberger et al. Reference Hornberger, Zabriskie and Freeman2010; Walsh Reference Walsh and Walsh2012). Some children thrived in remote learning, and survivors were able to regain physical strength after cancer treatments. One large study suggests that parents of children with cancer had less stress during the pandemic than before its onset due to their previous experience with similar restrictions (Cakiroglu et al. Reference Cakiroglu, Yeltekin and Fisgin2021). There is some support for this finding in our sample among families that found transitioning to the COVID-19 pandemic changes easier due to their previous experience. Thus, there may be significant variance in impact from the pandemic across samples of parents of children with cancer and further research is needed to better understand relevant risk factors.
Study limitations
Participants in this study were mostly non-Hispanic, White mothers. The lack of racial and ethnic diversity in this sample likely underrepresents the experiences of minoritized populations. Recruitment for this study was isolated to Facebook and, therefore, limited the sample to those with access to Facebook and may have introduced selection bias. The format of this qualitative study was 1 general question about “other effects of COVID-19” after parents completed the CEFIS. Some parents may not have shared experiences that they felt were already addressed in their quantitative responses to the CEFIS. This study could not directly compare the experiences of parents with healthy children with the experiences of parents with children with cancer as participants were only parents of children with cancer. Finally, this is a cross-sectional study during a long and evolving pandemic.
Conclusion and clinical implications
For families of children with cancer, many common pandemic-related challenges were heightened by the existing stress of caring for a child with cancer. Findings suggest health-care providers need to fill the gaps in support that have emerged for families of children with cancer during the pandemic. To bridge the social support gaps, psychosocial providers might connect parents to virtual support groups, particularly for families caring for a child with cancer, and expand existing telehealth services to include virtual visitation options for those without access to video calling on their personal devices. Revisions of in-person visitor restrictions, allowing all parents to accompany their child, may alleviate some stress experienced by families. Further, the pandemic continues to impact health-care access. Given long-term psychological and health-care consequences (e.g., staff shortages, post-traumatic stress, complex grief) of the COVID-19 pandemic (Rashid et al. Reference Rashid, Reeder and Sahu2022), clinicians and hospital administrators must address and anticipate ongoing patient and caregiver psychosocial and treatment needs. Future research can build off these findings by obtaining perspectives from oncology health-care providers. Moreover, future work is needed to examine specific risk factors and long-term psychosocial impacts of COVID-19 on parents of children with cancer.
Acknowledgments
This manuscript was written by M.S.S and C.J.S. M.S.S. and C.J.S. should be considered joint first authors. MAS, TF, CAG, and KB contributed to the study conception and design. Data collection and analysis were performed by M.S.S., M.A.S., and C.J.S. All authors commented on previous versions of the manuscript and approved the final version for publication. The authors gratefully acknowledge the families that participated in this work and shared their experience during the COVID-19 pandemic.
Competing interests
The authors declare none.








