Introduction
Cancer is a group of diseases and a major public health problem worldwide (Siegel et al., Reference Siegel, Miller and Jemal2019). Over the past few decades, advances in treatment protocols have made significant improvements in prognosis for children and adolescents with cancer (Smith et al., Reference Smith, Seibel and Altekruse2010). Drug therapy (chemotherapy), radiation therapy (radiotherapy), immunotherapy, stem cell transplant, and the use of surgical techniques significantly increase life expectancy and treatment rates in childhood cancers (NIH, 2020). Today, the rate of treatability in childhood cancers has increased to 75–80% due to the use of appropriate treatments (SEER, 2012). This increase in survival, combined with the development of increasingly aggressive therapies, has highlighted the importance of supportive care and symptom management for pediatric cancer patients (Tutelman et al., Reference Tutelman, Chambers and Stinson2018).
Pain is the most common and feared symptom associated with cancer affecting all dimensions of life (Collins, Reference Collins2001; Wilson et al., Reference Wilson, Stack and Hester2014). Pain can affect children in many ways, including their emotional, behavioral, and nutritional habits, as well as their interaction with their environment and family (Dinçer et al., Reference Dinçer, Yurtçu and Günel2011). Pediatric oncology patients experience pain due to the disease itself, medical treatments, or invasive medical procedures such as blood collection, intramuscular injection, lumbar puncture, bone marrow aspiration, and biopsy. Pediatric oncology patients report that invasive procedures are the most feared and common pain source in cancer treatment (NICE, 2005; Landier and Tse, Reference Landier and Tse2010; Griffiths et al., Reference Griffiths, Schweitzer and Yates2011; Hickman et al., Reference Hickman, Varadarajan, Weismann, McGrath, Stevens, Walker and Zempsky2014; Bukola and Paula, Reference Bukola and Paula2017). Unfortunately, many invasive procedures are needed for the diagnosis and treatment of the disease. Diagnostic tests and treatment regimens for pediatric cancers include invasive and painful procedures (Bukola and Paula, Reference Bukola and Paula2017). In addition, pain and distress can also occur as the side effects of chemotherapy and other treatments (Anderson and Kunin-Batson, Reference Anderson and Kunin-Batson2009; Hickman et al., Reference Hickman, Varadarajan, Weismann, McGrath, Stevens, Walker and Zempsky2014). The primary cause of treatment-related pain in children is chemotherapy (Zernikow et al., Reference Zernikow, Smale and Michel2006). Most chemotherapy-induced pain is caused by mucositis, mucosal damage, infection, peripheral neuropathy, gastritis, and other side effects (Zernikow et al., Reference Zernikow, Meyerhoff and Michel2005; Madi and Clinton, Reference Madi and Clinton2018). Pain also is a side effect of pediatric chemotherapy protocols that include platinum compounds (e.g., cisplatin) and vinca alkaloids (e.g., vincristine) (Vondracek et al., Reference Vondracek, Oslejskova and Kepak2009; Gilchrist, Reference Gilchrist2012). During the treatment of cancer patients, chemotherapy and other drugs are mostly administered in the form of intravenous (IV) infusion (ACS, 2019).
Studies have shown that unmanaged pain in children with cancer has many negative consequences; tThese include declines in quality of life (Calissendorff-Selder and Ljungman, Reference Calissendorff-Selder and Ljungman2006), difficulty with sleep (Walter et al., Reference Walter, Nixon and Davey2015), increased pain sensitivity (Weisman et al., Reference Weisman, Bernstein and Schechter1998), and procedural distress (Katz et al., Reference Katz, Kellerman and Siegel1980). Therefore, it is very important to identify the location and nature of the pain in children, to make continuous assessments, and to apply necessary and relevant interventions and procedures (Dincer et al., Reference Dinçer, Yurtçu and Günel2011).
Pharmacological, non-pharmacological methods or both can be used in the management of cancer-related pain (Gatlin and Schulmeister, Reference Gatlin and Schulmeister2007; Bao et al., Reference Bao, Kon and Yang2014). A multi-modal approach that combines non-pharmacological pharmacological techniques is required to maximize analgesic efficacy and procedural tolerance while minimizing side effects and psychological squeal (Wilson-Smith, Reference Wilson-Smith2011). Distraction is one of the non-pharmacological methods used often to reduce pain. In this technique, setting a stimulus as the focus of attention decreases the person's interest in other stimuli (Uman et al., Reference Uman, Chambers and McGrath2006; Mollahosseini et al., Reference Mollahosseini, Sahbaee and Ebrahimi2007). There are two types of distraction techniques: active and passive. The active distraction method involves encouraging children to engage in an action while undergoing a painful procedure (Srouji et al., Reference Srouji, Ratnapalan and Schneeweiss2010; Koller and Goldman, Reference Koller and Goldman2012; Wohlheiter and Dahlquist, Reference Wohlheiter and Dahlquist2013). The forms of active distraction commonly used in clinical practice are interactive toys, electronic games, controlled breathing, virtual reality (VR), and guided imagery/relaxation (Algren and Algren, Reference Algren, Algren, Tobias and Deshpande2005; Çetingül and Conk, Reference Çetingül and Conk2005; Koller and Goldman, Reference Koller and Goldman2012). In a randomized controlled study by Inal and Kelleci (Reference Inal and Kelleci2012), distraction cards were used during the blood draw process in children aged 6–12, and it was found that they were successful in reducing procedural pain and anxiety. Indovina et al. found that VR has proven to be effective in reducing procedural pain, as almost invariably observed even in patients subjected to extremely painful procedures, such as patients with burn injuries undergoing wound care and physical therapy. Moreover, VR seemed to decrease cancer-related symptoms in different settings, including during chemotherapy (Indovina et al., Reference Indovina, Barone and Gallo2018). Dahlquist et al. (Reference Dahlquist, McKenna and Jones2007) showed that active distraction (i.e., playing a video game) was more effective than passive distraction (i.e., watching pre-recorded footage generated by someone else playing the same video game). Shahid et al. (Reference Shahid, Benedict and Mishra2015) found that distraction by using an iPad during immunizations reduces the parent's perception of their child's pain and distress. Canbulat et al. (Reference Canbulat, Inal and Sönmezer2014) compared attention distraction cards with kaleidoscope and found that distraction cards were more effective in reducing procedural pain and anxiety during the blood drawing process in children aged 7–12 years. Şahiner and Bal separated 120 children between the ages of 6–12 into four groups, and while the control group was applied only the routine blood drawing procedure, distraction cards, blowing balloons, and listening to cartoon music were applied to the study groups. As a result, it was found that the pain and anxiety scores of those who were applied distraction cards were significantly lower than the control group. All other distraction techniques (balloon blowing and listening to cartoon music) were also found to be effective in the management of procedural pain and anxiety (Sahiner and Bal, Reference Sahiner and Bal2016). Mikaeili et al., found that watching cartoons and making bubbles help to reduce the pain that felt by children during chemotherapy. They also found that the method of making bubbles instead of watching cartoons helped reduce pain in children during chemotherapy (Mikaeili et al., Reference Mikaeili, Fathi and Kanani2019). It is best to choose toys that have light and robust features and offer interaction opportunities to distract the child's attention from the painful event (e.g., blowing bubbles) (Short et al., Reference Short, Pace and Birnbaum2017). Mutlu and Balcı determined that children in the intervention groups (cough trick and balloon inflation) had significantly lower pain scores during the drawing of venous blood samples than children in the control group. They also found that the pain score of children in the balloon group fell from 4.55 before the procedure to 1.68 during the procedure (Mutlu and Balcı, Reference Mutlu and Balcı2015). Besides, interactive toys, one of the distracting techniques, activate the audio-visual, kinaesthetic, and tactile senses thereby requiring the child to use cognitive, motor, and visual skills. To be played successfully, toys require an adequate amount of attention, encouraging the child to engage in the game and be less aware of their surroundings (Nilsson et al., Reference Nilsson, Enskär and Hallqvist2013; Green et al., Reference Green, Cadogan and Harcourt2018). When distraction techniques are used, parents perceive less pain and distress in their children, which can contribute to a greater sense of satisfaction from the hospital experience (Sinha et al., Reference Sinha, Christopher and Fenn2006).
Play, a non-pharmacological pain relief method used in children, is the most important part of childhood. Disease stress and hospital environment increase the value of play (Haiat et al., Reference Haiat, Bar-Mor and Shochat2003; Emiroğlu and Akay, Reference Emiroğlu and Akay2008). Hospitals have limited play programs. The fact that children play with toys suitable for their age and developmental period increases their power to cope with stress. Toys for children older than three can be made of all kinds of materials, including plastic, wood, cardboard, and so on. Sometimes medical materials such as empty pillboxes, cotton, and gloves can be much more effective and useful than other items sold in stores, as they promote children's creativity (Oktay, Reference Oktay2002). The child learns to control many emotional reactions, such as fear, pity, anxiety, fear, friendship, gladness, loving, confidence, and these reactions through play (Bekmezci and Özkan, Reference Bekmezci and Özkan2015). Medical materials used during cancer treatment can create fear in children as they cause pain. Making toys and playing games from these materials are thought to be effective in reducing fears by gaining familiarity in children, distracting attention, and increasing the sense of control. This research has been planned considering that making toys using medical materials can be effective in reducing the pain felt during IV treatment by distracting and increasing the sense of control in children. This research has been planned considering that making toys using medical materials can be effective in reducing the pain felt during IV treatment by distracting in children. Distraction is an effective method of reducing procedural pain and can be easily used in children. It is applicable by games and without the need for special education and with little facilities for children according to their age and interest (Kaheni et al., Reference Kaheni, Sadegh Rezai and Bagheri-Nesami2016). In addition, distraction has been shown to be a cost-effective method of addressing pain management and encouraging cooperation in children (Short et al., Reference Short, Pace and Birnbaum2017). In this study, access to medical materials is easy in the hospital environment where the child is located. The cost of these materials is not a great burden on the patient or institution. In practice, it is possible to be provided by the institution without reflecting the cost to the family and without imposing any burden on the institution. Also, since making toys from medical materials is very easy and does not take much time, nurses can easily use these toys in the care of children with cancer and during painful procedures. The use of medical materials commonly used in patient care by turning them into toys may reduce children's fears about these materials. It is thought that by reducing children's fears, it may be effective in reducing phobias related to painful procedures that may develop in the future.
Nurses who provide care for children with pain should know how they perceive the pain, their physical and psychological reactions to the pain, and how to assess the pain. They should also know pharmacological and non-pharmacological methods and necessary nursing practices for controlling the pain (Elçigil, Reference Elçigil2011; Elçigil and Tuna, Reference Elçigil and Tuna2011).
This research aims to examine the effect of playing games with toys made of medical materials in children with cancer on pain that occurs during IV treatment. The researcher worked with the child and family member to make the toys and asked the children to do simple operations such as painting and cutting. This, in turn, may have been effective in reducing the pain associated with painful procedures by distracting children and improving their creativity. The involvement of a family member in play activities may have increased the feeling that the child is safe. It is believed that familiarity with materials such as gloves, injectors, and cotton, which are commonly used during painful procedures in children, may also have been effective in reducing pain by reducing fears about these materials.
Research Hypothesis: The experience of playing with toys made from medical materials during invasive treatments reduces the pain in children with cancer.
Materials and methods
Design
This study was conducted as a randomized controlled clinical trial model.
Setting and sample
The population of the study consisted of children with cancer between the ages of 3 and 6 who were hospitalized at the Turgut Ozal Medical Centre pediatric oncology/hematology clinic in 2016. The number of pediatric patients in the clinic was 1,387. The study included children between 3 and 6 years of age who were diagnosed with one of the cancers listed in the International Classification of Childhood Cancer (ICCC).
The sample size was determined to be 110 children with cancer by conducting power analysis. Power analysis was performed based on the independent sample t test. The power analysis was based on an alpha of 0.05 error level, power of 0.95, and assumed effect size of 0.7 for the sample size estimation. It was aimed to determine a 0.7 level difference between the experiment and the control group as a standard in terms of the pain level of the initiative. Namely, the effect size was taken as 0.7, considering that the expected mean difference between the experimental and control groups of the applied intervention would be at a medium level. In the calculation made after the research, the effect size was found to be 0.47. In fact, the effect size was determined as the difference between the medium level groups after the research. The children were randomly assigned to experimental and control groups. For this, the simple random sampling method from probabilistic sampling methods was used. The patients were listed for the simple random sampling method and selected by using the random number table. In this study, a single blinding method was used.
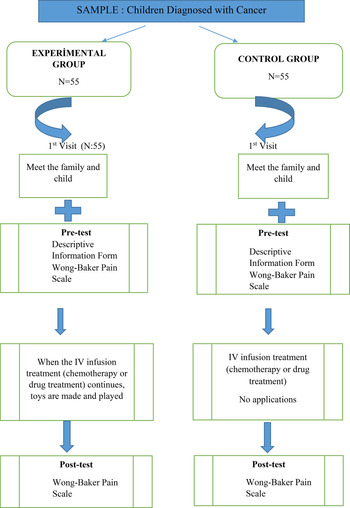
So, 55 children with cancer were selected in the experimental group, and 55 children with cancer were selected in the control group (Figure 1).
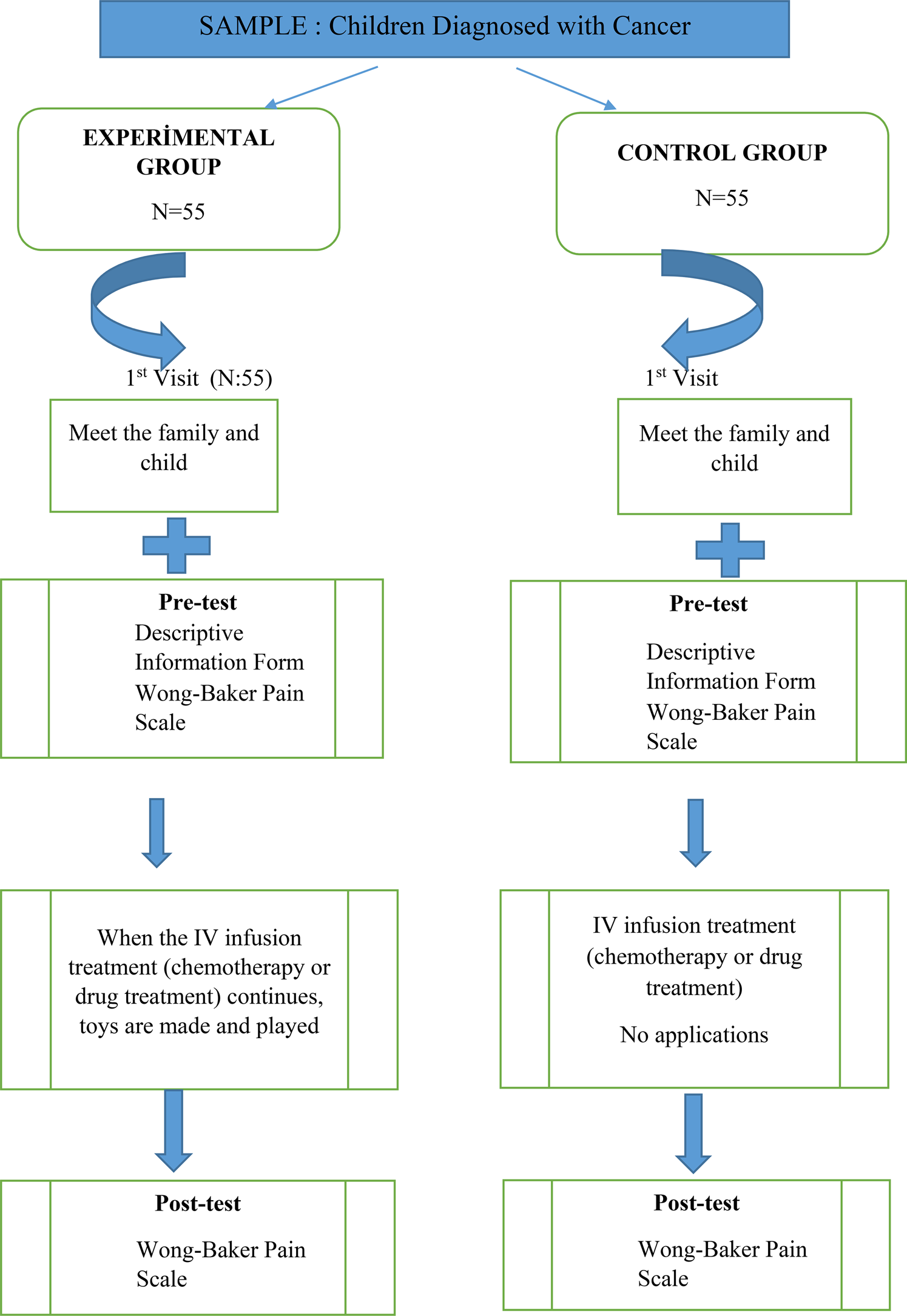
Fig. 1. Research implementation plan.
The inclusion criteria of the study; being diagnosed with cancer, getting IV treatment, being open to communication and cooperation, and being voluntary to participate in the study.
Data collection tools
The data were collected using the descriptive information form and the Wong–Baker FACES Pain Rating Scale (WBS).
Descriptive information form
This form, created by the researcher, consists of a total of 10 questions about socio-demographic characteristics of the patients who received cancer treatment. These questions including such as age, gender, mother education level, father education level, diagnosis, treatment duration, number of hospitalization, previous surgical operations, type of catheter used during IV intervention, and used medications (chemotherapy and antibiotics).
Wong–Baker FACES Pain Rating Scale
This scale was developed by Wong and Baker (Reference Wong and Baker1988) and is a practical and valid measurement tool for evaluating cancer-related pain. Children's pain levels are assessed by numbering facial expressions as follows: 0 = No Pain, 5 = Worst Possible Pain. During this type of scoring, the facial expression changes as the number value increases; this indicates an increase in the level of pain (Wong and Baker, Reference Wong and Baker1988). This scale was adapted by Tüfekçi and Erci (Reference Tüfekçi and Erci2007) by drawing the same type of hairstyles on the original scale so that both girls and boys can perceive it better. In this study, the adapted scale was used by the researchers by coloring. In order to evaluate the comprehensibility of the scale, opinions of five experts in the field of pediatrics nursing were obtained. Based on expert opinions, it was determined that the scale was suitable for use. In addition, the scale was applied to 10 children who were not included in the study before starting the study and it was determined that it was understandable.
Data collection
The data of the study were collected between May 2016 and November 2017 by visiting the hematology/oncology clinic. The data were collected by the researcher with the face-to-face interview technique. Information about diagnosis and treatment was taken in children files. The children were shown the WBS and asked to select one of the face shapes expressing their pain score.
The pain scores of the children in the experimental group were measured before IV drug infusion was administered. The pain score of the child who continued to play with toys was measured again using the WBS, and the post-test data were collected. Children's pain scores were measured twice, during a patient visit before the drug infusion (pre-test data) and during the drug infusion (post-test data). The pain scores of children in the control group were measured before the IV drug infusion (pre-test data) and during the drug infusion (post-test data), using the WBS.
Interventions
The toys were made by the researcher together with the children in the pediatric oncology clinic. The researcher went to the clinic before the treatment time. The researcher met the children and their families, explained the procedures to be done to the families, and created an atmosphere of trust. The researcher and the children of the experimental group began to make toys during the IV drug infusion (chemotherapy or other drugs) was started. Toys were made of non-sterile glove, tongue depressor, cotton, injector, drug covers or boxes, and plasters. Each toy was made in about 5–10 min. Children painted, cut, and colored the medical materials while making the toys. The researcher and children made toys and played with these toys, and these toys were given to them. The researcher and the patient child made toys using real medical materials and played with these toys (about 30–45 min) during the IV infusion. Parents accompanied their children, while they were playing games. No intervention was applied to children in the control group. Children in the control group can play games with standard toys. The researchers were being in the patient's room during the treatment of children in the control group.
Made toys below following;
-
Making a chicken and a rabbit using cotton and non-sterile glove during the invasive procedure. Making a chicken; the researcher inflated a non-sterile glove. She cut molds for the chicken's beak, eyes, wings, and feet, using colored paper. The children painted the chicken's wings using the colors of their choosing. The researcher and children glued the chicken's beak, eyes, and wings. Making a rabbit; the researcher inflated a non-sterile glove. She cut molds for the rabbit's eyes, nose, feet, and teeth, using colored papers, and children painted molds, and then glued them to the glove. She made a tail for the rabbit using a pinch of cotton (Figure 2).
-
Making a toy airplane using an injector, tongue depressor, and plaster during the invasive procedure. The researcher removed the injector from its sheath. She taped the injector needle to the injector using plaster in order to prevent the tip from causing injury. Two tongue presses were used to make the wings of the plane. She taped two tongue depressors to the top and bottom of the injector using plaster. Then, children colored and painted the wings and body of the airplane (Figure 3).
-
Making a traffic light using tongue depressors. The researcher cut circular molds using colored paper, and the children colored these molds using red, yellow, and green colors. These molds were glued on the tongue depressor.

Fig. 2. Making a chicken and rabbit.

Fig. 3. Making an airplane.
Variables of the study
Dependent variables: pain during IV treatment.
Independent variables: playing games with toys made with medical materials.
Control variables: age, mother education level, father education level, diagnosis, treatment duration, type of catheter used in treatment, type of medicine used in treatment, surgical operation, and hospitalization duration.
Statistical analyses
The data were statistically analyzed using the SPSS 22 (Statistical Package for Social Science) package program. Percentage, mean, and standard deviation were used to evaluate the descriptive characteristics of the patients, and the Chi-square test was used for the comparison of control variables in the experimental and control groups. In addition, the independent samples t test and paired t test were used.
Ethical considerations
Ethical approval for conducting the study was obtained from Inonu University Medical Sciences Scientific Research and Publication Ethics Committee (2016/10-10) in Malatya, Turkey. Written institutional permission for carrying out the study in the pediatric oncology clinic was received from at Inonu University Turgut Ozal Medical Centre, in Malatya, in Turkey. In this context, informed consent was obtained from the children's families. Verbal and written consent was obtained from the families in order to use the children's photos, with their faces covered, in the study.
Results
The comparison of descriptive characteristics and control variables of patients in the experimental and control groups is presented in Table 1. The experimental and control groups were similar in terms of the control variables. Of the children in the experimental group, 32.7% were 5 years old, 56.4% were girls, 40% had primary school graduate mothers, and 29.1% had primary school graduate fathers. On the other hand, of the children in the control group, 27.3% were 5 years old, 43.6% were girls, 50.9% had primary school graduate mothers, and 41.8% had high school graduate fathers. In addition, the descriptive information of the children is given in Table 1.
Table 1. Comparison of descriptive characteristics and control variables of patients in experimental and control groups
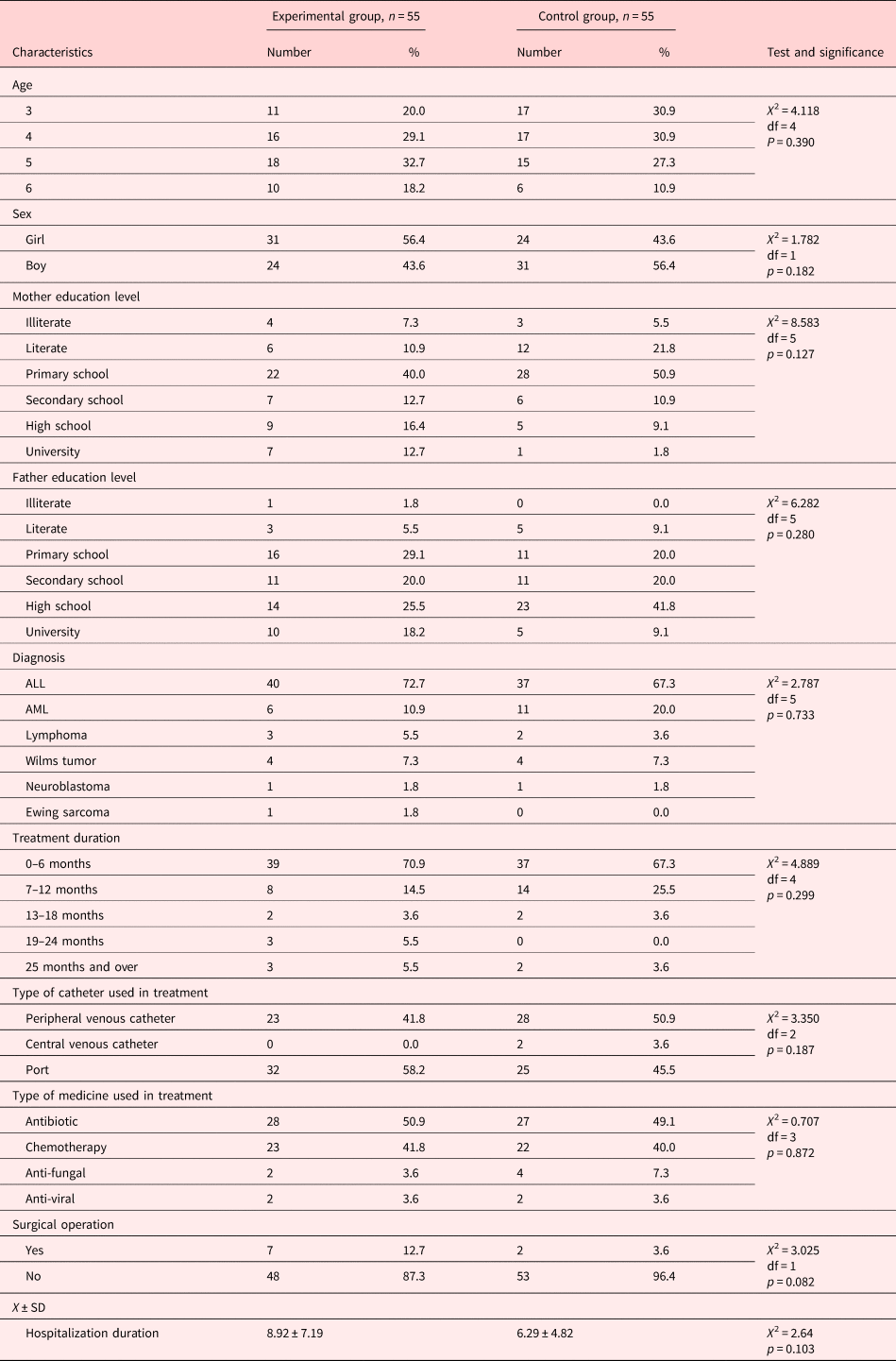
The comparison of pre- and post-test pain mean scores of patients in the experimental group is presented in Table 2. The pre- and post-test pain mean scores of patients in the experimental group were 2.27 ± 0.91 and 0.43 ± 0.66, respectively. The post-test pain mean score of the patients in the experimental group decreased dramatically, and a statistically significant difference was found between their pre- and post-test pain mean scores (p = 0.0001).
Table 2. Pre- and post-test pain mean scores of patients in the experimental and control group (n = 55)
The comparison of pre- and post-test pain mean scores of patients in the control group is presented in Table 3. The pre- and post-test pain mean scores of patients in the control group were 1.72 ± 0.82 and 3.34 ± 0.77, respectively. The post-test pain mean score of the patients in the control group increased dramatically, and a statistically significant difference was found between their pre- and post-test pain mean scores (p = 0.0001) (Table 2).
Table 3. Comparison of the experimental and control group pre and post-test mean scores WBS between groups
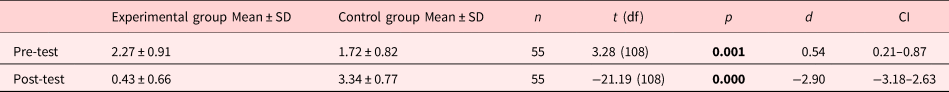
t, independent samples t test; p, significance level; CI, confidence interval. Significance level shown as bold.
The comparison of the experimental and control group pre- and post-test mean scores WBS between groups is presented in Table 3. This result indicates a statistically significant difference between the pre-test pain mean scores of children in the experiment and control groups (p = 0.001). In addition, a statistically significant difference was found between the post-test pain mean scores of children in the experimental and control groups (p = 0.0001) (Table 3).
Discussion
This study examined the effects of play on interventional pain in children, and the results obtained were discussed using relevant studies in the literature.
Cancer, which is considered a lethal disease by pediatric oncology patients and their families, and its treatment are important sources of pain. Studies report that procedural pain is very common in children (Boström, Reference Boström2004; Czarnecki et al., Reference Czarnecki, Turner and Collins2011; Griffiths et al., Reference Griffiths, Schweitzer and Yates2011). The present study, which was conducted to relieve invasive procedural pain in children, determined that children in both experimental and control groups had high pain scores before the IV infusion. Studies report that children experience stress, anxiety, and fear due to the pain felt during routine medical procedures such as blood collection and injection (Cassidy et al., Reference Cassidy, Reid and McGrath2002; Razzaq, Reference Razzaq2006). Rawe et al. (Reference Rawe, Trame and Moddeman2009) suggest that the level of anxiety and treatment pain may be affected by the type of medical procedure.
Nursing studies on the relief of procedural pain and the use of non-pharmacological treatment methods in children have become increasingly prevalent in recent years. Non-pharmacological treatment methods can be used alone in pain control or together with pharmacological treatment methods. An effective use of non-pharmacological treatment methods can be effective in relieving procedural pain. This study found that the post-test pain mean score of children in the experimental group was significantly lower than their pre-test pain mean score. This result suggests that play was effective in pain management because the invasive procedural pain of children in the experimental group had decreased. This result supports the hypothesis of “the experience of playing with toys made from medical materials used for invasive treatments relieves the procedural pain in children with cancer.”
This study's results are in parallel with the literature. Tsai et al. (Reference Tsai, Tsai and Yen2013) examined the effects of play therapy on fear of radiotherapy intervention in children with brain tumors. A total of 19 children were enrolled in the study, aged between 3 and 15 years old, 10 in the experimental group and 9 in the control group. The play therapy enabled the children to cooperate more in the treatment process by reducing their fear and to develop a doctor–patient relationship (Tsai et al., Reference Tsai, Tsai and Yen2013). Another work found that the video games played during chemotherapy reduced the frequency of nausea and vomiting in children with cancer, lowered their systolic blood pressure, and decreased their need for analgesia during and after the treatment (Griffiths, Reference Griffiths2005). Bukola and Paula (Reference Bukola and Paula2017) examined the efficacy of diversion therapy in relieving procedural pain of pediatric oncology patients and found that diversion therapy was effective in relieving the pain. The literature review shows that many non-pharmacological methods can be reliably used to relieve the pain occurring during painful medical procedures (Nguyen et al. Reference Nguyen, Nilsson and Hellstrom2010; Inal and Kelleci, Reference Inal and Kelleci2012; Uman et al., Reference Uman, Birnie and Noel2013; Canbulat et al., Reference Canbulat, Inal and Sönmezer2014; Mohammadi et al., Reference Mohammadi, Mehraban and Damavandi2017).
The post-test pain mean score of children in the control group was found to be significantly higher than their pre-test pain mean score. This result indicates that invasive procedures increase the pain in pediatric oncology patients. Studies report that procedural pain and distress are very important problems for children, caregivers, and health professionals (Duff, Reference Duff2003; Gaskell et al., Reference Gaskell, Binns and Heyhoe2005; McCarthy and Kleiber, Reference McCarthy and Kleiber2006). Blood collection, one of these procedural interventions, is the most feared intervention by children (McCarthy and Kleiber, Reference McCarthy and Kleiber2006). The present study results are consistent with the literature.
Non-pharmacological pain relief methods are very diverse. It is very important for children to play games that are appropriate for the development period for children. Hospitalization prevents children from performing play activities. Nurses who understand the importance of the game in terms of child health should actively use the game during their care. Positive results were obtained in this study, which looked at the effect of reducing the pain of playing games. The effect of nurses not to neglect to play games in cancer patients, and other symptoms related to cancer should also be considered. It is thought that results from the present study can guide nurses in regard to providing care for pediatric cancer patients and can help them determine practical priorities in regard to patient care.
Study limitations
The limitations of this study are as follows: children who migrated to Turkey and had language problems were not included in the study; infected and isolated patients were not included in the study. In this study, a single blinding method was used in the study, as the procedure for playing games with children was performed by the researcher herself. The children did not know that they were in the experimental or control group. The use of single blinding management in research and the collection of data in a single center are other limitations of research. In addition, there are many factors that cause pain in children with cancer. There can be found many factors that cause pain in children with cancer. For example, in this study, there were patients who had bone marrow aspiration, blood drawn, and a vascular pathway opened before treatment. It is understood from the pre-test results that the pain also existed before IV drug treatment. The fact that not all factors other than treatment that cause pain can be isolated is a limitation of the study. Still, the finding that playing games is effective in reducing children's pain is the strength of the study.
Conclusion
The following results were obtained in this study: the experience of playing with toys made from materials used for invasive procedures during the application of invasive procedures relieved IV infusion-related pain of the children. Invasive procedures increased the pain of children.
In line with these results, the following are recommended:
• To use small and simple toys made of the materials commonly used in hospitals and to make children playing with these toys during the application of invasive procedures in order to relieve their pain symptoms.
• To conduct other studies assessing the effects of play therapy, a non-pharmacological method, on symptom management.
• To conduct studies in different regions and to consider cultural differences in this regard.
• To conduct studies including different control variables.
• It is recommended that nurses support these toys so that they can be conveniently used for child patients in each clinic.
Acknowledgments
We thank all of the patients and their families who agreed to participate in the study.
Funding
The author(s) received no financial support for the research of this article.
Conflict of interest
The authors declare that they have no conflict of interests.