Introduction
With the aging of the world’s population, quality of life during the final phase has become a significant issue. Recent studies indicate that people prefer to receive palliative care (PC) rather than superfluous life-prolonging treatments (Chung et al. Reference Chung, Wong and Kiang2017; Scala et al. Reference Scala, Ciarleglio and Maccari2020). Therefore, there is an increasing need for care delivery in end-of-life (EOL) care. This care is part of the PC and includes managing physical support, providing psychological, social, and spiritual support, and ensuring that the wishes of patients and families are fulfilled. Patients can have bad experiences, including a traumatic death, if their EOL care needs are unmet (Spatuzzi et al. Reference Spatuzzi, Giulietti and Ricciuti2017; Van Lancker et al. Reference Van Lancker, Van Hecke and Verhaeghe2018). Families may also experience anxiety when their loved one’s wishes are not followed, or they see them suffer (Ramvi and Ueland Reference Ramvi and Ueland2019).
In most countries, PC services are either under development or must be fully established (WHO Reference Connor and Bermedo2014). Most EOL situations occur in environments not specialized in PC (Sharkey et al. Reference Sharkey, Loring and Cowan2018). Taking care of terminally ill patients and witnessing the entire process of their deterioration require health professionals to be prepared and knowledgeable. The professionals need to realize the importance of valuing their role in providing comfort care. They should be listened to and allowed to express their emotions (Raman et al. Reference Raman, Ebby and Ahmad2022).
Nurses and doctors play a vital role within the team that provides EOL care and are expected to be highly qualified professionals to provide holistic and comprehensive care to patients and families (Spatuzzi et al. Reference Spatuzzi, Giulietti and Ricciuti2017). Practicing EOL care is considered difficult for patients and professionals because it is challenging to develop a passion for care during these troubled times (Liu and Chiang Reference Liu and Chiang2017). Professionals who provide EOL care can be seen as vulnerable or carers of suffering, because sometimes they have negative feelings about death and EOL and gaps in curricular structure hinder preparedness for PC and EOL communication (Corradi et al. Reference Corradi, Duim and Rodrigues2021). On the other hand, cultural aspects can also influence the provision of EOL care by not encouraging professionals to discuss issues associated with death; instead, they are expected to give unrealistic hope to EOL patients (Dong et al. Reference Dong, Zheng and Chen2016).
Thus, identifying factors influencing the preparation and ability to provide EOL care is crucial. The knowledge, training, education (Hussin et al. Reference Hussin, Wong and Chong2018), attitudes, and positive beliefs (Andersson et al. Reference Andersson, Salickiene and Rosengren2016; Oppert et al. Reference Oppert, O’Keeffe and Duong2018) have been explored very timidly, and they are associated with providing effective and high-quality EOL care. Other factors, such as PC experience, enhanced skills, and training (Oppert et al. Reference Oppert, O’Keeffe and Duong2018) emotional and communication skills to deal with patients and their families’ psychological and emotional distress, are necessary for effective EOL care (Hussin et al. Reference Hussin, Wong and Chong2018).
Determining other relationships, PC knowledge, self-efficacy, spirituality, emotional intelligence, and EOL care performance (Rhee Reference Rhee2015), is practically non-existent, or current data are minimal. The self-efficacy theory assumes that increasing knowledge, enhancing attitudes, and modeling appropriate behaviors can facilitate changes in clinician performance. However, it is unclear whether the intervention had a meaningful impact on their expertise in PC or ability to overcome institutional barriers to providing effective EOL care (Azoulay and Siegel Reference Azoulay and Siegel2011). We currently know that to improve self-efficacy in PC improvement in knowledge and facilitation of positive attitudes are needed (Kim et al. Reference Kim, Heo and Yang2023). Preliminary studies (Kang and Choi Reference Kang and Choi2020) indicate that emotional intelligence has a predictive effect and a positive correlation on the perception of PC of future health professionals, and PC knowledge has a positive and direct influence on the ability to provide EOL care (Kim and Hwang Reference Kim and Hwang2014).
To fill the gap in the literature, this investigation analyses the impact of spirituality, emotional intelligence, PC knowledge, and self-efficacy on health professionals’ preparation and ability to provide EOL care. The perception of the structural equation model (SEM) of the relationships among study variables can be essential for defining the factors that inhibit or enhance the preparation and capacity of health professionals in providing care in the last hours or days of life.
Methods
Study design
This study adopted a descriptive cross-sectional research design conducted in a hospital in the north of Portugal in 2022.
Setting and participants
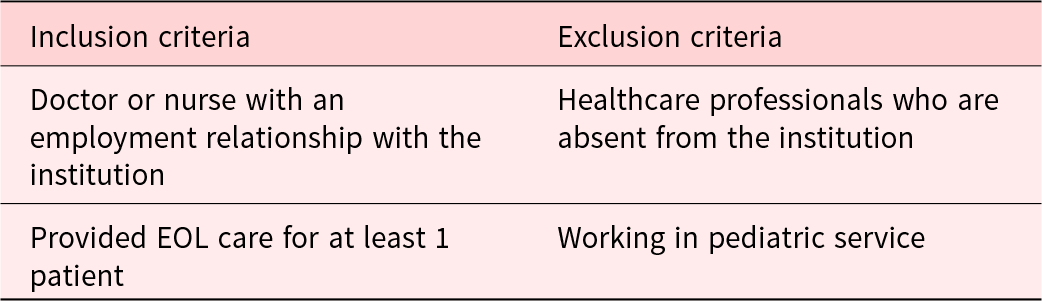
The target population of this study was doctors and nurses working in Portugal, in services likely to have contact with EOL patients (Table 1). We chose to carry out our work in a differentiated hospital in the north of Portugal with a large area of coverage and with a palliative medicine service, constituting this group our universe.
Table 1. Criteria for study participation
Ethical considerations
After obtaining the approval of the ethical committees and the permission to enter the hospital, the researchers invited all eligible nurses and doctors to participate. The researchers explained the study details and the confidentiality and anonymity of the participants. Procedures were adopted to obtain written free and informed consent from participants, prior to data collection.
Data collection
Regarding the data collection instruments, a self-completion questionnaire was carried out and applied between May and July 2022. A total of 710 questionnaires were distributed. The response rate was 55% (391 completed questionnaires), with 380 valid questionnaires.
Measurements
All variables were measured on 5-point Likert scales from the position: 1 – strongly disagree; 2 – partially disagree; 3 – neither agree nor disagree; 4 – partially agree, and 5 – completely agree, except for the spirituality scale whose items were evaluated on a numeric scale from 0 to 10 and PC knowledge scale (dichotomous scale: correct and incorrect). Higher values on the Likert scale correspond to higher indices of the variable.
The spirituality was measured using the Hodge (Reference Hodge2003) scale. This Intrinsic Spirituality Scale comprises 6 items and assesses the degree to which spirituality functions as an individual’s primary motive for both theistic and nontheistic populations, both within and outside religious structures. Participants read an incomplete statement (e.g., “Spirituality is …”) and response options range from 0 to 10, with 0 indicating low levels of spirituality (e.g., “It’s not part of my life”) and 10 indicating high levels of spirituality (e.g., “The main reason for my life, directing all other aspects of my life”). Three statements were put in reverse.
The concept of emotional intelligence was measured based on the Wong and Law Emotional Intelligence Scale (WLEIS) and validated by Rodrigues et al. (Reference Rodrigues, Rebelo and Coelho2011). The WLEIS consists of 16 items and seeks to measure the knowledge that individuals have about their own emotional abilities rather than their actual capabilities. The WLEIS comprises 4 dimensions, with 4 items each: assessment and expression of one’s own emotions; assessing and recognizing emotions in others; regulation of one’s own emotions; and using emotions to facilitate performance.
The self-efficacy and PC knowledge were measured with Bonn Palliative Care Knowledge Test (BPW) adapted and validated for the Portuguese population (Minosso et al. Reference Minosso, Martins and Oliveira2017). This is a 15-item measure of self-efficacy and a 23-item instrument designed to measure knowledge of PC toward providing care for terminally ill persons and their families. It consists of information on the philosophy of PC and physical/psychosocial symptom management.
For the preparation and ability to provide EOL care, we used the Perceptions of Preparedness and Ability to Care for the Dying R-I Scale (Todaro-Franceschi Reference Todaro-Franceschi2013), with 6 items. This consists of 3 items which include communication, symptom management skills, and competence.
Data analysis
The relationships between the variables were evaluated with the SEM technique by the partial least squares (PLS) method using the Smart PLS 3.0 software, while all the other analyses were performed with IBM SPSS Statistics for Windows (V.26).
Results
Sample characterization
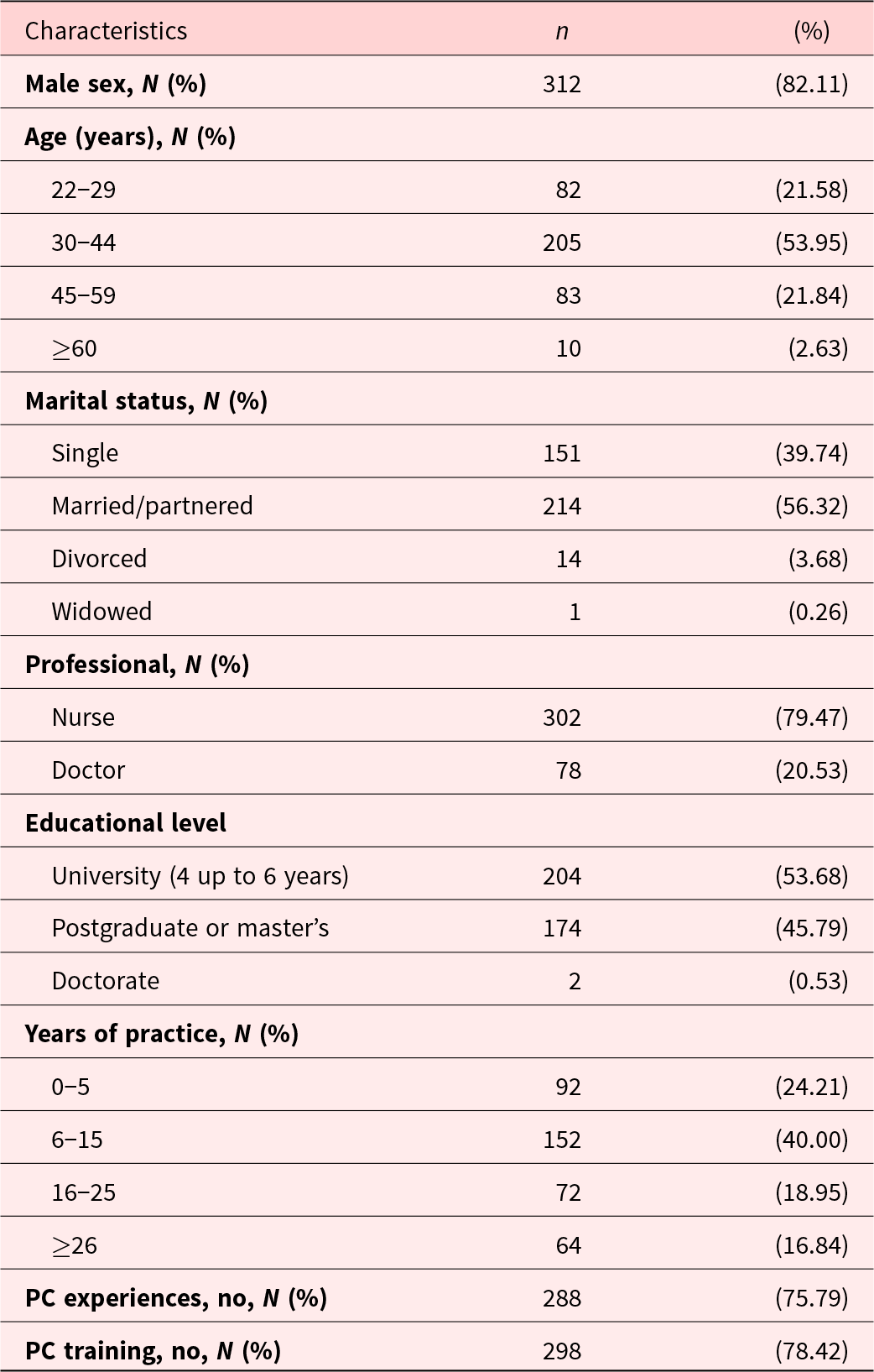
According to Table 2 of the 380 doctors and nurses participating in the study, only 24.21% have work experience in the PC and 21.58% have specific training in this area. The mean age is 37.38 years (±9.93 years).
Table 2. Participant demographics (n = 380)
Level of emotional intelligence, self-efficacy, spirituality, PC knowledge and preparation, and ability to provide EOL care
The mean (SD) scores of emotional intelligence, self-efficacy, spirituality, PC knowledge, and preparation and ability to provide EOL care are represented in Table 3. The dimension “Assessment of own emotions” was the one that most contributed to the average result obtained of 3.88 (±0.83) for emotional intelligence. This average value is higher than the midpoint of the scale (3), showing that the responding professionals have moderate to high levels of emotional intelligence. On the other hand, the dimension with the lowest value was related to “Regulation of emotions” (3.53 ± 0.87). With regard to the self-efficacy variable, the responses obtained indicate an average value of 3.90 ± 0.82, with all items having a percentage value greater than the midpoint of the scale. Taking into account the average values, a high degree of perceived self-efficacy is observed in health professionals. The mean value of spirituality was 5.06, slightly above the midpoint of the scale (5.0). Regarding PC knowledge, the respondents revealed a median level of knowledge (3.29 ± 1.10). Overall, the scale of perception of preparation and ability to provide EOL care had a value of 3.25 ± 0.95, so professionals are moderately prepared and qualified to provide EOL care.
Table 3. Reliability and validity of the constructs
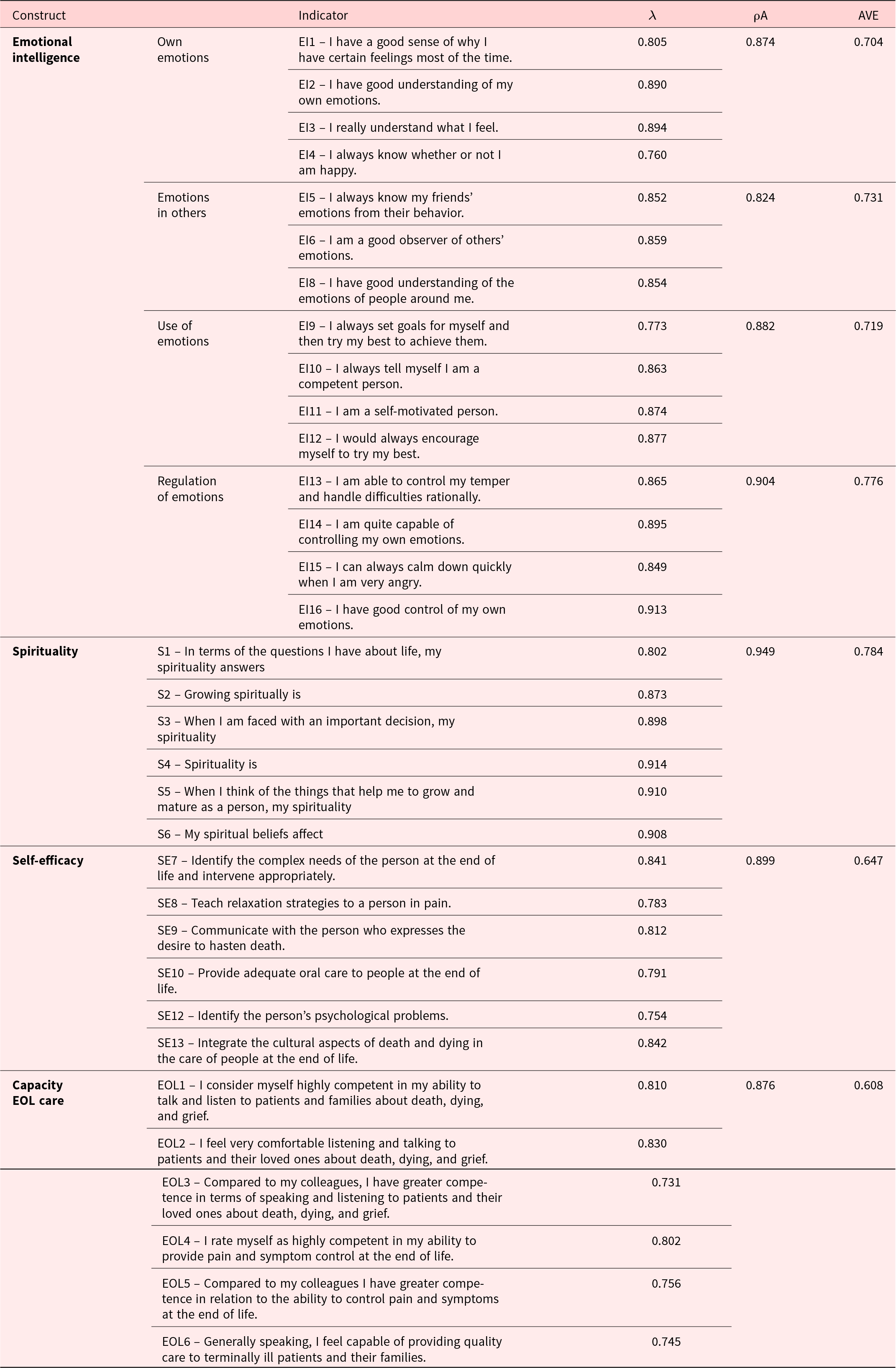
Measurement model assessment
Confirmatory factor analysis was conducted for the measurement model. The assessment of the quality of the measurement model for each construct was done by analyzing the convergent and discriminant validity. In the second step, we estimated the structural model. Therefore, the factor loadings (λ) are then analyzed, and values above 0.708 are recommended (Hair et al. Reference Hair, Risher and Sarstedt2019). After an analysis, some items from the emotional intelligence (item 7) and several items from the self-efficacy scales were eliminated. In accordance to Table 4, all remaining items have factors loading greater than 0.708 (varying between a minimum of 0.731 and a maximum of 0.914). The internal consistency, ρA, greater than 0.7 (Dijkstra and Henseler Reference Dijkstra and Henseler2015) was used. The constructs under study confirm ρA values between 0.822 and 0.949. The metric used for the assessment of convergent validity was the average variance extracted (AVE). All items have a factor loading greater than the square root of 0.5, and the AVE is necessarily greater than 0.5 in all constructs, ensuring convergent validity.
Table 4. Discriminant validity of the constructs

Finally, the discriminant or divergent validity was assessed. Henseler et al. (Reference Henseler, Ringle and Sarstedt2015) propose a value lower than 0.90 in the constructs from the same conceptual domain and lower than 0.85 from different domains. All the heterotrait–monotrait ratio correlation values are less than 0.85 (0.190 between 0.685) (Table 5).
Table 5. Coefficient of determination (R 2) of endogenous variables
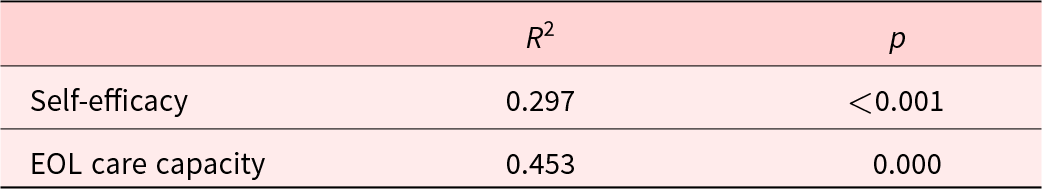
Structural model results
Through the proposal of a conceptual model, it is intended to investigate the influence of spirituality, emotional intelligence, PC knowledge, and self-efficacy on the preparation and ability to provide EOL care by nurses and doctors.
Considering that the evaluation of the measurement model was satisfactory, the next step consists of analyzing the structural model. The standard evaluation criteria for this model include the coefficient of determination (R 2), as well as the statistical significance and relevance of the structural coefficients (β) (Hair et al. Reference Hair, Risher and Sarstedt2019). R 2 measures the variance that is explained in each of the endogenous constructs, ranging from 0 to 1, with higher values indicating greater explanatory power. As a guideline, R 2 values greater than 0.75, 0.50, and 0.25 can be considered substantial, moderate, and weak, respectively (Hair et al. Reference Hair, Risher and Sarstedt2019). Table 6 shows the R 2 values of the endogenous variables, showing that 45.3% of the variance in the perception of the ability to provide EOL care and 29.7% of the variance in self-efficacy are explained by the model.
Table 6. Descriptive statistics among emotional intelligence, self-efficacy, spirituality, PC knowledge, and preparation and ability to provide EOL care (n = 380)

SD = standard deviation.
Figure 1 shows the mediating effect of self-efficacy in the relationship between the variables. Self-efficacy (β = 0.553, p < 0.001), spirituality (β = 0.283, p < 0.001), and PC knowledge (β = 0.171, p < 0.001) positively influence the preparation and ability to provide EOL care. Emotional intelligence in dimension regulating emotions (β = 0.240, p < 0.001) and recognizing the emotions of others (β = 0.263, p < 0.001) and spirituality (β = 0.132, p < 0.001) directly and positively affect self-efficacy.

Figure 1. The mediating effect of self-efficacy on the relationships between spirituality, emotional intelligence, preparation, and ability to provide EOL care.
Discussion
The results obtained indicate a moderate average value of emotional intelligence (3.88 ± 0.83) for the health professionals targeted by the study. Similar results were obtained in recent studies: 3.17 ± 0.56 (Ishii and Horikawa Reference Ishii and Horikawa2019); 4.67 ± 0.78 (Al-Ruzzieh and Ayaad Reference Al-Ruzzieh and Ayaad2021); 3.77 ± 0.47 (Wang et al. Reference Wang, Lin and Chen2022); and 3.33 ± 0.50 (Park and Oh Reference Park and Oh2019). For self-efficacy, the average value was relatively high (3.90 ± 0.82), which is in line with existing values in the literature: 3.71 ± 0.46 (Choi and Yu Reference Choi and Yu2022); 3.38 (Becker‐Haimes et al. Reference Becker‐Haimes, Wislocki and DiDonato2022; Elkhadragy et al. Reference Elkhadragy, Christ and Bashawri2021); and 3.60 ± 0.60 (Van der Voorn et al. Reference Van der Voorn, Camfferman and Seidell2022).
Concerning spirituality, a median value of 5.06 ± 2.30 is pointed and slightly higher in nursing (5.17 ± 2.27). This result does not portray the existing data in the literature that indicate substantially higher values of the spirituality of doctors and nurses, namely: 7.05 ± 2.08 (Caton Reference Caton2021); 7.18 ± 2.40 (Fradelos et al. Reference Fradelos, Alexandropoulou and Kontopoulou2022); and 7.71 ± 1.85 (Atarhim et al. Reference Atarhim, Lee and Copnell2019). To communicate effectively with patients, doctors and nurses need to understand how a person’s spirituality and culture affect their perceptions of health and illness, particularly their desires regarding EOL care. This result reinforces the importance of including themes about spirituality in training programs for physicians and nurses, since training enhances the ability to provide and recognize the importance of spiritual care (Best et al. Reference Best, Butow and Olver2016). The level of PC knowledge obtained in this study was 3.29 ± 1.10, being superior to other studies: 2.34 ± 0.57 (Etafa et al. Reference Etafa, Wakuma and Fetensa2020); 2.23 ± 0.23 (Menekli et al. Reference Menekli, Doğan and Erce2021); and 2.54 ± 0.67 (Tsao et al. Reference Tsao, Slater and Doyle2019). Although in the last 2 decades the role of doctors and nurses has been expanded to the level of PC (Pesut et al. Reference Pesut, Sawatzky and Stajduhar2014), studies carried out with nursing students reveal reduced values of PC knowledge: 1.86 ± 0.73 (Alwawi et al. Reference Alwawi, Abu-Odah and Bayuo2022) and 2.05 ± 0.70 (Dimoula et al. Reference Dimoula, Kotronoulas and Katsaragakis2019). Current studies (Farmani et al. Reference Farmani, Mirhafez and Kavosi2019; Hussin et al. Reference Hussin, Wong and Chong2018; Smets et al. Reference Smets, Pivodic and Piers2018) showed that the absence of curricular content and training in PC, length of professional experience, institution, individual education, and work unit significantly affect knowledge for the practice of PC and/or attitudes. Integrating theoretical and practical training in PC improves students’ knowledge and creates favorable attitudes toward death, dying, and EOL care (Chover-Sierra et al. Reference Chover-Sierra, Martínez-Sabater and Lapeña-Moñux2017; Wang et al. Reference Wang, Li and Zhang2018). Educational intervention is an effective way to improve professionals’ knowledge about PC (Menekli et al. Reference Menekli, Doğan and Erce2021).
Overall, the health professionals in this study are moderately prepared and qualified to provide EOL care (3.25 ± 0.95). These data are in accordance with the literature: 3.20 (Gelfman et al. Reference Gelfman, Morrison and Moreno2021); 3.08 ± 0.55 (Chan et al. Reference Chan, Chun and Man2018); 3.39 (Rodenbach et al. Reference Rodenbach, Kavalieratos and Tamber2020); 3.30 ± 0.98 (Tait and Hodges Reference Tait and Hodges2009); and 2.88 ± 0.78 (Todaro-Franceschi Reference Todaro-Franceschi2013). Health professionals’ preparation for providing EOL care involves understanding their personal beliefs about death and dying; being able to assist the patient and family; combining theoretical knowledge, personal and professional experience and available resources; balancing the dialogue between professional and personal roles; and finding strategies that make sense of the experience of dying, specifically through closure (Hall Reference Hall2020). Offering PC and EOL care is a complex and challenging task for younger professionals and is strongly influenced by cultural, religious, spiritual, and social factors (Oji et al. Reference Oji, Onyeka and Soyannwo2022).
The variable that had the most significant impact on the perception of preparation and ability to provide EOL care was self-efficacy. The higher the EOL care stress of nurses, the higher the death anxiety (Choi et al. Reference Choi, Gu and Oh2022). EOL care education increases perceived self-efficacy (Sabolish et al. Reference Sabolish, Wilson and Caldwell2021), comfort with EOL care and knowledge of coping resources (Lauderbaugh et al. Reference Lauderbaugh, Popien and Doshi2023).
Self-efficacy, spirituality, and PC knowledge positively and directly influence preparation and ability to provide EOL care, and emotional intelligence positively and directly influences self-efficacy. High levels of emotional intelligence have been associated with better performance and competence in providing EOL care; regulating one’s own emotions; decreasing moral distress in EOL care and also in responding appropriately to patient needs and expressing caring and empathy (Lewis Reference Lewis2019). Emotional intelligence affects positively the attitudes toward EOL care, as a basic reference for the development of education programs and EOL care protocols to improve EOL care among health professionals (Park and Oh Reference Park and Oh2019). Professionals with higher self-efficacy provide better safe services and patients in hospitals with a more positive safety culture experience fewer injuries (Rahmani et al. Reference Rahmani, Arjmand and Arabsorkhi2023).
Spirituality is the most unknown aspect of PC despite being the need that is most altered in the last moments of life. Health professionals recognize the importance of spiritual care for patients and give meaning to the actions when it comes to providing EOL care, achieving holistic care, humanizing death, and promoting a dignified end but feel little qualified to do so (García-Navarro et al. Reference García-Navarro, Medina-Ortega and García Navarro2021; O’Brien et al. Reference O’Brien, Kinloch and Groves2019). Preliminary studies found a positive correlation between professionals’ spiritual care skills and the frequency of spiritual care practices (Kurtgöz et al. Reference Kurtgöz, Keten Edis and Erarslan2023). In the literature, 1 study by Espinoza-Venegas et al. (Reference Espinoza-Venegas, Luengo-Machuca and Sanhueza-Alvarado2016) concludes that the perception of religious belief and/or spirituality does not influence the perception of preparation and ability to provide EOL care, but another study by Khraisat et al. (Reference Khraisat, Alkhawaldeh and Abuhammad2019) recognizes that greater preparation of nurses is a factor that facilitates the provision of EOL care for pediatric patients. Given these results, more investigations are needed to infer this relationship.
Spirituality has a positive and direct influence on self-efficacy. This result corroborates recent investigations (Kasapoğlu Reference Kasapoğlu2022; Rakhshanderou et al. Reference Rakhshanderou, Safari-Moradabadi and Ghaffari2021) emphasizing the role of spirituality and spiritual health on self-efficacy and other psychological perceptions. Self-efficacy is associated with spirituality, and these 2 attributes are strong motivators of human development (Adegbola Reference Adegbola2011). The knowledge level of EOL care also explains the variance in EOL care self-efficacy (Hsu and Chen Reference Hsu and Chen2019).
Limitations
A limitation of this investigation is its cross-sectional design, which does not allow for the examination of causal relationships and feedback effects between the variables under study. Since emotional experiences are transient, a 1-time assessment cannot capture personal fluctuations in employees’ daily emotional experiences. Thus, future studies could use a longitudinal design and a day-to-day approach to capture affective experiences at work more accurately. On the other hand, the study was conducted based on a convenience sample based on the perceptions of professionals from a single organization, preventing us from generalizing the results.
To avoid response bias, we previously applied a pre-test and introduced questions in reverse order, ensuring anonymity, and a neutral tone, with sufficient response options (Likert scale) and not revealing too much about the research question.
Conclusion
“Do spirituality and emotional intelligence improve the perception of the ability to provide care at the EOL? In accordance with the correlations and the causal model, found in this study the total effects of the variables, the strongest and most positive effect was self-efficacy, which is conceptually closest to the ability to provide EOL care. This study measured a moderate mean value of perceptions about spirituality, emotional intelligence, PC knowledge, self-efficacy and preparation, and ability to provide EOL care by healthcare professionals. Emotional intelligence and spirituality directly and positively affect self-efficacy. Emotional intelligence has an indirect effect, mediated by self-efficacy on the ability to provide EOL care.
This study helps to identify factors that influence the capacity and ability to provide EOL care. Thus, it provides some evidence that may be useful in creating work environments that improve the staff’s spiritual well-being, emotional intelligence, and self-efficacy toward dying patients and their families. The study suggests that the health educational curriculum may also be enhanced to ensure students are well-prepared to support EOL care and design interventions to address spirituality and emotional intelligence, underscoring the need to include these themes in curricular bases and continuing education programs for PC within healthcare organizations.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951524000257.
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Funding
Center for Transdisciplinary Development Studies (CETRAD) and also supported by national funds, through FCT – Portuguese Foundation for Science and Technology within the scope of the project UIDB/04011/2020.
Competing interests
The authors declared no potential conflicts of interest concerning this article’s research, authorship, and/or publication.










