The few turbulent years that Gio Batta Gori headed the National Cancer Institute’s Diet, Nutrition and Cancer Programme (NCI DNCP) started with high expectations of a new beginning for cancer prevention. After years of neglect, it seemed that the federal agency would take advantage of new opportunities to build on a growing body of epidemiological and experimental work that implicated diet and nutrition as causes of this group of diseases. The programme began in 1974 amid a flurry of new initiatives in cancer prevention and control. However, by 1977 it was in crisis, and in 1978 Gori left under a cloud. The DNCP might have begun with great expectations of a new beginning for cancer prevention, but these expectations were frustrated by the time that Gori left.
The story of the DNCP is often told within the NCI as part of a broader narrative of the difficult birth of federal support for cancer prevention. In this account, the NCI’s interest in cancer control initially focused on early detection and treatment.Footnote 1 Less attention focused on prevention – or, more specifically, what came to be known as ‘primary prevention’Footnote 2 – with the exception from the 1950s of smoking and tobacco. Then, in the late 1960s and 1970s this began to change. Researchers associated a growing number of occupational, environmental and lifestyle factors with cancer, and Congress and advocacy groups pressured a sometimes-reluctant NCI to devote more resources to aetiology and primary prevention (hereafter just ‘prevention’).Footnote 3 Federal support for diet and nutrition emerged with this new interest in prevention.
Prevention is only part of the story of the DNCP, however, and at times not even the main one. Its origins began with the problems of parents trying to feed their leukaemic children, and much of its funding went not on prevention, but on studies of the role of diet and nutrition in cancer therapy. Indeed, the early history of the DNCP is a microcosm of a broader struggle over research priorities in which physicians and scientists aggressively defended therapeutically related research against demands that more resources go to prevention. Such struggles, I suggest, were exacerbated by anxieties from the food and farming industries that the NCI’s interest in diet and nutrition in cancer causation might add to pressure to reduce consumption of their products on health grounds. None of this succeeded in ending prevention-related research, but it did ensure that advocates of prevention were thwarted in their more ambitious expectations of the DNCP, especially as the NCI’s budget began to tighten in the mid-1970s, and the DNCP found itself struggling against bigger, more established programmes, at the heart of NCI policy, and ever hungry for more money. The story of the DNCP is thus a tale of what happened to a marginal programme when funding got scarce, and when entrenched interests came to be threatened.
This paper has three aims. The first is to use the DNCP as a window onto the growth of federal support for research on diet, nutrition and cancer following the 1971 Cancer Act, the legislative beginning of what was sometimes known as the War on Cancer. This programme and the broader field of diet, nutrition and cancer research are largely neglected in the voluminous literature on the 1971 Act and its aftermath.Footnote 4 Nor do the general historiographies of either diet and nutrition or cancer therapeutics and prevention in the 1970s give them much attention.Footnote 5 In the case of cancer therapy, the best we have are a few internal accounts of technical developments in the nutrition of cancer patients and some comments on continued anxieties over diet as a form of ‘quack’ treatment.Footnote 6 In the case of prevention, diet and nutrition are – with two exceptions – largely subordinated to accounts of smoking and occupational and environmental cancers. One exception is a literature on additives and hormones such as diethylstilbestrol (DES) which were not the focus of the DNCP for reasons discussed below.Footnote 7 The other exception is a literature on the growing interest in diet, nutrition and cancer in the 1980s, but this last literature largely skips over the 1970s.Footnote 8 Part of the historiographic intent of this paper is to recover the missing decade of the 1970s: to explain why interest in diet, nutrition and cancer emerged during that decade, to document the range of interest in this field (beyond additives and hormones), to explore how the NCI responded to this interest and to describe why its early efforts foundered. The paper ends in 1978 when the DNCP’s first director left, and prevention and therapy separated within the programme.
The second aim of this paper is to explore the problematic relations between therapeutics and prevention within the DNCP in the 1970s. It is well known that the NCI was widely criticised during that decade for favouring therapeutics over prevention.Footnote 9 Much of the substantial historiography on this topic, however, is written from a prevention perspective in which arguments in favour of therapy tend to be portrayed as little more than barriers to prevention’s advancement. One of the goals of this paper is to recover the perspectives not only of those who advocated prevention, but also of those who advocated therapeutic research, and to show how each related to the other. The DNCP provides a valuable opportunity to explore this intertwined story. Both sides saw the programme as an opportunity to advance their research objectives, but there was never enough money to support all their proposals, and they became competitors for a limited funding pool. Yet, paradoxically, if they were competitors they were also uneasy allies. The DNCP’s marginal status within the NCI meant that the two sides were bound together in a fraught relationship as partners in preserving the programme as a whole against external threats. It was a difficult position for each. Both were forced to weigh their common interests in protecting the programme against their competing interests in securing funding from a small DNCP budget.
A third aim of the paper is to use the DNCP as a window on to the broader politics around diet, nutrition and cancer in the 1970s. The DNCP is a story of how a range of external stakeholders – with different, sometimes conflicting, interests and agendas – sought to shape NCI policy in this area. Thus, where some advocacy groups pressured Congress and the NCI for more funding for prevention, other stakeholders, such as the meat industry, worried that DNCP research might highlight public health issues that would undermine the commercial value of their products. Congress itself was divided, sometimes more willing to privilege the voices of advocates of therapeutics, sometimes those of prevention. And, within the NCI, advocates of prevention and therapeutics played up these divisions to argue political cases for their various positions, often backed up with data that they hoped would support more research in their fields and highlight the limitations of research favoured by their opponents.
This then is a story about how the fate of the programme in the 1970s was determined by the political struggles between various stakeholders, both within and without the NCI. It is also a story of how these struggles were complicated, on the one hand, by broader efforts by the NCI leadership to reform and restructure the organisation in the mid-to-late 1970s and, on the other hand, by Gio Gori, the director of the programme. Gori’s controversial efforts from 1977 to counter the DNCP’s budgetary problems, combined with his simultaneous involvement in disputes around smoking, succeeded in alienating powerful figures within the NCI. The DNCP director found himself in a hostile institutional environment, politically exposed and without allies having lost the support of former patrons during the reorganisation of the mid-to-late 1970s. Gori was eventually compelled to give up directorship of the DNCP, and his political problems helped set the stage for the growing institutional separation of therapeutics and prevention within the programme.
1974–77
The beginnings of the DNCP can be traced to one of the therapeutic ‘success’ stories of the post-war years – childhood cancer.Footnote 10 Where once a diagnosis of leukaemia had meant the death of the child, by the late 1960s and 1970s the situation was very different. Mortality from childhood leukaemia fell, children survived the disease longer and a new set of problems emerged around their long-term care. Among these problems diet and nutrition figured large. Parents found their leukaemic offspring often unable or unwilling to eat, fluctuating from skeletal to obese during the course of treatment, and their physicians often seemed at a loss to help. By the 1970s, a number of parents’ support groups had formed. One of these – the Candlelighters, based in Washington, DCFootnote 11 – was to set in motion the events that led to the creation of the DNCP.
The Candlelighters was the inspiration of Grace Ann Monaco (also known as Grace Powers Monaco), a young attorney in Washington, DC.Footnote 12 In 1968 her daughter, Kathleen Rea, was diagnosed with acute lymphoblastic leukaemia and began treatment at Children’s National Medical Center. There Monaco met parents of other children undergoing treatment, and – encouraged by the paediatrician Sanford Leiken and other physicians and nurses at Children’sFootnote 13 – together they formed a support group for parents of children with cancer. Monaco later recalled: ‘About 25 of us started meeting wherever we could find space – boiler rooms, corridors outside the emergency room – and Candlelighters was born.’Footnote 14 The parents lobbied Congress on issues such as better access to paediatric clinical trials, the establishment of a national comprehensive cancer registry for childhood and adolescent cancers, and outreach programmes for the demonstration of successful methods of treating those cancers.Footnote 15 The organisation also gained a reputation for its support of greater federal involvement in research, and for its ability to present practical suggestions on how this might be achieved in Congress.Footnote 16 One of the founding members, Richard (Dick) Sullivan, was a congressional staffer, which facilitated access to legislators. Sullivan’s daughter had a neuroblastoma and died in 1970, the same year as Kathleen Rea. The Candlelighters’ ‘birth’ – also in 1970 – came out of these personal tragedies.
The Candlelighters expanded beyond the Washington area. ‘Our traveling members really got the ball rolling’, Monaco later noted of members who visited children’s hospitals across the country.Footnote 17 ‘We talked about the importance of parent-peer support and networked with parents across the US and Canada.’ To build and maintain their network, Monaco and Julie Sullivan, Dick’s wife, founded a newsletter in 1970, written with the help of other parents, and printed on the House of Representatives’ mimeograph machine. The number of local Candlelighters groups jumped from perhaps three in the early 1970s to over 100 by the end of the decade, in 42 states, and in Europe and Canada.Footnote 18 By then the organisation had also developed what it called the Childhood Cancer Ombudsman Programme that used panels of volunteer doctors and lawyers to give free opinions on issues such as treatment choices, informed consent, employment discrimination against parents, educational discrimination, access to military service and barriers to insurance. In 1976, the Candlelighters created a Foundation to promote self-help groups, to improve communications between parents and parents’ groups, and to enhance the quality of information available to parents of children with cancer.Footnote 19
The poor quality of information available to parents had been a concern of the Candlelighters long before the establishment of the Foundation.Footnote 20 During debates over extending the 1971 National Cancer Programme, the organisation persuaded the House Sub-Committee on Health and the Environment headed by Paul Rogers (D-Fla) to write into the section of the bill authorising NCI information programmes a statement that such programmes should include ‘information respecting nutrition programs for cancer patients and the relationship between nutrition and cancer’. It was this proposed authorisation that marks the beginning of the Diet, Nutrition and Cancer Programme. At some point in the Congressional deliberations the terms of the authorisation expanded, and under the National Cancer Amendment enacted 23 July 1974 (P.L. 93-352) Congress ordered the NCI to increase its support for research into the role of nutrition in both the cause and treatment of cancer.Footnote 21 By November 1974, the first plans for what would become the DNCP were set out, and the programme was launched the following year.Footnote 22
The Diet, Nutrition and Cancer Programme
The DNCP might have started as an appeal for more nutritional information from parents trying to feed their sick children, but it had turned into much more. In 1974, the director of the NCI, Frank J. Rauscher, appointed an internal committee of NCI scientists – the Diet Nutrition and Cancer Coordinating Group (DNCCG) – to define the goals of this programme and to recommend an organisational structure. The DNCCG interpreted the 1974 Cancer Act as calling for a two-pronged programme in diet and nutrition focused on information provision and research, the latter including studies on cancer aetiology and on the treatment, long-term management and rehabilitation of cancer patients. (Hereafter treatment, management and rehabilitation will be abbreviated to therapy.)Footnote 23 Towards these ends, the DNCP began a literature survey on diet, nutrition and cancer, and organised two workshops in 1975 – one on diet in cancer therapy,Footnote 24 the other on nutrition and cancer causation.Footnote 25 These shifts towards therapy and aetiology seem to have had the approval of the Candlelighters, which remained a strong supporter of the programme throughout the 1970s, pressing the NCI to increase nutrition research.Footnote 26 In 1979, the NCI fulfilled a debt to the Candlelighters by producing a dietary resource book for parents of children with cancer.Footnote 27
Table 1: Gio Batta Gori’s appointments prior to joining NCI. Source: Gio Batta Gori, Resume (June 1968), NCI archives: item number DC-6800-006346.

To get the DNCP going the NCI began by appointing a programme director and an advisory committee. The directorship went to Gio Batta Gori, then deputy director of the NCI’s Division of Cancer Causes and Prevention (DCCP), see Figure 1.Footnote 28 Today, Gori is a controversial figure in part because of his subsequent career as a consultant to the tobacco industry, and critics have questioned his scientific and management credentials. Richard Kluger, for example, describes Gori as a ‘journeyman microbiologist’ whose ‘medical training had been at a backwater school, he had no scholarly publications to speak of, and he brought no depth of knowledge on the nuances of cancer’.Footnote 29 And Devra Davis adds to Kluger’s criticism. ‘What Gori lacked in scientific pedigrees at the time, he more than made up for in schmoozing ability’, she claims, ‘many of his colleagues found him to be an overdressed bureaucrat with an exaggerated sense of his own importance’.Footnote 30 But such evaluations seem to have come in part from critics within the NCI. For others within that organisation, Gori seems to have gained a reputation as an effective administrator.

Figure 1: Gio Batta Gori, c1975. Source: ‘Dr. Gio Gori Becomes Dep. Director of Cancer Cause, Prevention Div.’, The NIH Record, 27, 1 (14 January 1975), 7, courtesy of Rich McManus, editor of The NIH Record.
Born in Tarcento, Italy, Gori had trained in microbiology and botany at the University of Camerino, see Table 1. In 1959/60 he moved to Pittsburgh to work with Jonas Salk on the poliovirus. He returned briefly to Italy to establish a laboratory to produce polio vaccine in Siena, before re-crossing the Atlantic to join Hilary Koprowski, the microbiologist director of the Wistar Institute in Philadelphia. After the Wistar, Gori worked in private industry before joining the NCI in 1968, where he gained a reputation as an efficient manager, someone able to get along with most people. As we shall see, this reputation would be in tatters by the time he left NCI. At least in the beginning, however, it is likely that it was his good managerial reputation, more than his modest scientific accomplishments, that explains why he quickly moved up the administrative ladder. From 1973 to 1980, he was (Acting) Deputy Director of the DCCP, with simultaneous responsibilities as Director of the Smoking and Health Programme (1973–c.78), and Acting (Associate) Director of the Carcinogenesis Programme (1976–77). He was to be Director of the Diet, Nutrition and Cancer Programme from 1975 to c.1978 (Figure 2).Footnote 31
The advisory committee met for the first time on 19–20 August 1975. Chaired by the Massachusetts Institute of Technology (MIT) toxicologist, Gerald Wogan, the committee was eventually named the Diet, Nutrition and Cancer Advisory Committee – hereafter the DNCAC or the Advisory Committee (Table 2). According to Gori, the DNCAC was intended to reflect a cross section of scientific expertise in epidemiology, experimental carcinogenesis, animal nutrition, human clinical nutrition, the biochemistry of nutrition and clinical oncology, as well as the federal government, the academic community, industry, the American Cancer Society (ACS) and other interests.Footnote 32 Yet from the start there were tensions within it. In part, the issue was the division of power between Gori (as Director of the programme) and the Committee that advised him. The substantive problem, however, was how to divide the US$5000 000 (later US$6000 000) allotted to the programme between research on therapeutics and aetiology. To the dismay of advocates of therapeutics, Gori submitted a plan in which research on aetiology and therapy would each have 45% of the budget of the new programme – the remaining 10% going on general support.Footnote 33 (Table 3) It was this plan that marks the beginning of the struggle over research priorities within DNCP, pitting advocates of therapeutically related research against those who promoted prevention and aetiology.
Table 2: Members of the Diet, Nutrition and Cancer Programme Advisory Committee.

Table 3: Gori’s proposed breakdown of the budget for DNCP, August 1975 (% ![]() percentage of the total DNCP budget). Source: ‘Nutrition Program Starts to Zero in on Mass of Data, Plan Contract and Grant Project Areas’, The Cancer Letter, 1, 35 (29 August 1975), 1–6: 2–3.
percentage of the total DNCP budget). Source: ‘Nutrition Program Starts to Zero in on Mass of Data, Plan Contract and Grant Project Areas’, The Cancer Letter, 1, 35 (29 August 1975), 1–6: 2–3.

Diet and Therapy
Advocates of therapy argued there were pressing clinical reasons why they needed more resources than Gori proposed. They pointed out that the disease itself could cause malnutrition (through anorexia, hormonal disturbances or by other unknown mechanisms); that the resulting nutritional deficiencies could enhance or retard tumour growth directly, or through their effects on the immune system, or on drug absorption and metabolism; that the frequent presence of acute infection created further nutritional complications by increasing the basic metabolic expenditure by 30–40%; and that nutritional problems could also be caused or aggravated by cancer treatment, sometimes the result of the anorexia, nausea, vomiting and diarrhoea which could follow chemotherapy or radiotherapy, and sometimes the result of depletion by antimetabolite therapy (see Table 4).Footnote 34 However, despite numerous reports indicating that dietary factors might play a critical role in cancer treatment, commentators noted that there were few definitive studies on the contribution of diet to the clinical management of cancer. The complexity of the relationships among tumour, host and diet/nutrition made reproducible results difficult to obtain.Footnote 35
Table 4: Consequences of cancer treatment predisposing to nutrition problems. Source: Maurice E. Shils, ‘Nutritional Problems Arising from the Treatment of Cancer’, CA. A Cancer Journal for Clinicians, 20 (1970), 188–96: 193.

For many physicians, research into the role of diet and nutrition in cancer had particular urgency because of the anorexia and cachexia associated with the disease. Anorexia was a frequent problem in the treatment of cancer. It could persist for such a long time that the patient lost a huge amount of body weight, became malnourished and was less able to counteract the complicating factors of cancer, or to endure aggressive anti-cancer therapies such as radiation, surgery or chemotherapy. According to one estimate, about two-thirds of those who died of cancer were cachectic at death.Footnote 36 In some cases, the anorexia and cachexia seemed to be the result of reduced food intake, either because patients with cancer found it painful to eat or because they found their food to be much less palatable – the disease or its treatments sometimes seemed to affect taste and smell. In other cases, the anorexia or cachexia seemed to have little to do with food intake. Some patients continued to lose weight even when they ate and appeared to assimilate a normal diet, perhaps because the tumour pre-empted available nutrients, or because the host underwent an increased metabolic rate – scientists disagreed on the reason. In addition, some studies showed that food restriction generally inhibited tumour growth, lending support to suggestions that the cachexia might be an adaptive device of the host to starve the tumour. It was, therefore, possible that improving patient food intake would actually accelerate the growth of the tumour, and improve its viability and resistance to therapy.
For the DNCAC, such concerns opened a series of possible research projects, including studies of the nature of host–tumour competition, the causes of impaired food intake, the role of individual nutrients as they related to cancer treatment (including nutrient depletion by therapy) and the activities of enzymes involved in the metabolism of cancer chemotherapeutic agents. The Advisory Committee considered studies on why modified taste perception occurred, and discussed proposals for research to develop means for restoring normal taste patterns, to modify traditional tastes of foods so that they became palatable again and to change patient’s behaviours so that they increased food intake.Footnote 37 It also considered research into artificial methods of feeding (for those cases where conventional feeding was impossible) to improve the formulation of nutrient solutions, to reduce costs, to improve hardware, to reduce the chance of sepsis and to devise low-cost, mass-produced portable infusion units for ambulatory patients. The latter research was of particular interest to two members of the DNCAC, Jonathan Rhoads and Stanley Dudrick. In 1968, they had developed a technique of total parenteral nutrition (TNP) that became a standard American technique for providing patients with long-term nutritional support.Footnote 38
A final problem focused on the question of whether nutrition could be used as a direct form of cancer therapy. The recognition that the nutritional requirements of many tumours were quite different to those of the host – the patient – opened the prospect of adjusting available nutrients so as to starve the tumour while feeding the patient.Footnote 39 In addition, it was also possible that therapy might be based on the interruption of the cachexia, rather than the inhibition of the tumour, especially in the early stages of tumour growth before frank emaciation set in.Footnote 40
So far I have suggested that calls for research into the relations between diet, nutrition and cancer therapy were motivated, in part, by a series of clinical and scientific questions related to the practical problems of cancer therapy. These technical questions were given political urgency by growing public concern in the 1960s and 1970s of poor survival rates for patients undergoing therapy.Footnote 41 Despite years of research and millions of dollars, critics argued that survival rates had not significantly improved since the Second World War. For physicians these figures were confirmation of the need for more research into methods of improving cancer therapy, but they also raised a new quandary. Increasingly such figures were also used to argue that cancer research was too focused on therapeutics and basic laboratory studies, and that a fundamental reorientation towards prevention was needed. For therapists, all this gave new importance to research that promised practical methods of improving survival rates. Studies of artificial nutrition, direct nutritional therapy, and the role of diet and nutrition in the host/tumour relationship were particularly promising here, they claimed.
Yet, until the creation of the DNCP, the NCI seemed more focused on other research areas, and there seemed little prospect of change. As Gori noted, nutrition science was often poorly provided for in the medical schools, and tainted with the mark of quackery, not the sort of field that the NCI would generally support.Footnote 42 Practitioners interested in nutritional issues – nurses, nutritionists and others – were often low status and without a strong voice on the NCI. The Candlelighters’ initiative had improved the prospects for change and money for a host of new projects seemed a possibility. Yet with all these new possibilities came the unwelcome probability of having to share a small budget with researchers more interested in preventing cancer in the future than in dealing with the urgent needs of desperately ill patients in the 1970s. Whatever their sympathy for prevention, physicians remained focused on their sick patients, and anxious that money might disappear into a seemingly bottomless hole of aetiological research that offered little prospect of reducing cancer incidence or mortality for many years, if ever.
Diet as a Cause of Cancer
If advocates of therapeutically related research argued that their needs were pressing, so too did those interested in prevention. During the 1950s and especially the 1960s a growing body of epidemiological and experimental evidence had implicated diet and nutrition as causes of cancer. But – as with therapeutics – advocates of prevention argued that much more research was needed. In their view, the nature of the relationship between diet and nutrition was poorly understood, in part because of the historical neglect of prevention-related research, the technical difficulties of research in this area and the poor status of nutrition as a scientific field. The DNCP offered an opportunity to reverse such neglect at a time when public and Congressional concern about the NCI’s failure to promote prevention was growing. ‘Prevention is the only way we can make a major impact on survival’, commented the epidemiologist, Ernst Wynder, at the first meeting of the DNCAC,Footnote 43 ‘As interesting as therapy is, it will not make a major inroad on cancer…[it] has never wiped out a disease’.
Wynder’s was the strongest voice on the DNCAC arguing for more research into the cancer aetiology.Footnote 44 Best known for identifying cigarette smoking as a cause of lung cancer, Wynder became convinced that diet was a significant cause of this group of diseases, and that prevention was undervalued by the cancer establishment and often opposed by powerful industrial interests.Footnote 45 In 1969 he founded the American Health Foundation, eventually based in Valhalla north of New York City, to research cancer aetiology and prevention, including epidemiological and animal research in nutrition.Footnote 46 He told the committee that he thought about half of all cancers were nutrition related. According to Wynder, occupational cancers accounted for about 1% of the total, tobacco for 40% of cancers in males and, as he put it, ‘Most of the rest are related to nutrition’.Footnote 47
Wynder’s evidence for this statement derived from epidemiological studies of migrant populations that had blossomed in the 1960s, pioneered in part by NCI statisticians such as William Haenszel. Differences in colon, stomach, breast, kidney and bladder cancer rates between Japan and the US, he argued, had been attributed, to dietary differences.Footnote 48 Cancer rates in Puerto Rico were similar to those in Japan, and second-generation Puerto Rican migrants, like Japanese migrants, adopted a US diet and soon experienced cancer rates similar to the rest of the US. Had he wished to, Wynder could also have pointed to other studies – for example, among Polish migrants to the US, and rural migrants to Cali, ColombiaFootnote 49 – that showed that cancer incidence patterns of migrants changed from that of their native country/region to that common to the population of their new country/region; a transition often attributed to changes in dietary habits. Other studies of populations with special dietary practices, Wynder noted, showed positive evidence of a dietary relationship to cancer aetiology – Jewish populations in New York, Seventh-Day Adventists in California and the Mormon populations of Utah.Footnote 50 In migration studies, diet was difficult to disentangle from other environmental factors. These other studies offered an opportunity to control environmental factors: they focused on populations that lived in the same environment, but differed principally in terms of diet.
Such studies were not the first to link diet and cancer.Footnote 51 Yet earlier studies had remarkably little impact on the national cancer campaigns that emerged in the first two decades of the twentieth century. Dominated by physicians and scientists who tended to see cancer as a local cellular disease that subsequently spread to affect other parts of the body, such campaigns tended to focus efforts to control the disease on early detection and treatment.Footnote 52 Very little attention was paid to dietary causes of cancer or dietary means of preventing cancer, which were regarded as of unproven value and, like direct nutritional therapy, associated with quackery.Footnote 53 The creation of the NCI in 1937 did little to change the picture.Footnote 54 The new Institute broadly endorsed the model of early detection and treatment, and tended to share with other cancer control agencies a suspicion of claims that diet caused cancer. The Institute did support a small amount of research on diet and nutrition, notably Albert Tannenbaum’s important studies in the late 1930s and 1940s on the effects of caloric restriction on the development of spontaneous and chemically induced tumours in mice.Footnote 55 However, diet and nutrition were never central to its mission. According to Michael Shimkin, its intramural efforts in this area faded after 1950, paradoxically just as Wynder and others elsewhere began to take an interest in the subject.Footnote 56 Then, in the 1960s and especially the 1970s, the NCI’s disinterest in diet and nutrition came to be challenged by growing public and political interest in environmental and lifestyle causes of cancer and a growing acceptance within medicine of statistical associations as evidence of causal relations, notably following epidemiological research undertaken in the 1940s that identified cigarette smoking as a cause of lung cancer.Footnote 57 Such studies laid a foundation for the reception of studies of migrant and other populations that identified associations between diet and cancer.
This is not to say that the growing interest in environmental and lifestyle factors was unproblematic for the DNCP. As Robert Proctor has noted, much of the interest in environmental cancers in the 1970s focused not on diet and nutrition but on occupational cancers,Footnote 58 and where interest did focus on diet it often focused on subjects such as pesticides and additives that were beyond the remit of the DNCP.Footnote 59 It has already been noted that Wynder dismissed occupational cancers as a tiny proportion of cancers (1%), and he was similarly dismissive of additives and pesticides. Wynder argued that there were three major dietary factors in relation to cancer: food contaminants (which he regarded as the least important), specific nutritional deficiencies or imbalances, and specific nutritional excesses or imbalances notably in regard to fat and alcohol consumption (which he regarded as the most important). In his view, there was already enough evidence for the committee to advise the public to ‘reduce the total calories, reduce the calories from fat, and reduce the cholesterol intake’.Footnote 60
But, if Wynder had hoped for support from the DNCAC, he was to be disappointed. Even supporters of prevention on the committee were not persuaded of his arguments about dietary imbalances. Gori, for example, noted that there was very little scientific evidence as to what constituted a normal human diet, ‘rendering irrelevant talk of dietary excesses and deficiencies’.Footnote 61 In his view, it would only be possible to talk about excesses and deficiencies once the normalcy ranges for the human diet were known. This information, Gori claimed, combined with epidemiological studies, dietary surveys and exploratory studies in animals could help define the epidemiological significance and eventually the carcinogenic potential of altered dietary intake in humans. But the range of questions was immense – what was the impact of diet on the hormonal balance, internal secretions, the composition and substrates available to the enteric flora, and the carcinogenic and toxic stimuli that might intervene on cellular and genetic stability, the immune status, the detoxification and reproductive competence of the individual. There were so many unknowns about the relationship between cancer, nutrition and diet, and it was likely to take years to sort out.
It was here that the political weakness of prevention-related research was evident. While Congress was a strong advocate of such research, it was notoriously impatient for results, and spoke with more than one voice, pressing for a cure for the disease as much as (if not more than) it pressed for prevention. Critics of prevention were quick to highlight the point. ‘We could quickly use up $6 million in etiology, and it would be years before we could show progress’, noted the surgeon Stanley Dudrick,Footnote 62 ‘The legislators might become discouraged’. Dudrick and other critics argued that therapeutic-related research would provide quicker results than prevention;Footnote 63 that it was too early to reach conclusions on the relationship of diet to cancer;Footnote 64 that a focus on prevention might undermine efforts to do something for people whose cancers had already started;Footnote 65 and that the workshops sponsored by DNCP in 1975 came up with many more promising research ideas in therapy than in aetiology. The surgeon, Jonathan Rhoads (the Chair of the National Cancer Advisory Board), was moved to regret the poor showing of aetiology: nine of the top ten projects were in therapy or management and support, he noted.Footnote 66
Faced with such arguments, Gori retreated from his earlier position on prevention. He conceded that therapeutic research was likely to have a faster pay-off than that of aetiology, and that they had to show quick results if legislators were not to become discouraged. Congress had, he argued, been motivated to include diet and nutrition in the 1974 Act more by a concern about therapy than by statistics on aetiology. The epidemiological evidence, he noted, pointed to a variety of causative factors, but it pointed to too many things, and there was a consensus that the epidemiological approach to aetiology would be slow and difficult. By the end of the debate, the therapeutic lobby had prevailed. Instead, of Gori’s proposal of a budget split of 45%–45%–10%, the Advisory Committee recommended that the budget be divided 55% for therapy; 35% for aetiology and 10% for programme management and support.Footnote 67 In practice, therapeutics got an even larger slice of the cake: the actual funding in the fiscal year 1976 was 67.4% for therapy, 25.4% for aetiology and 7.2% for management and support, with the largest percentage increase going to work on artificial alimentation.Footnote 68 (Table 5) In the following years Congressional pressure would increase the percentage going to prevention.Footnote 69 The base-line from which future negotiations would start, however, had been set.
Table 5: ‘DNCP Recommended and Actual Funds Allocation, Fiscal Year 1976’. Source: Diet, Nutrition and Cancer Program, Status Report and Working Papers for the Advisory Committee Meeting December 14–15, 1976, National Institutes of Health, Building 31, Wing C, Conference Room 10, Bethesda Maryland 20014 (Bethesda: National Cancer Program, 1976), 12.

1977–78
So far the story of the DNCP is a tale of internal committee struggles over NCI research priorities in which epidemiologists and statisticians defended prevention-related research against pressure for more resources to go on therapeutics – and found themselves giving ground. But from 1977 these struggles moved out of the committee rooms and into a broader public arena. Frustrated with their poor showing against the therapists, and upset by NCI cutbacks in spending on diet and nutrition, advocates of prevention began a political and media campaign critical of NCI neglect of prevention research. This revitalised campaign brought the DNCP into the sights of the food industry, which was increasingly concerned about the direction of federal food policy. It also alienated senior figures within the NCI with its public criticism of their policies towards prevention. These problems, combined with Gori’s involvement in the separate debates over smoking, meant the DNCP faced a very unclear future.
Budget Problems
The DNCP had been established when the NCI was flush with money for small new projects in the early 1970s. Its budget had jumped after the 1971 Act, from US$190 million in 1970 to just under US$1 billion in 1977, allowing the NCI to initiate a range of new programmes, including the DNCP.Footnote 70 By 1977, the golden days were over. The budget continued to rise, but the money was draining out elsewhere, notably to the Comprehensive Cancer Centres (established across the country from 1973 to bring results of research rapidly to patients), and to the Special Virus Cancer Programme.Footnote 71 Other programmes began to feel the financial pinch. The NCI – under funding pressure from the Ford and Carter administrations – cut Gori’s proposed budget in half.Footnote 72
Gori reported in 1977 that funding limitations meant that the DNCP had not been able to implement many research recommendations of its Advisory Committee.Footnote 73 Congress had allocated US$6 million to the DNCP in 1975 rising to US$7.7 million in 1977. The problem was that these sums did not come close to meeting the needs of the programme. Gori estimated that proposed projects would cost about US$25 570 000, with about 103 projects needing support, and no-one knew where the money was to come from. Despite early concerns that few scientists would be interested in such a low status area of research as nutrition and diet, Gori had found himself deluged by enquiries and proposals for research at a time when the NCI faced a financial shortfall.Footnote 74 Nutrition research seemed to be caught between its own success and the general budget crunch. It was not the only NCI programme to suffer this way, but Gori took the difficulties to heart.
Frustrated with his inability to change NCI policy, in February 1977 Gori and his Advisory Committee went over the heads of NCI bosses, and wrote to the newly inaugurated President Carter and key congressional figures to complain about poor funding.Footnote 75 The previous month, Newsday had published a 16-day series of articles critical of the NCI’s war on cancer.Footnote 76 The nub of the Newsday criticism was that the NCI was losing the war on cancer, that too much emphasis was given to the virus programme and comprehensive cancer centres at the expense of more promising areas of research including prevention and that a reason for this was that the NCI’s peer review system and its advisory committee – the National Advisory Committee on Cancer – were loaded with people who were the recipients of funding and few had an interest in prevention, including diet and nutrition.Footnote 77 In short, NCI decision-making was rife with conflicts of interest that worked against promoting work in the most productive areas. Gori was one of Newsday’s sources.
According to Newsday, Gori charged that the heavy emphasis on virus research and treatment centres was a misuse of federal funds: the scientific consensus was that virus research was no longer the best route to a cure (the virus programme was ‘a flop’, an unnamed scientist was quoted by Newsday); nor was the focus on therapy the best route to reducing cancer incidence or mortality. In spite of the enormous increase in treatment money, the survival rates of cancer victims – except for some cancers in children – had not increased substantially in 30 years. How different the prospects seemed for prevention. Gori noted that the evidence was that the majority of cancers were environmentally produced and could be prevented. ‘In spite of this clear evidence’, Gori was quoted as saying, ‘the money is not where the priorities are’.Footnote 78
Public criticism set the seal on a growing rift between Gori and his NCI superiors. As one report put it later, ‘Going public with an intramural fight over the budget is a no-no in the federal government’.Footnote 79 Gori’s comments in Newsday, and the DNCAC’s approach to Carter, attracted the ire of Benno Schmidt (Chairman of the President’s Cancer Panel) and Guy Newell (the NCI’s acting director: Frank Rauscher having left to join the ACS, 1 November 1976). Newell began by publicly warning (unnamed) Advisory Committees not to engage in lobbying.Footnote 80 Then, in April 1977, he cut all of Gori’s advisory committees – the carcinogenesis, tobacco, and diet and nutrition committees.Footnote 81
The Carter administration – which had run on a promise of reducing the size of the federal government – had urged the NCI to reduce the number of its advisory groups. (Advisory group members were considered FTEs – full-time equivalents – and were an immediate target for downsizing.) Newell denied that his focus on Gori was retribution for the Diet and Nutrition Cancer Advisory Committee’s action, but commentators saw a connection.Footnote 82 Without the DNCAC, Gori was unable to use it to critique ongoing research or to generate new research priorities. One former member of the Advisory committee came to worry that it left the NCI inadequately advised on nutrition issues, a sign of its lack of commitment to the field.Footnote 83 At the same time, a shift in the NCI’s funding mechanisms – from contracts to grants – further reduced Gori’s ability to control diet and nutrition research.
Academic researchers had pushed hard for this shift, since grants were investigator initiated and gave more influence to the researchers than government administrators. From the point of view of researchers, contract mechanisms were vulnerable to favouritism, a means of extending the National Institutes for Health (NIH) intramural research without a proper review, potentially harmful to cancer research (research, they claimed, often targeted areas where basic knowledge about cancer was underdeveloped), and based on a flawed ‘philosophy that the role of management of fundamental science is the same as the role of management for engineering or development when the fundamental knowledge is available’.Footnote 84 By contrast, from the point of view of administrators, contracts were a convenient and quick means of promoting work in targeted areas, of differentiating programme objectives from scientific objectives and of maintaining management control over scientists who, in administrators’ views, often confused scientific and programmatic endpoints. As one DCCP document put it, advocating management through a mix of contracts and grants: ‘[M]any scientists do not understand that even successful completion of their proposed project may not necessarily contribute to the attainment of program goals’.Footnote 85 Contracts had the added benefit, for administrators, that they could be initiated without undergoing the sorts of review that was expected of grants. This is not to say that contracts were not subject to peer review: they were, but in different ways to grants. The 1974 amendments to the National Cancer Act required research and development contract proposals to be subject to peer review by groups composed of not less than 75% of non-federal employees.Footnote 86
In 1976 the vast bulk of therapeutic research was carried out by contract (65.9% of the total DNCP budget distribution), which included all the research on artificial alimentation and anorexia. By contrast 1.5% of the budget went on therapeutic research funded through cancer research emphasis grants (CREGs), a targeted grant established in the mid-1970s that aimed to replace some of the work done under contract. The equivalent figures for aetiology were 8.6% of total budget distribution on contracts and 16.8% on CREGs. With the appointment of Arthur Upton as NCI director, on 29 July 1977, all this was about to change. The NCI underwent a major reorganisation in 1978 in which Upton sought to separate programme management from grant and contract administration, and from the peer review of grants and contracts. Resources were diverted to fund more investigator-initiated grants, and heads of internal NCI research programmes were banned from wielding direct control over how funds were to be awarded to extramural investigators. Such developments limited the autonomy of the DNCP, which would have less independence than formally.Footnote 87
To complicate matters further, with the NCI in limbo searching for a new director before Upton’s appointment, the Director of the NIH, Donald Frederickson, attempted to reassert NIH authority over the NCI, lost after the 1971 Act, when the director of NCI had been made a direct Presidential appointee. (Before 1971, the director of NCI, like other directors at the NIH, had operated under authority delegated to him by the Surgeon General.) Part of the problem for Gori was that in 1975 the NIH established its own Nutrition Coordinating Committee (NCC).Footnote 88 Gori was a member of this committee, but he came to suspect that NIH was not particularly sympathetic to the difficulties faced by the NCI’s programme, since the NCC allowed the NIH to assert authority over the DNCP by integrating it into an overall set of NIH priorities in nutrition.Footnote 89 Things did not get much better for Gori with the appointment of Upton. While Upton was able to reassert NCI’s independence of NIH, he fired Gori’s boss at the DCCP, James Peters, and replaced him with an acting director, Gregory O’Conor, who eventually became director in April 1978.Footnote 90 Gori remained deputy director of DCCP, but rumours circulated that O’Conor wanted to choose his own deputy.Footnote 91
McGovern
Gori’s position in the NCI might have weakened, but he retained support in Congress, notably from Senator George McGovern (D-SD) who chaired a select committee on Nutrition and Human Needs.Footnote 92 Originally created in July 1968 to lead the ‘war’ against hunger among the nation’s young, old and poor, the committee later broadened its focus to include more controversial areas of food policy such as the role of diet in promoting chronic and degenerative diseases, including cancer. In 1976 the committee began a series of hearings, labelled ‘Diet Related to Killer Diseases’, which Gori allegedly shocked when he told it in August 1976 that diet might be related to more than half of all cancers in women and one-third of all cancers in men.Footnote 93 (He and Wynder published revised figures the following year, suggesting that about 60% of cancers in women and 40% in men might be diet related.Footnote 94) In 1977 the Committee released six dietary goals for the Nation: to increase carbohydrate consumption, and reduce the consumption of fat, saturated fat, cholesterol, sugar and salt. Briefly put, the committee sought to encourage people to eat more fruit, vegetables, whole grains, poultry and fish; to reduce their consumption of meat, eggs and foods high in fat, butterfat, sugar and salt; and to abandon whole milk in favour of non-fat milk. The report received a mixed reception from dieticians and nutrition scientists. Protests by the meat, egg, sugar and dairy industries forced McGovern to issue revised (and to these industries, less draconian) goals later in the year.Footnote 95
With the food industry alerted to its activities, in June 1978, the subcommittee on Nutrition undertook hearings into the diet and nutrition programme, under the chairmanship of McGovern, and with the support of the republican senator for Kansas, Bob Dole.Footnote 96 Gori did not provide evidence to the committee, but it was clear that it largely backed his position. As McGovern put it, about half of all cancers were linked to nutrition, and yet the NCI only spent about 1% of its funds on diet and cancer research and there appeared to be no prospect of an increase. In his view, the virus programme was not producing the results it promised, and stagnant survival figures for treatment did not support the NCI’s continued emphasis on therapeutic research.Footnote 97 Picking up on issues raised by Newsday, members of McGovern’s committee attacked the NCI for conflicts of interest in its review process that worked against nutrition research, and highlighted the neglect of nutrition in the medical schools, including Arthur Upton’s former institution, the State University of New York at Stony Brook. Called before the Committee, Upton was repeatedly put on the defensive, forced to regret the neglect of nutrition in the medical schools and to confess that the NCI had difficulty in knowing exactly how much it spent on nutrition. He also conceded that controls on spending were inadequate, that the NCI did not do enough in the field and that it would seek more for nutrition research.Footnote 98
Upton’s difficulties with the McGovern Committee can have done little to endear Gori to the NCI director. Gori’s close connections to McGovern were well-known: he was a regular advisor to McGovern, as well as to Dole and another congressional supporter, the former presidential candidate, Hubert Humphrey. The difficulty for Gori was that these connections were becoming as much a liability as a help. Dole was rising in the Republican Party, but McGovern’s political star was on the wane after the problems of the Nutrition committee’s 1977 report, and Humphrey was dying of cancer.Footnote 99
Then, in August 1978, Gori sealed his political fate on a completely separate issue, when he and Cornelius Lynch published an article that sought to quantify ‘less hazardous’ levels of smoking by calculating the number of cigarettes of different brands that could theoretically be smoked without exceeding what they called critical levels for six major toxic smoke components. A report in the Washington Post that Gori and Lynch had identified safe or tolerable cigarettes generated a public storm. The article not only angered his bosses at NCI, but also drew the ire of the Surgeon General, the ACS and the Department of Health, Education, and Welfare (HEW) Secretary Joseph Califano, then in the midst of an anti-smoking campaign.Footnote 100 The article was the end of what influence Gori retained at NCI, and by September 1978 he had effectively lost control of all his programmes. Gori remained as DCCP deputy director, but he went to Johns Hopkins University to do a Master of Public Health (MPH) degree, a move widely seen as removing him from significant power within NCI.Footnote 101
Thus, after a volatile four years, Gori was gone. With his MPH in hand, he returned to his position as Deputy Director of the DCCP, but without many of his former responsibilities. He left the NCI in 1980, joined the Franklin Institute with a US$400 000 endowment from the Brown and Williamson Tobacco Company, and later worked as a consultant to the company in its legal cases.Footnote 102 The DNCP, which had been administered by the Division of Cancer Cause and Prevention, was reorganised and decentralised (Figures 3a and 3b). The DNCP itself was transferred to the Office of the Director of NCI, and programme development was devolved to the divisions under the umbrella of the DNCP.Footnote 103 Put another way, the new DNCP would co-ordinate but not direct the nutrition work of the Division of Cancer Treatment (DCT), the DCCP and the Division of Cancer Control and Rehabilitation. This structure was in line with Upton’s broader reorganisational goal of separating programme management from grant and contract administration, and from the peer review of grants and contracts.
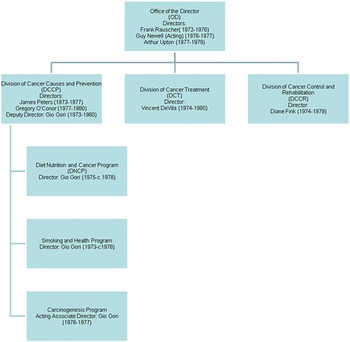
Figure 2: NCI offices, divisions and programmes associated with the DNCP, 1974–78

Figure 3: Structure and framework of the Diet, Nutrition and Cancer Programme, 1978. Figures (a) and (b) provide two snapshots of the DNCP structure and framework as it evolved in 1978. Both illustrate the decentralisation of the programme after Newell took over, components of the programme being developed within the three divisions rather than by the DNCP Director. Figure (a) illustrates the structure of the DNCP as it was envisaged by Newell shortly after he took over in 1978, and includes the individuals responsible for the diet and nutrition research within each division, as well as the DCRRC (Division of Cancer Research Resources and Centres), the division responsible for managing NCI grant supported activities, including the review and coordination of programmes such as DNCP. Figure (b), which was published about the same time, provides a slightly different structure, and may be a later iteration, and sets out the research areas of each division and the relation of the DNCP to the NCI director. The absence of the DCRRC should not be taken as indicating that it had no review function in relation to the DNCP. Sources: Figure (a) Guy Newell, ‘Presentation to the National Cancer Advisory Board’, 18 September 1978, NCI archives: item number PB003861. The full names of the directors/officials are Guy R. Newell, Mildred Ellison, Thaddeus J. Domanski, Daniel L. Kisner and Lawrence D. Burke. There is no original paper copy of this document, and the quality of the PDF/photocopy image is very poor. This image has been enhanced for clarity by Hank Grasso. Figure (b) Diet, Nutrition and Cancer Program. Status Report. September 1978 (Bethesda, MD: Diet, Nutrition and Cancer Program, September 1978), 26.
Upton gave the job of programme coordinator to Gori’s nemesis, Guy Newell, who shortly after turned it over to Diane Fink, the head since 1974 of the NCI’s Division of Cancer Control and Rehabilitation. ‘I view my role as one of management rather than direction. The direction will come from within the major NCI Divisions’,Footnote 104 Newell noted in September 1978, discussing the role of the ‘director’ within the new decentralised DNCP structure (Figure 3). Newell also announced that whereas in the past much of the research supported by the DNCP had been funded under contracts, in FY 1979 grants would be emphasised as the means of funding research. Contracts would be used for a much more limited range of activities, not generally including research.Footnote 105
Prevention and Therapy
In a series of articles written in the 1970s, the Washington Post journalist, Daniel S. Greenberg, attacked the NCI for favouring basic research and cures rather than studies of environmental causes of cancer.Footnote 106 Behind such an emphasis, Greenberg detected the hidden hand of the ACS, the major non-profit organisation concerned with cancer. In his view, the ACS (dominated by physicians interested in cancer therapy) exploited its extensive social and business connections to overwhelm a politically timid NCI. The result, according to him, was that most of the NCI’s money went either on therapeutic research or on work on cancer causation that was unlikely to upset any significant political or business constituency, with the possible exception of the tobacco industry. By contrast, studies of environmental carcinogens were politically much more difficult, since many were produced by powerful industrial corporations. The point was particularly significant in the case of diet and nutrition. As evidence mounted about the carcinogenic effects of pesticides, food additives and diets high in meat or certain fats and sugars, the farming and food-processing industries began to become alarmed. Greenberg saw such interests – combined with the low status of nutrition science and elitism within NIH – behind federal neglect of nutrition research.Footnote 107 Whatever the truth of Greenberg’s assertions, he was repeatedly able to force the NCI to issue rebuttals to his attacks. In 1977, a world-weary NIH director forwarded one Greenberg article to the NCI director congratulating him ‘on being considered worthy of a despairing sigh by Daniel S. Cassandra’.Footnote 108
Greenberg’s analysis would have found many supporters within the DNCP, and it captures and elaborates one of the themes of this essay – the uneasy birth of federal support for cancer prevention in the 1970s. But if this essay is a story of the problems of prevention research, it is also story of the problems of therapeutics. It tells the tale of how growing public criticism of the NCI in the 1960s and 1970s gave diet and nutrition research increasing significance as a means of improving therapy, and so brought advocates of therapy into competition with prevention over scarce resources. As we have seen, therapists were able to persuade the DNCAC that therapeutically related research proposals had stronger scientific merit, were more likely to produce results and quickly, and were more likely to appease the programme’s supporters in Congress. Even Gori – an advocate of prevention – came to acknowledge the political calculation that prevention research was unlikely to provide the sorts of results that would satisfy Congress, especially as it also risked aggravating allies of the food industry on Capitol Hill. The mere threat that the industry’s powerful supporters could cause problems for a field already struggling to satisfy Congress was enough to make prevention research seem a risky political venture.
The DNCP can, therefore, be seen, in part, as a microcosm of broader tensions within the NCI between therapeutics and prevention over funding priorities. But, if its early history is a story of the tensions between the two, its later history is a story of an emergent (albeit temporary and uneasy) alliance between prevention and therapeutics, as from the mid-1970s the DNCP came into competition for funds with larger NCI programmes, notably the Special Virus Cancer Programme and the Comprehensive Cancer Centres. In some ways, this competition exacerbated tensions between therapy and prevention on the DNCAC, for it was advocates of prevention who figured most prominently in the political and media campaigns to save the DNCP, and much of their criticism was directed at the therapeutic orientation of the NCI. Yet, I suggest, it also brought the two sides of the DNCAC together to fight the common threat to their programme. Advocates of prevention saw political benefits in allying themselves with therapists (given the latter’s political clout within the NCI and on Capitol Hill), while therapists also saw political benefits in allying themselves with advocates of prevention (given the strong sympathy for prevention within Congress and in certain sections of the media).
As the debate on diet and nutrition intensified in 1977, strains between prevention and therapeutics grew. The temptation to jump ship, however, was briefly held in check as all sides of the DNCAC waited to see how events would play themselves out. The move to go over the heads of the NCI and appeal to President Carter resulted in no (public) criticism from any member of the DNCAC, advocate of therapy or prevention. Privately, some may have disagreed with this move, but Newell’s response – the cutting of Gori’s committees – seems to have temporarily sealed an uneasy union, since it ended any opportunity for anyone to use the DNCAC to promote their agendas, and opened the possibility of all having to compete against other investigator-initiated proposals rather than determine policy behind committee doors.Footnote 109 The union ended with Gori’s removal, and probably more importantly Upton’s reorganisation of NCI and the DNCP in 1978, which meant that the actual direction of research shifted to the division responsible for administering that part of the programme (Figure 3). The reorganisation was presented as a means of broadening the scope of the programme, and of integrating all diet and nutrition elements of the national cancer programme. It also gave sectional interests a greater level of autonomy, however, and reduced administrators’ ability to shape the programme, especially with the shift from contracts to investigator-initiated grants. The sorts of political alliance that had held under Gori’s tenure began to break up and new ones to form.
The story of the DNCP is thus a tale of shifting alliances and co-evolving relations between cancer therapy and prevention. Its emergence began with parental concerns about their sick children expressed though the Candlelighters, one of a new breed of single-issue health advocacy groups that emerged in the 1960s and 1970s pressuring Congress to redirect NCI spending to areas of their interest.Footnote 110 It was also facilitated by a growing political interest in environmentalist critiques of medicine in the 1960s and 1970s, and Congressional concern about the neglect of nutrition in the medical schools, the role of diet and nutrition in the onset of chronic disease, and the NCI’s focus on therapeutics and basic (virus) research. But Congress was often a divided house, subject to conflicting lobbies from commercial, biomedical, patients’ and other advocacy groups, and these divisions were exploited within the NCI to direct funding one way or another – as when supporters of therapeutics persuaded the DNCP that it would be politically worthwhile directing more resources to therapeutics at the expense of aetiology, or when the political calculations changed in 1977 and therapists came to support advocates of prevention to save the DNCP from outside predations. The history of the DNCP was thus the product of struggles and negotiations between numerous often conflicting groups and individuals, distributed across many institutions (governmental and voluntary), all seeking to promote their own interests and agendas.
Such struggles were exacerbated by Gori who emerged as a polarising figure in the fights over the DNCP. The NCI was an organisation sensitive to public criticism, in which budgetary decisions were often fought out behind closed doors, with public displays of consensus masking internal conflict. This is not to say that it was not possible to make discontent public, but it was often done discreetly, perhaps through third parties and anonymous leaks, and always in ways that did not embarrass those higher up the organisational hierarchy upon whom subordinates depended for support. By the mid-1970s, Gori had abandoned such discretion, and so opened himself to attacks from powerful groups and individuals within the NCI, public expressions of discontent being especially dangerous to smaller, weaker groups within the organisation, and those who worked within them. It could be argued that the DNCP would have suffered cuts in the mid-1970s no matter who was chief. Gori’s strategy, personality and simultaneous involvement in controversies over tobacco, however, ensured a more spectacular conclusion to his directorship than others might have achieved. As one report put it euphemistically he was ‘one of NCI’s less inhibited infighters at budget distribution time’.Footnote 111
Gori’s problems thus provide an insight into the patronage system within the NCI.Footnote 112 The agency in the 1970s often presented itself as a meritocracy in which the route to success on the Bethesda campus of the NIH was research or administrative excellence. But, if the NCI was a meritocracy, it was also a hierarchical organisation that revolved around networks of patronage. The Institute was a warren of fiefdoms headed by the NCI director (from 1971, a Presidential appointee), who presided over subordinate directors, who in turn presided over more minor officials. Each director and subordinate supported individuals and groups within his or her section of the organisation, which might also be subdivided into further sub-sections, headed by subordinate subordinates, all of whom offered patronage to those under them and (at least public) support and loyalty to those above. Thus a key to advancing a career within the NCI could involve finding powerful patrons and keeping them on board as supporters. These patrons might act as mentors and advisors, and could shield less powerful individuals from political harm. Equally, a patron could leave a subordinate vulnerable if the latter did not live up to expectations, the politics got too hot, the patron was negligent of support or moved on elsewhere. In all such circumstances a previously sheltered subordinate could suddenly feel chill winds.
Gori fell afoul of such shifts. Starting under the wing of his director/patron James Peters, he found himself isolated and vulnerable after Peters’ left, with rumours that his new boss wanted someone else in his place. As economic circumstances changed in the mid-1970s, Gori found himself constantly struggling against the NCI hierarchy for more funds, and loosing support, especially after he tried to circumvent his seniors within the NCI by appealing to their political masters. This, and the political miscalculation of his involvement in the smoking debate, left him vulnerable and without support from powerful individuals within the organisation, and he lost control of the DNCP, and eventually had to leave the NCI. This did not end the programme, but it allowed it to be split along pre-existing lines of tension, which ensured that therapeutic and preventive research on diet, nutrition and cancer were carried out relatively autonomously under separate parts of the NCI, albeit still under the umbrella of the DNCP.
Subsequent NCI leaders would distance themselves from Gori, and some erased him from historical accounts of the programme.Footnote 113 But, it is also arguable that his willingness to go public maintained pressure on the NCI to improve what in 1978 one staff member on McGovern’s Senate Committee on Nutrition and Human needs called ‘the abysmal nutrition research effort by the NCI’.Footnote 114 Gori might have gone, but he had set the stage for NCI interest in diet and nutrition research in the 1970s and especially the 1980s, as it sought to address an emergent scientific consensus that diet and nutrition were the major preventable causes of cancer after smoking.Footnote 115










