INTRODUCTION
The principle of radiotherapy is to treat the tumour to the highest possible dose, whilst sparing the normal surrounding tissue.Reference Symonds and Foweraker1 Ensuring accuracy and reproducibility is vital, to allow dose escalation to the target volumes while keeping the toxicity to surrounding tissues, minimal. Modern radiotherapy techniques require tight margins around the target volume in order to spare the organs at risk (OAR’s).Reference Huddart, Nahum and Neal2 Patients undergoing radiotherapy to the prostate require a tight margin around the target volume due to the proximity of the rectum. The rectum is shielded as much as possible to reduce the potential side effects.Reference Hanley, Lumley and Mageras3 In order to achieve this level of accuracy it is essential that the treatment position used is reliable and reproducible so that the treatment given does not result in a geometric miss. To ensure that the patient lies still and in exactly the same position, appropriate immobilisation must be used.Reference Zelefsky, Happersett and Leibel4 Pelvic setups can be difficult with ongoing debates over whether supine or prone is better.Reference Boehmer, Maingon and Poortmans5 Current departmental setup is to have the patient prone with no rigid immobilization, which is not always the most stable as patients can be uncomfortable. The introduction of a bellyboard was proposed to immobilise the patient and to hopefully make the setup more reproducible. Bellyboards have been used by several authors when treating rectal and gynaecological cancer patients.6,7,8 These studies suggest that the bellyboard does allow reproducible setup with these patients. This study will evaluate the introduction of a bellyboard to the existing technique used for treating radical prostate patients and the influence this had on accuracy and reproducibility. The null hypothesis that will be tested is that the introduction of the bellyboard into the technique will have no statistically significant effect on the reproducibility and accuracy of the treatment at the 5% level.
MATERIALS AND METHODS
This was a single institution study which had approval from the medical research ethics committee within the NHS trust. The bellyboard that was used for this study was the CIVCO medical solutions Contoura Carbon Fibre Bellyboard.9 All patients were treated using a Varian Linear accelerator with energies of either 6 megavolts (MV) or 10MV.
Sample
The control group contained 30 participants treated in the standard manner. The first 30 patients on the bellyboard were selected, within the same time frame so that bias was reduced. This gave a total of 60 patients, which was thought to be achievable when the number of prostate patients going through the department was taken into account, during the period that the bellyboard was available. Thus the sampling used was non random namely purposive sampling.Reference Polit and Hungler10
Inclusions
All participants were male and underwent conformal radical radiotherapy treatment for localised prostate cancer. All patients were deemed suitable by the consultant. The research group underwent treatment on a bellyboard in the prone position. The control participants consisted of patients treated in the prone position with no rigid immobilisation. Both sets of participants underwent radical radiotherapy following standard protocol. Standard protocol within the department for the patients is a three field isocentric technique with an anterior (ant) field, left posterior oblique (lpo) field and a right posterior oblique (rpo) field. The oblique fields have 120 degrees between them. The patients were treated at a fixed bed height rather than tattoo position due to studies showing the benefits of this technique.Reference van Lin, Nijenhuis, Huizenga, van der Vight and Visser11 Patients routinely undergo a 20 fraction treatment schedule following an initial verification fraction. Patients had electronic portal images (EPI’s) taken following protocol for the duration of their treatment. Any patient in whom protocol was not followed was excluded.
Exclusions
Patients were excluded, if they had undergone palliative radiotherapy rather than radical, could not lie in the prone position or anyone unable to complete their course of treatment.
Image analysis
Anatomy matching was performed on all portal images acquired throughout the patients’ treatment. The matching of anatomy begins with the outlining of clearly visible stable bony anatomy on the portal images. It is recommended by the Royal College of Radiologists that a minimum of three points are used for anatomy matching.12 In this case it is likely that the three anatomical landmarks used were the symphysis pubis, superior pubic ramus and the obturator foramen. The process of anatomy matching allowed all deviations from the isocentre position to be noted. This was performed for all three treatment fields – ant, lpo and the rpo. The directions that were noted were left-right, superior-inferior (sup-inf) and anterior-posterior (ant-post).
Statistical methods
The results from both sets of data were analysed statistically using Statistical Package for Social Sciences (SPSS). The results were checked for normality using the Shapiro–Wilks test and then the Mann–Whitney test was utilised to check for statistical significance. It is important when considering the introduction of any new technique to look at the random and systematic errors of both the existing and the new technique. Both factors together give the total error, although the random error is harder to determine than the systematic, which is expected and predictable.Reference Hurkmans, Remeijer, Lebesque and Mijnheer13 Guidelines from a document from the Royal College of Radiologists12 on how to calculate the systematic and random error have been followed to assist with this analysis.
The following equation for the population systematic error taken from page 30 of the aforementioned reference was used.
For the population random error the following equation was used taken from the same reference on page 31.
RESULTS
Data was collated for a total of 60 patients which was equally split between the control and bellyboard groups. An EPI was taken for each field. For each field a total of 120 images were taken and analysed in every direction. In total, data from 720 images was analysed. The number 720 came from images being taken for the three fields on each of the four imaging days, which were the verification, days 1, 2 and 11. This meant that each patient had 12 images and there were 60 patients in total giving 720 images. The actual data from each image was for a shift in either the left-right or sup-inf direction in the case of the ant image and in the ant-post and sup-inf direction for the rpo and lpo images. So there was data for 1440 shifts. The Shapiro–Wilk test showed that the data was not normally distributed.
Mean and standard deviations
The data from the test for normality also gave information on the mean and standard deviations for each group for all fields and directions. The values for these can give valuable information about the techniques with a low standard deviation indicating the data set is close together and in turn a high standard deviation indicates the data is spread over a range of values. Once the data had been analysed it could be seen that there was not any meaningful variation in the mean or standard deviations for either group. This was the same for each field and direction. The mean for the control group in the sup-inf direction varied between –0.05 & 0.06 cm, in the ant-post direction it was between –0.19 & –0.12 cm and in the left-right direction it was found to be –0.1 cm. The mean for the bellyboard group in the sup-inf direction was –0.01 & 0.03 cm, in the ant-post direction it was –0.20 & –0.14 cm and in the left-right direction it was –0.04 cm. For the standard deviation the values for the control group varied between 0.17 & 0.37 cm. For the bellyboard group the standard deviation was between 0.24 & 0.29 cm.
Distribution of displacements
The distribution of the displacements for both groups in all directions is displayed in Figure 1.
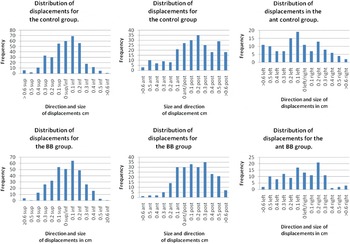
Figure 1. Distribution of displacements in all directions. (a,b) Displacements in the Sup–Inf direction. (c,d) Displacements in the ant–post direction. (e,f) Displacements in the left–right direction.
DISCUSSION
Although the results showed no statistical significance there are other factors that must be taken into consideration. When the mean and standard deviations were compared for each group there was little difference. On all occasions the standard deviation for the sup-inf direction for the control group had a smaller value. Figure 1 shows that a small number of displacements over 0.5 cm were found in the sup-inf direction agreeing with this. This is not surprising as with the bellyboard technique there is a need to have the patient at a precise point on the board that is not required with the control technique; therefore, introducing potential for error. It will be interesting to see if this reduces in time as radiographers become more familiar with its use.
An interesting study by Griffiths et al. discussed the different ways in which departments set up their patients using tattoo’s, lasers and table height in different combinations.Reference Griffiths and Sydes14 The most effective was found to be aligning the tattoos with the laser level and in turn with the table height. This was the method used when setting up the control and bellyboard patients. Using table height alone was not found to give a desirable outcome. Importantly it is mentioned that what works in one centre does not necessarily work in another. A study by Harris et al. looked at the addition of immobilisation when treating obese pelvic patients in the prone position.Reference Harris, Daniel, Elder, Luffman, Bowen and Casebow15 They found that this cast dramatically reduced the accuracy of the treatment and in fact stopped the study after four patients due to this. It was thought that skin pulling caused by the cast caused the discrepancies. It would be hoped that the bellyboard and the presence of the hole would mean that no skin pulling occurred. Certainly results indicate that there is not a drastic effect caused by the addition of the bellyboard as this would have shown up in images. If this had been the case the study would have been halted. It would be interesting to investigate further to see, if perhaps this does occur to a much lesser extent than that found by Harris et al. perhaps in those with excess skin.
For the left-right shift the standard deviation is smaller for the bellyboard group. This was also noted for the anterior-posterior shift that the bellyboard group had a smaller standard deviation. Again Figure 1 backs up these results. Both may be due to the contoured surface which some patients mentioned made them feel more stable and then in turn more relaxed. Patients were given the opportunity to lie on the treatment couch alone as well as on the board.
During the course of a patient’s treatment it is sometimes necessary to make corrections to the setup. There were 3 patients in the bellyboard group, participant number 1, 18 and 23, where this was the case. Participant 1 had a daily stop and check to ensure correct lateral positioning. Participant 18 had an adjustment to correct for an ant-post shift from the intended isocentre position. A similar situation was found with participant 23. Participant number 18 was the first patient on the bellyboard which may go a little way to explain this discrepancy. Eight patients in the control group required corrections to their treatment – participants 1, 3, 9, 11, 17, 20, 21 and 28. Two of these required more than one alteration in order to achieve the desired treatment. Participant 9 required both a change in the anterior-posterior direction and in the left-right direction. Participant 21 posed a more difficult task and actually required three alterations during the treatment course, consisting of a shift in the left-right direction and two changes in the anterior-posterior direction resulting in the need for resimulation. This result is in keeping with the literature suggestions that prone patients should be appropriately immobilised otherwise they are unstable. The remainder of the participants had a mixture of both left-right and anterior-posterior shifts. Ten percent of the bellyboard patients had corrections to their treatment setup. In the control group 37% of the patients had changes made to their treatment. The control group was being treated with a technique, which has been established within the department for over 10 years. The bellyboard technique has only been in use within the department for the duration of these 30 patients.
It was noted when examining the data that there were several outlying data sets. Outliers are important and can sometimes show valuable information. Outliers can show underlying problems with a technique; for instance if all outliers happened to be obese it may be that the bellyboard was unsuitable for this category of patients. Outliers were classified as those participants with a deviation of over 0.5 cm from the isocentre. The value of 0.5 cm is the set tolerance limit used within the department and so any deviation over this was deemed out of tolerance. All of the data for the outliers was collated and it was decided that only those participants that displayed two or more deviations over 0.5 cm from the isocentre position would be deemed as true outliers. Participants with only one deviation over 0.5 cm could result from a one off random event. When there is only one occurrence it is impossible to say that this is due to a systematic error.
Analysis of displacements over 0.5 cm.
The information shown in Table 1 agrees with that found from the mean and standard deviations and Figure 1.
Table 1. Number of images that showed deviations over 0.5 cm in each group
Within the control group the maximum displacements for left-right = –1.3 cm, sup-inf = 0.7 cm and ant-post = –1.3 cm. For the bellyboard group the maximum displacements were left-right = 0.7 cm, sup-inf = 1.0 cm and ant-post = –1.3 cm.
When anatomy matching the fields to examine any displacements that are there, it is normally found that the ant field is the easiest to do this with. The oblique fields can sometimes pose more of a problem due to the anatomy being more difficult to see when the image is from an oblique angle. Since this is the case for both the control and bellyboard group it would be assumed that this issue would be even between the two groups.
Systematic and random error
A combination of systematic and random error gives the total error for the associated technique. Within the department the technique must allow accuracy within 0.5 cm. The combined error was within 0.5 cm for all directions. This implies, both techniques are able to allow reproducible setups to within 0.5 cm accuracy. This is vital when introducing any new technique within a department and is necessary to show how reproducible a technique is.
Trends
In the anterior-posterior direction in both groups it appears there is more of a shift in the posterior direction. It can be seen by looking at the mean values which are all negative ranging from –0.12 to –0.20 cm. This may be just a random event but the fact that it is occurring frequently would suggest not. The graphs in Figure 1 for the ant-post displacements agree with the results found for the mean values. The displacements appear to all be shifted to the right, which is a shift in the post direction. Several possible reasons that could explain this are discussed below.
If a patient is tense it can completely alter how they setup on treatment, possibly resulting in a shift from the isocentre position. Bujko et al.Reference Bujko, Czuchraniuk and Zólciak16 showed the effect that tensed muscles could have on altering treatment position. Within the department the anterior field is treated first, followed by the rpo and then the lpo. It is reasonable to assume the patient may gradually relax throughout, leading to differences between fields. Most patient manipulation takes place before any of the treatment has begun, to ensure the patient is in correct treatment position, and the patient will gradually become more relaxed once they are not being moved.
Equipment could be introducing an error into the techniques causing a discrepancy. It has been noted within the department that there may be couch sag. The CT, simulator and treatment couches are all different specifications as they have different manufacturers. The simulator couch is several centimetres thicker than the other couches. It is sensible to suggest that the sag on all three couches is different from one another. van Lin et al.Reference van Lin, Nijenhuis, Huizenga, van der Vight and Visser11 mention that a systematic error was introduced in this direction due to the sagging effect differing between the simulator and treatment couch top. Investigations are ongoing into this issue and whether anything can be done to reduce this, if it is indeed found to be the cause of a systematic error.
CONCLUSIONS
Although the null hypothesis was unable to be rejected there are some interesting aspects to the data. It can be seen that the introduction of the bellyboard was no worse or better than the control group technique. From the results that were found some inferences can be made. Within the control group there were eleven occasions where patients required alterations to their treatment to ensure they were being treated at the intended isocentre. Within the bellyboard group this only happened on three occasions. This would seem an encouraging result. Analysis of individual images showed that there were more deviations in the control group that are greater than 0.5 cm from the isocentre position in both the left-right direction and the anterior-posterior direction, although in the sup-inf direction there were found to be more within the bellyboard group. With time and more experience in the day to day positioning of the patient this potentially may decrease. All in all, these results showed promise for the new technique and it was deemed appropriate to further trial this equipment with more patients.
RECOMMENDATIONS
It will be interesting to investigate further, perhaps in a year’s time, to evaluate whether future results are still similar to those found in this study. The increased information that would be gained once a larger sample size has been achieved would only help to elucidate the situation more accurately. It may also be appropriate to look at the potential of introducing orthogonal fields for verification purpose only. This introduction would hopefully aid in making it easier to anatomy match those images as they would be at direct lateral angles rather than oblique ones. Although the EPI’s taken for the present study were useful in showing any differences between the two techniques they only really show a snap shot. By progressing on to intrafraction imaging a clearer picture may be gained with the continual imaging throughout each beam. This may be the next step to take.
Although not looked at in great detail it would be assumed that with increasing fraction number the size of displacements would decrease. Stanley et al. found that over the course of a patient’s treatment, displacements over 0.5 cm decreased. It would be interesting to see if this was the case in both groups.Reference Stanley, Griffiths and Sydes17 The fact that the patients become more settled makes a big difference to the way in which they set up on a daily basis. Another interesting avenue to explore may be the introduction of a booklet explaining the bellyboard and what is expected of the patient. Although there is a general explanation booklet it is a generalised overview and may benefit from being more tailored. Again to further look in this direction the use of prostate seeds with image verification may give an indication of the impact on organ motion. Although it is acknowledged that this may impact it was seen as out of scope of the current research.
Within the department, bladder patients are treated in the prone position without any stable immobilisation. In the future it may be introduced into this setup. Although further investigation at the CT stage may be necessary to see the impact the board has on the shape of the bladder and the knock on effect at the planning stage. The consultant has shown an interest in trying this equipment with patients who are having their spine treated and require to be in the prone position. The attenuation of the beam and the correction factors needed depending on where exactly the field ended up would be required. These are exciting prospects to further research in the future.




