Introduction
Colostrum is a concentrated form of ‘immature milk’, which is very high in protein, antibodies, vitamin A and other protective components that are important for newborn(Reference Silva1). According to the World Health Organization (WHO), colostrum is defined as the first milk, thick, sticky and clear to yellowish colour secreted during the first hour after birth up to 3 d. It is also called ‘liquid gold’ and ‘passport of life’ due to its highest content of antibodies as compared with mature breast milk(2). It contains all the necessary nutrients for infants’ growth and development and antibodies that can protect from many childhood illnesses(3,4) . This nutrient is the most suitable food for the newborn, universally acknowledged as the perfect first food for infants and a suggested regimen for expressing and storing it during pregnancy including counselling on skin-to-skin contact in the first 24 h to maximise breast milk production for long term(4). Neonates have a premature digestive system that outfits the small-volume rigorous form of the nutrient supply system of colostrum. The laxative influence of colostrum encourages the passage of newborn's first stool (i.e. meconium) which is important to prevent jaundice by removing extra bilirubin(Reference Gebrehiwot, Thampi and Kassaw5).
The WHO approved the infant feeding strategy which included the recommendations for exclusive breast-feeding until 6 months of age with sustained breast-feeding during optimal complementary feeding practice. This recommendation has been endorsed by many countries including Ethiopia. Early and exclusive breast-feeding, including colostrum feeding is one of the most important things to achieve sustainable development goals by 2030 through improving infant survival(6).
Globally, improving breast-feeding rates around the world could save the lives of more than 820 000 children under age 5 every year, the majority (87 %) under 6 months of age(3,Reference Victora, Bahl and Barros7) . It is one of the optimal breast-feeding practice not only saves the lives of children under 5 years but also improves children's quality of life(Reference Gupta, Holla and Dadhich8). In resource-limited countries (i.e. Ethiopia), lactating women have limited understanding of colostrum advantages(Reference Dhale and Mahakalkar9–Reference Mose, Dheresa and Mengistie11). As a result, they preclude their infants from colostrum feeding immediately following delivery. Colostrum discarding removes vital nutrients which lead to high infant morbidity and mortality(Reference Kakati, Rahman and Borah10,Reference Bililign, Kumsa and Mulugeta12–Reference Weldesamuel, Atalay and Zemichael14) . The prevalence of colostrum discarding varies from country to country and accounts for around 29⋅5(Reference Kakati, Rahman and Borah10), 20(Reference Joshi, Barakoti and Lamsal15) and 11⋅2 % in India, Nepal and Cameroon, respectively(Reference Tambe, Mimboe and Nchung16).
Different studies performed in different rural part of Ethiopia found that the prevalence of colostrum avoidance were 20⋅9(Reference Gualu, Adugna and Dilie17) and 6⋅3 %(Reference Weldesamuel, Atalay and Zemichael14) in Debre Markos and Aksum, respectively. Some societies considered colostrum as heavy, profuse, unclean, contaminated and risky for the health of infants. As a result, colostrum is thrown out, and honey, sugar water, glucose and water were given to the newborn as substitutes(Reference Weldesamuel, Atalay and Zemichael14). Even though there are some studies on the prevalence of colostrum avoidance practice in some parts of Ethiopia including the neighbourhood district called Kombolcha in South Wollo Zone and three districts of this study area with a result of positive predictors such as illness of index child, residence, counselling on timely initiation of breast-feeding, participation in pregnant women forum, husband employment and cultural beliefs with the prevalence of colostrum avoidance practice 11⋅4(Reference Gebreyesus, Girma and Cherie18) and 12 %(Reference Yimer and Liben19) with limited child age group with different study design. Still there has been a paucity of information about the level and determinant factors for colostrum avoidance which were not well studied mainly in this study area with the advantages of targeted age group. Therefore, the present study aimed to assess the level and predictors factors of colostrum avoidance among mothers having children aged 6–59 months in North Wollo Zone, Ethiopia. The findings of the present study are essential to develop evidence-based specific nutrition intervention for colostrum avoidance primarily in the study setting and also throughout the country with similar socioeconomic characteristics as a whole.
Methods
Study area and design
The North Wollo Zone is located at 521 km far from Addis Ababa and 251⋅75 km from the capital city of regional state called Bahirdar. North Wollo is one of eleven zones of the Amhara Region of Northern Ethiopia. South Wollo borders it on the south, on the west by South Gondar, on the north by Wag Hemra, on the Northeast by Tigray Region and on the east by Afar Region; part of its southern border is defined by the Mille River. Weldiya (also spelled Woldia). North Wollo acquired its name from the former province of Wollo. It is subdivided into 14 Woredas and 312 kebeles (276 rural and urban 36). The climatic condition of the Zone has varied between 10 and 27°C. Cereals are the staple foods. Most of this Zone is mountainous and characterised by steep slopes, which are unsuitable for agriculture and severely limits the cultivated area. An average farmland shared by a household is less than or equal to 0⋅7 hectare. Based on the national census conducted by the Central Statistical Agency of Ethiopia (CSA), this Zone has a total population of 1 788 901, of whom 895 189 are male and 893, 712 female; with an area of 12 172.50 km2. Of these, 241 502 are children aged 6–59 months. The governmental health institution of the Zone has 6 public hospitals, 68 health centres and 296 functional health posts.
Study design and period
An institution-based cross-sectional study was conducted among mother–child pair aged 6–59 months attending under five child health services in the North Wollo Zone from 01 November to 24 December 2020.
Source and study population
All mother–child pair aged 6–59 months who attends under five children in public health services at the North Wollo Zonal were taken as source population. All selected mother–child pair aged 6–59 months who attend under five children in public health services in the North Wollo Zonal until the end of data collection were the study population.
Inclusion criteria
All mother–child pair aged 6–59 months coming for under five children public health services at the North Wollo Zonal during data collection was included.
Exclusion criteria
Non-biological and mothers who were involuntary, severely ill and unable to communicate were excluded from the study during data collection.
Sample size determination, sampling technique and sampling procedure
The minimum sample size was calculated using a single population proportion formula considering 95 % Confidence Interval (CI), 5 % margin of error, the proportion of colostrum avoidance 13⋅2 %(Reference Tshering, Gurung and Wangmo20), design effect 2 and none response allowance 10 %. Finally, based on the assumptions, the required minimum sample size was taken as 388. A multi-stage sampling technique was employed. The North Wollo Zonal health institutions were selected purposively. The selected zone had a total of six public hospitals and 68 health centres which were stratified into hospitals and health centres. Among the existed zonal health institutions, one hospital and nine health centres were selected randomly with a lottery method. The first patient flow in the preceding 6 months was revised from the ANC registration book to compile the sampling frame. The sample size was then allocated based on population proportional to the size of under five children of each selected health facilities (one hospital and nine health centres) ANC registration book. Finally, the study units were selected from each health facilities ANC registration book by using a simple random sampling method. Data on mother–child pair were collected from mothers by reviewing ANC registration and family folder (for addition information) when they came to the selected facility for healthcare services at under five child healthcare units.
Data collection tool and quality control
The questionnaire was consisting of socio-demographic characteristics, maternal and child healthcare practice. Data were collected using a 10 % of study subjects’ pre-tested interviewer-administered semi-structured questionnaire through a critical review of relevant literature. The questionnaire was prepared first in English and translated into Amharic (the local and national language), then back to English to check for consistency. The Amharic version of the questionnaire was used to collect the data. Eleven master of general public health students who can speak the local language were recruited as data collectors after 2 d training. Informed consent was obtained from all mothers. All women were interviewed personally with the help of a fixed questionnaire, regarding their feeding practices. When mother–child pair found having two or more eligible children, one of them was selected randomly via the lottery method.
Study variable
The dependent variable was colostrum avoidance. The dependent variable was categorised into two: that mother–child pair whom were deprived of colostrum to the infant after delivery coded as ‘1’ and those who received colostrum coded as ‘0’ for regression analysis. The independent variables were maternal characteristics such as age, occupation, educational status, marital status and religion. Household characteristics like family size, household head for decision making and paternal educational status. Obstetric characteristics such as antenatal care (ANC), place of delivery, postnatal care (PNC) and mode of deliver. Child characteristics (sex, age), child feeding practices (colostrum feeding, pre-lacteal feeding, breast-feeding initiation and ever breast-feeding) and child feeding advice at ANC and PNC follow-up.
Data processing and analysis
Data were checked for completeness and inconsistencies. It was also cleaned, coded and entered into Epi data version 4.6.02 software. Then, statistical product and service solutions (SPSS) version 25 was used to analyse the data. Descriptive statistics were estimated for continuous variables while frequency distribution was used to express the distribution of categorical variables and to show the prevalence of colostrum avoidance. Binary logistic regression analysis was performed. The crude odds ratio (COR) with a 95 % CI was estimated to assess the association between each independent variables and colostrum avoidance. Variables with a P-value < 0⋅25 in the binary logistic regression analysis were considered in the multivariable logistic analysis. The Hosmer-Lemeshow goodness-of-fit with enter procedure was used to test for model fitness. Adjusted odds ratio (AOR) with a 95 % CI was estimated to assess the strength of the association. Variables with a P-value < 0⋅05 in the multivariable logistic regression analysis were considered statistically significant and independent predictors of colostrum avoidance.
Ethical approval
The study was approved by the Institutional Review Board (IRB) of Woldia University (Reference number: WDU/IRB/005/20; dated: 12 April 2020). The participants enrolled in the study were informed about the study objectives, expected outcomes, benefits and the risks associated with it. Consent was taken from the participants before the interview and measurement. Confidentiality of responses was maintained throughout the study.
Operational definition
• Colostrum avoidance: This is a dependent variable which was categorised into two, those mother–child pair whom were deprived of colostrum to the infant after delivery coded as ‘1’ and those who received colostrum coded as ‘0’ for regression analysis(Reference Mose, Dheresa and Mengistie11,Reference Gebreyesus, Girma and Cherie18,21) .
• Pre-lacteal feeding: defined as providing foods and/or drink other than human milk for the infant before breast-feeding was established(Reference Bililign, Kumsa and Mulugeta12,Reference Argaw, Asfaw and Ayalew22) .
• Breast-feeding initiation: are the proportion of children born in the last 59 month who were made to breast-feed within 1 h of birth(21,Reference Argaw, Asfaw and Ayalew22) .
Result
Socio-demographic characteristics of study participants
A total of 385 mothers having children aged under 5 years were included in the present study with 99⋅2 % response rate. Nearly two-third 236 (61⋅3 %) were orthodox by religion and almost all respondents 378 (98⋅2 %) belongs to Amhara by ethnicity. The majority of respondents were married 363 (94⋅3 %). More than half 219 (56⋅9 %) of the mothers were found in the age group of 25–34 years. The mean (±sd) age of mothers was 29⋅2 (±6⋅1) and ranged from 15 to 49 years. More than one-third 133 (34⋅5 %) of mothers were illiterate. Nearly one-third 130 (33⋅8 %) of the spouses/husbands of them also did not attend any school for education (Table 1).
Table 1. Socio-demographic characteristics of mother–child pair aged 6–59 months in North Wollo Zone, Amhara Region, Ethiopia, 2021 (n 385)

a Tigray, Oromia.
b Protestant, Muslim.
c Single, divorced and widowed.
d Governmental, NGOs, and daily labour.
Maternal health and child care characteristics
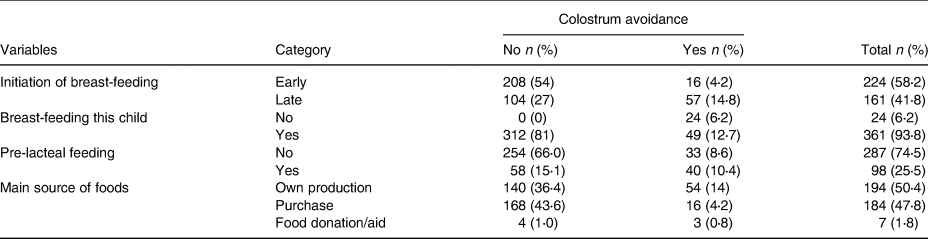
Half of 196 (50⋅9) the mothers attended at least four and above ANC visit but one-tenth 39 (10⋅1 %) of them did not attend ANC follow-up. Of all study participants, one-fourth (20⋅8 %) of mothers were delivered their index child at their home. Regarding about maternal mode of delivery about 34 (8⋅8 %) were caesarean section (Table 2). About 361 (93⋅8 %) children aged 6–59 months were still on breast-feed. About 194 (50⋅4) child got the main source of food was from their own family production. Nearly one-fourth 98 (25⋅5) of children were exposed for pre-lacteal feeding practice (Table 3).
Table 2. Maternal health-related characteristics among mother–child pair aged 6–59 months in North Wollo Zone, Amhara Region, Ethiopia, 2021 (n 385)

Table 3. Child feeding-related characteristics among mother–child pair aged 6–59 months in North Wollo Zone, Amhara Region, Ethiopia, 2021 (n 385)
Prevalence of colostrum avoidance
Colostrum avoidance was 19 % (95 % CI 15⋅03, 22⋅89 %) among mother–child pair aged 6–59 months. From the total of 378 (98⋅2 %) Amhara ethnic group, study participants about 68 (17⋅7 %) were avoid the colostrum. Regarding from Orthodox religious fellow among 236 (61⋅3 %) mother–child pair about one-tenth 42 (10⋅9 %) of them were deprived of colostrum. From the total of 305 (79⋅2), mother–child pair aged 6–59 months attended institutional delivery about 38 (9⋅9 %) avoid colostrum. Among the total, 361 (93⋅8 %) of mother–child pair breast-feed children about 49 (12⋅7 %) were avoid the colostrum. From more than half of 207 (53⋅8), the respondents with four and below family size in the household about one-tenth 39 (10⋅1 %) were avoid the colostrum. Among one-fifth 80 (20⋅8 %) of respondents who delivered at home nearly one-tenth 35 (9⋅1 %) of them were avoid colostrum (Tables 1–3).
Predictor of colostrum avoidance practice
Variables such as mode of delivery, radio, family size and maternal nutritional status were not eligible for colostrum avoidance during the statistical testing process in binary logistic regression analysis. The variables like paternal education, maternal education, maternal age, ANC visit and TV were associated with the dependent variable in the bi-variable regression analysis, but they failed to maintain their association consistently with the dependent variable in the multivariable logistic regression analysis. Finally, the multivariable analysis identified pre-lacteal feeding AOR 3⋅464; 95 % CI (1⋅721, 6⋅973), household decision about child feeding AOR 3⋅585; 95 % CI (1⋅563, 7⋅226), Index child sex AOR 2⋅103; 95 % CI (1⋅015, 4⋅358) and health facility delivery AOR 3⋅033; 95 % CI (1⋅293, 7⋅117) as associated factors for colostrum avoidance (Table 4).
Table 4. Predictors of colostrum avoidance among mother–child pair aged 6–59 months in North Wollo Zone, Amhara Region, Ethiopia, 2021 (n 385)

* P < 0⋅0001, **P < 0⋅001, ***P < 0⋅005, ****P < 0⋅05.
Discussion
Colostrum is still discarded from different parts of the globe particularly in developing country in Ethiopia(Reference Weldesamuel, Atalay and Zemichael14,Reference Gebreyesus, Girma and Cherie18) . The present study was conducted to assess the level of colostrum avoidance and its predictors among mother–child pair aged 6–59 months in North Wollo Zone, Amhara Region, Ethiopia.
It was slightly similar with systematic review and meta-analysis database studies revealed in Motta 20⋅3 %(Reference Tewabe, Mandesh and Gualu23). The finding was almost similar to another study revealed from Bure district 14⋅5 %(Reference Mose, Dheresa and Mengistie11), Gozamen district 22⋅1 %(Reference Azene, Mulunesh and Alamneh24). It was higher than the previous studies revealed from different parts of Ethiopia such as 12 %(Reference Yimer and Liben19), Aksum town 6⋅3 %(Reference Weldesamuel, Atalay and Zemichael14), Bahirdar city 8⋅8 %(Reference Ayalew and Asmare25), Derbretabor 10⋅5 %(Reference Addisu, Melkie and Bezie26) and Kombolcha town 11⋅5 %(Reference Gebreyesus, Girma and Cherie18). Studies conducted in African countries such as Cameroon 11⋅2 %(Reference Tambe, Mimboe and Nchung16) and Bhutan 13⋅2 %(Reference Tshering, Gurung and Wangmo20) had lower colostrum avoidance as compared to this finding.
On the other hand, the present study was lower than other studies revealed from Debre tabor 25⋅6 %(Reference Abie and Goshu13), Afar 76⋅9 %(Reference Gebretsadik and Tkuwab27), Jima Arjo district 27⋅5 %(Reference Tamiru, Belachew and Loha28). It was also lower than outside Ethiopian country such as Rural Pakistan 27⋅9 %(Reference Sohail and Khaliq29), Block RS Pura 76 %(Reference Raina, Mengi and Singh30) and Gujarat India 29⋅5 %(Reference Kakati, Rahman and Borah10). The possible explanation for this observed discrepancy might be the fact that the study population, socio-demographic characteristics, socio-cultural characteristics, study design and different study setting.
According to the present study, place of delivery, breast-feeding initiation, decision making, pre-lacteal feeding and index child sex preferences are predictor variables for colostrum avoidance.
In the present study, regarding factors associated with colostrum avoidance, mothers having late initiation of breast-feeding were 6⋅369 times more likely to discard colostrum as compared with their counterparts. This is consistent with studies revealed in Kombolcha district(Reference Gebreyesus, Girma and Cherie18), pastoralist Afar community(Reference Gebretsadik and Tkuwab27), Bahirdar City(Reference Ayalew and Asmare25). This might be also indicating the presence of poor nutrition-specific intervention mothers who did not get counselling about timely imitation of breast-feeding(Reference Gebreyesus, Girma and Cherie18,Reference Azene, Mulunesh and Alamneh24,Reference Hadona, Weldehawariat and Sorrie31) . It might be also due to the fact that absence of ANC follow-up, poor knowledge(Reference Hadona, Weldehawariat and Sorrie31), elders and or relative advice(Reference Kakati, Rahman and Borah10) and poor attitude(Reference Mose, Dheresa and Mengistie11,Reference Gebreyesus, Girma and Cherie18,Reference Azene, Mulunesh and Alamneh24) .
Mothers attended home deliveries were depriving their children from colostrum feeding more than three times than those who delivered at health institutions. This finding was consistent with studies revealed from Gozamen district(Reference Azene, Mulunesh and Alamneh24), Wolaita Sodo town(Reference Gargamo32), India(Reference Kakati, Rahman and Borah10). This finding was also consistent with studies revealed from the previous study of this area(Reference Yimer and Liben19). This might be due to the fact that lack of receiving ANC counselling about optimal breast-feeding practice(Reference Gebreyesus, Girma and Cherie18,Reference Azene, Mulunesh and Alamneh24,Reference Addisu, Melkie and Bezie26,Reference Gargamo32,Reference Yeshambel Wassie, Atnafu Gebeyehu and Abebe Gelaw33) .
The present study showed that mothers who gave pre-lacteal feeding to their children were 3⋅46 times more likely to discard colostrum as compared with those who had the colostrum for their children. This was supported by studies revealed from Northern parts of Ethiopia(Reference Yimer and Liben19,Reference Azene, Mulunesh and Alamneh24) . The possible explanation might be due to the fact that mothers might not participating in pregnant mothers forum(Reference Gebreyesus, Girma and Cherie18), inadequate follow-up visit for ANC and PNC visit, poor maternal level of information about colostrum(Reference Weldesamuel, Atalay and Zemichael14,Reference Setegn, Belachew and Gerbaba34) .
Paternal household decision about child feeding had 3⋅58 times more likely for discarding colostrum as compared with those who were deciding together both husband and mother to their children feeding practice. This is supported by findings from nationally representative data from Ghana women's participation in household decision-making and higher dietary diversity(Reference Amugsi, Lartey and Kimani-Murage35).
Being female index child had 2⋅1 times more likely for discarding colostrum as compared with those mothers who had children with sex being male. This is supported by different studies revealed from Ethiopia and outside Ethiopia such as Cameroon, India(Reference Tambe, Mimboe and Nchung16). This might be also due to the deep-rooted cultural influences, ethnic background and a range of socio-demographic factors. These were more likely to influence the roles of mothers and fathers in child rearing, feeding and ensuring diversity in parents participating in interventions that will be critical to building a robust evidence base for the role of early feeding practices of both parents(Reference Daniels36).
Limitations of the study
Recall bias about colostrum avoidance was one of the limitations. The lack of qualitative data supplementation especially to explore deep-rooted cultural believes why the community practiced the colostrum avoidance and how to reduce it through targeted participants of mothers, health workers and key influential leaders in the community. It also shares the limitation of cross-sectional study design.
Conclusion
The present study revealed that 19 % of mother–child pair avoids the colostrum. Place of delivery, late breast-feeding initiation, paternal decision-making, pre-lacteal feeding and sex preferences were the most important predictors.
Therefore, it should be strengthening adolescent maternal–infant young child nutrition policy through counselling about the significant role of mothers for optimal child development to curve and correct sex preferences.
The shared household decision about colostrum feeding through the promotion of the free home delivery policy of Ethiopia is significantly important to reduce colostrum avoidance.
Finally, the scientific community should study with a prospective cohort study design including with supplementation of qualitative data to identify other potential independent predictors.
Acknowledgements
We would like to express our deepest gratitude to Woldia University, College of Health Science for ethical clearance. Our great thanks also deserve to our study participants, data collectors, supervisors and language translators for their invaluable contribution to this study.
This was a self-funded (from pocket) research.
The datasets analysed during the present study are available from the corresponding author upon reasonable request.
M. L. L. had conceived and designed the study. M. L. L., N. B. Y. and F. W. F. performed the statistical analysis, involved in the interpretation of findings and manuscript preparation. Finally, all the authors read and approved this manuscript.
All authors declared that they have no competing interests.






