Introduction
Chronic kidney disease (CKD) affects 9⋅1 % of the population worldwide, placing substantial burden on healthcare systems(Reference Hill, Fatoba and Oke1,Reference Webster, Nagler and Morton2) . The development and rapid progression of kidney dysfunction is associated with sub-optimal dietary intake(Reference Lopez-Vargas, Tong and Sureshkumar3). Not only is low diet quality detrimental to CKD, it can also result in poor management of underlying comorbidities like cardiovascular disease, diabetes mellitus and hypertension which can further progress CKD(Reference Lopez-Vargas, Tong and Sureshkumar3,Reference Slattery4) . For these reasons, there is potential for healthful dietary patterns, like the Mediterranean diet, to aid in the prevention and management of CKD(Reference Campbell and Carrero5).
Emerging evidence links a Mediterranean diet with improved cardiometabolic health, glycaemic control and reduced incidence of CKD(Reference Campbell and Carrero5–Reference Estruch, Ros and Salas-Salvadó8). The Mediterranean diet is based on high intake of fruits, vegetables, whole-grain bread and cereals, olive oil, legumes, nuts and seeds; moderate intake of dairy products, egg, seafood, poultry and wine; low intake of red meat and discretionary foods(Reference Simopoulos9). In a multi-centre trial, a Mediterranean diet supplemented with extra-virgin olive oil or nuts was associated with a 31 % lower incidence of major cardiovascular events in people at high cardiovascular risk(Reference Estruch, Ros and Salas-Salvadó8). Moreover, the Mediterranean diet has been associated with lower blood pressure, low-density lipoprotein and higher estimated glomerular filtration rate (eGFR) in people with CKD(Reference Palmer, Maggo and Campbell10). Likewise, adherence to a Mediterranean diet was associated with reduced levels of HbA1c, plasma glucose and insulin in adults with and without type 2 diabetes mellitus(Reference Huo, Du and Xu11,Reference Nordmann, Suter-Zimmermann and Bucher12) . Lastly, a recent prospective cohort study among CKD patients found that those with highest adherence to a Mediterranean diet had a lower adjusted risk for CKD progression(Reference Hu, Coresh and Anderson13). Taken together, a Mediterranean diet seems to be a prudent diet for people at risk of or with CKD, due to its impact on comorbidities, which may contribute to the development or progression of CKD.
The protective effects of a Mediterranean diet may not only be due to the intake of nutrients and foods but also include non-nutrient factors such as psychological, social and physical factors that represent a Mediterranean lifestyle(Reference Bach-Faig, Berry and Lairon14,Reference MacKinnon, Wilkinson and Clarke15) . These factors have been shown to modulate comorbidities associated with CKD and to a lesser extent, CKD and its progression(Reference Ricardo, Anderson and Yang16,Reference Georgousopoulou, Mellor and Naumovski17) . Physical activity is well documented to decrease body weight, blood pressure, low-density lipoprotein and total cholesterol levels(Reference MacKinnon, Wilkinson and Clarke15,Reference Afsar, Siriopol and Aslan18–Reference Patnode, Evans and Senger21) . Moreover, sedentary behaviour and reduced physical activity are associated with an increased risk of CKD, as well as increased mortality and decline in renal function in CKD populations(Reference MacKinnon, Wilkinson and Clarke15,Reference Lynch, White and Owen19) . Socialisation has been identified to be inversely associated with the presence of hypertension(Reference Georgousopoulou, Mellor and Naumovski17) and depression(Reference Sánchez-Villegas, Ruíz-Canela and Gea22). Lastly, conviviality has been associated with healthy weight, improved eating habits and dietary choices(Reference Diolintzi, Panagiotakos and Sidossis23). Taken together, it appears the benefits of a Mediterranean lifestyle are not exclusive to dietary intake; thus, further consideration to its role in the health outcomes and progression of kidney disease in people with non-dialysis dependent CKD is warranted.
The aim of the present study was to investigate the adherence to a Mediterranean lifestyle and its association with cardiometabolic markers and kidney function in people with non-dialysis dependent CKD from a non-Mediterranean country.
Methods
Study design and setting
This cross-sectional observational study was conducted at the Nephrology department of the Sunshine Coast Hospital and Health Service, Queensland, Australia. People with non-dialysis dependent CKD stages 3 to 5 (eGFR ≤60 ml/min/1⋅73 m2) were recruited via convenience sampling. The CKD stage was determined according to the National Kidney Foundation clinical practice guidelines(Reference Stevens and Levin24). The primary outcome was adherence to a Mediterranean lifestyle and secondary outcomes were kidney function and cardiometabolic health. Dependent variables were kidney function (eGFR) and cardiometabolic markers (total cholesterol, LDL-cholesterol, HbA1c, random blood glucose and blood pressure). Independent variables included Mediterranean lifestyle adherence, socioeconomic status, the presence of comorbidities, age, weight and body mass index (BMI). Exclusion criteria included kidney transplant recipients, people receiving dialysis, non-English-speaking individuals, cognitive impairment, pregnancy and current enrolment in another research project. Nil reimbursement or incentives were provided. Participants provided written informed consent prior to inclusion to the study. Ethical approval was obtained from the Prince Charles Hospital Human Research Ethics Committee (HREC/17/QPCH/370) and the University of the Sunshine Coast Human Research Ethics committee (S181179).
Measurements
Height, weight and brachial blood pressure were measured by trained clinical nurses using standard protocols(Reference O'Brien, Asmar and Beilin25,Reference Stewart A and Olds26) during a routine visit at the Nephrology department. BMI was calculated from height and weight measurements and categorised according to the World Health Organisation Criteria (Healthy: BMI ≥ 18⋅5 to <25 kg/m2; Overweight: BMI ≥ 25 to <30 kg/m2; Obese: BMI ≥ 30 kg/m2)(27). The most recent biochemical parameters (taken within the last 6-months), the number of diagnosed comorbidities (including diabetes, cardiovascular disease, hypertension and depression) and medication use were recorded from medical charts.
Questionnaire
Socio-demographic information, source of nutrition information and Mediterranean lifestyle habits were assessed using a self-administered paper-based survey.
Socio-demographic information
Socio-demographic data included age, sex, country of birth, employment, educational attainment, marital status, previous dietetic input and postcode. Employment status and level of education were surrogates for socioeconomic status.
Mediterranean lifestyle habits
The Mediterranean lifestyle (MEDLIFE) index(Reference Sotos-Prieto, Moreno-Franco and Ordovas28) was used to assess adherence to a Mediterranean lifestyle, including diet, physical activity patterns and social interaction. The MEDLIFE index has been validated in a middle-aged Spanish working-class cohort and showed significant association with the Alternate Mediterranean Diet Index and the Mediterranean Diet Adherence Screener(Reference Sotos-Prieto, Moreno-Franco and Ordovas28). The index consists of 28-items which are divided into three blocks, namely (1) food consumption (fifteen items), (2) traditional Mediterranean dietary habits (seven items) and (3) physical activity, rest, social habits and conviviality (six items). In block one, participants self-reported the average number of serves of specific foods and beverages using visual guides on portion sizes which was provided by the research team. Block two and three indicated adherence to Mediterranean dietary and lifestyle habits, respectively. Each item was scored one point if the guideline was met or zero if the guideline was not met, resulting in a total score out of 28. The higher the score, the greater adherence to a Mediterranean lifestyle is.
Sample size estimation
A total sample size of 102 was calculated using G-power(Reference Faul, Erdfelder and Buchner29) with a medium effect size (δ 0⋅50), 80 % power and significance set at P < 0⋅05 to identify differences between two independent groups. A total of 111 participants were recruited between July and September 2020, of which 12 participants did not return their surveys, resulting in a final sample size of 99 (89 % response rate).
Statistical analysis
Data analysis was performed using IBM SPSS statistical software package version 24 (SPSS, Inc., Chicago, IL, USA) and significance set at P < 0⋅05. Descriptive statistics are presented as mean and standard deviation (SD) for parametric variables or median and interquartile range (IQR) for non-parametric variables. Categorical data are presented as frequencies and percentage of the total group. Data were stratified into dichotomous groups according to the median MEDLIFE index score of the cohort (cut-off: ≤11 v. >11). Additionally, participants were stratified based on kidney function, early (stages 3a and 3b) or advanced CKD (stages 4 and 5) to explore differences in socio-demographic and cardiometabolic markers. Differences between groups were determined with independent T-tests for parametric variables, Mann–Whitney U tests for non-parametric variables and χ 2 test for categorical variables. Associations between independent and dependent variables were explored using χ 2 test or Pearson correlations, adjusting for age, gender and weight. Adjusted R-values are reported unless otherwise indicated.
Results
Participant characteristics and cardiometabolic markers
Participant demographics and comorbidities are summarised in Table 1 for the total group, as well as between groups based on the MEDLIFE index score and kidney function. Participants were mostly male, older than 70 years of age, unemployed and the majority obtained either a secondary or tertiary education. Overall, 32⋅6 % were classified as overweight and 50⋅0 % were obese. Most participants presented with two or more comorbidities, with only 7⋅3 % of participants presenting with no comorbidity and 25⋅0 % presenting with one comorbidity. Significant differences were found between systolic blood pressure and a diagnosis of hypertension and/or cancer between those with early CKD compared with advanced CKD.
Table 1. Participant demographics and comorbidities (n 99)
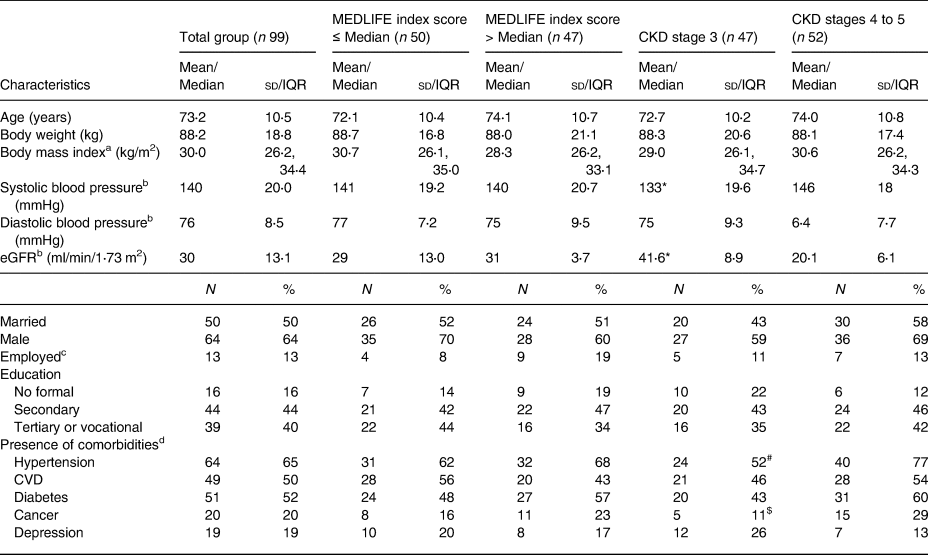
Note. Data presented as mean and standard deviation (SD), median and interquartile range (IQR, 25th; 75th percentile), or frequency and percentage of the total group.
MEDLIFE, Mediterranean lifestyle; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; CVD, cardiovascular disease.
a Data missing for thirteen participants.
b Data missing for one participant.
c Includes full-time, part-time and casual employment.
d Participants presented with multiple comorbidities; values do not add up to 100.
* Significant difference between CKD stage 3 compared with stages 4 and 5, P < 0⋅01.
# χ 2 6⋅599, P = 0⋅01.
$ χ 2 4⋅856, P = 0⋅028.
Table 2 shows biochemistry, MEDLIFE index score and cardiometabolic markers for the group. No significant differences were found for cardiometabolic markers or kidney function between groups according to the median MEDLIFE index score. Significant differences were found in creatinine, potassium, phosphate and triacylglycerols between those with early CKD compared with advanced CKD.
Table 2. Participant biochemistry, cardiometabolic markers and Mediterranean lifestyle index (n 99)
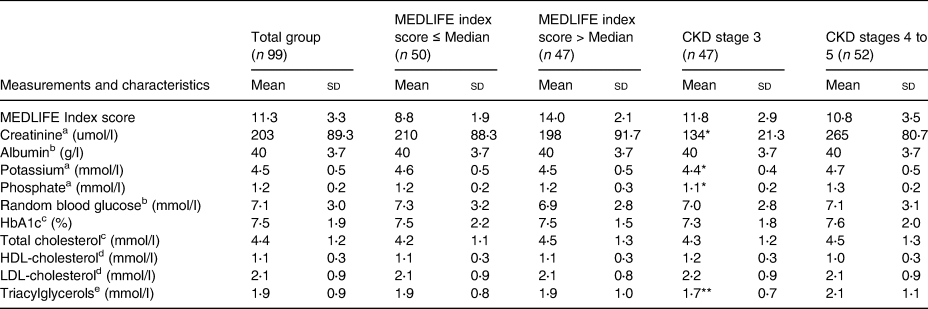
Note. Data presented as mean and standard deviation (SD).
MEDLIFE, Mediterranean lifestyle; CKD, chronic kidney disease; HbA1c, glycated haemoglobin A1C; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
a Data missing for one participant.
b Data missing for three participants.
c Data missing for seven participants, nil readings within 6 months.
d Data missing for forty participants, nil readings within 6 months.
e Data missing for thirteen participants, nil readings within 6 months.
* Significant difference between CKD stage 3 compared with stages 4 and 5, P < 0⋅01.
** Significant difference between CKD stage 3 compared with stages 4 and 5, P < 0⋅05.
The most common source of nutrition information was a dietitian (30⋅3 %), doctor (29⋅3 %), friends or family (29⋅3 %) and the internet or online resources (21⋅2 %).
Mediterranean lifestyle habits
Two participants completed less than 70 % of the MEDLIFE index and were omitted from data analysis. The average MEDLIFE index score for the total group was 11⋅3 ± 3⋅3 (n 97). Table 3 represents the average scores for each block, as well as individual items of the MEDLIFE index.
Table 3. Adherence to a Mediterranean lifestyle, the MEDLIFE index raw scores (n 97)
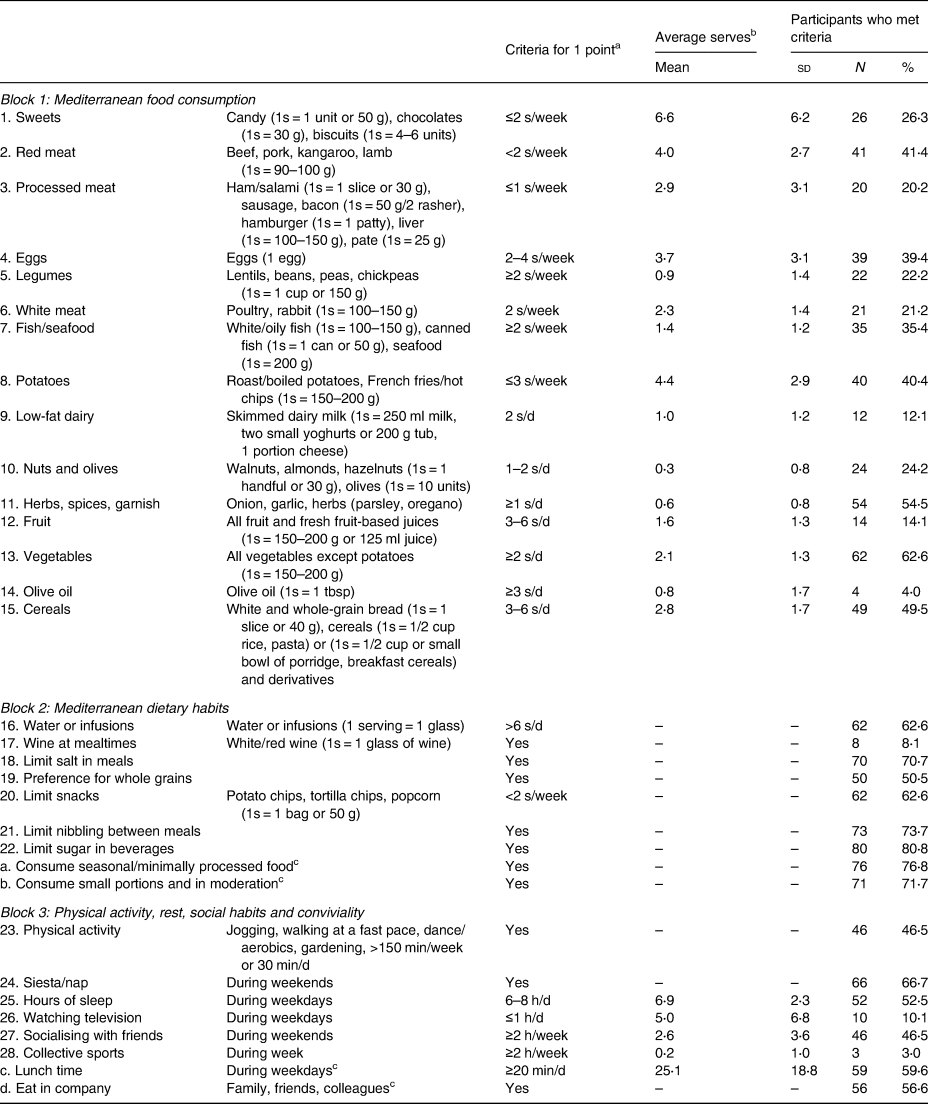
Note. S, serves.
a 0 points if criteria were not met.
b Data presented as mean and standard deviation (SD), or frequency and percentage of the total group.
c Questions denoted with a letter (a, b, c, d) are supplementary questions of the MEDLIFE index and are not included in the final index score.
Considering the recommended cut-offs for Mediterranean food consumption, on average, the number of serves for vegetables was met and most participants used herbs and spices to flavour food. In contrast, the number of serves for pastries, red meat, processed meat and potatoes were in excess, while the number of serves for legumes, low-fat dairy, olive oil, nuts, fruit, fish and seafood were not met. The majority of participants met the criteria for Mediterranean dietary habits with the exception of drinking wine daily at mealtimes. Over half of the participants met criteria for most Mediterranean lifestyle habits, excluding television viewing, participation in team sports or physical activity and socialising with friends.
Correlations
Socio-demographics and Mediterranean lifestyle
The total MEDLIFE index score was associated with employment which remained significant after adjusting for age and gender (r 0⋅30, P = 0⋅004). An association between women and preference to consume fresh, minimally processed and seasonal produce (χ 2 6⋅525, P = 0⋅011), as well as preference to eat in moderation and trying to choose small portions (χ 2 10⋅371, P < 0⋅01) was found. There was an association between men and eating in company (χ 2 6⋅047, P = 0⋅014). Previous dietetic input was associated with consumption of fresh, minimally processed and seasonal produce (χ 2 3⋅670, P = 0⋅055).
Cardiometabolic markers, kidney function and Mediterranean lifestyle
Kidney function was negatively associated with systolic blood pressure which remained significant after adjusting for confounders (r −0⋅32, P = 0⋅002). Kidney function was associated with not receiving nutrition information from the internet or online sources (r 0⋅23, P = 0⋅026).
The total MEDLIFE index score was negatively associated with diastolic blood pressure but lost significance after adjusting for confounders (r −0⋅20, P = 0⋅058). Adherence to limiting sugar in beverages was associated with lower diastolic blood pressure before and after adjusting for confounders (r 0⋅32, P = 0⋅002).
Body weight was negatively associated with HDL-cholesterol (r −0⋅40, P = 0⋅002). Not adhering to consumption of less than two servings of snack foods per week was associated with LDL-cholesterol after adjusting for confounders (r 0⋅41, P = 0⋅002). An association was also found with total cholesterol, but significance was lost after adjusting for confounders (r 0⋅21, P = 0⋅054). Interestingly, preference of minimally processed and seasonal produce and preference to eat in moderation and choosing small portions was inversely associated with total cholesterol after adjusting for confounders (r −0⋅25, P = 0⋅019; r −0⋅22, P = 0⋅04, respectively).
Random plasma glucose was associated with non-adherence to eating in moderation and trying to choose small portions and remained significant after adjusting for confounders (r 0⋅21, P = 0⋅043). In addition, there was an association between participants presenting with diagnosed diabetes and non-adherence to preference to eat in moderation and trying to choose small portions (χ 2 4⋅174, P = 0⋅041). Not adhering to consumption of less than two servings of snack foods per week was associated with HbA1c and remained significant after adjusting for confounders (r 0⋅29, P = 0⋅037).
Interestingly, eating in company was associated with a lower frequency of diagnosed depression (χ 2 5⋅975, P = 0⋅015).
Discussion
The present study aimed to investigate adherence to a Mediterranean lifestyle and its association with cardiometabolic markers and kidney function in people with non-dialysis dependent CKD. Key findings include moderate adherence to a Mediterranean lifestyle, employment was associated with higher adherence to a Mediterranean lifestyle, components of Mediterranean dietary habits were associated with various cardiometabolic markers and those that ate with others had a lower occurrence of depression. No associations between kidney function and a Mediterranean lifestyle were found.
Evidence points toward an association between adherence to a Mediterranean diet, renal function and delayed CKD progression(Reference Campbell and Carrero5,Reference Banerjee, Liu and Crews30) . In a systematic review of nine studies, increased adherence to a Mediterranean diet was significantly associated with a 10 % reduced risk of CKD in community-dwelling adults(Reference Hansrivijit, Oli and Khanal31). Additionally, a cross-sectional study (n 2813) found that greater adherence to a Mediterranean diet was associated with higher eGFR in people with CKD stage 3(Reference Heindel, Baid-Agrawal and Rebholz32). No significant associations were observed between a Mediterranean lifestyle adherence and CKD in the present study. This may be partly explained by the small sample size and the use of different tools to measure adherence to a Mediterranean diet and/or lifestyle. The present study assessed food intake, dietary habits, physical activity and social interaction which differs from the tools used in previous studies (e.g. Mediterranean Diet Score, Mediterranean Diet Adherence Screener, Mediterranean Diet Scale, Short Mediterranean Diet Questionnaire) that predominately focused on food and/or nutrients(Reference Gil, Martinez de Victoria and Olza33). Lifestyle factors such as physical activity and sedentary behaviour may be useful in the prevention of CKD progression as well as comorbidities such as cardiovascular disease which are common among people with CKD(Reference MacKinnon, Wilkinson and Clarke15,Reference Afsar, Siriopol and Aslan18–Reference Aridi, Walker and Roura20) . Therefore, the present study used an a priori index tool that included some of these lifestyle factors. Despite the lack of associations between kidney function and a Mediterranean lifestyle, we did find associations between Mediterranean lifestyle components and cardiometabolic markers which may act to modulate CKD progression(Reference Lee, Lee and Li34). Nevertheless, the role of a Mediterranean lifestyle in the prevention of CKD and CKD progression requires further investigation.
Proposed strategies to attenuate CKD development and progression is to effectively manage risk factors of CKD, including underlying comorbidities like cardiovascular disease, hypertension and diabetes(Reference Ricardo, Anderson and Yang16,Reference Lee, Lee and Li34,Reference Fraser, Roderick and May35) . Our findings demonstrated that adherence to a Mediterranean lifestyle, especially Mediterranean dietary habits, was associated with favourable cardiometabolic health markers. These findings are supported by a meta-analysis of eleven studies(Reference Grosso, Marventano and Yang36) which reported that in non-CKD populations those with the highest adherence to a Mediterranean diet had 24 % lower risk of incident cardiovascular disease and 28 % lower risk of incident coronary heart disease. In agreement, a recent meta-analysis of six trials showed that the Mediterranean diet had positive effects on cardiovascular parameters, including total cholesterol and blood pressure(Reference Nordmann, Suter-Zimmermann and Bucher12). Likewise, a meta-analysis of nine randomised control trials demonstrated that a Mediterranean diet had beneficial effects on weight and cardiovascular risk factors (total cholesterol, triacylglycerols and blood pressure) in people with type 2 diabetes mellitus(Reference Huo, Du and Xu11). Furthermore, a parallel-group, intervention trial that assessed the efficacy of Mediterranean diets on primary cardiovascular prevention (PREDIMED study) among 7447 people, a Mediterranean diet supplemented with extra-virgin olive oil or nuts, was associated with a lower rate of major cardiovascular events (myocardial infarction, stroke or death from cardiovascular causes) compared with a reduced-fat diet(Reference Estruch, Ros and Salas-Salvadó8). Similarly, a cross-sectional study in Australia found that higher adherence to a Mediterranean diet was associated with lower total cholesterol and LDL-cholesterol levels, systolic blood pressure and a lower risk of dyslipidaemia(Reference Aridi, Walker and Roura20). Taken together, a Mediterranean diet is effective to improve cardiovascular health, potentially reducing CKD development and progression(Reference Ricardo, Anderson and Yang16). Notably, the role of dietary habits and other lifestyle factors, such as the physical lifestyle environment, was not assessed. A surprising result from the present study was the unexpected inverse association between total cholesterol and some Mediterranean dietary habits. This may be explained by the potential 6-month lag between the measurement of biochemical parameters and completion of the survey. Furthermore, perhaps individual dietary preferences did not necessarily translate into action.
Interestingly, an association between eating in company and lower presence of depression was identified in the present study. Eating in company represents social support and a sense of community; thus, conviviality of meals may positively affect dietary behaviour and, in turn, health status(Reference Bach-Faig, Berry and Lairon14). In fact, high adherence to a Mediterranean diet and socialisation was associated with a lower risk of developing depression in a prospective cohort study of Spanish adults(Reference Sánchez-Villegas, Ruíz-Canela and Gea22). The present study, therefore, supports the notion that non-nutritional aspects of a Mediterranean lifestyle, such as social and cultural factors, are fundamental to help procure the well-known benefits of a Mediterranean lifestyle.
In the present study, adherence to certain Mediterranean dietary habits was associated with improved glycaemia and a lower frequency of diagnosed type 2 diabetes mellitus. Our findings are in agreement with the body of evidence on the Mediterranean diet and glycaemia(Reference Huo, Du and Xu11,Reference Nordmann, Suter-Zimmermann and Bucher12) . A meta-analysis of nine studies, investigating the effects of a Mediterranean diet on glycaemic control and cardiovascular risk factors, highlighted that adherence was associated with reduced levels of HbA1c, fasting glucose and insulin among patients with type 2 diabetes(Reference Huo, Du and Xu11). Similarly, a meta-analysis of six studies found that a Mediterranean diet had positive effects on plasma glucose in most healthy adults(Reference Nordmann, Suter-Zimmermann and Bucher12). It is concluded that management of type 2 diabetes mellitus may improve with adherence to a Mediterranean diet, thereby slowing renal function decline.
Non-adherence to a Mediterranean lifestyle was observed in the present study. Adherence may be influenced by contextual factors, including the fact that participants were from a non-Mediterranean country, as well as factors relating to food access, food acceptance and socio-cultural norms(Reference Afsar, Siriopol and Aslan18,Reference Minami, Nishi and Fukaya37) . Difficulty adhering to a Mediterranean diet within Australia, with the absence of an intensive intervention, was highlighted in a recent systematic review(Reference Minami, Nishi and Fukaya37). Potential avenues to improve adherence included the translation of key Mediterranean diet principles into the Australian Dietary Guidelines, thus acknowledging socio-cultural norms, sustainability, acceptability and palatability(Reference Minami, Nishi and Fukaya37). Nevertheless, further research is warranted into the transferability of a Mediterranean diet and lifestyle into recommendations for non-dialysis dependent CKD patients from non-Mediterranean countries while maintaining associated health benefits. Employment was also linked with higher adherence to a Mediterranean lifestyle in the present study. Evidence suggests improved health outcomes for older adults that maintain some form of employment status after the age of 65 years(Reference Minami, Nishi and Fukaya37,Reference Staudinger, Finkelstein and Calvo38) . With this in mind, the role of employment in achieving and maintaining a healthier lifestyle in older adults with non-dialysis dependent CKD needs further investigation.
The limitations of the present study include a small sample size, a single centre study and the use of self-reported tools which can result in reporting errors or bias(Reference Kipnis, Subar and Midthune39–Reference Halbesma, Bakker and Jansen41). Furthermore, there was potential for up to a 6-month variance between measured biochemical parameters and data collection within the research study. Due to financial constraints, fasting blood samples could not be taken at the time of the study but were sourced from medical records. Retirement was not recorded, and it was, therefore, not possible to distinguish between unemployment due to retirement or due to inability to secure work. As the majority of participants (71⋅7 %) were 65-years and older, it is possible that many were retired; however, it cannot be assumed. In addition, the cross-sectional nature of the study design precludes conclusions pertaining to causality between a Mediterranean lifestyle, kidney function and cardiometabolic markers(Reference Boushey, Harris and Bruemmer42).
Conclusion
In summary, despite only moderate adherence to a Mediterranean lifestyle, components of a Mediterranean lifestyle were associated with improved health outcomes in this group of people with non-dialysis dependent CKD. The present study extends the body of knowledge by highlighting the potential role of Mediterranean lifestyle factors such as dietary habits, the physical environment and social interaction on cardiometabolic markers, kidney function and/or other health outcomes in people with non-dialysis dependent CKD. Further studies are warranted in larger samples investigating the role of both dietary and non-dietary Mediterranean lifestyle factors in the progression of CKD, as well as factors influencing adherence. In addition, validated tools measuring Mediterranean lifestyle quality, contextualised for people from non-Mediterranean countries, are needed.
Acknowledgements
The authors thank the staff and participants of the Sunshine Coast Hospital and Health Service Renal Outpatient Unit for their significant contribution to this study. The assistance provided by Dr. Benjamin Law for data collection is greatly appreciated. This study was funded by the School of Health and Sport Sciences, University of the Sunshine Coast. In-kind contribution was received from the University of the Sunshine Coast and Sunshine Coast Hospital and Health Service.
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
H. W., L. S. and N. G. identified the research question and study design; K. B. contributed to the study design, formulation of research questions, recruitment, data collection, data analysis and interpretation and wrote the first manuscript draft; H. W. contributed to research questions, data analysis, interpretation and writing of final manuscript; N. G. contributed to research questions, study design and recruitment; All authors read and approved the final version of the manuscript.
The authors declare that they have no relevant financial or personal conflicts of interest.





