Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by
Crossref.
Aragón, Javier
Costa, Clarinda
Coelhoso, Isabel
Mendoza, Gracia
Aguiar-Ricardo, Ana
and
Irusta, Silvia
2019.
Electrospun asymmetric membranes for wound dressing applications.
Materials Science and Engineering: C,
Vol. 103,
Issue. ,
p.
109822.
Genevro, Giovana Maria
Gomes Neto, Reginaldo Jose
Paulo, Letícia de Almeida
Lopes, Patrícia Santos
de Moraes, Mariana Agostini
and
Beppu, Marisa Masumi
2020.
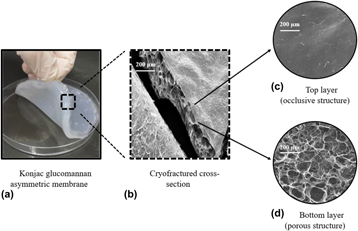
Glucomannan asymmetric membranes for wound dressing–Erratum.
Journal of Materials Research,
Vol. 35,
Issue. 2,
p.
216.
Santos, Nathalia Leal
Ragazzo, Gabriel de Oliveira
Cerri, Bianca Carreiro
Soares, Marcio Roberto
Kieckbusch, Theo Guenter
and
da Silva, Mariana Altenhofen
2020.
Physicochemical properties of konjac glucomannan/alginate films enriched with sugarcane vinasse intended for mulching applications.
International Journal of Biological Macromolecules,
Vol. 165,
Issue. ,
p.
1717.
Stoica, Alexandra Elena
Chircov, Cristina
and
Grumezescu, Alexandru Mihai
2020.
Nanomaterials for Wound Dressings: An Up-to-Date Overview.
Molecules,
Vol. 25,
Issue. 11,
p.
2699.
Mousavi, Seyyed Mojtaba
Zarei, Maryam
Hashemi, Seyyed Alireza
Ramakrishna, Seeram
Chiang, Wei-Hung
Lai, Chin Wei
Gholami, Ahmad
Omidifar, Navid
and
Shokripour, Mansoureh
2020.
Asymmetric Membranes: A Potential Scaffold for Wound Healing Applications.
Symmetry,
Vol. 12,
Issue. 7,
p.
1100.
Yang, Bo
Chen, Yushan
Li, Zhiqiang
Tang, Pengfei
Tang, Youhong
Zhang, Yaping
Nie, Xiaoqing
Fang, Cheng
Li, Xiaodong
and
Zhang, Hongping
2020.
Konjac glucomannan/polyvinyl alcohol nanofibers with enhanced skin healing properties by improving fibrinogen adsorption.
Materials Science and Engineering: C,
Vol. 110,
Issue. ,
p.
110718.
Aderibigbe, Blessing A.
2021.
Modeling and Control of Drug Delivery Systems.
p.
79.
Wegrzynowska-Drzymalska, Katarzyna
Mlynarczyk, Dariusz T.
Chelminiak-Dudkiewicz, Dorota
Kaczmarek, Halina
Goslinski, Tomasz
and
Ziegler-Borowska, Marta
2022.
Chitosan-Gelatin Films Cross-Linked with Dialdehyde Cellulose Nanocrystals as Potential Materials for Wound Dressings.
International Journal of Molecular Sciences,
Vol. 23,
Issue. 17,
p.
9700.
Chiaoprakobkij, Nadda
Seetabhawang, Sutasinee
Okhawilai, Manunya
Uyama, Hiroshi
and
Phisalaphong, Muenduen
2022.
Multifunctional bacterial cellulose-gelatin containing mangosteen extract films with improved antibacterial and anticancer properties.
Cellulose,
Vol. 29,
Issue. 12,
p.
6811.
Khaliq, Touba
Sohail, Muhammad
Minhas, Muhammad Usman
Ahmed Shah, Syed
Jabeen, Nazish
Khan, Shahzeb
Hussain, Zahid
Mahmood, Arshad
Kousar, Mubeen
and
Rashid, Haroon
2022.
Self-crosslinked chitosan/κ-carrageenan-based biomimetic membranes to combat diabetic burn wound infections.
International Journal of Biological Macromolecules,
Vol. 197,
Issue. ,
p.
157.
Zhou, Ning
Zheng, Shengxuan
Xie, Wanzhen
Cao, Guoyu
Wang, Lin
and
Pang, Jie
2022.
Konjac glucomannan: A review of structure, physicochemical properties, and wound dressing applications.
Journal of Applied Polymer Science,
Vol. 139,
Issue. 11,
Yaşayan, Gökçen
Alarçin, Emine
Bal-Öztürk, Ayça
and
Avci-Adali, Meltem
2022.
Bioactive Natural Products.
Vol. 74,
Issue. ,
p.
367.
Yang, Li
Zhao, Quan
Guo, Zhaoyuan
Liu, Yilin
Gao, Wenxia
Pu, Yuji
and
He, Bin
2022.
Konjac glucomannan hydrogel dressing and its combination with Chinese medicine for the wound treatment.
New Journal of Chemistry,
Vol. 46,
Issue. 48,
p.
23077.
Firoozbahr, Meysam
Kingshott, Peter
Palombo, Enzo A.
and
Zaferanloo, Bita
2023.
Recent Advances in Using Natural Antibacterial Additives in Bioactive Wound Dressings.
Pharmaceutics,
Vol. 15,
Issue. 2,
p.
644.
Khaliq, Touba
Sohail, Muhammad
Minhas, Muhammad Usman
Mahmood, Arshad
Munir, Abubakar
Qalawlus, Aya Hamid Mohammad
Jabeen, Nazish
Kousar, Mubeen
and
Anwar, Zobia
2023.
Hyaluronic acid/alginate-based biomimetic hydrogel membranes for accelerated diabetic wound repair.
International Journal of Pharmaceutics,
Vol. 643,
Issue. ,
p.
123244.
Paulino, Larah Gondim Santos
Avila, Luisa Bataglin
Moraes, Caroline Costa
Khan, Mohammad Rizwan
Manoharadas, Salim
dos Reis, Glaydson Simões
Dotto, Guilherme Luiz
and
da Rosa, Gabriela Silveira
2023.
Double-Layer Membranes of Chitosan and Sodium Alginate Added to Natural Olive Leaf Extract for Potential Use in Skin Lesions.
Resources,
Vol. 12,
Issue. 9,
p.
97.
Alves, Rafael Carvalho
Contessa, Camila Ramão
Moraes, Caroline Costa
and
Rosa, Gabriela Silveira da
2023.
Biopolymeric Membranes with Active Principle of Olive Leaves (Olea europaea L.) for Potential Topical Application.
Macromol,
Vol. 3,
Issue. 2,
p.
314.
Lopes, Laise Maia
Germiniani, Luiz Guilherme L.
Rocha Neto, João Batista Maia
Andrade, Patricia Fernanda
da Silveira, Gabriel Augusto T.
Taketa, Thiago Bezerra
Gonçalves, Maria do Carmo
and
Beppu, Marisa Masumi
2023.
Preparation and characterization of porous membranes of glucomannan and silver decorated cellulose nanocrystals for application as biomaterial.
International Journal of Biological Macromolecules,
Vol. 250,
Issue. ,
p.
126236.
Fu, Yijun
Li, Chaowei
Xue, Mengdi
Cao, Youchang
Zhang, Wei
and
Li, Dawei
2023.
Liquid handling properties of carboxymethyl modified chitosan nonwovens for medical dressings.
Journal of Molecular Structure,
Vol. 1292,
Issue. ,
p.
136118.
Ernesto, Julia V.
Severino, Patricia
Venturini, Anna C.
Yoshida, Cristiana M. P.
da Silva, Classius F.
and
Lopes, Patricia S.
2024.
Food Packaging Materials.
p.
233.