Introduction
Benign paroxysmal positional vertigo (BPPV) is the most prevalent episodic vestibular condition encountered in clinical practice.Reference Neuhauser1 It is characterised by recurrent episodes of vertigo lasting less than 1 minute that are induced by changes in head position, especially lying down, turning over in bed, looking up or leaning forward.Reference von Brevern, Bertholon, Brandt, Fife, Imai and Nuti2 Spontaneous remission typically occurs, although the episodes may persist for days, weeks or even months without treatment.Reference Imai, Ito, Takeda, Uno, Matsunaga and Sekine3 It is a recurring disorder, with around 50 per cent of patients experiencing recurrences even after successful treatment.Reference Nunez, Cass, Furman and Holt4,Reference Sfakianaki, Binos, Karkos, Dimas and Psillas5 Although such attacks are usually benign and self-limiting, they impose a significant personal and socioeconomic burden, including risk of falling.Reference Lopez-Escamez, Gamiz, Fernandez-Perez and Gomez-Fiñana6
Guidelines for the diagnosis and treatment of BPPV have been developed by the American Academy of Otolaryngology – Head and Neck Surgery FoundationReference Bhattacharyya, Gubbels, Schwartz, Edlow, El-Kashlan and Fife7 and the Bárány Society.Reference von Brevern, Bertholon, Brandt, Fife, Imai and Nuti2 Different manoeuvres test different semi-circular canals, and the characteristic nystagmus and vertigo associated with each one allows the clinician to determine the affected side, the pathophysiology and, as a result, the best canalith repositioning procedure to perform.Reference Parnes, Agrawal and Atlas8 These canalith repositioning procedures are extremely effective in the treatment of BPPV, often bringing about immediate relief to the patients suffering.Reference Hilton and Pinder9
However, by the time patients present to a vestibular clinic, they are frequently in remission, making the diagnosis impossible to confirm. The clinical practice guidelines recognise the risk of BPPV recurrence and the need to educate patients accordingly.Reference Bhattacharyya, Gubbels, Schwartz, Edlow, El-Kashlan and Fife7 Nevertheless, in real clinical practice, it is unclear how best to achieve this, and considerable practice variations still exist, especially in terms of the availability of follow up. Patients often fear the consequences of a relapse, and this uncertainty can add to the burden of the condition.
In order to address this clear gap in the guidelines, an open access pathway for recurrent BPPV was created, allowing patients to self-refer to the vestibular physiotherapy department if they had a clinical history consistent with positional vertigo, enabling earlier recognition of recurrent BPPV and return for successful canalith repositioning procedures. This study aimed to evaluate the findings of the service. Specifically, we were interested in the recurrence rates, the diagnostic rates at referral and follow up, and the proportion of patients who experienced a recurrence in a different semi-circular canal.
Materials and methods
Participants and setting
The study comprised adult patients (aged at least 18 years) with probable or definite BPPV, who were referred to the Vestibular Physiotherapy Outpatient Department from the Audio-Vestibular Outpatient Clinic at St George's Hospital in London over a four-year period (2018 to November 2022). St George's Hospital is a major trauma centre, and some patients with head injury are also referred directly, when a diagnosis of ‘definite’ BPPV has been made by a physiotherapist on the wards who has received additional vestibular training. All patients consented to be included in the registry.
Design
This is a retrospective service evaluation. Consenting patients with a diagnosis of ‘definite’ or ‘probable’ BPPV were consecutively added to the open access registry. Patients were educated regarding the nature of their condition and the possibility of recurrence. The patients were encouraged to call a direct number to book an appointment if they experienced further positional vertigo. A total of four 30-minute emergency appointments are available, spaced across each week, and typically patients are seen within a couple of days of calling, rarely more than a week. Following each physiotherapy contact, the diagnosis and corresponding semi-circular canal was confirmed and recorded. These patients subsequently underwent treatment for their BPPV (if confirmed), and the total number of treatment sessions was also recorded.
Analysis
The diagnosis of probable or definite BPPV, and the relevant subtypes, were based on the latest Bárány Society criteria,Reference von Brevern, Bertholon, Brandt, Fife, Imai and Nuti2 but no distinction was made between canalithiasis and cupulolithiasis variants. A diagnosis of ‘definite’ BPPV was only given when canal-specific positional nystagmus was observed during diagnostic positional manoeuvres. ‘Probable’ BPPV is diagnosed based on patient history alone, usually during the symptom-free period when diagnostic positional manoeuvre findings are normal.
The data were extracted from the open access registry, which was a password-protected data file. Clinical and demographic data were routinely recorded on the registry by the treating physiotherapist, based on the patient's electronic hospital records. The data collected included: date of birth, sex, referral date and date last seen by physiotherapy, history of head injury or pre-existing vestibular hypofunction, initial involved semi-circular canal, and number of appointments. Complimentary vestibular function testing was not routinely conducted unless a pre-existing disorder of the inner ear was suspected and analysed against normative values for the respective test(s). Data on the number of recurrent episodes of BPPV and the subsequent semi-circular canal involved were also collected. Descriptive data are presented.
Results
In total, 664 patients (76 per cent female), with a mean age of 63 ± 15 years (range of 20–95 years) were referred with a diagnosis of probable or definite BPPV, and were included in the analysis. Table 1 provides the full demographic and clinical characteristics of the sample. Twelve per cent of the patients (n = 76) had a history of head trauma and 20 per cent (n = 130) had a known pre-existing vestibular dysfunction.
Table 1. Demographic and clinical details

SD = standard deviation; BPPV = benign paroxysmal positional vertigo
A total of 310 patients experienced recurrence (47 per cent) and 562 BPPV episodes were recorded. The rate of BPPV recurrence in the total sample was 34 per cent (42 out of 122) in patients with follow up of at least one year, 41 per cent (69 out of 167) for patients with follow up of one to two years, and 53 per cent (199 out of 375) in patients with follow up of two years or more. Of the 322 patients with an initial diagnosis of definite BPPV, the recurrence rate was 58 per cent (n = 186). The median number of BPPV episodes was one (interquartile range = 3). The median number of appointments received per patient was two (interquartile range = 1). On initial referral, 52 per cent of patients (n = 342) had unconfirmed BPPV, of which 36 per cent (n = 124) had a recurrence where it was possible to confirm the diagnosis of definite BPPV (Figure 1).
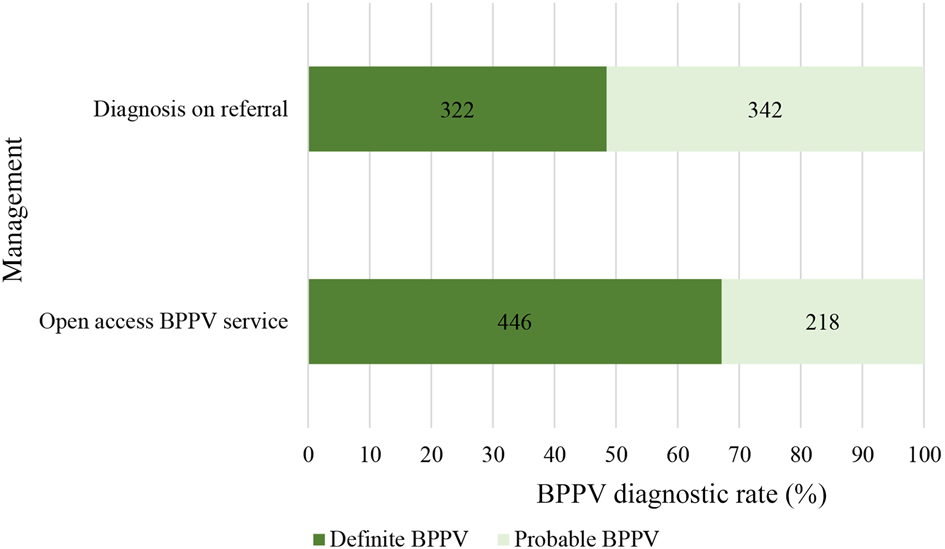
Figure 1. ‘Definite’ versus ‘probable’ benign paroxysmal positional vertigo (BPPV) diagnostic rate.
The most affected semi-circular canal was the posterior canal (87 per cent), followed by the horizontal canal (7 per cent) (Table 1). Multi-canal involvement was observed in 5 per cent of cases. The right side (49 per cent) was more commonly involved than the left (37 per cent). Bilateral involvement was observed in 14 per cent of episodes. For the patients with definite BPPV at follow up (n = 446), 21 per cent (n = 95) had experienced a recurrence in another semi-circular canal at some point, requiring a different canalith repositioning procedure.
Discussion
This service evaluation found that offering open access priority management of recurrent BPPV improved diagnostic rates by around 40 per cent. The recurrence rate for the entire sample was 47 per cent, but ranged from 34 per cent to 53 per cent, increasing with the length of follow up. Those patients with a diagnosis of definite BPPV on referral had the highest rate of recurrence (58 per cent), and one in five patients experienced a recurrence of BPPV in a different semi-circular canal.
Our data reinforce previous studies which found that females are more likely to be affected than malesReference Kim and Zee10 (female: male ratio of 3:1 in this study), with the age of onset most commonly being between the fifth and seventh decades of life.Reference Hornibrook11 Benign paroxysmal positional vertigo predominantly affects the posterior canal,Reference Parnes, Agrawal and Atlas8 followed by the horizontal and multiple canals. Anterior canal/atypical BPPV is rare, and usually warrants further investigation if it does not respond to treatment.Reference Yacovino, Hain and Gualtieri12 Like von Brevern et al.,Reference von Brevern, Seelig, Neuhauser and Lempert13 we found that the right ear is affected more often than the left. Several theories for this laterality have been suggested, such as sleep position, but the precise cause remains unclear.
The improvement in diagnostic rate also supports other authors who advocate for a multidisciplinary approach to BPPV and vestibular disorders generally.Reference Thomas and Newman-Toker14 Over a third of patients with ‘probable’ BPPV went on to have ‘definite’ BPPV confirmed through the direct access service, improving diagnostic rates by around 40 per cent, and reducing the burden on consultant and primary care services.
Small differences observed between other studies can largely be explained by clinical variations. Patients accessing tertiary (specialist) vestibular services in the UK typically wait a long time to be referred, and this may bias the study samples, with the inclusion of more patients who are already experiencing high rates of recurrence. The lower prevalence of horizontal canal BPPV in our sample, for example, could be explained by the finding that horizontal canal BPPV has a higher rate of spontaneous resolution, so perhaps those patients do not seek specialist opinion.Reference Parnes, Agrawal and Atlas8 Although this study did not analyse specific risk factors related to recurrence, the fact that patients with a diagnosis of ‘definite’ BPPV on referral had the highest recurrence rate would be expected, as it is likely that patients with ‘probable’ BPPV reflect some diagnostic uncertainty.
These data nevertheless support a high recurrence rate of BPPV, and suggest that BPPV can be considered a long-term ‘syndrome’ rather than isolated to a particular side and canal.Reference Pérez, Franco, Cuesta, Aldama, Alvarez and Méndez15 Current clinical practice guidelines do not include clear pathways or recommendations for the need to manage BPPV recurrence. There is no single risk factor for recurrence, but rather several, including advanced age, female sex, head trauma, and vascular and other vestibular co-morbidities.Reference Sfakianaki, Binos, Karkos, Dimas and Psillas5 When analysed at the level of the individual patient, this makes it difficult to predict if or when a recurrence will occur.
At present, some clinicians advise management of recurrent BPPV cases with a self-administered canalith repositioning procedure based on the previous type of BPPV identified. That one in five patients with definite BPPV experienced recurrence in a different semi-circular canal has important implications for management. Patients should be educated about this possibility, and about the need to test every canal on both sides to ensure the appropriate canalith repositioning procedure is administered, in order to facilitate effective treatment and resolution of BPPV.
There are other potential advantages to this service. We have found that access to specialist support can help reduce anxiety and intolerance of uncertainty. Early identification of BPPV may therefore reduce the risk of developing secondary functional dizziness and residual symptoms between attacks. We can also identify patients over time who present with BPPV ‘mimics’ and who require further medical investigation, or help patients differentiate symptoms if more than one condition exists (e.g. vestibular migraine vs BPPV).
• Benign paroxysmal positional vertigo (BPPV) is a recurrent episodic vestibular disorder
• The best method to manage future BPPV episodes is not explicitly stated in current guidelines
• Offering open access management of recurrent BPPV improved diagnostic rates by nearly 40 per cent
• One in five recurrences occurred in a different semi-circular canal
• The BPPV recurrence rates were 34, 41 and 53 per cent with follow up of at least one year, one to two years, and two years or more, respectively
The study is limited, as are all studies of this nature, as it lacks the tight control of a clinical trial. The data are a record of only those patients who attended appointments, and thus the study is likely to underestimate the true recurrence rate. This study also covers the coronavirus disease 2019 period, when the service was temporarily closed, and the pandemic may have influenced patients’ willingness to request another appointment. Nevertheless, these real world clinical data are invaluable as they help other clinical services compare and collect real world data, supporting future research.
Conclusion
This study further highlights the importance of assessing each recurrent BPPV episode, to allow an accurate diagnosis in order to establish which semi-circular canal is involved; this is crucial for effective treatment planning. It is therefore important that medical departments which routinely assess patients with suspected or confirmed BPPV consider partnering with allied health professionals. The ability to offer open access physiotherapy assessment and treatment is an effective method for managing recurrent BPPV episodes and, in turn, reducing personal, healthcare and societal burden.
Acknowledgements
We would like to thank the audio-vestibular team and patients at St George's Hospital, London.
Competing interests
None declared




