Introduction
Eustachian tube dysfunction is common. Symptoms may include aural fullness, hearing loss, pain and an inability to equalise middle–ear pressure. Eustachian tube dysfunction is considered a risk factor for several pathologies, such as acute and chronic otitis media, tympanic membrane retraction, and cholesteatoma, all with their associated well-known morbidity and rare mortality.Reference Bluestone1
Risk factors for Eustachian tube dysfunction include sinusitis, smoking and gastroesophageal reflux disease;Reference White, Heavner, Hardy and Prazma2–Reference Arens, Sin, Willen, Bent, Parikh and Freeman5 these are seen in only a portion of patients with Eustachian tube dysfunction. Recently, obstructive sleep apnoea syndrome (OSAS) was identified as an independent risk factor for Eustachian tube dysfunction,Reference Robison, Wilson, Otteson, Chakravorty and Mehta6–Reference Chou, Chang, Lin, Li and Tsou8 although OSAS alone may be a risk factor for sinusitisReference Arens, Sin, Willen, Bent, Parikh and Freeman5 and gastroesophageal reflux disease.
Obstructive sleep apnoea syndrome is characterised by a decrease in airflow (hypopnea) or cessation of breathing (apnoea), resulting from recurrent upper respiratory tract obstruction during sleep, and is frequently observed together with a decrease in oxygen saturation.Reference Patil, Schneider, Schwartz and Smith9 It is the most prevalent organic sleep disorder.Reference Flemons10 Clinical signs of OSAS include snoring, witnessed apnoea and excessive daytime sleepiness.Reference Naëgelé, Thouvard, Pépin, Lévy, Bonnet and Perret11 The majority of patients with OSAS have no detectable respiratory disorder while awake.Reference Collop, Shepard and Strollo12
Negative pressure in the upper airway is ubiquitous in patients with OSAS. This negative pressure results in pharyngeal soft tissue collapse, as can be observed in drug-induced sleep endoscopy. As the middle-ear cleft is an extension of the pharynx, it is possible that the negative pressure disturbs Eustachian tube opening, resulting in Eustachian tube dysfunction. Additionally, OSAS is known to cause: local pharyngeal oedema;Reference Anastassov and Trieger13 an increase of pro-inflammatory factors;Reference Alam, Lewis, Stephens and Baxter14,Reference Ryan and McNicholas15 and a change of pharyngeal connective tissue composition, with a reduction of elastin and an increase of reticular fibres.Reference Dantas, Mauad, Silva, Lorenzi-Filho, Formigoni and Cahali16,Reference Paulsen, Steven, Tsokos, Jungmann, Müller and Verse17
Moderate to severe OSAS may be treated surgically. One of the most common surgical interventions for severe OSAS is expansion sphincter pharyngoplasty. The goal of expansion sphincter pharyngoplasty is to prevent pharyngeal soft tissue collapse and reduce OSAS severity.
This study aimed to compare Eustachian tube function in OSAS patients who are candidates for expansion sphincter pharyngoplasty with controls, and to discuss the possible role of OSAS in the pathogenesis of Eustachian tube dysfunction. A secondary aim was to examine the potential negative impact of the expansion sphincter pharyngoplasty procedure on Eustachian tube function.
Materials and methods
The study was approved by the research ethics committee of a tertiary referral medical centre, and patient consent was obtained. The prospective data collection of all patients hospitalised in our medical centre for drug-induced sleep endoscopy as a part of OSAS evaluation was performed during 2017. Excluded patients included those with an additional otological condition, patients treated with radiotherapy to the head and neck, those with a connective tissue disorder, and patients previously operated on for OSAS.
Eustachian tube dysfunction was diagnosed by history taking and physical examination. It was measured using a Hebrew version of the Eustachian Tube Dysfunction Questionnaire-7, which had previously been validated by the authors.Reference Ungar, Cavel, Golan, Oron, Wasserzug and Handzel18
Each participant answered the Hebrew Eustachian Tube Dysfunction Questionnaire-7 at least once. Patients treated conservatively (with continuous positive airway pressure (CPAP), a dental appliance or weight reduction) answered the questionnaire a month after drug-induced sleep endoscopy via a telephone interview. Patients who underwent expansion sphincter pharyngoplasty answered the questionnaire in pre-set time intervals: the night before surgery (which served as a baseline measurement), the day of nasogastric (NG) tube removal, and on post-operative days 7, 14, 28 and 70.
Patient's height, weight, body mass index, smoking status and apnoea-hypopnea index data were collected and analysed. All results were compared to those of healthy controls, which had been collected for the Hebrew Eustachian Tube Dysfunction Questionnaire-7 validation in 2016.
Statistical methods
Categorical variables were described as frequencies and percentages. Continuous variables were evaluated for normal distribution using histograms and Q-Q plots. Normally distributed categorical variables were expressed as means and standard deviations (SDs), and skewed variables were described as medians and interquartile ranges. The Spearman's rank correlation co-efficient was used to determine associations between continuous variables. The Mann–Whitney test and independent samples t-test were used to compare continuous variables between categories. All the statistical analyses were two-tailed. A p-value of less than 0.05 was considered statistically significant. SPSS software (SPSS Statistics for Windows, version 22.0; IBM, Armonk, New York, USA) was used for all statistical analyses.
Results
Thirty-one patients (19 males, 12 females), with a median age of 43 years (interquartile range = 31–55 years), who underwent expansion sphincter pharyngoplasty for moderate to severe OSAS, were enrolled. The median body mass index (BMI) was 28 kg/m2 (interquartile range = 27–30 kg/m2) and the median apnoea-hypopnea index was 34 events per hour (interquartile range = 25–48 events per hour). Three patients were excluded for loss to follow up.
The pre-operative Eustachian tube function of this cohort was compared to that of a control group. The control group comprised 99 healthy volunteers (males:females = 48:51), with a median age of 55 years (interquartile range = 30–68 years).
Smoking status was similar between the surgical candidates and the controls (Table 1). Median BMI was 23 kg/m2 (interquartile range = 20.5–26 kg/m2). The general population had a significantly lower average Hebrew Eustachian Tube Dysfunction Questionnaire-7 score of 10.25 (SD = 0.8); in comparison, the patient cohort had an average score of 16 (SD = 3.7) (p < 0.05; Figure 1).
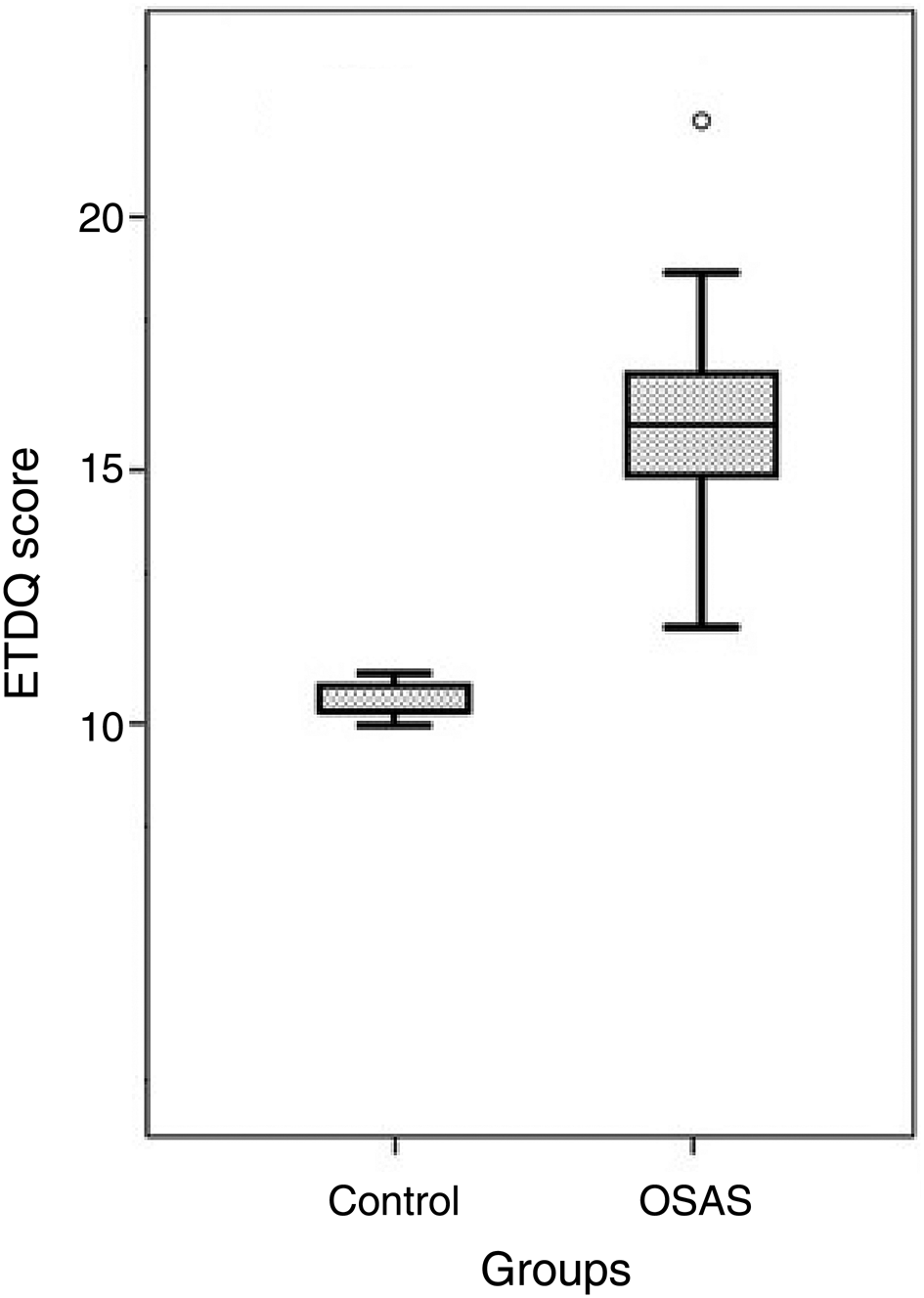
Fig. 1. Eustachian Tube Dysfunction Questionnaire (ETDQ) scores for the obstructive sleep apnoea syndrome (OSAS) patients versus controls (p < 0.05).
Table 1. Demographics and clinical characteristics of the study and control groups

*Body mass index data were available for only 72 of 99 participants in this group. OSAS = obstructive sleep apnoea syndrome; IQR = interquartile range; BMI = body mass index; ETDQ = Eustachian Tube Dysfunction Questionnaire; SD = standard deviation; pre-op = pre-operatively; AHI = apnoea-hypopnea index
Eustachian tube function before and after surgery was investigated (Figure 2). Prior to expansion sphincter pharyngoplasty (baseline measurement), the average Eustachian Tube Dysfunction Questionnaire score was 16 (SD = 3.7). On the day of NG tube removal (usually post-operative day 5–6), the questionnaire score was significantly elevated, at 22 points (SD = 6.9), which was statistically significantly worse than at baseline (Friedman test (chi-square = 122.97, p < 0.001) and Wilcoxon signed-rank test). There was no statistically significant change throughout the following week, through to post-operative day 14, when the scores remained similar. Post-operative days 28 and 70 were characterised by reduced mean questionnaire scores, of 17 (SD = 1.2) and 16 (SD = 1.5), respectively. Hence, the baseline status was reached, with no further improvement (Table 2). There was no significant statistical difference between the baseline Eustachian Tube Dysfunction Questionnaire score and the scores on post-operative days 28 and 70 (p = 0.546 and p = 0.483, respectively).

Fig. 2. Eustachian Tube Dysfunction Questionnaire (ETDQ) scores of expansion sphincter pharyngoplasty candidates as a function of time from operation (p < 0.001). NG = nasogastric; post-op = post-operative
Table 2. Z scores for Eustachian Tube Dysfunction Questionnaire scores as a function of time from operation

NG = nasogastric; post-op = post-operative
There was no significant correlation between age and Eustachian tube function score (p = 0.473). However, significant correlations between BMI, apnoea-hypopnea index and minimal saturation during sleep and Eustachian tube function score were found (p = 0.007, p = 0.021 and p = 0.005, respectively).
Discussion
The pathophysiology of Eustachian tube dysfunction is complex and not completely understood. Dysfunction can be divided into the better known (and more common) dilatory dysfunction and an inability to adequately close the tube's lumen in its resting position, the ‘patulous Eustachian tube’. Dilatory dysfunction is thought to result in an inadequate supply of air to the middle-ear cleft, thereby contributing to the creation of negative pressure in this chamber.Reference Buckingham and Ferrer19 Factors contributing to the pathogenesis of dilatory dysfunction include inadequate peri-tubal muscular activity, congenital malformation such as cleft palate, obstructing masses, chronic and acute inflammation, and surface factors, such as the lack of adequately functioning surfactant.
Eustachian tube dysfunction can result in significant morbidity (and exceedingly rarely in mortality, as a complication of otitis media). Traditionally, treatment was based on circumnavigating the Eustachian tube malfunction by placing a ventilation tube through the tympanic membrane. The advent of balloon Eustachian tuboplastyReference Ockermann, Reineke, Upile, Ebmeyer and Sudhoff20 has allowed for the direct treatment of Eustachian tube dysfunction. Despite these advancements, possible prevention by modifying risk factors could be better utilised.
A number of methods have been developed to measure Eustachian tube dysfunction. Each method has its own merit, but none has been found to be an accurate and clinically relevant tool. McCoul et al. developed the Eustachian Tube Dysfunction Questionnaire;Reference McCoul, Anand and Christos21 its Hebrew version has been validated.Reference Ungar, Cavel, Golan, Oron, Wasserzug and Handzel18 The questionnaire is emerging as an important tool for assessing Eustachian tube function.Reference Van Roeyen, Van de Heyning and Van Rompaey22
Inspiratory and expiratory upper airway resistance values are higher in OSAS patients than in normal subjects, both during wakefulness and sleep.Reference Hudgel23,Reference Anch, Remmers and Bunce24 In individuals with OSAS, airway abnormalities occur both during expiratory and inspiratory phases of ventilation. In order to maintain upper airway patency during inspiration, it appears reasonable that the forces generated by the respiratory pump muscles, which decrease intraluminal upper airway pressure and tend to collapse the airway, should be balanced by dilating forces. The upper airway dilator muscles deliver these dilating forces in normal subjects but fail to do so among OSAS patients.
In candidates for palate surgery due to OSAS, Eustachian tube dysfunction, as measured by the validated Hebrew version of the Eustachian Tube Dysfunction Questionnaire-7, differed significantly from healthy controls. This is a selected group of patients with OSAS severe enough to warrant surgery, with pharyngeal and palatal underlying pathologies. However, others have found an association between obstructive sleep apnoea (OSA) and an increased risk for Eustachian tube dysfunction. Magliulo et al. found that 20 per cent of adults with OSAS had Eustachian tube dysfunction as measured by the Eustachian Tube Dysfunction Questionnaire-7, a metrics combining manometric measurements with additional subjective and objective tools.Reference Magliulo, de Vincentiis, Iannella, Ciofalo, Manno and Pasquariello25 In a population-based study, patients with sleep-disordered breathing had a 1.54-times higher risk for Eustachian tube dysfunction.Reference Pinto, Ribeiro, da Silva Cavallini, Duarte and Freitas26 The Eustachian tube dysfunction prevalence of 32 per cent in infants with OSA is increased compared to the general paediatric prevalence of 4–7 per cent.Reference Robison, Wilson, Otteson, Chakravorty and Mehta6 Sivri et al. found that OSAS treatment with six months of CPAP increased middle-ear pressure,Reference Sivri, Sezen, Akbulut and Coskuner27 although Aksoy et al. found no such change.Reference Aksoy, Serin, Polat, Ünal and Tanyeri28
Several studies have investigated possible mechanisms associating OSAS and Eustachian tube dysfunction. In the paediatric population, it is possible that the relationship between OSA and Eustachian tube dysfunction reflects two different clinical manifestations of a common anatomical abnormality such as adenoid hypertrophy.Reference Robison, Wilson, Otteson, Chakravorty and Mehta6 Adenoid hypertrophy and adenoiditis may then lead to functional obstruction of the nasopharynx, which subsequently leads to OSA and Eustachian tube dysfunction through blockage and inflammation of the nasal airway and Eustachian tube, respectively.
The increased prevalence of Eustachian tube dysfunction in OSA patients promotes the suggestion that any patient being evaluated for OSAS should also be screened for Eustachian tube dysfunction, to help provide more comprehensive care. In the adult population, where adenoid hypertrophy is less common, smoking, rhinosinusitis, allergic rhinitis, gastroesophageal reflux disease and obesity are risk factors for both OSAS and Eustachian tube dysfunction, and may serve as confounders in this setup.Reference White, Heavner, Hardy and Prazma2–Reference Brunworth, Mahboubi, Garg, Johnson, Brandon and Djalilian4,Reference McNicholas, Tarlo, Cole, Zamel, Rutherford and Griffin29–Reference Yasan, Doǧru, Tüz, Çandir, Uygur and Yariktaş31 The effect of these possible confounders on the development of Eustachian tube dysfunction has been analysed previously; it was found that the risk of developing Eustachian tube dysfunction was significantly higher in the OSAS patients, even those without any confounders.Reference Chou, Chang, Lin, Li and Tsou8 Eustachian tube dysfunction has been shown to be more prevalent among OSAS patients than in the general population using several Eustachian tube assessment methods.Reference Magliulo, de Vincentiis, Iannella, Ciofalo, Manno and Pasquariello25 This is possibly because patients with OSA often show severe nasal obstruction, chronic sinusitis, and/or a deficit of nasal mucociliary clearance with nasopharyngeal stagnation of secretions.Reference Robison, Wilson, Otteson, Chakravorty and Mehta6,Reference Pinto, Ribeiro, da Silva Cavallini, Duarte and Freitas26,Reference McNicholas, Tarlo, Cole, Zamel, Rutherford and Griffin29,Reference Olsen, Kern and Westbrook30
The immediate and prolonged impact of conservative interventions (such as CPAP) and surgical procedures (such as expansion sphincter pharyngoplasty) for OSAS, is a subject of controversy in the literature. Because the risk of Eustachian tube dysfunction was found to be increased in patients with OSAS,Reference Robison, Wilson, Otteson, Chakravorty and Mehta6–Reference Chou, Chang, Lin, Li and Tsou8 treatment of OSAS could potentially improve Eustachian tube dysfunction. The possible benefits of OSAS surgery include a reduction in the obstructive pressure of the Eustachian tube, as well as an increase in the normal physiological function of this structure. For example, adenoid enlargement has been reported to not only occlude the nasopharyngeal opening of the Eustachian tube but also to impair mucociliary clearance through fibrotic changes in the neighbouring adenoid tissue.Reference Yasan, Doǧru, Tüz, Çandir, Uygur and Yariktaş31 Additionally, septoplasty and turbinoplasty are associated with improved nasal mucociliary clearance.Reference Polat and Dostbil32,Reference Cassano, Granieri, Del Giudice, Mora, Fiocca-Matthews and Cassano33
• Eustachian tube dysfunction is probably worse among morbid obese adults than controls
• Expansion sphincter pharyngoplasty is not associated with Eustachian tube function improvement
• There is a mild worsening of Eustachian tube dysfunction in the immediate post-operative period
In our study, there was immediate impairment in Eustachian tube function post-operatively, probably due to local oedema, a change in peri-tubal muscular activity, the presence of an NG tube and oral breathing. In addition to their direct effect of Eustachian tube dysfunction, these factors may negatively impact mucociliary clearance. Mucociliary function has been found to differ in patients with OSAS compared to controls.Reference Magliulo, de Vincentiis, Iannella, Ciofalo, Manno and Pasquariello25 From post-operative day 7 to 70, during a 9-week period, there was a gradual but persistent improvement in Eustachian tube function. At post-operative day 70, 10 weeks after the operation, the surgical wound had healed completely, and the Eustachian Tube Dysfunction Questionnaire scores were similar to those pre-operatively. This suggests that, in the long term, expansion sphincter pharyngoplasty had no effect on Eustachian tube dysfunction. A temporary negative effect of OSAS surgery on middle-ear function was observed after palatopharyngoplastyReference Lin, Friedman, Chang, Shao, Pulver and Chen34 and the placement of Pillar® implants.Reference Lin, Friedman, Chang, Lai, Chin and Lin35
Conservative management of OSA included CPAP, among other treatment options (e.g. weight reduction and use of a dental appliance), which is always offered prior to surgical intervention. In our cohort (n = 31), 25 patients (81 per cent) tried using CPAP prior to expansion sphincter pharyngoplasty. Six patients did not try CPAP: three refused a trial, two were unable to appropriately seal the face mask and one suffered claustrophobia. Hence, the majority of pre-operative (basic) Eustachian Tube Dysfunction Questionnaire-7 scores were calculated among active CPAP-using patients. A parallel cohort (n = 43) with moderate to severe OSA patients who efficiently use CPAP with good results (making surgery unnecessary) could not be compared to the surgical cohort, because significant demographic and metabolic (age, gender distribution and BMI) differences were found, and these are likely to be confounders (age and BMI).
This study has two major limitations. One is the relatively small cohort size (31 OSAS patients vs 99 controls). The second limitation, which is common to other studies, is the possible presence of confounders that might be independent risk factors for Eustachian tube dysfunction, such as morbid obesity, gastroesophageal reflux disease and sinusitis, which are more common among OSAS patients than in healthy controls. In addition, tympanometry was not routinely performed in the cohort. Manometry may pose significant discomfort for patients undergoing pharyngopalatal surgery.
Conclusion
Eustachian tube dysfunction, as measured by the Eustachian Tube Dysfunction Questionnaire-7, is worse in candidates for pharyngeal surgery due to OSAS than in controls. Surgery (expansion sphincter pharyngoplasty) is not associated with Eustachian tube function improvement. There is a need to further explore the association between Eustachian tube dysfunction and OSAS in the adult and paediatric populations. The possible presence and contribution of OSAS should be explored in patients with Eustachian tube dysfunction.
Competing interests
None declared






