Introduction
Minimally invasive approaches and endoscopic techniques for frontal sinus pathologies are constantly evolving with advances in technology. Although endoscopic surgery has become an essential tool for modern frontal sinus surgery, open approaches remain pertinent for complex or revision cases. Open frontal sinus surgery in combination with an obliterative procedure is indicated in cases with a narrow anteroposterior diameter of the frontal recess, laterally based lesions, and multiple pneumatised frontal sinus cells or type III and IV frontal cells, as well as in revision surgery or following failure of prior surgery.Reference Kristin, Betz, Stelter, Berghaus and Leunig1
Polymethylmethacrylate, a significant component of acrylic bone cement, has been used in the field of orthopaedics for more than 60 years.Reference Kuehn, Ege and Gopp2 This cement is commonly used for bone reconstruction, filling of bone defects, vertebroplasty, kyphoplasty, cranioplasty, and frontal sinus fractures.Reference Kuehn, Ege and Gopp2
Tutopatch is a biological implant that offers safety, strength, and support for revascularisation and remodelling, while having the property of conforming to anatomical structures, making it suitable for surgical applications (Figure 1).

Fig. 1. Image of Tutopatch.
Several studies have described fat obliteration in frontal sinus mucoceles.Reference Kristin, Betz, Stelter, Berghaus and Leunig1,Reference Mendians and Marks3 However, the use of acrylic bone cement with Tutopatch for the obliteration of frontal sinus mucoceles has not yet been reported. This study aimed to investigate the use of acrylic bone cement with Tutopatch for frontal sinus obliteration performed via an external approach alone, in patients with a frontal sinus mucocele occurring after head trauma, and to evaluate patient satisfaction post-operatively.
Materials and methods
The study group included only those who underwent the external approach (osteoplastic frontal sinus obliteration). Patients who had a recurrent frontal mucocele with no posterior table erosion, and those with anterior table erosion, were excluded from the study.
This study was approved by the local institutional review board (approval number: 509.2020). Written informed consent was obtained from the patients.
This was a prospective study comprising patients with a recurrent frontal sinus mucocele with erosion of the posterior table, registered at the department of otolaryngology at a tertiary care centre, between July 2016 and December 2018.
Surgical procedure
An external incision procedure that was unachievable with the endoscopic approach was planned when frontal sinus mucoceles reoccurred. All surgical procedures were performed after reviewing the patients’ history and physical examination findings, and all patients underwent pre-operative magnetic resonance imaging and computed tomography (Figures 2 and 3).
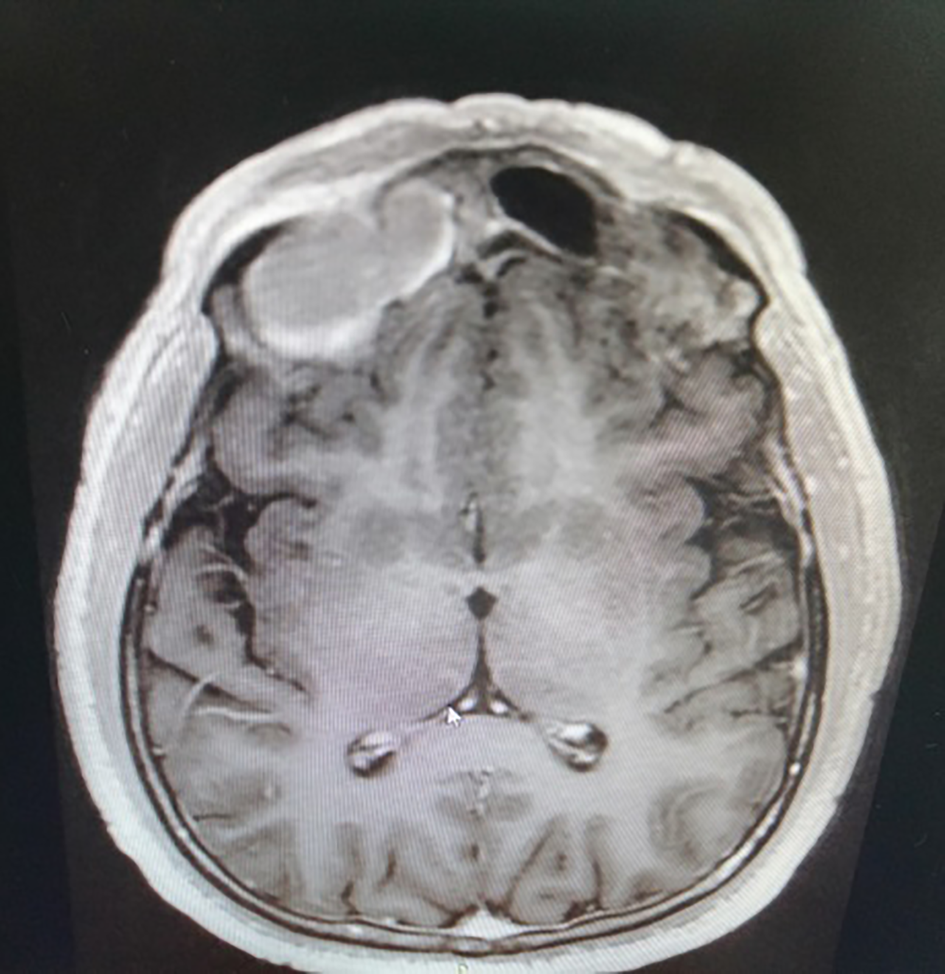
Fig. 2. Axial T2-weighted magnetic resonance imaging scan shows frontal sinus mucocele.

Fig. 3. Axial computed tomography image shows frontal sinus mucocele with posterior table erosion.
Surgery was performed through a bicoronal incision, in the subperiosteal plane, and dissection continued down to the superior orbital rim. Tutopatch was placed between dura and the acrylic bone cement (Figure 4). The frontal sinus mucosa was completely stripped and the sinus obliterated with acrylic bone cement (Figure 5). The cavity and frontal recess was obliterated with acrylic bone cement.

Fig. 4. Intra-operative image showing the obliteration of dura with Tutopatch.

Fig. 5. Intra-operative image of obliteration of frontal sinus mucocele repaired with acrylic bone cement.
The occurrence of potential complications, such as meningitis, cerebrospinal fluid leak, sinusitis, brain abscess, extrusion, mucopyocele, headache, periorbital infection and incision-related problems (alopecia, hypertrophic scars), was determined during the follow-up visit.
Acrylic bone cement
The bone cement pack includes a pouch of 40 g ethylene oxide steriliser powder and one ampoule with 20 ml ultra-filtration-sterilised liquid. The bone cement becomes concentrated in spongy and cortical bones. The active ingredient of bone cement is polymethylmethacrylate; it also contains gentamicin. It has two main components: a liquid monomer and a powdered polymer.
Tutopatch
Tutopatch (Tutogen Medical, Neunkirchen, Germany) is a bovine pericardium graft, which is a type of collagen implant material consisting of a mesh of collagen fibres after the degradable proteins have been removed. Tutopatch undergoes a validated multi-step chemical preservation and sterilisation process that removes antigenic properties and inactivates pathogens. The material's structural properties are well suited for use as a dural graft.
It comes in sheets of uniform thickness and has a good tensile strength with slight elasticity, yet remains supple, and easy to cut, manipulate and suture. Tutopatch promotes rapid revascularisation, repopulation and remodelling. We placed the Tutopatch between the dura and acrylic bone cement to close the open dural defect.
Survey
Visual analogue scales (VAS) were used to subjectively evaluate patient-reported severity of symptoms before and after surgery. A VAS score of 0 to 3 was classified as mild, more than 3 to 7 as moderate, and more than 7 to 10 as severe. The scoring was done on a 10-point scale corresponding to the degree of symptom severity. The lowest score of 1 point reflected no symptom, whereas the highest score of 10 points referred to the highest symptom severity.
Statistical analysis
The paired t-test was used to compare parameters before and after surgery. Statistical analysis was performed using MedCalc Statistical Software version 12.7.7 (MedCalc Software, Ostend, Belgium).
Results
Amongst the 16 patients included in the study, there were 9 men (56.2 per cent) and 7 women (43.8 per cent), with a mean age of 42.6 years (range, 36–48 years). The mean post-operative follow-up duration was 3.2 years (range, 2.3–4.5 years). The VASs for symptom severity were completed before and at one year after surgery. The most common pre-operative symptoms were chronic headache, pressure-like pain in the forehead region, and persistent nasal obstruction.
The average respective VAS scores before and at one year after surgery were 7.2 versus 0.8 for chronic headache, 6.9 versus 0.9 for pressure-like frontal pain, and 5.4 versus 2.4 for persistent nasal obstruction. The score for overall reduction in condition, which assesses the post-operative cosmetic results compared with the pre-operative complaints, was 0.8 points (Table 1). Symptom severity declined after surgery for all symptoms except hyposmia (Table 1). Generally, the patients experienced a subjective improvement in their symptoms.
Table 1. Comparison of patients' pre- and post-operative VAS scores

Data were obtained using visual analogue scales (VASs) of symptom severity: score of 0 to 3 = mild; more than 3 to 7 = moderate; more than 7 to 10 = severe. *Indicates statistical significance (p < 0.05). Pre-op = pre-operative; post-op = post-operative
Some patients had multiple post-operative complications, such as paraesthesia at the incision site (n = 7), scarring (n = 4), inflammation of the incision (n = 2) and alopecia (n = 2). Despite the complications, all patients were satisfied in terms of both the surgical and the post-operative results (Table 2). All patients expressed post-operative satisfaction.
Table 2. Complications of surgery and severity

Data were obtained using a subjective non-standardised questionnaire that included visual analogue scales (VASs) to assess severity of complications: score of 0 to 3 = mild; more than 3 to 7 = moderate; more than 7 to 10 = severe
Discussion
Our study revealed the following novel results: (1) Tutopatch can be used to protect the dura from infections in cases of a recurrent frontal sinus mucocele with erosion of the posterior table; and (2) patients with frontal sinus mucoceles occurring after head trauma were satisfied with the use of acrylic bone cement with Tutopatch for frontal sinus obliterations performed via an external approach alone.
Previous studies have reported patient-based results for frontal sinus obliteration using the osteoblastic flap technique for chronic sinusitis, trauma, neoplasia and mucoceles.Reference Kristin, Betz, Stelter, Berghaus and Leunig1,Reference Mendians and Marks3,Reference Alsarraf, Kriet and Weymuller4 This study investigated post-operative satisfaction in patients with frontal sinus mucoceles specifically with erosion of the posterior tabula, which could not be reached endoscopically. Our results showed that use of acrylic bone cement with Tutopatch was effective in frontal sinus reconstruction when an endoscopic approach was not feasible.
Endoscopic sinus surgery has developed rapidly in recent years and has become a solution for many frontal sinus pathologies.Reference Kristin, Betz, Stelter, Berghaus and Leunig1,Reference Mendians and Marks3,Reference Chen, Wormald, Payne, Gross and Gross5,Reference Banks, Garcia, Grayson, Yeon Cho and Woodworth6 Although endoscopic approaches provide excellent results, the open approach with osteoblastic flap continues to be the saviour in certain cases.Reference Lee, Lee and Lawson7 The modified endoscopic Lothrop procedure can be used for frontal mucoceles. However, if posterior table erosion has occurred, complete removal of the mucosa is very difficult with this approach.Reference Khong, Malhotra, Selva and Wormald8 An osteoblastic flap with obliteration was used for frontal mucoceles with posterior table erosion in this study. Khong et al. support this technique and report that mucosal excision is adequate with open techniques.Reference Khong, Malhotra, Selva and Wormald8
Regardless of the technique, whether obliterative or non-obliterative, the material used for frontal sinus obliteration can determine the results.Reference Ochsner and DelGaudio9 Friedman et al. reported the superiority of hydroxyapatite cement over acrylic bone cement for reconstruction because of its high biocompatibility.Reference Friedman, Costantino, Synderman, Chow and Takagi10 However, Ochsner et al. showed that, irrespective of which bone cement is used for frontal sinus obliteration, infection can occur, which makes revision surgery difficult.Reference Ochsner and DelGaudio9 In our study, infection was not observed in any of the patients during follow up. The possibility of infection was prevented by placing Tutopatch between the dura and the cement.Reference Filippi, Schwarz, Voth, Reisch, Grunert and Perneczky11 Tutopatch used for duraplasty prevented the spread of infections.
In addition to stripping of the mucosa, obliteration of the frontal sinus and nasal cavity is essential. Obliteration of the sinus with fat prevents long-term complications, such as a mucocele.Reference Kristin, Betz, Stelter, Berghaus and Leunig1 The ‘gold standard’ material for frontal sinus obliteration is fat.Reference Kristin, Betz, Stelter, Berghaus and Leunig1 However, Ochsner et al. reported that similar revision rates were observed in patients who underwent obliteration with fat and bone cement.Reference Ochsner and DelGaudio9 Kristin et al. used abdominal fat for frontal sinus obliteration, and reported that 7 of 10 patients complained of temporary pain on the abdominal donor side, soft tissue hardening, pain on palpation and itching lasting for a month.Reference Kristin, Betz, Stelter, Berghaus and Leunig1
The advantages of bone cement over adipose tissue include the absence of such complaints and the ability to obliterate the frontal sinus without a second incision. The additional advantage of acrylic bone cement is its inexpensive cost. Furthermore, no major complications were observed during follow up in the present study. The inclusion of an antibiotic, such as gentamicin, within the acrylic bone cement may also help in preventing infection. Thus, acrylic bone cement used with Tutopatch is a reliable combination for frontal sinus mucoceles with erosion of the posterior table.
• Endoscopic surgery has become essential in modern frontal sinus surgery; however, open approaches remain pertinent for complex or revision cases
• Tutopatch could be used to protect the dura from infection in recurrent frontal sinus mucocele cases with posterior table erosion
• Acrylic bone cement with Tutopatch is a reliable combination for frontal sinus mucoceles with posterior table erosion
Headache, pressure-like pain and nasal obstruction were the main symptoms observed in our study, similar to those reported in previous studies.Reference Kristin, Betz, Stelter, Berghaus and Leunig1 A significant reduction was observed in the average scores of nearly all subjective variables post-operatively (Tables 1 and 2). There was a significant decrease in the intensity of all symptoms except hyposmia. Kristin et al. reported results similar to those of our study.Reference Kristin, Betz, Stelter, Berghaus and Leunig1 Ours is the first study to examine the use of acrylic bone cement combined with Tutopatch, and assess its effect on patient satisfaction. A limitation of the study is the subjective evaluation of the results. Further research, including objective evaluation of the results using standard tests, should be conducted.
Conclusion
Our results indicate that acrylic bone cement combined with Tutopatch can be effectively used in the reconstruction of the frontal sinus in recurrent frontal mucocele cases when an endoscopic approach is not feasible. Further research in this regard is necessary to obtain objective results.
Competing interests
None declared









