Introduction
The term ‘acoustic shock’ is now commonly used in health care. It is a diagnosis predominantly made in individuals employed within the call centre industry.Reference Milhinch, Doyle and Byrne1, Reference Hinke and Brask2 It can be seen quoted on medical certificates from general practitioners, and in reports from audiologists, some industrial health officers, ENT surgeons and, occasionally, psychiatrists.
Acoustic shock has been defined by the Australian Communications Industry Forum as ‘any temporary disturbance of the functioning ear, or nervous symptom, which may be caused to the user of a telephone by a sudden sharp rise in the acoustic pressure produced by it’.3 Acoustic shock may have a variety of origins, including feedback oscillations, fax tones, signalling tones and malicious human shrieks.Reference Dillon and Ching4
An ‘acoustic incident’ has been defined by the Australian Communications Industry Forum as ‘the receipt [by] the telephone user of an often unexpected sound that may cause adverse reaction in some telephone users’.3
‘Acoustic shock injury’ is a term coined by some to explain a cluster of symptoms that may occur after exposure to an acoustic incident, which is usually a brief, loud, unexpected sound.Reference Milhinch, Doyle and Byrne1
The first report of acoustic shock injury came from Denmark in 1999.Reference Hinke and Brask2 The sentinel paper, authored by Milhinch and Doyle in 2000, was a ‘… study which involved examination of case records of 103 call centre operators who experienced an acoustic incidence’.Reference Milhinch, Doyle and Byrne1 These individuals ‘…experienced a wide range of symptoms including pain (81 per cent), tinnitus (50 per cent), vestibular disturbance (48 per cent), [and] hyperacusis (38 per cent)’. Other symptoms comprised ‘headaches and sensations of numbness, burning, tingling, blocking, pressure or fullness, [and] echo or hollow feeling in the ear’. The authors reported that each patient experienced a mean number of 2.7 different symptoms. They concluded that, because of the ‘consistency’ of the reported symptoms, ‘…there is evidence of injury’. Whilst recognising that there may be ‘psychological aspects’, the authors thought that acoustic shock injury was most likely a ‘neurophysiological problem’.
Following this sentinel paper, there have been numerous articles dealing with general descriptions of acoustic shock and hypotheses regarding its pathophysiological basis.Reference Dillon and Ching4–Reference Westcott11 However, only one of these papers described cases and presented audiological findings.Reference Lawton7 Since the publication of Milhinch and Doyle's 2000 paper, acoustic shock has been increasingly diagnosed in Australia, New Zealand, the UK and Denmark. The aim of the present paper is to examine in detail the presentation and medical findings of a group of Australian individuals diagnosed with acoustic shock.
Method
The findings of 16 patients previously diagnosed with acoustic shock, who presented to a medico-legal practice, were reviewed and possible explanations for symptoms considered.
The majority of these patients were told by their general practitioner to stop working with telephones, following advice from an audiologist. This advice was based on the principle that exposure to further noise would delay resolution of symptomatology. Tinnitus retraining therapy and tinnitus maskers were recommended for associated tinnitus, and the use of musicians' earphones was advised for noise sensitivity. Cognitive behavioural therapy was recommended in some cases.Reference Westcott6 Three cases in this series were referred to psychiatrists, and treated with anti-anxiety and anti-depressive medication. No patient was diagnosed with post-traumatic stress disorder or any other major psychiatric illness.
Results
The findings of the 16 cases were analysed. Patients' ages ranged from 29 to 63 years, with a mean age of 43 years. Nine patients were female and seven were male. Twelve cases occurred whilst patients were working in the call centre industry, and four during work in other industries. All patients were diagnosed as suffering from acoustic shock, and all presented to a medico-legal practice between 2005 and 2010.
Twelve of the patients were call centre workers. Three complained of symptoms following a loud noise in their telephone headset during a thunderstorm, five reported a loud noise in their headset of undetermined origin, and four complained of symptoms following exposure to a male voice (Table I). The four non-call centre cases variously involved exposure to a small generator backfiring, a train horn blast, a classroom science experiment explosion, and acoustic feedback in a small auditorium (Table I).
Table I Nature of acoustic incidents

Pts = patients
All patients related their symptoms to their acoustic incident. Eleven stated that their symptoms occurred immediately following the acoustic incident. Four patients reported that the onset of their symptoms was delayed by 1–14 days, and 1 patient reported a delay of several months.
The commonest symptoms were otalgia (n = 12) and tinnitus (n = 11). Patients' descriptions of tinnitus suggested that it was mild to moderate in intensity (i.e. McCombe grade two or three).Reference McCombe, Baguley, Coles, McKenna, McKinney and Windle-Taylor12 Ten patients complained of noise sensitivity and eight of hearing loss. Five patients also complained of headache and five of dizziness. Six patients complained of hearing loss plus tinnitus (Table II).
Table II Symptoms

Pts = patients
Audiometric findings are summarised in Table III. Four patients had normal hearing (age range, 29–41 years; mean age, 33 years). Eight patients had a mild, high-frequency hearing loss (age range, 28–61 years; mean age, 42 years). Four patients had moderate to severe, high-frequency, sensorineural hearing loss (age range, 44–63 years; mean age, 52 years). One of the 16 patients appeared to have a flat, 55 dB, sensorineural hearing loss, which proved to be invalid on Stenger testing and showed normal hearing on cortical evoked response audiometry.Reference Tsiu, Wong and Wong13 Another patient had a profound, unilateral, sensorineural hearing loss; however, the discovery of a pre-injury audiogram revealed that this hearing loss was present prior to the acoustic incident in question.
Table III Audiometric findings

Pts = patients
All audiometry was performed by a qualified audiologist in a sound-treated room. In some cases, audiometry had to be repeated two or three times to obtain consistent audiometric thresholds.Reference Lawton7 Stenger testing was performed in all cases that appeared to have unilateral hearing loss, and cortical evoked response audiometry was performed in cases that had persistently inconsistent audiometric thresholds.
In most patients with audiometric hearing loss, bilateral, symmetrical, high-frequency hearing loss was seen. Six of the patients with this audiometric pattern also complained of tinnitus, which they related to their acoustic incident.
On examination, one patient had small, bilateral attic retraction pockets. He had bilateral, mild, low- and mid-range frequency, conductive hearing loss. Another patient was observed to have subtotal perforation of one tympanic membrane, with severe to profound sensorineural hearing loss in that ear.
Five patients had headaches for which no underlying pathological cause could be found.
Five patients complained of dizziness, described as light-headedness or feeling unsteady. On clinical examination, there were no positive findings to suggest vestibular dysfunction.
Descriptions of eight cases of particular note are given below.
Case one
This case involved a 32-year-old man who described himself as a ‘university dropout’. He had had various jobs before commencing work with the Australian Taxation Office. He had worked there for four years prior to developing symptoms following what he described as ‘an acoustic incident’. This incident occurred when he was talking to a male customer on the telephone. He said that the tone of the voice made him feel ‘uncomfortable’. He swapped the telephone receiver to the opposite ear, but developed pain in both ears, nausea, vomiting and headache. He reported that he did not hear any acoustic shriek.
He stopped work for four weeks and was moved to a different area; however, he said he was still occasionally exposed to ‘acoustic incidents’. He stated that, a year later, hearing his screaming son had caused stabbing pain in his ear, nausea, vomiting and headaches. He took 2 days off work and after returning had required analgesics because of sensitivity to low- and high-frequency noises.
He subsequently sought advice from an audiologist, who diagnosed acoustic shock injury and organised musicians' earplugs and tinnitus retraining therapy. The patient also commenced cognitive behavioural therapy with a psychologist. At the time of evaluation, the patient was taking anti-depressant medication and had not worked for over a year. He said that he experienced pain in the ears when exposed to noise.
The patient had a normal audiometric evaluation and no other findings on clinical examination.
Case two
This 39-year-old man had been employed by the Australian Taxation Office for 18 months when he was exposed to a loud ‘feedback’ noise in his left ear whilst working with a telephone. He described the pain as like ‘someone sticking a knitting needle into my left ear’, and reported that since that time the pain ‘has never gone’. He also complained of hearing a noise in his left ear. He was diagnosed with temporomandibular joint neuralgia and managed with a dental splint worn at night; however, he stated that he chewed through this splint within four months. He complained of noise sensitivity, left tinnitus and intermittent dizziness. He stated that his general health was good apart from depression and obesity. He reported that his ear pain caused his depression and led to over-eating.
Pure tone audiometry showed a bilateral, very mild, high-frequency, sensorineural hearing loss seen only at 6000 and 8000 Hz. The patient complained of pain in his left ear when tested at these frequencies. He called the practice staff several days later stating that his tinnitus had worsened following the audiological evaluation and that the audiometry had been performed incorrectly for his condition (in that it had been performed in a reverse fashion, from suprathreshold down to threshold rather than from subthreshold up to threshold, thus increasing his noise sensitivity problems).
Subsequent photographic evidence showed the patient standing amongst a group of plane watchers at the end of an airport runway, with a Boeing 747 aeroplane visible immediately overhead.
Case three
This patient, a 49-year-old woman, had been working in emergency services telecommunications when she heard a loud noise through her telephone headset whilst taking a call from a member of the police force. She stated that ‘it was hard to hear him, I couldn't hear him’. She said that her team leader told her to get off the telephone, after replaying a tape of the incident. She said that following this incident she felt ‘light-headed, dizzy, nauseated, and was walking funny’. She reported that she rested in a quiet room for a period of time, but she still could not hear in her left ear and had left-sided tinnitus. She complained of left tinnitus ever since this time.
On otological examination, there was little to find apart from a small tympanosclerotic plaque on the left tympanic membrane. The patient winced when a tuning fork was placed 12 cm from the left ear. Pure tone audiometry showed a bilateral, mild, symmetrical, high-frequency, sensorineural hearing loss maximal at 8000 Hz (Figure 1).

Fig. 1 Audiogram for case three, showing bilateral, high-frequency, sensorineural hearing loss, which was the commonest audiometric finding in patients found to have hearing loss.
The patient stated she was fearful of working again in case she experienced a similar incident affecting either ear.
She was seen by a psychiatrist, who diagnosed a mild adjustment disorder, and by two otolaryngologists (for a medico-legal opinion), who diagnosed acoustic shock syndrome.
Case four
This case involved a 50-year-old woman who worked in a call centre for a major telecommunications company. She reported that, whilst attending to an ‘upset customer’ on a ‘bad line’, she heard a noise in the earphone which was ‘continuous and loud’. She was unable to describe the characteristics of the sound apart from saying it was a ‘sharp noise’ coming into her right ear. She was not sure of the duration of the sound, but said she had been speaking to the customer for less than 5 minutes. She said she was eventually told to ‘get off the line’ by her supervisor. The next morning, her right ear was painful and she reported the incident to a team leader. Later, she became aware of a noise in her right ear, accompanied by intermittent, stabbing pain in that ear and noise sensitivity. From that time onwards, she was unable to carry out her normal tasks as a call centre operator.
There was little to find on clinical examination. Pure tone audiometry showed a bilateral, very mild, symmetrical, high-frequency hearing loss maximal at 6000 and 8000 Hz.
The patient was diagnosed by an otolaryngologist, who gave the medico-legal opinion that she was suffering from an ‘acoustic shriek injury’.
Case five
This patient, a 29-year-old woman, had previously worked for the Australian Taxation Office. She stated that, whilst taking a call from a client, she was exposed to 2, approximately 5–10-second noise bursts in the right headset over a 10-minute period. Her description of the noise suggested white noise. She was wearing a telephone headset provided by her employers. She continued to work on her normal duties and reported no issues to her manager at that time. Two weeks later, she approached her manager regarding issues with her right ear, saying she believed these were related to the incident experienced two weeks previously.
Her general practitioner referred her to an audiologist for evaluation. The audiologist advised her to seek advice from another audiologist with a special interest in acoustic shock. The latter audiologist diagnosed acoustic shock injury. The patient was also referred to a psychologist, who diagnosed a long list of problems and recommended that the patient commence a weekly plan of ‘cognitive behavioural therapy, stress and anxiety management, relaxation techniques, and goal planning’. The patient said she had been told by her doctor (the latter of whom was quoting advice from the patient's audiologist) that she should not go back to a call centre environment. The patient also reported that she used a speaker telephone at home and preferred to send ‘text’ messages rather than talk directly on her mobile phone.
On the day of evaluation, the patient carried earplugs with her, which she stated she wore at work and when using public transport as she was unable to tolerate noise. She said she could only work on a telephone for 15 minutes, with the telephone in speaker mode.
Clinical and audiological evaluations were normal.
Case six
This 29-year-old woman had worked in customer services for a major telecommunications company for several years. She reported that, on the day of the acoustic incident, she heard a loud noise in the left telephone headset, which she attributed to a ‘break-up during a storm’. She complained of hearing loss and a persistent ringing sensation, both in the left ear, with left otalgia and pain in the left side of the head, and said she felt slightly unsteady at the time. She was seen by an ENT surgeon who diagnosed left-sided, sensorineural hearing loss and organised a magnetic resonance imaging scan, which was reportedly normal. She was subsequently seen by Australian Hearing Services, who considered fitting the left ear with a hearing aid.
The otological examination was normal. Pure tone audiometry indicated a left, flat, 55 dB, sensorineural hearing loss with consistent audiometric thresholds on retesting (Figure 2). However, the Stenger test was positive at several frequencies. Arrangements were then made for cortical evoked response audiometry, which confirmed the presence of normal hearing in the left ear.
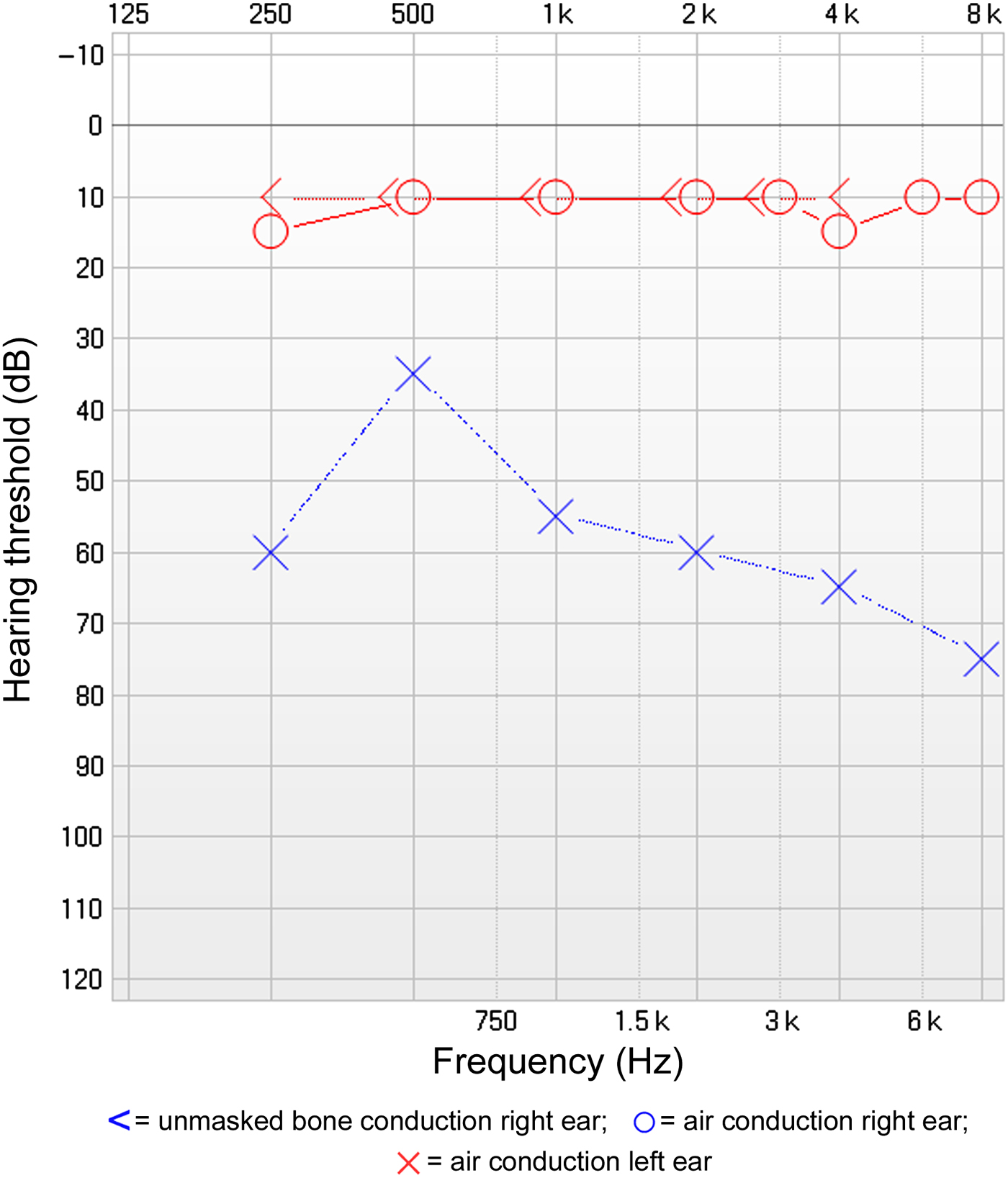
Fig. 2 Audiogram for case six, showing a flat, sensorineural hearing loss with consistent audiometric responses. However, the patient had a positive Stenger test at three separate frequencies and normal cortical evoked response audiometry results.
Case seven
This patient, a 61-year-old woman, had been working as a call centre operator for a large bank. She stated that an incident occurred when she was working on ‘in and out calls’ using a double telephone headset. She was talking with a male customer who was speaking via a mobile phone in his work place. She reported that a loud noise from a machine in the background, heard in addition to the customer's speech, ‘hit me in the ear’. She said she was exposed to this noise for over a minute. She had arranged for the call centre to send a recording of this interview. The recording revealed that she had called the customer whilst he was in a noisy work environment. She had spoken for 25 seconds whilst he was in this noisy environment, until he walked outside to a quiet environment. The interview continued for a further 20 seconds, when it was ended at the customer's request. The patient attended her general practitioner that same day complaining of a blocked sensation in her left ear, left tinnitus and headaches. She went back to work 2 days later, after a weekend break, but was distressed by a noise in the left ear.
The headaches and blocked sensation in the left ear persisted. Ten days later, an audiogram was performed. The patient reported that, immediately prior to audiography, she had experienced a ‘spike up’ in the ear whilst dealing with a customer on the telephone; she described this as a sharp noise. She did not return to work after this experience. She stated that her symptoms were more marked in the left ear because the right earphone of the double headset was ‘not working very well’.
There was little to find on clinical examination. However, pure tone audiometry showed a bilateral, mild, high-frequency, sensorineural hearing loss which was slightly more marked in the left ear than the right.
The patient was diagnosed by her local otolaryngologist as having an acoustic shock injury.
Case eight
This case involved a 41-year-old man employed within a government department. He reported that, whilst preparing a microphone for a Citizenship Day function, feedback occurred on three occasions in an enclosed area. He stated that on the third occasion, the noise caused pain in his ears. He described the duration of the feedback as only a few seconds. Two days later, he noticed sound sensitivity in his ears, particularly to high-pitched noises. He had a hearing test performed at an eye and ear hospital and was told that his hearing was ‘fine’. His treating ENT surgeon sent him back to this same hospital for further audiometric tests. The audiologist at the hospital told him that he had ‘hyperacusis’ related to ‘acoustic shock’. The patient was subsequently referred by his general practitioner to an audiologist with an interest in acoustic shock. This audiologist advised the patient to stop working with telephones as this would worsen his condition.
There were no abnormal findings on clinical examination. Pure tone audiometry (ascending technique) was normal.
The patient had travelled to the evaluation on his motorbike, and stated that he had attended a live concert in a pub two nights previously. He said that he now had no problems with noise exposure, and could use telephones at home and mobile phones. He stated that he was upset by the ‘enforced bureaucracy’ which prevented him from using telephones at work.
This case was one of only two in which symptoms had resolved by the time of evaluation.
Discussion
Although there is a paucity of evidence-based data, it is claimed that acoustic shock costs Australian industry AUD$550 million per year.Reference Groothoff and McMinn8 Trade unions have claimed that this condition has cost the call centre industry billions of dollars. One UK trade union has stated, ‘Acoustic shock is a devastating 21st century industrial injury ruining call centre workers' lives and costing the industry millions’. British Telecom has settled over 700 claims for acoustic shock. The union has stated, ‘Inappropriate protection response and rehabilitation systems have led to litigation in the United Kingdom and call centre workers [have] been awarded substantial amounts of compensation’; one worker received £90 000 compensation for tinnitus related to acoustic shock.14 These estimations of the total cost to industry are derived from websites linked to trade unions, which do not supply itemisation of total costs regarding contributing factors such as absenteeism, job relocation, medical expenses, legal fees and workers' compensation payouts.
In 2004, such claims prompted the UK Government Health and Safety Executive to issue new guidelines on the evaluation of acoustic shock syndrome.15 The previous 2001 guidelines from this organisation stated that ‘An extensive [Health and Safety Executive] study incorporating evidence from 15 call centres in the United Kingdom indicated that call centre workers were not normally exposed to levels that were likely to cause permanent hearing loss’.Reference Patel and Broughton16 The 2004 guidelines stated that, since the Health and Safety Executive had carried out its own research, new evidence had emerged from Australia. In fact, Australia has played a major role in the legitimisation of acoustic shock as a pathological entity. In 2001, a seminar was conducted in Fremantle, Western Australia, entitled Risks in Acoustic Shock. This was followed by a further seminar later that month in Sydney, New South Wales, entitled Beyond Acoustic Shock. Further, related papers were given at an International Congress in Audiology in March 2002 in Melbourne, Victoria.Reference Dillon and Fisher5 Since that time, the diagnoses acoustic shock and acoustic shock injury have been increasingly made in call centre workers in Australia, New Zealand, the UK and Denmark.Reference Hinke and Brask2, Reference Lawton7, Reference Groothoff and McMinn8
The possibility of acoustic trauma to telephone workers has been discussed for many years. In 1969, Glorig et al. reported a study of Californian telephone operating personnel over a 20-year period.Reference Glorig, Whitney, Flanagan and Guttman17 They found no significant hearing threshold shifts, either temporary or permanent. Nevertheless, telephone operators' concerns regarding headset noise exposure persisted. In 1979, Alexander et al. performed audiometry immediately after 51 acoustic disturbances reported by 36 of 129 telephone operators, who had all undergone baseline audiometry.Reference Alexander, Koenig, Cohen and Lepo18 These authors reported no statistically significant difference in mean hearing thresholds at baseline versus immediately after acoustic disturbance, for any frequency. In nine of the assessed incidents, the telephone operator's position was monitored using recording apparatus. Seven of these nine incidents (including two related to reported pain) were associated with signals of 94 dB sound pressure level (SPL) or more (range, 94–105 dB SPL). Alexander et al. stated that a few operators complained of persistent symptoms, and that some showed inconsistencies on later audiometric evaluations. It was felt that the probable cause of these delayed audiometric inconsistencies was ‘functional or volitional interference with the test procedure’. The authors also stated that 2000 random hours of magnetic tape recording of operator positions identified the occurrence of 36 spurious signals of 94 dB SPL or more lasting from 0.4 to 145 seconds. The maximum amplitude recorded was 109 dB SPL.
In the 1980s, there was a series of published case reports of sensorineural hearing loss allegedly resulting from sound levels produced by cordless telephones.Reference Gerling and Jerger19, Reference Orchik, Schmaier, Shea, Emmett, Moretz and Shea20 These reports were predominantly anecdotal, although some included baseline audiometry indicating that the hearing loss may have been a consequence of exposure to noise from the cordless telephone. There were some reported cases of operators being affected by a loud, piercing noise from early model cordless telephones.Reference Orchik, Schmaier, Shea and Moretz21 In these telephones, the ring tone was produced in the ear piece; because of this and the absence of limiters, these cordless telephones produced much higher noise levels (up to 140 dB) than would be experienced by modern telephone headset users, thus causing symptoms more consistent with acoustic trauma. The noise levels produced by a cordless telephone have been measured using a KEMAR® manikin.Reference Van Moorhem, Woo, Liu and Golias22 Gerling and Jerger analysed the ring tone noise levels of three cordless telephones, and reported a maximum level of 140 dB.Reference Gerling and Jerger19
The noise levels experienced by telephone headset users in modern call centres are very different from those experienced by users of cordless telephones. Current noise regulations do not have sufficient bearing on acoustic shock. The sound received through a headset telephone is not loud enough to cause direct damage, in the manner of acoustic blast trauma, as the noise levels involved are always less than 140 dB. Furthermore, modern headsets should have a maximum sound pressure limitation of 118 dB, which is well below the level that will cause damage to the cochlea over a short duration. These noise levels are further reduced by modern volume limiter technology. Volume limiter amplifiers have an upper limit (‘acoustic ceiling’, typically 85–95 dB), beyond which sound levels are automatically reduced. These amplifiers may be powered by batteries so that they are unaffected by power supply problems. More sophisticated headset amplifiers, in addition to having wide band inhibitors, also incorporate narrow band shriek rejection. This technology continuously monitors the incoming signal. When a high-pitched sound occurs, the frequency is measured and the transmission of further sound at this frequency is blocked. Shriek tones are thus detected and blocked within a few hundredths of a second, thus greatly diminishing exposure to acoustic shrieks without affecting speech reception.Reference Dillon and Fisher5
Some have theorised that the symptoms of acoustic shock are the result of excessive contractions of the tensor tympani muscles, precipitated by the startle reflex. This tonic tensor tympani syndrome was first described by Klockhoff.Reference Klockhoff23 Patuzzi,Reference Patuzzi and Ching10 cited in Westcott,Reference Westcott6 stated that tonic tensor tympani syndrome can be induced by the startle reflex, which can be activated by sudden, unexpected sounds at intensities as low as 60 dB.Reference Blumenthal and Goode24 Patuzzi hypothesised that the symptoms of otalgia, tinnitus and a blocked sensation in the ear may be related to this mechanism. Activation of the startle reflex causes spasm of numerous muscles in the upper limbs and neck. Spasms of the masticatory muscles may cause temporomandibular joint neuralgia and explain the symptom of otalgia immediately after an acoustic incident. If a person is anxious prior to the startle stimulus, the magnitude of the startle response is heightened.
Increased awareness of tinnitus could be explained by the Jastreboff model, which states that individuals become more aware of sounds when they are worried that something has gone wrong.Reference Jastreboff and Hazell25 They are likely to focus on those sounds, which tends to amplify them. Hazell stated that this could explain noise sensitivity as well as tinnitus, and postulated that individuals who have reason to focus on their ears, frequently complain of a variety of symptoms some of which may seem bizarre.Reference Hazell, Reich and Vernon26 Kaltenbach, cited in Westcott, hypothesised that non-auditory brainstem structures can be implicated in the control of attention and emotional responses.Reference Westcott11 Kaltenbach believed that neurological structures such as the locus coeruleus, reticular formation and raphe nuclear complex can influence, and be influenced by, the spontaneous activity of the dorsal cochlear nuclei. Based on this mechanism, Kaltenbach hypothesised that hyperactivity of the locus coeruleus contributes to dorsal cochlear nuclei hyperactivity, thus explaining the symptoms of noise sensitivity and tinnitus exacerbation.
Katzenell and Marriage, cited in McFerran and Baguley, suggested that a disturbance of the central auditory serotoninergic pathways may result in altered sound tolerance, and believed that this increased sound sensitivity was also seen in other conditions such as migraine, post-traumatic stress disorder and depression.Reference McFerran and Baguley9 Disturbance of medial efferent system function has also been suggested as another possible cause of hyperacusis, as these fibres are important in monitoring auditory gain.Reference Sahley, Nodar and Musiek27
Although this could account for acute symptomatology seen after exposure to an acoustic incident, they are more problematic as a basis for the chronicity of the symptoms, which are predominantly subjective.
Patients reporting acoustic shock incidents frequently complain of dizziness; however, this is more commonly described as a light-headed ‘woozy sensation’, rather than a hallucination of movement. Nevertheless, Klockhoff and Westerberg considered vertigo in this setting to be of central reticular formation origin because vestibular tests were usually normal.Reference Klockhoff, Westerberg, Arslan, Ricci and Salmon28 These authors also noted that ‘elevated psychic tension seems to be the essential aetiological factor in almost all [such] cases’.Reference Klockhoff and Westerberg29
Patients involved in acoustic shock legal claims, who are often middle-aged and well-educated, seem to have a high incidence of psychiatric and psychological problems. In some cases, a more in-depth history indicates that social issues are a factor. It has been stated that employees who work in call centres are four times more likely than other employees to miss time from work due to psychiatric conditions such as stress and depression.30 It may be difficult to prove that work causes depression, whereas a diagnosis of acoustic shock, attached to the patient's condition by a recognised practitioner, offers a causal link to support a work-related injury claim.30
Notably, call centres have been established in India for nearly 20 years. However, no cases of acoustic shock appear to have been reported, despite the publication of research detailing multiple stress-related problems in Indian call centre workers.Reference Sudhashree, Rohith and Shrinivas31
All of the symptoms described in cases of acoustic shock are subjective and, apart from hearing loss, impossible to quantify. Some cases are clearly due to malingering; patients feigning a hearing loss following an acoustic incident are particularly obvious, although often surprisingly consistent in their audiometric responses (see Figure 2). Stenger testing should be performed in all patients purporting to have unilateral hearing loss. Cortical evoked response audiometry is a valuable tool in validating audiometric thresholds.Reference Tsiu, Wong and Wong13 Some patients claiming noise sensitivity stretch credulity, and their cases can be proven invalid on observation. In the current series, 5 cases had a delay ranging from 1 day to 2 weeks between the acoustic incident and the onset of symptoms; this tends to mitigate against a pathophysiological basis of symptomatology. The symptom of tinnitus is by nature subjective and impossible to quantify; in patients who are making a work-related legal claim, the possibility of exaggeration should be considered.Reference Lawton7 In the present series, tinnitus was not a major complaint (being quantified as McCombe grade two or three, following McCombe and colleagues' grading system).Reference McCombe, Baguley, Coles, McKenna, McKinney and Windle-Taylor12 The majority of patients in the current series who complained of tinnitus had a bilateral, symmetrical, sensorineural hearing loss.
There is evidence of clusters of reported acoustic shock events in settings where there is awareness of the condition (e.g. call centres), suggesting that hysteria may also be a factor. In a Danish study of reports of acoustic shock in 14 call centres, some of the call centres reported no incidents, but one reported that 22 per cent of its 90 call workers had experienced acoustic shock.Reference Hinke and Brask2 In 2003, several workers in the same telecommunications call centre in Brisbane, Queensland, complained of nausea and dizziness following a power surge during an electrical storm. This is reminiscent of the 2005 ‘gas incident’ at a Melbourne Airport terminal, which kept the ambulance service busy for hours and closed the terminal for 2 days, costing millions of dollars.Reference Bartholomew32 Notably, prior to the 1998 DanishReference Hinke and Brask2 and 2000 AustralianReference Milhinch, Doyle and Byrne1 acoustic shock reports, there appear to be no published reports of similar symptoms in telephone industry workers, despite manual telephone exchanges being commonplace for many years.
Conclusion
It appears that work pressures and poor job satisfaction contribute to the outcome of patients reporting acoustic shock. Medical issues are also important; some patients believe they have sustained major underlying injuries, and may believe that avoidance will aid recovery or prevent recurrence of the problem. Medical ambiguities in the information on and management of this problem may prolong symptomatology and contribute to poor outcome.
Unfortunately, modern sound limiting technology and changes in call centre design and operation (including staff training in appropriate equipment usage) have not reduced the incidence of the problem. In fact, the current protocols of incident reporting and awareness of the condition may contribute to consolidation of symptomatology.
The relatively short duration of noise exposure, which in most cases involves sound levels that do not exceed statutory limits, together with variation in the onset of symptomatology, suggest that the condition is psychogenic. Cases of pseudohypacusis indicate that malingering is sometimes a factor.
Acoustic shock is usually only reported when there are work-related issues.30 Medical management is important. All affected individuals should have their full, detailed history recorded, and should undergo otological examination and audiological evaluation performed by a sympathetic practitioner. Patients should then be reassured that they have not sustained a major injury and that returning to work will not be detrimental to their prognosis. Should symptoms persist, an evaluation of possible workplace-related issues by a psychologist is appropriate. There may be a place for psychological intervention and a desensitisation programme. A psychiatric referral may be indicated in some cases.







