Introduction
Social insurance (SI) is a specific social protection model based on membership, social contributions and solidarity principles. First formally introduced in the 1880s in Germany, the SI model has developed into one main type of social protection in social policy fields such as pensions, accident insurance and health care (see, eg. International Labour Organization (ILO), 2017; Schmid et al., Reference Schmid, De Carvalho, Basilicata and Rothgang2021). More recently, some countries have also opted for introducing SI schemes specifically for long-term care (LTC), which constitutes a comparably novel field of social policy making (Österle & Rothgang, Reference Österle, Rothgang, Béland, Morgan, Obinger and Pierson2021, p. 525). Following the System of Health Accounts set out by the Organisation for Economic Co-operation and Development (OECD), the World Health Organization (WHO) and Eurostat (2011), LTC can be defined as “a range of medical, personal care and assistance services […] for people with a degree of long-term dependency, assisting them with their personal care (through help for activities of daily living, ADL, such as eating, washing and dressing) and assisting them to live independently (through help for instrumental activities of daily living, IADL, such as cooking, shopping and managing finances)” (Organisation for Economic Co-operation and Development, 2021b). While the need for LTC can in principle arise at any point during the life course, the prevalence of LTC dependency is clearly and highly associated with (very) old age (Colombo et al., Reference Colombo, Llena-Nozal, Mercier and Tjadens2011, pp. 40–41). Thus – in the light of demographic ageing and other societal changes which reduce the supply of informal caregiving – in the last decades many countries have engaged in drafting and reforming social protection systems for LTC in various forms.
In contrast to the majority of tax-funded, state-regulated public LTC systems existing, in diverse form and scope, for instance, in Scandinavian countries, Australia, Spain or Uruguay, social long-term care insurance (SLTCI) systems are based on entitlements in exchange for (mandatory, often earnings-related) membership contributions (Campbell, Reference Campbell, Conrad and Lützeler2002; Colombo et al., Reference Colombo, Llena-Nozal, Mercier and Tjadens2011, p. 220). By establishing a separate SI branch in the social security system, countries with an SLTCI system treat LTC as a truly distinct social risk. This makes them a particular interesting case to study if we want to learn more about the ways and reasons LTC is developing into a social policy field of its own. Even if only a small number of countries have so far introduced SLTCI schemes, this is quite remarkable in light of the traditional low institutionalisation of LTC as a social policy (Ranci & Pavolini, Reference Ranci and Pavolini2015, p. 271). Consequently, interest in SLTCI schemes is high: A number of country studies have analysed the design, politics and effects of particular SLTCI systems (eg. Borowski & Schmid, Reference Borowski and Schmid2001; Campbell, Reference Campbell, Conrad and Lützeler2002; Maags, Reference Maags2020; Rhee, Done, & Anderson, Reference Rhee, Done and Anderson2015; see also Chen, Zhang, & Xu, Reference Chen, Zhang and Xu2020). However, so far there is little research with a broader comparative perspective on what constitutes SLTCI as a model of social protection for LTC as such, both empirically and conceptually. Which characteristics from the social (health) insurance literature do SLTCI systems conform to? What are the main features of “real-world” SLTCI schemes? How and to what extend do they differ from each other?
Addressing these questions, the present article analyses the original and present configurations of all six globally introduced national-level SLTCI systems, covering the schemes in the Netherlands, Israel, Germany, Japan, Luxembourg and the Republic of Korea (hereafter South Korea). In doing so, we aim to achieve a more comprehensive understanding of the SLTCI model, laying a foundation for both explaining SLTCI variation and assessing LTC system performance. Furthermore, from a more practical perspective, a comparative mapping of existing schemes can inform policy design possibilities for future SLTCI introductions and reforms. This is of particular relevance as, in the wake of global demographic ageing, the need for assistance with daily living following from care dependency will likely continue to increase substantially, arguably necessitating the establishment of novel social protection systems for LTC worldwide (ILO, 2017, pp. 108–109; WHO, 2015, p. 129).
Building on the concept of the “care diamond”, the present article employs an actor-centred framework to compare systematically who – the state, societal actors, private for-profit actors or private individual actors – bears how much responsibility in each SLTCI scheme (see also Fischer, Frisina Doetter, & Rothgang, Reference Fischer, Frisina Doetter and Rothgang2022; Lyon & Glucksmann, Reference Lyon and Glucksmann2008; Ochiai, Reference Ochiai2009; Razavi, Reference Razavi2007). While this conceptual focus can by no means capture each and every feature of an LTC system, it provides crucial insight into the societal organisation of care relations. As actors’ involvement might substantially vary across the different dimensions of LTC systems (Barr, Reference Barr2012, pp. 72–74; Wendt, Frisina, & Rothgang, Reference Wendt, Frisina and Rothgang2009), care diamonds are drafted and analysed separately for SLTCI financing, provision and regulation in each of the six countries. To allow for a systematic comparison of the actor types’ relevance across cases, we employ fuzzy-set analysis for coding the collected data about the schemes into standardised scores.
The remainder of the article starts by reviewing the extant research on SLTIC and briefly summarising the characteristics of SI in general. Subsequently, the six studied cases of national-level SLTCI schemes are introduced. The following sections, firstly, introduce the actor-centred, multi-dimensional conceptual framework and, secondly, the research design and methods which are employed for comparing the SLTCI configurations. Afterwards, the resulting care diamonds for SLTCI financing, provision and regulation are depicted and described in detail. The subsequent discussion outlines the main characteristics of the SLTCI model and considers some potential factors with could explain the differences discovered between schemes. The concluding section reflects on limitations and open questions.
Research on SLTCI
Being a rather recent policy field of its own, country-comparative LTC research has mainly developed since the 1990s. Seminal early contributions which compare European countries based on their respective (child and elder) care arrangements such as Anttonen and Sipilä’s (Reference Anttonen and Sipilä1996) and Bettio and Plantenga’s (Reference Bettio and Plantenga2004) classifications as well as conceptual work on social care, for instance by Daly (Reference Daly2002) and Daly and Lewis (Reference Daly and Lewis2000), have importantly paved the way for studies on LTC in comparative welfare policy scholarship. To date, there exist multiple single, small- and medium-n studies of LTC systems analysing the features of introduced policies and reform trajectories in Europe and Asia as well as multiple LTC typologies (for recent reviews, see eg. Ariaans, Linden, & Wendt, Reference Ariaans, Linden and Wendt2021; Fischer, Frisina Doetter, & Rothgang, Reference Fischer, Frisina Doetter and Rothgang2022). Important institutional features and developments which have received plenty of scholarly attention in the last two decades are, among others, cash-for-care benefits (eg. Da Roit & Le Bihan, Reference Da Roit and Le Bihan2010; Riedel & Kraus, Reference Riedel and Kraus2016) and marketisation trends in LTC systems (eg. Brennan et al., Reference Brennan, Cass, Himmelweit and Szebehely2012; Theobald et al., Reference Theobald, Szebehely, Saito and Ishiguro2018). In contrast, while SLTCI is commonly mentioned in comparative LTC research, there is yet neither an in-depth discussion of the model’s specific characteristics nor a broader empirical comparison available as the following review indicates.
In comparative studies on LTC, SI (sometimes also called “public insurance”) is commonly introduced as one particular (funding) model for LTC, usually followed by a brief outline of (dis)advantages of the scheme and/or case examples (eg. Colombo et al., Reference Colombo, Llena-Nozal, Mercier and Tjadens2011, pp. 220–222; Joshua, Reference Joshua2017; Scheil-Adlung, Reference Scheil-Adlung2015). Furthermore, there is a body of literature dealing with the (economic) evaluation of SLTCI (Barr, Reference Barr2012, p. 143; see also Eling & Ghavibazoo, Reference Eling and Ghavibazoo2019). As regards the empirical instances of SLTCI, there seems to be no clear consensus in the LTC literature on which countries should be addressed under this label, and a discussion of definitions and criteria is mostly absent. While Germany, Japan and South Korea’s SLTCI schemes are usually undisputed and frequently studied (Chen, Zhang, & Xu, Reference Chen, Zhang and Xu2020, p. 7), the SLTCI label has also been attached to a number of diverse LTC systems including Austria, France, Luxembourg, the Netherlands, Taiwan and the United States (see, eg. Chen, Zhang, & Xu, Reference Chen, Zhang and Xu2020; Colombo et al., Reference Colombo, Llena-Nozal, Mercier and Tjadens2011; De Roo, Chambaud, & Güntert, Reference de Roo, Chambaud, Güntert, Saltman, Busse and Figueras2004; Maags, Reference Maags2020).
Besides a large number of single-case studies on SLTCI systems in individual countries, there are some small-n comparative analyses focusing on the features of the respective systems and/or the politics of introduction and reform. A systematic comparison of three SLTCI schemes’ characteristics such as financing and eligibility is provided by Maags (Reference Maags2020) and Rhee, Done, and Anderson (Reference Rhee, Done and Anderson2015). Furthermore, several comparative case studies investigate why SLTCI schemes were introduced and took on a certain form, most notably for the cases of Japan and Germany (eg. Campbell, Reference Campbell, Conrad and Lützeler2002; Campbell, Ikegami, & Kwon, Reference Campbell, Ikegami and Kwon2009; Maags, Reference Maags2020; Morel, Reference Morel, Bonoli and Armingeon2006; Theobald & Kern, Reference Theobald and Kern2011). Overall, the literature agrees that an interplay of theoretical approaches and concrete factors is best suited for explaining the establishment and design of the systems. Besides the important role played by a variety of domestic political and societal actors and events in each individual case, the significance of existing institutional structures, international policy transfer and timing is particularly stressed in these studies.
While existing comparative case studies include three SLTCI countries at most, this article sets out to compare all six identified national-level SLTCI schemes in a cross-temporal perspective, including SLTCI in the Netherlands, Luxembourg and Israel, which have received less attention in comparative research so far. We aim to contribute to the existing literature by identifying the shared attributes and characteristics of SLTCI systems with regard to actor configurations and discussing potential factors behind system variation.
SLTCI: Concept and cases
SLTCI is a kind of SI scheme focusing specifically on protection against the risk of LTC. Generally, SI systems are based on the one hand on an insurance or equivalence rationale, while relying on the principle of social solidarity on the other (Pennings, Reference Pennings and Greve2018, p. 357). The insurance principle manifests mainly in the contributory nature of SI, ie. the members of the scheme pay premiums in advance and will benefit from the pooled insurance funds if and when the social risk occurs (Barr, Reference Barr2012, p. 98; ILO, 2017, p. 194). Unlike commercial, actuarial insurance, however, SI premiums are not based on individual risk but on ability to pay (mostly on the level of wage-income) and, to ensure viability, contribution is compulsory (Barr, Reference Barr2012, p. 98; Marmor, Reference Marmor2018, p. 1016). While both of these features crucially differentiate SI from voluntary private insurance, SI and compulsory private insurance schemes share the state-mandated obligation to insure and can, depending on concrete design and extent of regulation, be quite similar in practice (OECD, WHO, & Eurostat, 2011, pp. 161–164). However, there are also important differences between the latter two: In contrast to (compulsory) private insurance, SI has a stronger redistributive focus (Saltman, Reference Saltman, Saltman, Busse and Figueras2004, p. 5) and prohibits discrimination (Schmid, Reference Schmid2017, p. 41). In contrast to other forms of social protection schemes which are often more vulnerable to political decisions, SI schemes generally come with a guaranteed individual benefit entitlement for members (Marmor, Reference Marmor2018, p. 1017; Scheil-Adlung, Reference Scheil-Adlung2015).
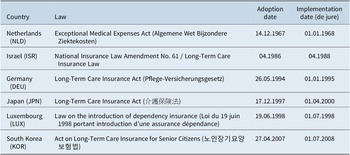
Building on the concept of SI discussed above, for the purpose of this article we define SLTCI as a country-wide, distinct (ie. specific and independent) social protection scheme for LTC establishing defined entitlements, which is compulsory and (at least partly) contribution based and contains a redistributive/solidarity element. Applying this definition, six countries worldwide, all located in Asia or Europe, classify as having introduced SLTCI: the Netherlands in 1967, Israel in 1986, Germany in 1994, Japan in 1997, Luxembourg in 1998 and South Korea in 2007.Footnote 1 Table 1 provides an overview of the respective legal bases and introduction dates. In an effort to capture the full spectrum of “real-world” SLTCIs, we analyse the configurations in all six countries at the time of initial implementation of the scheme and also, in the event of (major) changes, record their main features today (see Supplementary Table A2 for details). Consequently, in total (up to) 12 cases are studied. By incorporating a cross-temporal perspective in addition to the country comparison, it is possible to learn more about time-variant characteristics of the SLTCI model. Furthermore, instead of describing the LTC mix in the whole country, the focus here is exclusively on the configuration of the respective SLTCI scheme only. This way, the comparison is not distorted by inclusion of additional public provisions like social assistance programmes or private arrangements existing in the respective countries.
Table 1. Overview of six SLTCI systems.
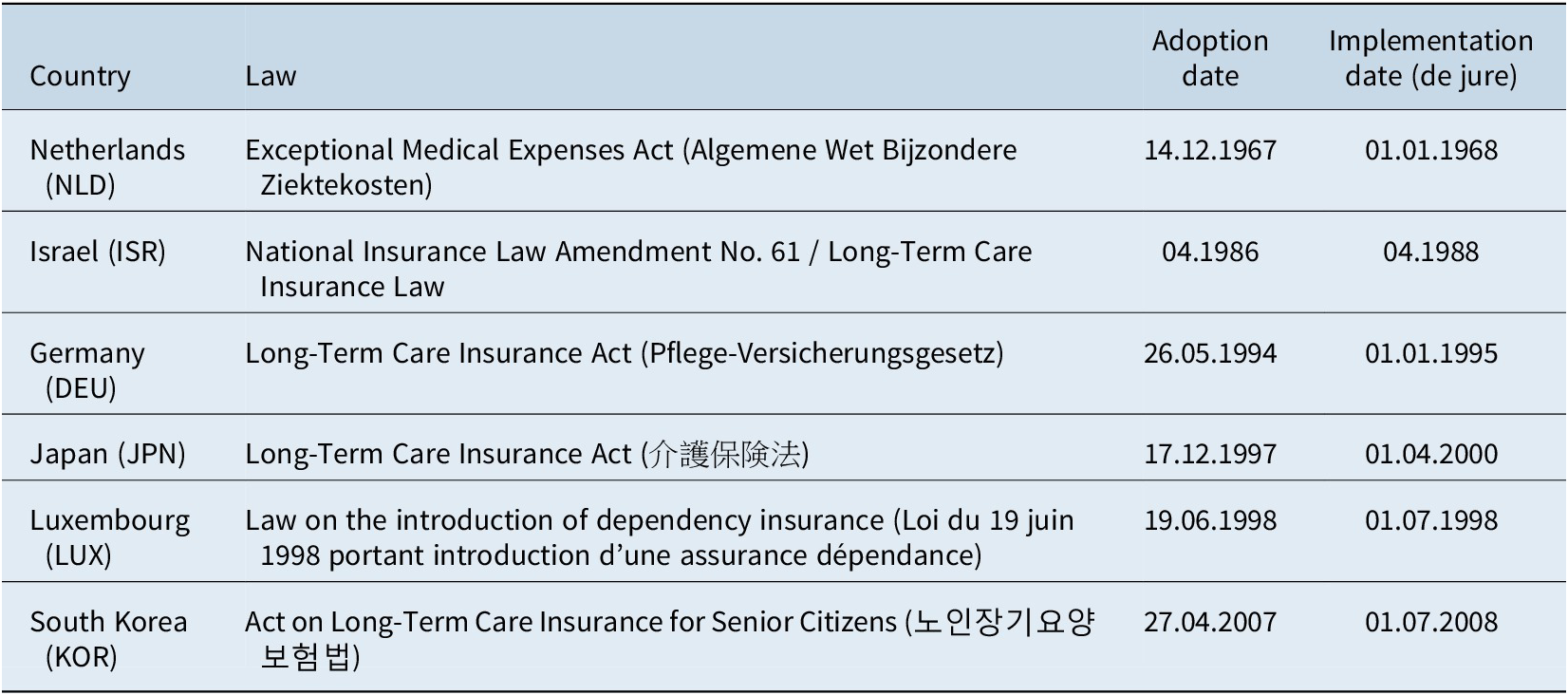
Source: Own compilation from laws and secondary sources.
Before we move on, it is important to reflect briefly on the inclusion of the LTC system in the Netherlands as an SLTCI case. Unlike the other five countries, the Netherlands is exceptional not only inasmuch as it is by far the first country globally to introduce a distinct LTC system, but also because the original scheme (AWBZ) focuses on “exceptional” medical expenses more generally and is not an insurance exclusively created for LTC (Dijkhoff, Reference Dijkhoff, Becker and Reinhard2018, p. 310). While the criterion of being a “distinct” insurance for LTC is therefore not as strictly fulfilled as in the other countries, LTC was a major motivation and rationale for the AWBZ (Companje, Reference Companje and Companje2014; Schut & van den Berg, Reference Schut and van den Berg2010). We thus include the Netherlands in the population of SLTCI systems for the purpose of this analysis. As for the features of the system “today”, for the sake of comparability we analyse the late AWBZ scheme as it was on the eve of the major reform of the Dutch LTC system in 2015 (see, eg. Dijkhoff, Reference Dijkhoff, Becker and Reinhard2018).
Conceptual framework
One central question when analysing care arrangements is who – ie. which type of (corporate) actor – bears responsibility in the LTC system (Daly & Lewis, Reference Daly and Lewis2000, p. 286; Jenson, Reference Jenson1997; Razavi, Reference Razavi2007). Such an actor-centred focus allows us, for instance, to gain insight into how care work is organised and recognised within a society (Lyon & Glucksmann, Reference Lyon and Glucksmann2008) and which modes of interaction logics – eg. hierarchy, coordination, competition – predominantly apply (Rothgang et al., Reference Rothgang, Cacace, Frisina Doetter, Grimmeisen, Schmid and Wendt2010, pp. 14–15). Furthermore, actor configurations can have implications for access, risk sharing and societal power relations. There are different types of actors, both public and private, which are relevant with regard to LTC. A common and useful classification in welfare and care research is the distinction of four major groups: state, societal actors, private for-profit actors and private individual actors (see, eg. Gough, Reference Gough and Kennett2013; Lyon & Glucksmann, Reference Lyon and Glucksmann2008; Ochiai, Reference Ochiai2009; Pijl, Reference Pijl, Evers, Pijl and Ungerson1994).Footnote 2 This fourfold actor conceptualisation can be depicted as the so-called welfare or care “diamond”, as shown in Figure 1 (Ochiai, Reference Ochiai2009; Pijl, Reference Pijl, Evers, Pijl and Ungerson1994; Razavi, Reference Razavi2007). Regarding the public actor types, we define the state including all state levels (local, regional, central) as the public institutions comprising the political-administrative system, while the nature of societal actors is formal, self-governing, non-governmental and non-profit oriented (see also Johnson, Reference Johnson1999, pp. 30–31; 147–148). As such, non-profit organisations, employee associations and SI funds are examples of societal actors. In contrast, private for-profit actors are commercial organisations or individuals selling care services or insurance policies on the market, while private individual actors consist of the care recipient’s family or household members or wider social network (Fischer, Frisina Doetter, & Rothgang, Reference Fischer, Frisina Doetter and Rothgang2022, p. 40).
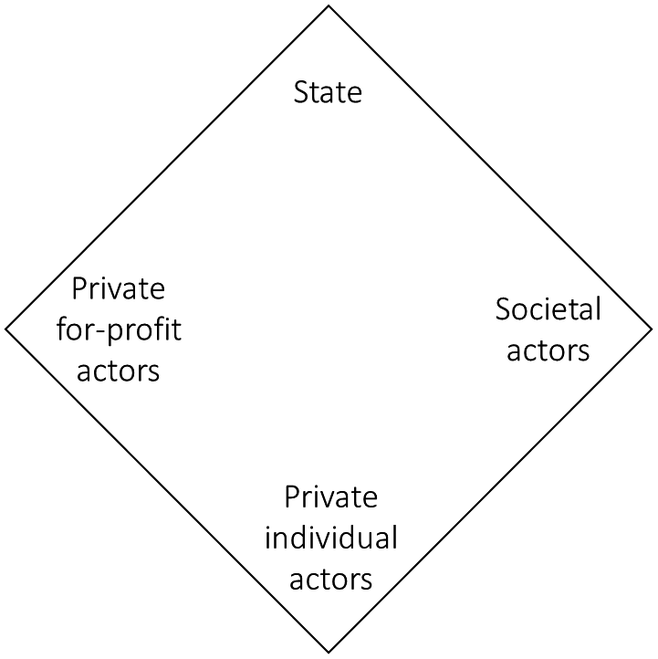
Figure 1. Long-term care diamond.
Source: Own presentation based on Pijl (Reference Pijl, Evers, Pijl and Ungerson1994) and Razavi (Reference Razavi2007).
While the care diamond is often applied in the context of the provision of services, a multi-dimensional approach is particularly fruitful for gaining a differentiated and comprehensive view on actors’ roles in LTC systems. For this purpose, we can conceptualise the LTC system as consisting of three (interrelated) dimensions. These are service provision, ie. the actual performance of assistive tasks as the primary function of the care system in residential, home or community settings, financing, ie. the resource input for “producing” LTC, and regulation, ie. the governance of the system’s production structure (Barr, Reference Barr2012, pp. 72–74; Fischer, Frisina Doetter, & Rothgang, Reference Fischer, Frisina Doetter and Rothgang2022; Wendt, Frisina, & Rothgang, Reference Wendt, Frisina and Rothgang2009). Each of these dimensions can comprise different actor constellations, which is why we analyse the intersection of actor types and dimensions separately. While for the financing and provision dimensions, the analysis will rely on the fourfold actor distinction of the diamond as displayed in Figure 1, in the regulatory dimension we will employ a “triangle” made up of state, societal actors and private actors only, as it does not seem feasible or particularly meaningful to differentiate two forms of private regulation (Fischer, Frisina Doetter, & Rothgang, Reference Fischer, Frisina Doetter and Rothgang2022, pp. 40–41). It is important to note that, while according to our understanding of regulation the non-state actors can (self-)regulate the LTC system, in any publicly created system the state always possesses a “meta” regulatory power in that it can delegate (or withdraw) regulatory competencies to the other actors.
Before moving on to investigate the shapes of the SLTCI care diamonds empirically, it can be helpful to reflect on hypotheses on which “diamonds” we expect to find for SLTCI systems. For the financing dimension, it is evident that societal actors – as carriers of social contribution funding (see section “Operationalisation”) – should be overwhelmingly dominant (eg. Campbell, Reference Campbell, Conrad and Lützeler2002; Scheil-Adlung, Reference Scheil-Adlung2015). Regarding LTC provision, Campbell’s (Reference Campbell, Conrad and Lützeler2002) description of the ideal-typical SLTCI system stresses the recipients’ choice between multiple providers as a particular feature. As there is otherwise not much discussion or evidence about particular SLTCI provision configurations, we can consider this as a very preliminary assumption. Similarly, a discussion of the main characteristics of SLTCI regulation such as setting contributions and fees, controlling providers or conducting eligibility assessments, is also largely absent in the literature. Therefore, it might be instructive to draw hypotheses from what is known about regulation of social health insurance (SHI), as SLTCI often adheres to the administrative structure of the pre-existing SHI systems (Campbell, Ikegami, & Kwon, Reference Campbell, Ikegami and Kwon2009). In these schemes, societal actors in the form of non-profit, non-governmental insurance funds are often key administrative agencies, governing by means of corporate self-regulation (De Roo, Chambaud, & Güntert, Reference de Roo, Chambaud, Güntert, Saltman, Busse and Figueras2004; Rothgang et al., Reference Rothgang, Cacace, Frisina Doetter, Grimmeisen, Schmid and Wendt2010; Wendt, Reference Wendt2019). Accordingly, we can expect that societal actors also play a substantial role in regulating SLTCI.
Research design and methods
Data
For each of the cases, data on the relevance of the four different actor types – state, societal actors, private for-profit actors, and private individual actors – in financing, providing and regulating the SLTCI scheme were collected. Due to a lack of international comparative information, we compiled data for each case separately employing a multitude of (mostly English language) sources: country case studies of the respective LTC systems (both academic literature and reports/grey literature), laws, official statistics and reports, and comparative publications and datasets. A summary of the relevant information, plus all sources used, is specified in the Supplementary Tables A2–A4. It is important to note that the kind and quality of information on the relevance of LTC actors varies greatly. To generate transparency about the data quality, confidence in the respective results was rated for each case/dimension as high (where reliable primary data such as laws, official statistics or at least two independent secondary sources were used), medium (for one reliable secondary source, and potentially some uncertainty) or low (for a high degree of uncertainty or conflicting sources).
Operationalisation Footnote 3
The assessment of the relevance of actors necessitates a procedure for operationalisation for each dimension. In financing, the shares of funding sources of the SLTCI system were essentially equated with the actor types: tax funding equals state, SI contributions equal societal actors, private insurance premiums equal private for-profit actors and out-of-pocket expenditure/individual co-payments equal private individual actors (see also Böhm et al., Reference Böhm, Schmid, Götze, Landwehr and Rothgang2013; Organisation for Economic Co-operation and Development (OECD), the World Health Organization (WHO), & Eurostat, 2011). In the service provision dimension, we generally followed three steps for determining the (approximate) shares of provider groups based on the number of care recipients whenever possible. Firstly, the share of each benefit type existing in the system, ie. of home and community-based services, institutional care services and/or cash benefits was recorded. Secondly, the share of the four actor types per benefit type was retrieved. Thirdly, with the data from the previous steps, the aggregate actor shares in the SLTCI system overall were calculated.
The regulatory dimension is particularly complex and can be operationalised in various ways (Wendt, Frisina, & Rothgang, Reference Wendt, Frisina and Rothgang2009). Besides recording which type of agency/organisation formally bears the main responsibility for managing the SLTCI scheme in the respective country, we analyse several objects of regulation to gain an in-depth picture of who is responsible for regulating different aspects of the LTC system and, consequently, de facto bears most responsibility. Previous research on LTC and health care systems has outlined six regulatory sub-dimensions which govern the triangular relationship between care recipients, care providers and financing bodies (Böhm et al., Reference Böhm, Schmid, Götze, Landwehr and Rothgang2013; Rothgang et al., Reference Rothgang, Fischer, Sternkopf and Frisina Doetter2021; Wendt, Frisina, & Rothgang, Reference Wendt, Frisina and Rothgang2009). These pertain to who assesses eligibility/need for LTC (1), who decides about contributions to the SLTCI (2), who regulates provider access to the system (3), who determines the remuneration for care providers (4), who decides which providers (5) and types of benefits (6) care recipients receive. Each of these sub-dimensions can be regulated by one or more actor types. It is important to note that, as outlined above, for the regulatory dimension we use an aggregate category of private actor regulation, employing a care “triangle” rather than a diamond.
Coding and visualisation
For comparing the actor configurations between cases, two transformations for systematising the “raw” data were subsequently conducted, namely the coding of data into fuzzy-set membership scores (MS), and the generation of a graphical representation of these scores. Fuzzy-sets theory is well suited for systematically and transparently analysing diversity (Kvist, Reference Kvist, Rihoux and Grimm2006; Ragin, Reference Ragin2000, pp. 12–13). By employing fuzzy-sets as a tool to measure “qualitative concepts […] quantitatively” (Lee, Reference Lee2013, p. 1912), the relevance of actor types in SLTCI systems can be compared in a standardised way across cases, which is especially helpful in light of the “messy” raw data available. When employing set theory, concepts are regarded as sets in which an empirical instance is – or is not – a member (Lee, Reference Lee2013). In contrast to dichotomous or “crisp” sets, fuzzy-sets allow for graded set membership, ie. the MS can vary between full set membership coded “1” and full non-membership, coded “0” (Kvist, Reference Kvist, Rihoux and Grimm2006).
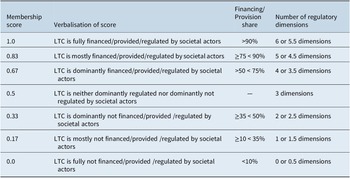
The transformation of the verbal data summaries into MS was roughly oriented to the calibration steps outlined by Ragin (Reference Ragin2000, pp. 166–171). Before assigning MS, it is important to define the number of values which can be assigned in light of the theoretical concepts and empirical evidence. We opted for discrete seven-scale sets which allow a differentiation of three grades of (non-)membership each, plus the crossover point 0.5, which indicates that an SLTCI system is neither a set member nor a non-member. For the (partly) non-standardised/non-comparable data available, this grading of MS provides a reasonable balance between summarising information and recording relevant differences (Ragin, Reference Ragin2000, pp. 155–156). Table 2 shows the MS, their meaning and the operationalisation for each LTC dimension exemplarily for societal actors. In total, one set is calibrated per actor type for each dimension (see Supplementary Tables A2, A3, A5). In a next step, the fuzzy-set values were depicted to represent the welfare diamond/triangle for each country (see similar visualisations eg. by Lyon & Glucksmann, Reference Lyon and Glucksmann2008; Ochiai, Reference Ochiai2009), with the size of the circles attached to the corners indicating the relevance of actor types. The area of the circles directly corresponds to the underlying MS (see Supplementary Table A1). The darker grey circles depict the actor configurations at the introduction point of each system, while the lighter grey circles indicate the relevance of the actors today in event of a substantial transformation, ie. an MS change.
Table 2. Operationalisation of fuzzy-set membership scores for societal actor financing, provision and regulation.
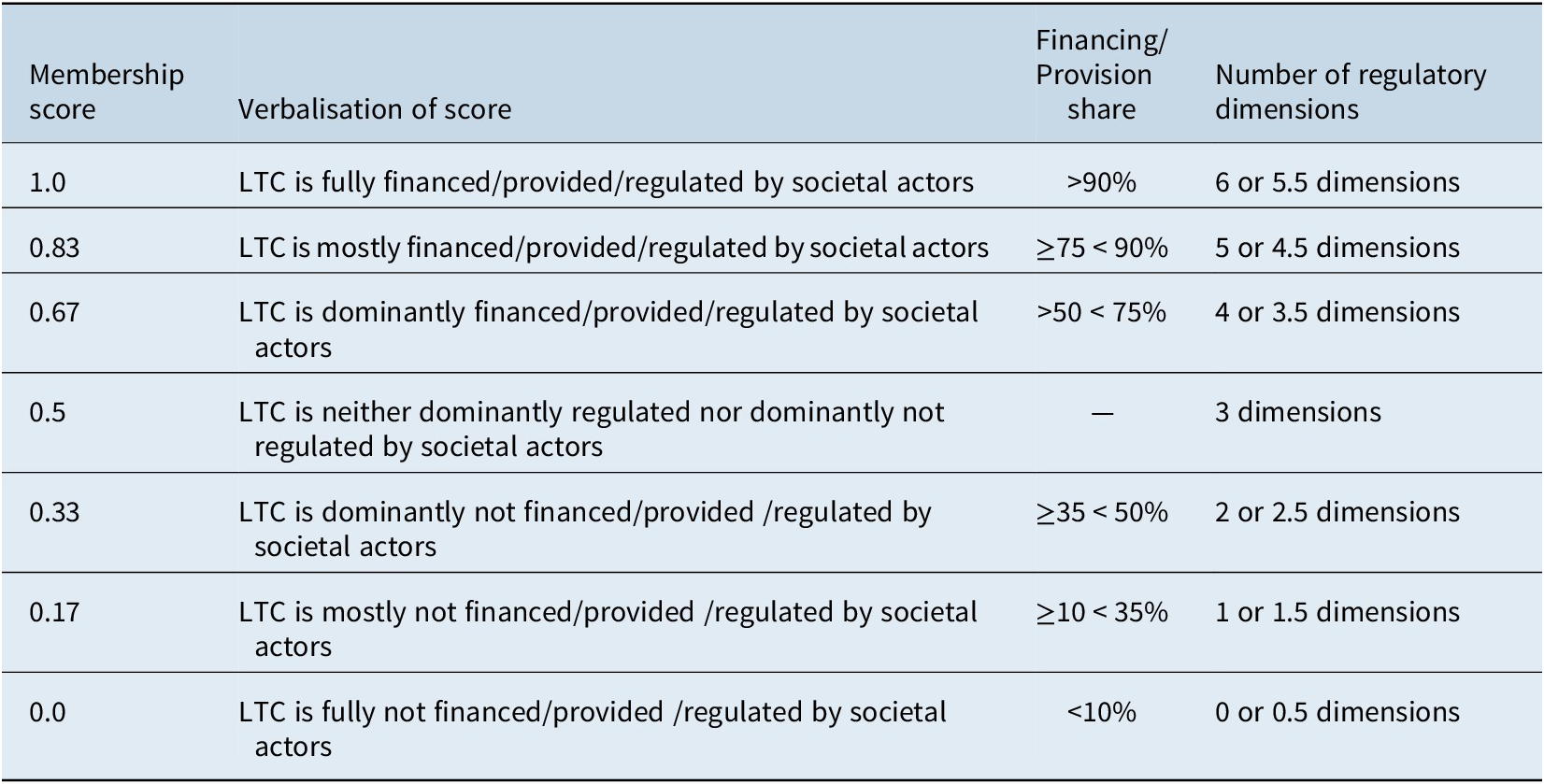
Source: Own representation.
Abbreviation: LTC, long-term care.
Actor configurations of SLTCI schemes
This section presents the results of the comparative analysis of the six SLTCI countries, analysing the main differences and similarities of the systems. Figures 2–4 show the welfare diamonds/triangles for the financing, provision and regulation dimension, respectively. In the following sub-sections, we describe and compare the actor configurations for each dimension, beginning with financing.
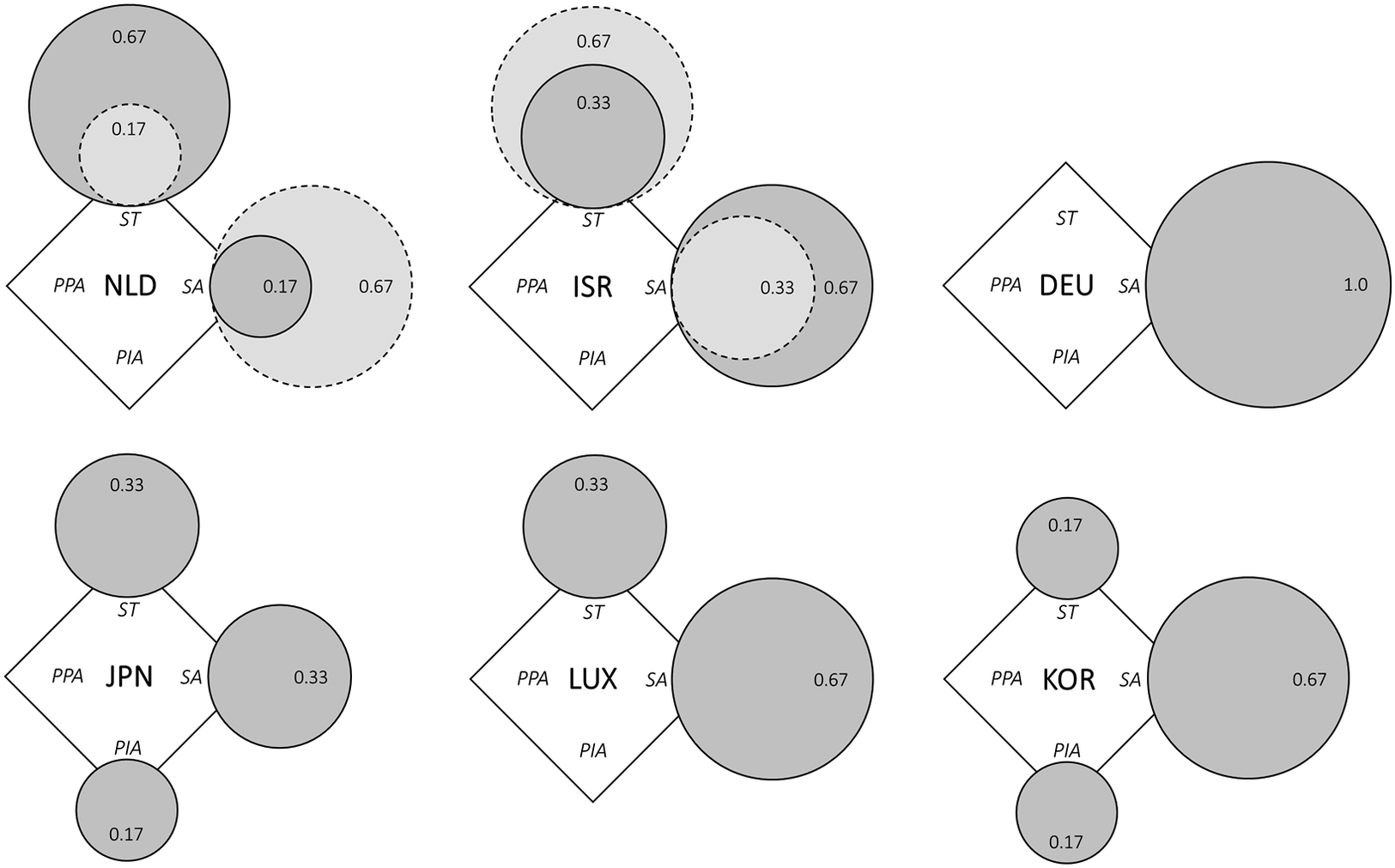
Figure 2. SLTCI diamonds for the financing dimension.
Source: Own representation based on data and fuzzy-set scores specified in Supplementary Table A2. Dark grey circles refer to system introduction, and light grey circles with dotted line show current diverging actor configurations, where applicable.
Abbreviations: NLD, Netherlands; ISR, Israel; DEU, Germany; JPN, Japan; LUX, Luxembourg; KOR, South Korea; ST, state; SA, societal actors; PPA, private for-profit actors; PIA, private individual actors.
Financing dimension
When taking a look at the financing mix of the six SLTCI systems displayed in Figure 2, we see that in the majority of cases societal actors are at least dominantly financing the system (MS ≥ 0.67). This is the case for the Netherlands today, Israel at introduction and Germany, Luxembourg and South Korea throughout. The only country with a higher score than 0.67 is Germany, though, where the SLTCI is fully financed by social contributions (MS = 1.0). Surprisingly, there are also three instances where societal actors are not the dominant funding actor. By design, the public financing of the SLTCI system in Japan is split equally between taxes and insurance contributions (Ozawa & Nakayama, Reference Ozawa and Nakayama2005). In the Netherlands, at the inception of the AWBZ in the late 1960s, it was dominantly funded by the state (MS 0.67) and mostly not by societal actors (MS 0.17) (Poske, Reference Poske1985). However, this strong state co-financing was only initially used to avoid abruptly increasing overall SI contributions (Winters, Reference Winters1996, p. 120). By the beginning of the 1980s, state financing share stood at around 20 per cent and social contributions had become the dominant source (Poske, Reference Poske1985, p. 109; Schut & van den Berg, Reference Schut and van den Berg2010). In Israel, by contrast, the share of earmarked LTC insurance contributions declined over time, so that a major share of the SLTCI funding today comes from the government budget as well as general social security revenues of the National Insurance Institute (NII), which are rededicated to the LTC programme (Asiskovitch, Reference Asiskovitch2013).
Overall, state co-financing of the SLTCI schemes is widespread, being present in every configuration except Germany’s. By contrast, substantial financing by private individual actors, ie. out-of-pocket co-payments, is only explicitly integrated in the schemes in Japan and South Korea at 10 per cent and 15–20 per cent, respectively (Rhee, Done, & Anderson, Reference Rhee, Done and Anderson2015). While this is one possibility to implement cost-sharing, it has to be borne in mind that these schemes are not generally less generous but rather stipulate an explicit designation of individual contributions within the SLTCI framework rather than capping benefit levels, as done for instance in Germany or Israel (Borowski, Reference Borowski2015; Colombo et al., Reference Colombo, Llena-Nozal, Mercier and Tjadens2011, pp. 229–239). All in all, most similar financing configurations of SLTCI schemes can be found in the Netherlands, Israel and Luxembourg with both substantial state and societal actor shares, as well as to some extent in the Japanese and South Korean systems, which rely on three funding sources. Furthermore, it is evident that pure financing by societal actors is not the reality in all but one of the SLTCI.
Provision dimension
In the care provision dimension, there is also a mix of several actor types for the cases (see Figure 3). However, in contrast to financing, private for-profit actors play a major role here in addition to societal actors, while state provision is largely absent. Societal actors are present in every country at the time of introduction as well as today, but in some instances such as the original Israeli and Dutch systems, where initially they provided care mostly or fully, their relevance as LTC providers has decreased to some extent over time (Borowski, Reference Borowski2015; van Hooren & Becker, Reference van Hooren and Becker2012). Societal actors are still dominant providers in SLTCI systems in Japan and the Netherlands today but have lost their primacy in Israel. Conversely, the market share of private for-profit actors has increased over time in several systems, most notably Israel, where they became dominant approximately 15 years after the establishment of the SLTCI (MS 0.17 ➔ 0.67), but also in Japan (MS 0.17 ➔ 0.33), the Netherlands (MS 0.0 ➔ 0.17) and Germany (albeit without a change in score). In the “youngest” SLTCI in South Korea, commercial providers were already dominant right from the start in 2008, with a share of around 75 per cent in the subsequent decade (Jeon & Kwon, Reference Jeon and Kwon2017; see also Supplementary Table A3). For Luxembourg, both private for-profit and societal actors seem to be most relevant in provision, but no data on exact provider shares were available (see also Pacolet & Wispelaere, Reference Pennings and Greve2018).
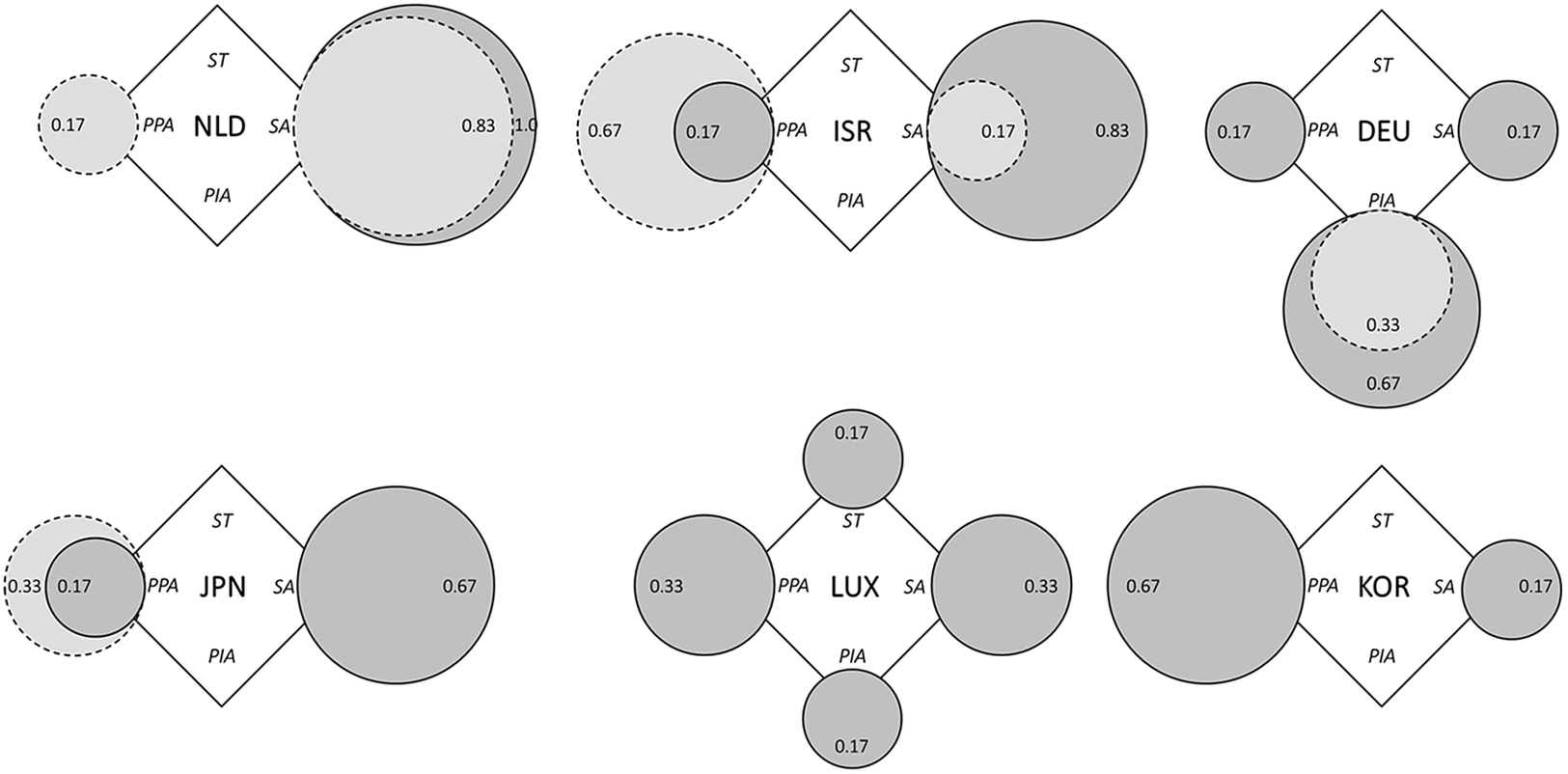
Figure 3. SLTCI diamonds for the provision dimension.
Source: Own representation based on data and fuzzy-set scores specified in Supplementary Table A3. Dark grey circles refer to system introduction, and light grey circles with dotted line show current diverging actor configurations where applicable.
Abbreviations: NLD, Netherlands; ISR, Israel; DEU, Germany; JPN, Japan; LUX, Luxembourg; KOR, South Korea; ST, state; SA, societal actors; PPA, private for-profit actors; PIA, private individual actors.
Private individual actors, ie. family members, and so forth providing informal care, only play a notable role in SLTCI schemes in Germany and Luxembourg, the two countries where a regular cash benefit option is available (Theobald & Kern, Reference Theobald and Kern2011). At introduction, the acceptance of (pure) cash benefits has been much higher in Germany, though (53 per cent of benefits in 1998) than in Luxembourg (26 per cent of benefits in 2002), where cash benefits are granted more restrictively (Bundesministerium für Gesundheit, 2020; OECD, 2005; Pacolet & Wispelaere, Reference Pennings and Greve2018). In both countries, the number of care recipients opting for monetary benefits has declined over time; in Germany, private individual actors shifted from being main providers (MS 0.67) at SLTCI introduction to non-dominant providers (MS 0.33) in the current scheme. Interestingly, this is not only due to a diminished take-up of cash benefits, but also to their (assumed) use, as more care recipients employ migrant domestic care workers to substitute/support family care in recent years (Benazha et al., Reference Benazha, Leiblfinger, Prieler, Steiner, Aulenbacher, Lutz and Schwiter2021). In the other four SLTCI countries, cash benefits were/are not very prevalent, strictly limiting the role of private individual actors within the SLTCI systems. This may have changed with recent reforms of the Dutch and Israeli LTC systems, which extended the options for non-in-kind benefits (Dijkhoff, Reference Dijkhoff, Becker and Reinhard2018; Hasson & Buzaglo, Reference Hasson and Buzaglo2019); however, an analysis of these more recent developments is beyond the scope of this article. Generally, the systems which bear most similarity in the provision dimension are Israel and Japan at introduction and Israel and South Korea today. The most evident shared traits of the SLTCI systems are the absent/limited role of the state as an LTC provider as well as the provision mix of (at least) private for-profit and societal actors. With the provision dimension being the one with most changes recorded since system introduction, we see tentative trends of increased relevance of private for-profit actors in recent years, but without them becoming dominant in most cases.
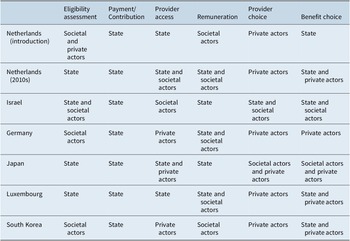
Regulation dimension
Moving on to the regulation dimension, in all but one country the main administrative agencies responsible for managing the SLTCI schemes are societal actors (see Supplementary Table A6). In the Netherlands, Germany, Luxembourg and South Korea they are linked to or part of the SHI administration/funds (Companje, Reference Companje and Companje2014; Pacolet & Wispelaere, Reference Pennings and Greve2018; Rhee, Done, & Anderson, Reference Rhee, Done and Anderson2015), while in Israel the NII is in charge (Asiskovitch, Reference Asiskovitch2013). The exceptional case is Japan, where the municipalities rather than a specific societal agency act as the insurers (Ozawa & Nakayama, Reference Ozawa and Nakayama2005). In all countries, however, many aspects such as needs assessment or contribution levels are not (only) regulated by these designated agencies. Therefore, we used the following six sub-dimensions for a detailed comparison of the regulatory actor mix, asking for each item which actor type bears the main regulatory responsibility (see also section “Operationalisation”): eligibility assessment, payment/contributions, provider access to the system, remuneration/fees, provider choice and benefit choice. The dominant actors – state, societal actors, private actors – for each sub-dimension are detailed in Table 3.
Table 3. Actors present in each regulatory sub-dimension per case.
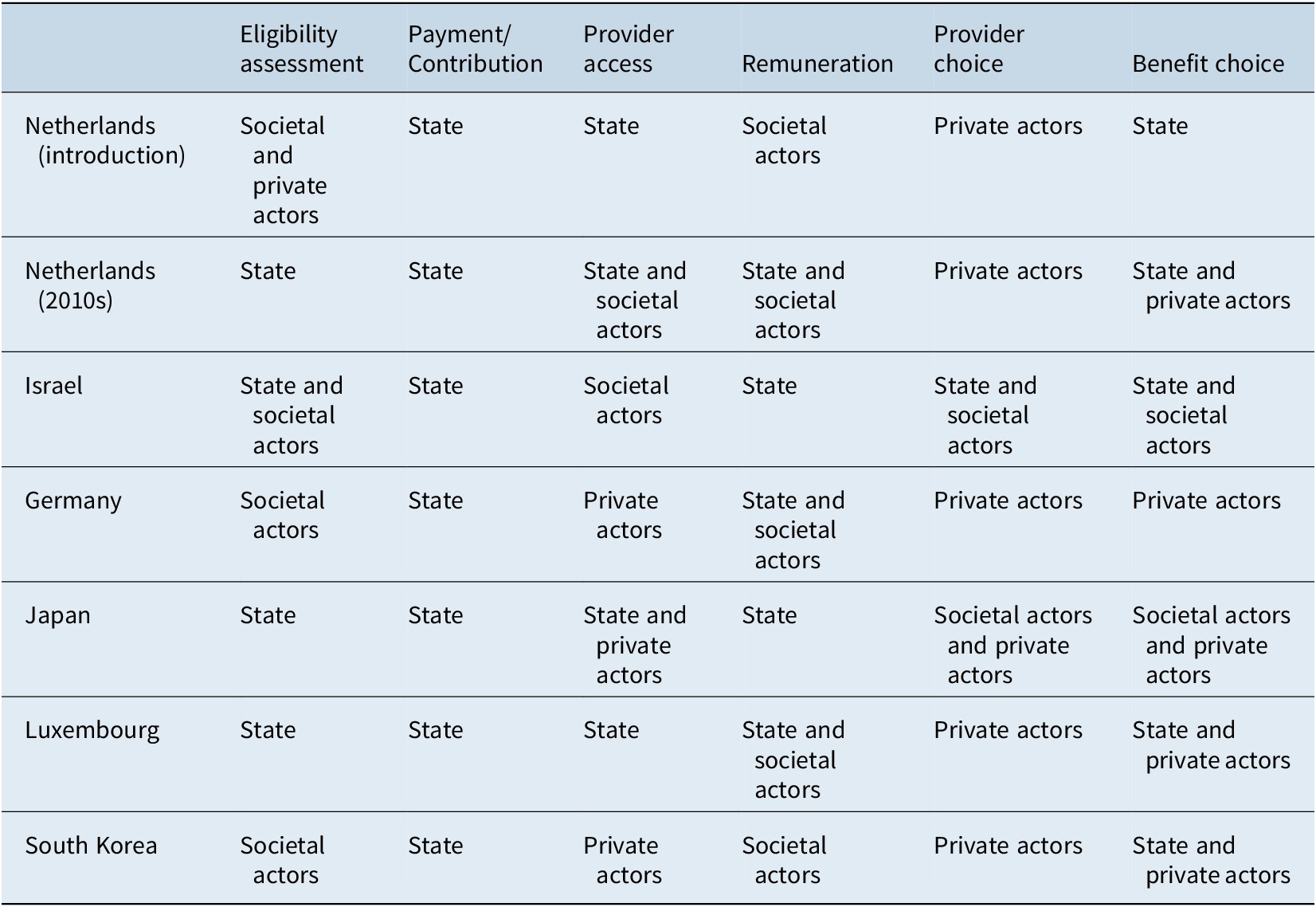
Source: Own representation based on summary of data specified in Supplementary Table A4.
The triangles in Figure 4 show that in most cases all three types of actors are present, while the sub-dimensions populated by the state prevail. The state is the dominant regulator (MS 0.67) of the SLTCI systems in Israel, Japan, Luxembourg and the Netherlands today (previously it was at 0.5). Societal actors, by contrast, in general have a more limited role; even in Israel and South Korea, where they are most relevant, they are only dominantly not regulating (MS 0.33) the system. This is surprising, because on the one hand administrative agencies are mainly societal actors, while on the other, the SHI literature stresses the role of corporate self-regulation (see section “conceptual framework”). The two sub-dimensions where societal actors are most present are eligibility assessment and provider remuneration, but even here state actors are also heavily involved. Almost all SLTCI schemes include some aspects of choice where decisions and (self-)regulation are left to private actors. This is most evident in the provider choice sub-dimensions. Private actors are most in charge in the systems in Germany (MS 0.5) and South Korea (MS 0.33), where provider access to the system and benefit choice are also (in part) privately regulated (Rhee, Done, & Anderson, Reference Rhee, Done and Anderson2015; Rothgang, Reference Rothgang2010). In both cases, the dominance of private actors is a result of prevailing private choice possibilities as regards both the concrete care provider as well as the type of benefits (eg. between cash and in-kind benefits in Germany) and the absence of specific entry controls for providers to offer services within the SLTCI (see Table 3). However, it is important to note that this does not imply an absence of “meta” state regulation, meaning that states do set crucial standards by means of legislation and administrative decisions also in the cases of the public LTC systems in Germany and South Korea. Consequently, the regulatory triangles of both countries are quite similar, as are the actor mixes of Japan and the Netherlands today. Overall, a plurality of all three actor types seems to be a key feature of SLTCI regulation – a characteristic which has also remained stable over time.
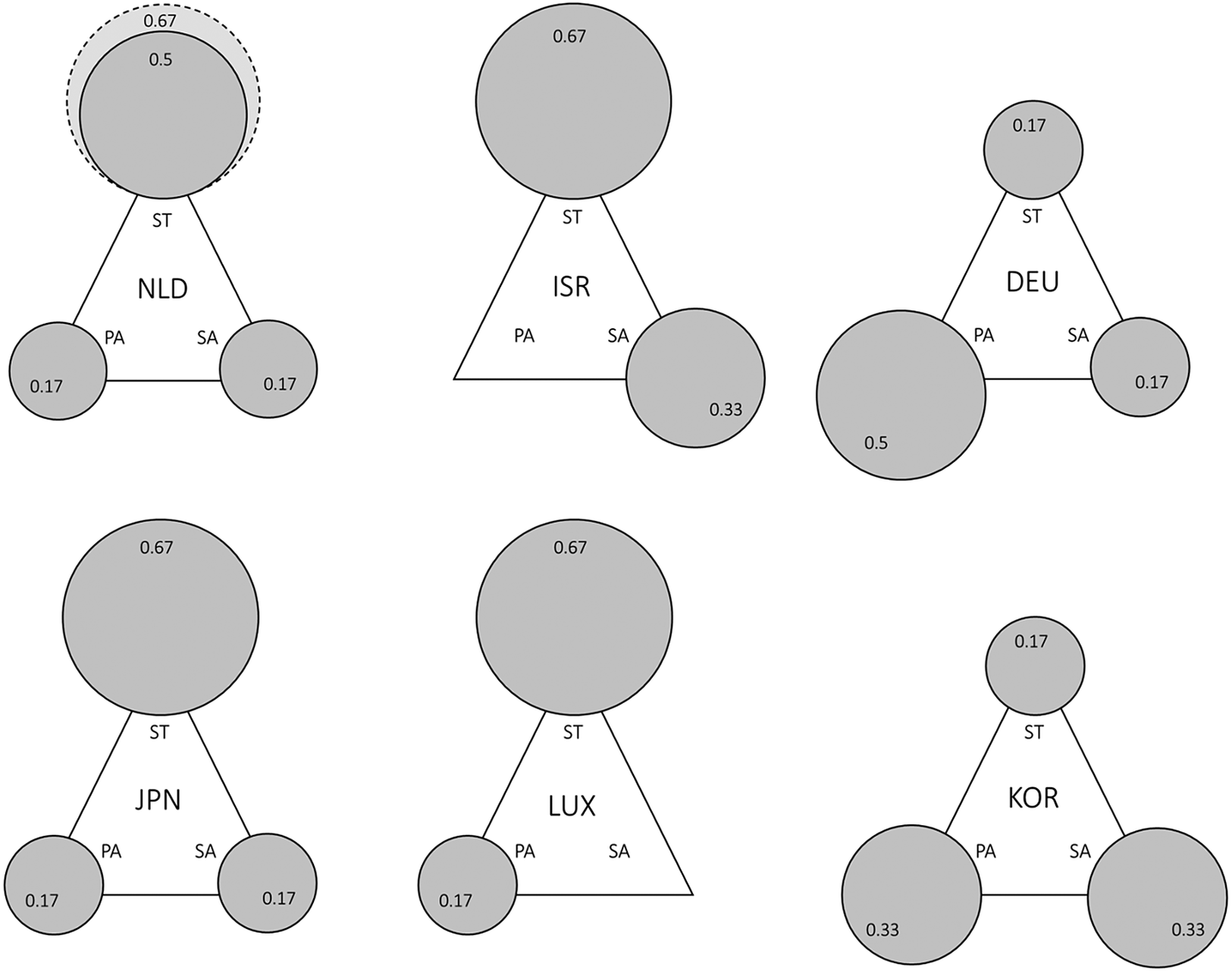
Figure 4. SLTCI triangles for the regulatory dimension.
Source: Own representation based on data and fuzzy-set scores specified in Supplementary Tables A4 and A5. Dark grey circles refer to system introduction, and the light grey circle with dotted outline shows diverging actor configurations for today.
Abbreviations: NLD, Netherlands; ISR, Israel; DEU, Germany; JPN, Japan; LUX, Luxembourg; KOR, South Korea; ST, state; SA, societal actors; PA, private actors.
Discussion
Summing up the findings from the previous section, we have been able to detect several similarities characterising SLTCI systems. In financing, a mix of societal actor and state funding is common, with social contributions as the main funding source in most cases. In the provision dimension, the characteristic feature is a mix of societal and private for-profit actors, with the latter becoming more relevant over time. State provision generally does not play a role. Lastly, the regulation of SLTCI schemes is characterised by a mix of all three actor types. Overall, state regulation is most relevant, social actor regulation far less present and private actor involvement in provider and benefit choice is common. In light of the tentative hypotheses about typical SLTCI configurations formulated in the section “Conceptual framework”, some of these findings were expected, while others are surprising. While the predominance of societal actors in financing is confirmed, overall state funding covers a larger proportion than expected. The results also confirm our tentative hypothesis of an actor mix in provision. The limited role of societal actor regulation is most puzzling, especially as we know that societal actors are de facto the key administrative agency in most systems. Still, compared to our hypothesis drawn from SHI observations, societal actors are only one regulator among two important others, and the triangles show that most responsibility rests with the state.
Despite the highlighted similarities of SLTCI systems, there is quite some variation present in each dimension as well. For instance, private individual actors are certainly relevant in financing and providing LTC in some of the countries, but not at all in others. Also, the extent of state financing and the balance of private for-profit versus societal provision differ substantially. A crucial question emerging from the preceding analysis is thus: what accounts for the substantial variation between the six different SLTCI actor configurations? For investigating this question, it can be useful to consider theoretical strands which have been employed in comparative welfare study (see, e.g. Orloff, Reference Orloff, Adams, Clemens and Orloff2005; Seelkopf & Starke, Reference Seelkopf and Starke2019, pp. 5–8): Socio-economic or functionalist pressures, political interests and actors constellations, institutional structures and path dependencies, existing (care) cultures or the (international) spread of ideas could all shape SLTCI policy design in individual cases. While we cannot fully investigate this issue here, in the following we explore a selection of possible structural driving factors which have also been highlighted in the extant literature, namely the existence of regional or temporal clusters which are more alike than more distant cases as well as institutional path dependencies stemming from pre-existing social policies (see section “Literature review”).
One key argument in the literature on policy diffusion and transfer is that policy learning is more likely to occur between similar entities, ie. in particular, countries which are geographically (or culturally) proximate (Elkins & Simmons, Reference Elkins and Simmons2005, p. 45; Schmitt & Obinger, Reference Schmitt and Obinger2013). If this were the case here, one might, eg. expect to find an east Asian SLTCI configuration with highly similar schemes in Japan and South Korea, or a central European one comprising the Netherlands, Luxembourg and Germany. As outlined above, there is some evidence for policy transfer between these countries, especially by South Korea from Japan, and Luxembourg from Germany – but also by Japan from Germany and Scandinavia, dampening the “proximity hypothesis” (Campbell, Ikegami, & Kwon, Reference Campbell, Ikegami and Kwon2009; Maags, Reference Maags2020; Theobald & Kern, Reference Theobald and Kern2011). Indeed, the hypothesised geographical clusters are largely not present when comparing the empirical constellations across all three dimensions. The geographically close countries with most similarities are Japan and South Korea, but the correspondence of the two is only high in financing, while being marginally present in provision and not at all in regulation. In fact, no countries, whether geographically proximate or distant, share strong similarities in total, ie. over all three dimensions. Therefore, at least for actor configurations of SLTCI systems, regional proximity does not provide a lead for explaining variation.
Another structural difference which could explain differences in actor configurations relates to the time point of system introduction and analysis. In the field of LTC, there is extensive literature which stresses marketisation and privatisation trends in public LTC systems since the 1990s (eg. Ledoux, Shire, & van Hooren, Reference Ledoux, Shire and van Hooren2021; Ranci & Pavolini, Reference Ranci and Pavolini2015; Theobald et al., Reference Theobald, Szebehely, Saito and Ishiguro2018). This could hasten a growing role for private for-profit actors in SLTCI service provision or regulation, eg. through the introduction of “consumer choice” models. As regards the initial set up of service provision in the SLTCI schemes, we can indeed observe that private individual actors did not have a place in the AWBZ as established in the late 1960s and only a limited role in the systems of the 1980s and 90s, but a predominance in the latest SLTCI introduced in South Korea in 2007; the reverse is partly visible for societal actors. While there is a marginal relationship between timing of system introduction and provision patterns, a periodical effect seems to be more pronounced concerning the development in countries over time. Here, the share of private for-profit provision clearly increases, most notably in the Netherlands and Israel, but also Japan and Germany. In contrast, in financing and regulation we can neither observe an increased relevance of private actors nor any other clear temporal development. Therefore, there is only limited evidence – particularly for the provision dimensions – that “temporal clusters” drive SLTCI variation.
As geographical or temporal location of SLTCI systems does not seem to drive the observed differences to a large extent, institutional factors, ie. pre-existing rules, norms and structures, could in contrast be relevant. The explanatory LTC literature discusses various institutions which could shape countries’ LTC arrangements, ranging from the set-up of the political system in general, including veto players and electoral procedures, (eg. Maags, Reference Maags2020) to concrete welfare institutions like historical care provision or health care system structures (Campbell, Ikegami, & Kwon, Reference Campbell, Ikegami and Kwon2009; Morel, Reference Morel, Bonoli and Armingeon2006). While not dismissing the potential relevance of political institutions for individual SLTCI introduction or design, we focus here on the second, more LTC-specific set of institutional “path dependencies”. The role of pre-existing health care system structures could be especially instructive in analysing SLTCI systems as all six cases had SHI schemes in place and many are managed by the same organisations (eg. Campbell, Ikegami, & Kwon, Reference Campbell, Ikegami and Kwon2009; Colombo et al., Reference Colombo, Llena-Nozal, Mercier and Tjadens2011, pp. 220–221; see above). Do SLTCI actor configurations vary because they are modelled after (different) pre-existing SHI systems existing in the countries a time of SLTCI introduction?
Indeed, there seems to some initial evidence supporting this hypothesis. Overall, both systems are very similarly constructed in Germany, Luxembourg and South Korea (Böhm et al., Reference Böhm, Schmid, Götze, Landwehr and Rothgang2012), while in the other three countries there are large differences. However, while in Israel the LTCI does clearly not build on the health care system at all (Shirom, Reference Shirom1995), there is an institutional link between SHI and SLTCI in the Netherlands and Japan: the Dutch AWBZ was introduced as a complement to the compulsory health insurance law specifically for “high medical risks” (Companje, Reference Companje and Companje2014), the Japanese LTCI resembles one branch of the SHI system, namely the Citizens Health Insurance which (also) covers pensioners (Campbell, Reference Campbell, Conrad and Lützeler2002). When comparing the actor configurations across dimensions, we see that the funding mixes and the regulatory responsibilities are quite alike. Taking OECD health expenditure statistics by financing schemes at the time point of respective SLTCI introduction, we see that in Germany and Luxembourg, financing shares of SHI and SLTCI are nearly identical, while in Israel, Japan and South Korea the mix is somewhat similar as well, albeit with higher co-payments in health (OECD, 2021a).Footnote 4 According to the classification of health care systems by Böhm et al. (Reference Böhm, Schmid, Götze, Landwehr and Rothgang2012), in these three countries, the actor mix in regulation also shows most parallels. Interestingly, the Dutch, Japanese and South Korean SHI are, despite being SHI models, also not dominantly regulated by societal actors but the state. This is, in turn, not the case for Germany and Luxembourg, where societal governance of SHI is much stronger than in the field of LTC, leading to marked differences in regulation (Böhm et al., Reference Böhm, Schmid, Götze, Landwehr and Rothgang2012). In the provision dimension, the parallels between both systems seem to be generally small, except the limited involvement of the state in both cases: private for-profit provision is much more pronounced in SHI schemes (except in South Korea) (Böhm et al., Reference Böhm, Schmid, Götze, Landwehr and Rothgang2012), while private individual actors are not a relevant actor in health care systems per se. Overall, this preliminary comparison of health and LTC systems shows that some variation in actor constellations of SLTCI systems really seems to be driven by pre-existing SHI structures. This seems in particular to be true for financing, where we see marked parallels in state and societal actor shares, and the strong role of the state in some SLTCI systems in regulation.
Conclusion
This article has investigated similarities and differences in SI systems in the – comparably novel – social policy field of LTC by analysing the welfare diamond/triangle of all six country-wide SLTCI systems introduced globally. It has been established that the typical SLTCI scheme is characterised by societal actor funding with substantial state shares, a combination of societal actor and private for-profit provision, and a tripartite regulatory actor mix dominated by state regulation. These findings were somewhat unexpected, in particular as regards the considerable role of the state in regulation and financing. However, we have also seen that there are crucial differences between the schemes, for instance in the inclusion of private individual provision and the extent and types of financial sources used beyond social contribution funding. These variations can partly be traced back to temporal developments (in the provision dimension) and pre-existing SHI system features (in the financing and regulation dimension), while regional clusters are only marginally evident.
While the discussion has explored some initial factors for understanding the variation between the SLTCI configurations in different countries, a more in-depth analysis aiming to explain individual actor constellations would have to examine political and societal actors, institutions and discourses in more depth. In particular, it might be instructive to take a more in-depth look at pre-existing LTC and health care arrangements of the respective countries, as they could have influenced features of the SLTCI systems. Furthermore, socio-economic factors such as the availabilities of funds as well as the role of political interest groups such as provider or women associations could be considered as possible explanatory factors in future research. Besides the rudimentary explanation, the article is also limited in other ways. While the “who” question has proven to be a crucial lens for studying care arrangements, there are of course further characteristics of SLTCI systems worth studying, eg. benefit types, generosity or inclusiveness of the schemes, which this article has touched upon only marginally. The same also pertains to linking the configurations with (normative) outcomes such as availability, affordability or quality of care. Furthermore, the analysis is strongly focused on a historical perspective, which has the benefit of providing a comprehensive picture, but inhibits a more thorough analysis of current schemes. Nevertheless, the empirical analysis of SLTCI systems has contributed to a better understanding of the model as well as individual cases, while shedding some light on factors driving variation. In addition to a more extensive explanatory analysis, it could also be insightful to compare SLTCIs with other types of distinct LTC systems in future research to investigate what distinguishes SLTCI systems from other prevalent models.
Acknowledgements
The author would like to thank Kristin Noack, Heinz Rothgang and the participants in his doctoral colloquium for helpful comments and suggestions on earlier versions of this article and Vicki May for editorial support.
Disclosure statement
No potential conflict of interest was reported by the authors.
Notes on Contributors
Johanna Fischer is a postdoctoral researcher at the Collaborative Research Center (CRC) 1342 “Global Dynamics of Social Policy” and SOCIUM research Center on Inequality and Social Policy at the University of Bremen, Germany. She completed her PhD on Economic and Social Sciences at the University of Bremen on the emergence and types of long-term care systems worldwide. Her current research within the CRC project A07 “Global Dynamics of Long-Term Care Policies” focuses on comparatively analysing the generosity of long-term care schemes and at elder care policy on the inter- and transnational level. Her research interests include comparative social policy and politics, global social policy, care and ageing.
Funding
This work was funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) – Project number: 374666841 – SFB 1342.
Supplementary Materials
To view supplementary material for this article, please visit http://doi.org/10.1017/ics.2022.9.