1. Introduction
In aortic valve replacement therapy, moderate to severe aortic stenosis is treated by replacing the diseased native aortic valve by a valve prosthesis which is manufactured either of man-made materials (mechanical heart valve, MHV) or of biological tissue (bioprosthetic heart valve, BHV) (Yoganathan, He & Jones Reference Yoganathan, He and Jones2004; Head, Çelik & Kappetein Reference Head, Çelik and Kappetein2017). Besides their superior durability, MHVs require life-long anti-coagulation therapy for the patient due to flow-induced thrombogenicity which is caused by excessive shear stresses in the flow field that cause platelet activation (Yun et al. Reference Yun, Dasi, Aidun and Yoganathan2014; Hedayat, Asgharzadeh & Borazjani Reference Hedayat, Asgharzadeh and Borazjani2017; Klusak & Quinlan Reference Klusak and Quinlan2019). A BHV creates a more physiological flow field and exhibits lower thrombogenicity. Nevertheless, turbulent flow during the systolic phase of the cardiac cycle is observed (Becsek, Pietrasanta & Obrist Reference Becsek, Pietrasanta and Obrist2020), possibly triggering leaflet calcification and eventually leading to structural valve deterioration (Dvir et al. Reference Dvir2018; Gomel, Lee & Grande-Allen Reference Gomel, Lee and Grande-Allen2019; Li Reference Li2019; Tsolaki et al. Reference Tsolaki2023) or causing bioprosthetic leaflet thrombosis (Egbe et al. Reference Egbe, Pislaru, Pellikka, Poterucha, Schaff, Maleszewski and Connolly2015; Holmes & Mack Reference Holmes and Mack2017; Puri, Auffret & Rodés-Cabau Reference Puri, Auffret and Rodés-Cabau2017). Therefore, turbulent blood flow after BHVs is detrimental to valve performance and may be a factor for their limited durability of less than 20 years, which prevents their usability for younger patients (Kheradvar et al. Reference Kheradvar2015). To understand the origin of turbulent flow after a BHV, the identification of hydrodynamic instabilities and the understanding of laminar–turbulent transition mechanisms in the vicinity of the valve prosthesis is crucial.
Fluid–structure interaction (FSI) of blood flow and bioprosthetic aortic valves has been described and investigated both experimentally (e.g. Saikrishnan et al. Reference Saikrishnan, Yap, Milligan, Vasilyev and Yoganathan2012; Hasler & Obrist Reference Hasler and Obrist2018; Jahren et al. Reference Jahren, Heinisch, Hasler, Winkler, Stortecky, Pilgrim, Londono, Carrel, Von Tengg-Kobligk and Obrist2018; Oechtering et al. Reference Oechtering2019; Lee et al. Reference Lee, Rygg, Kolahdouz, Rossi, Retta, Duraiswamy, Scotten, Craven and Griffith2020) and numerically (e.g. Borazjani Reference Borazjani2013; Bavo et al. Reference Bavo, Rocatello, Iannaccone, Degroote, Vierendeels and Segers2016; de Tullio & Pascazio Reference de Tullio and Pascazio2016; Hedayat et al. Reference Hedayat, Asgharzadeh and Borazjani2017; Chen & Luo Reference Chen and Luo2018; Gilmanov, Stolarski & Sotiropoulos Reference Gilmanov, Stolarski and Sotiropoulos2018; Becsek et al. Reference Becsek, Pietrasanta and Obrist2020; Gallo, Morbiducci & de Tullio Reference Gallo, Morbiducci and de Tullio2022; Johnson et al. Reference Johnson, Rajanna, Yang and Hsu2022; Asadi & Borazjani Reference Asadi and Borazjani2023).
Various complex flow phenomena are present during the opening of the valve. With a central aortic jet emerging from a non-circular time-varying valve orifice area, a highly unsteady downstream flow field is created including a shear layer separating the forward flow towards the ascending aorta (AAo) and the retrograde flow towards three cavities enclosing the valve, known as sinus of Valsalva. Immediately following valve opening, a non-circular starting vortex ring of threefold symmetry is formed which breaks down to smaller-scale vortices shortly thereafter. It marks the onset of turbulence during systolic acceleration (see e.g. figure 5 in Becsek et al. (Reference Becsek, Pietrasanta and Obrist2020)). The identification of hydrodynamic instabilities contributing to this laminar–turbulent transition is intricate due to the existence of various spatial and temporal scales of the flow problem.
Instabilities initiating turbulent flow around MHVs were evaluated by simplification of the problem with a bottom-up approach and a geometrical submodel (Zolfaghari & Obrist Reference Zolfaghari and Obrist2019; Zolfaghari et al. Reference Zolfaghari, Kerswell, Obrist and Schmid2022). Highly-resolved two- and three-dimensional direct numerical simulations (DNS) were performed for a rigid, fixed MHV in open systolic position. The use of linear stability analysis (LSA) tools enabled the identification of a pocket of absolute instability which caused nonlinear breakdown of the flow farther downstream. This discovery provided cues for an optimized leaflet design which allowed the delay of the laminar–turbulent transition such that unfavourable flow phenomena downstream of the aortic valve in the AAo could be eliminated.
In contrast to MHVs, bioprosthetic aortic valves include anisotropic, hyperelastic leaflet behaviour which adds to the problem complexity due to FSI (Soares et al. Reference Soares, Feaver, Zhang, Kamensky, Aggarwal and Sacks2016). Strongly dependent on the valve design, a complex interplay of downstream turbulence, recirculating flow within the sinus of Valsalva and structural anisotropy of the leaflets may cause so-called fluttering describing a nonlinear oscillating leaflet motion (Lee et al. Reference Lee, Scotten, Hunt, Caranasos, Vavalle and Griffith2021). Previous studies of valve performance in the presence of fluttering have shown both increased thrombosis risk due to higher turbulent kinetic energy levels (Hatoum et al. Reference Hatoum, Yousefi, Lilly, Maureira, Crestanello and Dasi2018) and also accelerated valve deterioration due to cyclic stresses (Johnson et al. Reference Johnson, Wu, Xu, Wiese, Rajanna, Herrema, Ganapathysubramanian, Hughes, Sacks and Hsu2020). Therefore, valve fluttering might contribute to the limited long-term durability of BHVs. Experimental as well as computational results have shown the influence of valve diameter and valve thickness on the fluttering frequency (Lee et al. Reference Lee, Scotten, Hunt, Caranasos, Vavalle and Griffith2021). According to results of Johnson et al. (Reference Johnson, Rajanna, Yang and Hsu2022), reduced flexural stiffness is considered a primary factor for increased leaflet flutter resulting in additional vortex formation in the valve vicinity, blood flow disturbance and an oscillatory pressure field. By varying the leaflet thickness, Chen & Luo (Reference Chen and Luo2020) investigated the impact of bending rigidity identifying an optimal range located between reduced rigidity resulting in flapping motion lowering the valve performance index and increased rigidity leading to hampered opening and closing as well as higher resistance. However, whether the origin of laminar–turbulent transition can be linked to hydrodynamic instabilities developing in the downstream flow field or to the active perturbation of the fluid by an oscillating structure remains unclear.
The identification of the mechanisms leading to laminar–turbulent transition past bioprosthetic aortic valves is important to find ways to suppress or control turbulence in the AAo and therefore to prevent unfavourable flow phenomena. Previous computational studies focused on modelling the full kinematic and morphological complexity of a BHV. While this approach leads to comprehensive understanding of large-scale flow phenomena, the interaction of multiple complex flow features like recirculation and shear layers with the fluttering motion of hyperelastic structures complicates the isolation of instabilities with such a top-down approach. Basic fundamental questions remain unanswered such as the specific types of instabilities, their origin and their individual role in the laminar–turbulent transition mechanisms. Thus, we propose a bottom-up approach breaking down the complex flow problem into sub-problems targeting a more isolated and focused study of instability mechanisms.
First, we derive extended Orr–Sommerfeld equations which include FSI to study basic linear instability mechanisms in a simplified one-dimensional model. Second, we perform numerical FSI simulations of simplified two-dimensional models of the aortic root with different geometries (e.g. different aortic diameters) and with rigid or flexible leaflets. The resulting flow fields feature various instabilities which interact in different ways with each other. Finally, a comparison between the results obtained from linear stability analysis and the flow patterns observed in numerical data provides deeper insight into the pathways towards transition.
The remainder of this paper is structured as follows. Section 2 illustrates the developed theoretical framework accounting for FSI in LSA (§ 2.1) and gives an overview of the results of temporal LSA (§ 2.2). Section 3 introduces the governing equations and numerical method of our numerical FSI simulations (§ 3.1) as well as the two-dimensional parametrized aortic model (§ 3.2). Numerical results are described (§ 3.3), specifically focusing on the influence of aortic wall geometry and the relevance of FSI on observed flow phenomena. Section 4 relates results of LSA to the numerical FSI-DNS. Section 5 concludes the paper.
2. Linear stability analysis
2.1. Derivation of the modified Orr–Sommerfeld equations with FSI extension term
To first understand the basic instability mechanisms occurring during the interaction of fluid and flexible leaflet tissue, we derive an approach incorporating FSI into the classic Orr–Sommerfeld equations. We conduct temporal LSA for multiple base flows (figure 1) in a simplified one-dimensional model with and without a flexible wall representing the valve leaflet.

Figure 1. Streamwise velocity field in the aortic root with inserted BHV. Base flow profiles are extracted along the green line (aortic jet) with boundary conditions representing a rigid wall (blue) and flexible wall (red) for the (![]() $b_1$) wall-bounded case, (
$b_1$) wall-bounded case, (![]() $b_2$) pure shear flow case and (
$b_2$) pure shear flow case and (![]() $b_3$) FSI case with flexible wall.
$b_3$) FSI case with flexible wall.
We study three different configurations. Configuration ![]() $b_1$ represents the aortic jet bounded by two fixed leaflets at
$b_1$ represents the aortic jet bounded by two fixed leaflets at ![]() $\tilde {y}=\pm 0.5$. Configuration
$\tilde {y}=\pm 0.5$. Configuration ![]() $b_2$ features the same aortic jet after leaving the valve orifice. Two rigid walls represent the aortic walls at
$b_2$ features the same aortic jet after leaving the valve orifice. Two rigid walls represent the aortic walls at ![]() $\tilde {y}=\pm 1$ and we assume zero flow between the aortic jet and the rigid walls. In configuration
$\tilde {y}=\pm 1$ and we assume zero flow between the aortic jet and the rigid walls. In configuration ![]() $b_3$ the aortic jet is bounded by flexible leaflets at
$b_3$ the aortic jet is bounded by flexible leaflets at ![]() $\tilde {y}=\pm 0.5$ which separate the jet from the zero-flow region between the flexible leaflets and the rigid aortic walls at
$\tilde {y}=\pm 0.5$ which separate the jet from the zero-flow region between the flexible leaflets and the rigid aortic walls at ![]() $\tilde {y}=\pm 1$. The definition of the base flow profile for the aortic jet is described in Appendix A. As the applied base flows are slightly asymmetric, we cannot exploit symmetry to retrieve strictly sinous or varicose modes, but need to consider the full domain.
$\tilde {y}=\pm 1$. The definition of the base flow profile for the aortic jet is described in Appendix A. As the applied base flows are slightly asymmetric, we cannot exploit symmetry to retrieve strictly sinous or varicose modes, but need to consider the full domain.
The derivation of the eigenvalue problem starts with the non-dimensional incompressible Navier–Stokes equations (non-dimensional quantities indicated with a tilde) including a force density ![]() $\tilde {\boldsymbol {f}}_{{FSI}}$ which we introduce to account for the interaction between fluid and flexible wall:
$\tilde {\boldsymbol {f}}_{{FSI}}$ which we introduce to account for the interaction between fluid and flexible wall:
 $$\begin{gather} \frac{\partial \tilde{\boldsymbol{u}}_{f}}{\partial t} + \rho_{f} (\tilde{\boldsymbol{u}}_{f} \boldsymbol{\cdot} \boldsymbol{\nabla}) \tilde{\boldsymbol{u}}_{f} ={-}\boldsymbol{\nabla} \widetilde{p_{f}} + \frac{1}{\textit{Re}} \nabla^2 \tilde{\boldsymbol{u}}_{f} + \tilde{\boldsymbol{f}}_{{FSI}}, \nonumber\\ \boldsymbol{\nabla} \boldsymbol{\cdot} \tilde{\boldsymbol{u}}_{f} = 0 . \end{gather}$$
$$\begin{gather} \frac{\partial \tilde{\boldsymbol{u}}_{f}}{\partial t} + \rho_{f} (\tilde{\boldsymbol{u}}_{f} \boldsymbol{\cdot} \boldsymbol{\nabla}) \tilde{\boldsymbol{u}}_{f} ={-}\boldsymbol{\nabla} \widetilde{p_{f}} + \frac{1}{\textit{Re}} \nabla^2 \tilde{\boldsymbol{u}}_{f} + \tilde{\boldsymbol{f}}_{{FSI}}, \nonumber\\ \boldsymbol{\nabla} \boldsymbol{\cdot} \tilde{\boldsymbol{u}}_{f} = 0 . \end{gather}$$
The non-dimensionalized force density ![]() $\tilde {\boldsymbol {f}}_{{FSI}}$ depends on a material-specific constant
$\tilde {\boldsymbol {f}}_{{FSI}}$ depends on a material-specific constant ![]() $\xi$ (derivation described in Appendix B) and the second derivative of the wall displacements
$\xi$ (derivation described in Appendix B) and the second derivative of the wall displacements ![]() $\tilde {\eta }_{-}$ at
$\tilde {\eta }_{-}$ at ![]() $\tilde {y}=\tilde {y}_{-}=-0.5$ and
$\tilde {y}=\tilde {y}_{-}=-0.5$ and ![]() $\tilde {\eta }_{+}$ at
$\tilde {\eta }_{+}$ at ![]() $\tilde {y}=\tilde {y}_{+}=0.5$ to model the effect of wall tension. It is given as
$\tilde {y}=\tilde {y}_{+}=0.5$ to model the effect of wall tension. It is given as
This formulation with the Dirac delta function ![]() $\delta (\kern0.7pt y)$ follows the immersed boundary concept by Peskin (Reference Peskin2002). A similar problem with a main focus on flexural stiffness of the structure has been studied by Lebbal, Alizard & Pier (Reference Lebbal, Alizard and Pier2022). Here, flexural stiffness (associated with the fourth derivative of the wall displacement) is neglected because of the thin membrane-like geometry of the leaflet.
$\delta (\kern0.7pt y)$ follows the immersed boundary concept by Peskin (Reference Peskin2002). A similar problem with a main focus on flexural stiffness of the structure has been studied by Lebbal, Alizard & Pier (Reference Lebbal, Alizard and Pier2022). Here, flexural stiffness (associated with the fourth derivative of the wall displacement) is neglected because of the thin membrane-like geometry of the leaflet.
A normal mode ansatz for the perturbation velocity components ![]() $[u^{\prime },v^{\prime } ]$ and perturbation displacements
$[u^{\prime },v^{\prime } ]$ and perturbation displacements ![]() $[\eta ^{\prime }_-,\eta ^{\prime }_+]$ is applied to the linearized extended Navier–Stokes equations:
$[\eta ^{\prime }_-,\eta ^{\prime }_+]$ is applied to the linearized extended Navier–Stokes equations:
with associated amplitudes ![]() $[\hat {u}(\tilde {y}), \hat {v}(\tilde {y}), \hat {\eta }_-, \hat {\eta }_+ ]$, wavenumber
$[\hat {u}(\tilde {y}), \hat {v}(\tilde {y}), \hat {\eta }_-, \hat {\eta }_+ ]$, wavenumber ![]() $\alpha$ and complex phase speed
$\alpha$ and complex phase speed ![]() $c = \omega /\alpha$.
$c = \omega /\alpha$.
The displacement amplitudes ![]() $[\hat {\eta }_-,\hat {\eta }_+]$ are substituted by the vertical velocity amplitude
$[\hat {\eta }_-,\hat {\eta }_+]$ are substituted by the vertical velocity amplitude ![]() $\hat {v}$ considering interface conditions at
$\hat {v}$ considering interface conditions at ![]() $\tilde {y}=[\tilde {y}_{-},\tilde {y}_{+}]$:
$\tilde {y}=[\tilde {y}_{-},\tilde {y}_{+}]$:
The insertion of the base flow profile ![]() $U = u(x_1,y_1,t ) / U_{max}$ leads to a modified Orr–Sommerfeld equation with FSI extension terms:
$U = u(x_1,y_1,t ) / U_{max}$ leads to a modified Orr–Sommerfeld equation with FSI extension terms:
 \begin{align} &
\left[(U-c)(\mathcal{D}^2-\alpha^2)c-U^{\prime\prime}c+\frac{\mathrm{i}}{\alpha{\textit{Re}}}
(\mathcal{D}^2-\alpha^2)^2 c\right.\nonumber\\ &\left.\quad
\vphantom{\frac{\mathrm{i}}{\alpha{\textit{Re}}}}
-\alpha^2\delta(\tilde{y}-\tilde{y}_{-})\xi-\alpha^2
\delta(\tilde{y}-\tilde{y}_{+})\xi \right] \hat{v} =
0,
\end{align}
\begin{align} &
\left[(U-c)(\mathcal{D}^2-\alpha^2)c-U^{\prime\prime}c+\frac{\mathrm{i}}{\alpha{\textit{Re}}}
(\mathcal{D}^2-\alpha^2)^2 c\right.\nonumber\\ &\left.\quad
\vphantom{\frac{\mathrm{i}}{\alpha{\textit{Re}}}}
-\alpha^2\delta(\tilde{y}-\tilde{y}_{-})\xi-\alpha^2
\delta(\tilde{y}-\tilde{y}_{+})\xi \right] \hat{v} =
0,
\end{align}
with ![]() $\mathcal {D} = {\rm d} / {\rm d}\tilde {y}$ and the Reynolds number defined as
$\mathcal {D} = {\rm d} / {\rm d}\tilde {y}$ and the Reynolds number defined as
with ![]() $L$ as the spanwise orifice of fully open, stable valve leaflets. In this linearized form the positions
$L$ as the spanwise orifice of fully open, stable valve leaflets. In this linearized form the positions ![]() $y_\pm$ are fixed at
$y_\pm$ are fixed at ![]() ${\pm }0.5$.
${\pm }0.5$.
The resulting quadratic eigenvalue problem
is transformed into a generalized eigenvalue problem (Tisseur Reference Tisseur2000)
with ![]() $\varphi = (c \hat {v},\hat {v})^{\rm T}$ and the boundary conditions
$\varphi = (c \hat {v},\hat {v})^{\rm T}$ and the boundary conditions ![]() $\hat {v}={\partial \hat {v}}/{\partial \tilde {y}} = 0$ at
$\hat {v}={\partial \hat {v}}/{\partial \tilde {y}} = 0$ at ![]() $\tilde {y}=\pm 1$.
$\tilde {y}=\pm 1$.
2.2. Temporal LSA
First, base flow ![]() $b_1$ with a flow profile between two rigid walls is analysed. It reflects the inflow condition of the aortic jet between two fixed leaflets before entering the AAo. The flow remains linearly stable up to
$b_1$ with a flow profile between two rigid walls is analysed. It reflects the inflow condition of the aortic jet between two fixed leaflets before entering the AAo. The flow remains linearly stable up to ![]() ${\textit {Re}}=5240$.
${\textit {Re}}=5240$.
Beforehand, we define a wavenumber region considered relevant in our later investigation of a finite valve leaflet. Taking into account its one-sided fixation and the finite leaflet length ![]() $H$, we define wavelengths
$H$, we define wavelengths ![]() $\lambda _{min} = H$ and
$\lambda _{min} = H$ and ![]() $\lambda _{max} = 4 H$ as
$\lambda _{max} = 4 H$ as ![]() $\alpha _0=5.55$ and
$\alpha _0=5.55$ and ![]() $\alpha _{1/4}=1.39$, respectively. As indicated by the schematic drawings in figure 2 and 5 the interval
$\alpha _{1/4}=1.39$, respectively. As indicated by the schematic drawings in figure 2 and 5 the interval ![]() $[\lambda _{min},\lambda _{max}]$ defines a range of typical wavelengths observed in fluttering valve leaflets (compare, for example, with figure 6 in Becsek et al. (Reference Becsek, Pietrasanta and Obrist2020)).
$[\lambda _{min},\lambda _{max}]$ defines a range of typical wavelengths observed in fluttering valve leaflets (compare, for example, with figure 6 in Becsek et al. (Reference Becsek, Pietrasanta and Obrist2020)).
The analysis is conducted for base flows ![]() $b_2$ and
$b_2$ and ![]() $b_3$ to quantify the effect of the flexible wall on stability regions. Growth rates
$b_3$ to quantify the effect of the flexible wall on stability regions. Growth rates ![]() $\omega _i = \mbox {Im}(c \alpha )$ for a physiologically relevant Reynolds number of
$\omega _i = \mbox {Im}(c \alpha )$ for a physiologically relevant Reynolds number of ![]() $Re=3318$ (see Appendix A) are shown in figure 2. The separation of zero-flow and jet-flow regions by a flexible wall decreases the range of unstable wavenumbers to
$Re=3318$ (see Appendix A) are shown in figure 2. The separation of zero-flow and jet-flow regions by a flexible wall decreases the range of unstable wavenumbers to ![]() $\alpha _3=[0,12.7]$ for
$\alpha _3=[0,12.7]$ for ![]() $b_3$ compared with the pure shear flow case
$b_3$ compared with the pure shear flow case ![]() $b_2$ which is unstable in
$b_2$ which is unstable in ![]() $\alpha _2=[0,19.7]$. Evaluating the corresponding range of unstable physical wavelengths
$\alpha _2=[0,19.7]$. Evaluating the corresponding range of unstable physical wavelengths ![]() $\lambda$, base flow
$\lambda$, base flow ![]() $b_2$ shows a minimum unstable wavelength of
$b_2$ shows a minimum unstable wavelength of ![]() $\lambda _2=0.28H$ while base flow
$\lambda _2=0.28H$ while base flow ![]() $b_3$ becomes unstable for a minimum wavelength of
$b_3$ becomes unstable for a minimum wavelength of ![]() $\lambda _3 = 0.44 H$. Also, the maximum growth rate of
$\lambda _3 = 0.44 H$. Also, the maximum growth rate of ![]() $b_3$ is smaller and located at a lower wavenumber (
$b_3$ is smaller and located at a lower wavenumber (![]() $\omega _{i,3,max} = 1.32$ at
$\omega _{i,3,max} = 1.32$ at ![]() $\alpha _{3}=6.0$ corresponding to
$\alpha _{3}=6.0$ corresponding to ![]() $\lambda _{3} = 0.93 H$) compared with pure shear flow
$\lambda _{3} = 0.93 H$) compared with pure shear flow ![]() $b_2$ (
$b_2$ (![]() $\omega _{i,2,max} = 1.62$ at
$\omega _{i,2,max} = 1.62$ at ![]() $\alpha _{2}=8.2$ corresponding to
$\alpha _{2}=8.2$ corresponding to ![]() $\lambda _{2}= 0.68 H$).
$\lambda _{2}= 0.68 H$).
Figure 3 for ![]() $\alpha _0$ and figure 4 for
$\alpha _0$ and figure 4 for ![]() $\alpha _{1/4}$ give further insight into the unstable mode pairs at
$\alpha _{1/4}$ give further insight into the unstable mode pairs at ![]() ${\textit {Re}}=3318$ of base flows
${\textit {Re}}=3318$ of base flows ![]() $b_2$ and
$b_2$ and ![]() $b_3$. Real and imaginary parts of the normalized eigenfunction
$b_3$. Real and imaginary parts of the normalized eigenfunction ![]() $\bar {v}$ are shown together with the corresponding reconstructed two-dimensional streamwise velocity fields
$\bar {v}$ are shown together with the corresponding reconstructed two-dimensional streamwise velocity fields ![]() $\tilde {u}$. The two-dimensional velocity field is reconstructed by
$\tilde {u}$. The two-dimensional velocity field is reconstructed by
with ![]() $\bar {u} = \mathrm {i} \mathcal {D} \bar {v} / \alpha$ based on the continuity equation. The wall displacement
$\bar {u} = \mathrm {i} \mathcal {D} \bar {v} / \alpha$ based on the continuity equation. The wall displacement ![]() $[\tilde {\eta }_{-}(\tilde {x}),\tilde {\eta }_{+}(\tilde {x})]$ is reconstructed by applying the previously defined interface conditions (2.5):
$[\tilde {\eta }_{-}(\tilde {x}),\tilde {\eta }_{+}(\tilde {x})]$ is reconstructed by applying the previously defined interface conditions (2.5):

Figure 3. Normalized amplitude ![]() $\tilde {v}$ and dimensionless streamwise velocity field
$\tilde {v}$ and dimensionless streamwise velocity field ![]() $\tilde {u}$ for
$\tilde {u}$ for ![]() $\epsilon = 0.08$ with streamlines of (a) the most unstable mode of base flow
$\epsilon = 0.08$ with streamlines of (a) the most unstable mode of base flow ![]() $b_2$, (b) the second most unstable mode of base flow
$b_2$, (b) the second most unstable mode of base flow ![]() $b_2$, (c) the most unstable mode of base flow
$b_2$, (c) the most unstable mode of base flow ![]() $b_3$ and (d) the second most unstable mode of base flow
$b_3$ and (d) the second most unstable mode of base flow ![]() $b_3$ for wavenumber
$b_3$ for wavenumber ![]() $\alpha _{0}$ at
$\alpha _{0}$ at ![]() ${\textit {Re}}=3318$ (corresponding to
${\textit {Re}}=3318$ (corresponding to ![]() $\boldsymbol {II}$ in figure 2).
$\boldsymbol {II}$ in figure 2).

Figure 4. Normalized amplitude ![]() $\bar {v}$ and dimensionless streamwise velocity field
$\bar {v}$ and dimensionless streamwise velocity field ![]() $\tilde {u}$ for
$\tilde {u}$ for ![]() $\epsilon = 0.08$ with streamlines of (a) the most unstable mode of base flow
$\epsilon = 0.08$ with streamlines of (a) the most unstable mode of base flow ![]() $b_2$, (b) the second most unstable mode of base flow
$b_2$, (b) the second most unstable mode of base flow ![]() $b_2$, (c) the most unstable mode of base flow
$b_2$, (c) the most unstable mode of base flow ![]() $b_3$ and (d) the second most unstable mode of base flow
$b_3$ and (d) the second most unstable mode of base flow ![]() $b_3$ for wavenumber
$b_3$ for wavenumber ![]() $\alpha _{1/4}$ at
$\alpha _{1/4}$ at ![]() ${\textit {Re}}=3318$ (corresponding to
${\textit {Re}}=3318$ (corresponding to ![]() $\boldsymbol {I}$ in figure 2).
$\boldsymbol {I}$ in figure 2).
For ![]() $\alpha _0$ in figure 3, two unstable modes exist for each base flow of which one affects the upper and the other the bottom shear layer (
$\alpha _0$ in figure 3, two unstable modes exist for each base flow of which one affects the upper and the other the bottom shear layer (![]() $b_2$) or flexible wall (
$b_2$) or flexible wall (![]() $b_3$). While the real part of the eigenfunction peaks at the distinct vertical location of maximum shear (
$b_3$). While the real part of the eigenfunction peaks at the distinct vertical location of maximum shear (![]() $b_2$) or flexible wall (
$b_2$) or flexible wall (![]() $b_3$), the location of the imaginary maximum of smaller amplitude is shifted slightly towards the jet core. Considering the reconstructed two-dimensional flow fields, base flow
$b_3$), the location of the imaginary maximum of smaller amplitude is shifted slightly towards the jet core. Considering the reconstructed two-dimensional flow fields, base flow ![]() $b_2$ shows classical Kelvin–Helmholtz (KH) flow features within the shear layer. The addition of the flexible wall for base flow
$b_2$ shows classical Kelvin–Helmholtz (KH) flow features within the shear layer. The addition of the flexible wall for base flow ![]() $b_3$ leads to similar flow patterns in the wall region at either
$b_3$ leads to similar flow patterns in the wall region at either ![]() $\tilde {y}_{-}$ or
$\tilde {y}_{-}$ or ![]() $\tilde {y}_{+}$. For smaller wavenumbers such as
$\tilde {y}_{+}$. For smaller wavenumbers such as ![]() $\alpha _{1/4}$ in figure 4, we can observe an interaction between both shear layers (
$\alpha _{1/4}$ in figure 4, we can observe an interaction between both shear layers (![]() $b_2$) or flexible walls (
$b_2$) or flexible walls (![]() $b_3$). While higher wavenumbers show a one-sided eigenfunction destabilizing the flow at only one of the vertical locations
$b_3$). While higher wavenumbers show a one-sided eigenfunction destabilizing the flow at only one of the vertical locations ![]() $\tilde {y}_{-}$ or
$\tilde {y}_{-}$ or ![]() $\tilde {y}_{+}$, lower wavenumbers are associated with eigenfunctions which couple the modes of both shear layers (
$\tilde {y}_{+}$, lower wavenumbers are associated with eigenfunctions which couple the modes of both shear layers (![]() $b_2$) or flexible walls (
$b_2$) or flexible walls (![]() $b_3$).
$b_3$).
When evaluating the neutral stability curves in figure 5, the critical Reynolds number for KH modes corresponding to configuration ![]() $b_2$ is higher (
$b_2$ is higher (![]() ${\textit {Re}}_{KH} = 299$) than for FSI modes corresponding to configuration
${\textit {Re}}_{KH} = 299$) than for FSI modes corresponding to configuration ![]() $b_3$ (
$b_3$ (![]() ${\textit {Re}}_{FSI} = 184$). An overlapping region of both KH and FSI modes exists for a large Reynolds number and wavenumber range which includes physiologically relevant Reynolds numbers and wavenumbers. Therefore, both instabilities (KH and FSI) are suspected to be present simultaneously after valve opening.
${\textit {Re}}_{FSI} = 184$). An overlapping region of both KH and FSI modes exists for a large Reynolds number and wavenumber range which includes physiologically relevant Reynolds numbers and wavenumbers. Therefore, both instabilities (KH and FSI) are suspected to be present simultaneously after valve opening.

Figure 5. Neutral stability curves for pure shear flow (base flow ![]() $b_2$, indicated in blue) and FSI case (base flow
$b_2$, indicated in blue) and FSI case (base flow ![]() $b_3$, indicated in green).
$b_3$, indicated in green).
Figure 6 shows the dependency of the eigenvalues on wavenumber ![]() $\alpha$ for base flows
$\alpha$ for base flows ![]() $b_2$ and
$b_2$ and ![]() $b_3$. The growth rate
$b_3$. The growth rate ![]() $\omega _i = \mbox {Im}(c \alpha )$ of the unstable eigenmode pair is displayed against the phase speed
$\omega _i = \mbox {Im}(c \alpha )$ of the unstable eigenmode pair is displayed against the phase speed ![]() $c_r = \omega _r/\alpha$ at
$c_r = \omega _r/\alpha$ at ![]() ${\textit {Re}}=3318$. In general, the phase speed
${\textit {Re}}=3318$. In general, the phase speed ![]() $c_r$ decreases with increasing wavenumber for both base flow configurations. Growth rates
$c_r$ decreases with increasing wavenumber for both base flow configurations. Growth rates ![]() $\omega _i$ of KH modes (base flow
$\omega _i$ of KH modes (base flow ![]() $b_2$) peak at higher wavenumber compared with FSI-related modes (base flow
$b_2$) peak at higher wavenumber compared with FSI-related modes (base flow ![]() $b_3$). The FSI-related modes generally grow slower than KH modes; however, phase speeds are higher. For
$b_3$). The FSI-related modes generally grow slower than KH modes; however, phase speeds are higher. For ![]() ${\textit {Re}}=3318$, the most unstable KH mode has a phase speed
${\textit {Re}}=3318$, the most unstable KH mode has a phase speed ![]() $c_r = \omega _r / \alpha$ of
$c_r = \omega _r / \alpha$ of ![]() $c_{r,2}(\alpha _2) = 0.424$ while the most unstable FSI-related mode is faster with a phase speed of
$c_{r,2}(\alpha _2) = 0.424$ while the most unstable FSI-related mode is faster with a phase speed of ![]() $c_{r,3}(\alpha _3) = 0.649$. In conclusion, unstable KH modes seem to grow faster than unstable FSI-related modes for their unstable wavenumber range. Also, we observe less dependency of the phase speed of the KH modes on the wavenumber. In comparison, FSI-related modes depend stronger on the wavenumber. While small wavelengths travel slowly, the phase speed of higher wavelengths is higher and varies more related to the wavenumber.
$c_{r,3}(\alpha _3) = 0.649$. In conclusion, unstable KH modes seem to grow faster than unstable FSI-related modes for their unstable wavenumber range. Also, we observe less dependency of the phase speed of the KH modes on the wavenumber. In comparison, FSI-related modes depend stronger on the wavenumber. While small wavelengths travel slowly, the phase speed of higher wavelengths is higher and varies more related to the wavenumber.

Figure 6. Path of locus for the unstable eigenmode pairs of base flow ![]() $b_2$ (pure shear flow, blue) and base flow
$b_2$ (pure shear flow, blue) and base flow ![]() $b_3$ (flexible wall, green) for wavenumbers
$b_3$ (flexible wall, green) for wavenumbers ![]() $\alpha$ at Reynolds number
$\alpha$ at Reynolds number ![]() ${\textit {Re}}=3318$.
${\textit {Re}}=3318$.
3. Numerical FSI simulations
3.1. Governing equations and numerical method
After the investigation of instability mechanisms in a simplified one-dimensional model, we now increase the modelling complexity by conducting highly-resolved two-dimensional FSI simulations of a parametrized aortic geometry. Hereby, we aim to obtain a deeper insight into more complex flow features as well as their temporal and spatial evolution.
The interaction of valve and blood flow is implemented within an in-house high-fidelity FSI solver developed for applications including blood flow and soft tissue on hybrid high-performance computing platforms. The flow field is solved by a GPU-accelerated high-order Navier–Stokes solver based on Henniger, Obrist & Kleiser (Reference Henniger, Obrist and Kleiser2010) and Zolfaghari & Obrist (Reference Zolfaghari and Obrist2021) on a structured, staggered grid using the incompressible Navier–Stokes equations:
 \begin{equation} \left.\begin{gathered} \rho_{f} \frac{\partial \boldsymbol{u}_{f}}{\partial t} + \rho_{f} (\boldsymbol{u}_{f} \boldsymbol{\cdot} \boldsymbol{\nabla}) \boldsymbol{u}_{f} ={-}\boldsymbol{\nabla} p_{f} +\mu_{f} \Delta \boldsymbol{u}_{f} + \boldsymbol{f} ,\\ \boldsymbol{\nabla} \boldsymbol{\cdot} \boldsymbol{u}_{f} = 0, \end{gathered}\right\} \end{equation}
\begin{equation} \left.\begin{gathered} \rho_{f} \frac{\partial \boldsymbol{u}_{f}}{\partial t} + \rho_{f} (\boldsymbol{u}_{f} \boldsymbol{\cdot} \boldsymbol{\nabla}) \boldsymbol{u}_{f} ={-}\boldsymbol{\nabla} p_{f} +\mu_{f} \Delta \boldsymbol{u}_{f} + \boldsymbol{f} ,\\ \boldsymbol{\nabla} \boldsymbol{\cdot} \boldsymbol{u}_{f} = 0, \end{gathered}\right\} \end{equation}
with the fluid density ![]() $\rho _{f}$, dynamic viscosity
$\rho _{f}$, dynamic viscosity ![]() $\mu _{f}$, pressure
$\mu _{f}$, pressure ![]() $p_f$, time
$p_f$, time ![]() $t$ and, in the present case, two-dimensional fluid velocity field
$t$ and, in the present case, two-dimensional fluid velocity field ![]() $\boldsymbol {u}_{f} = [u_{f,x},u_{f,y}]$. The added force term
$\boldsymbol {u}_{f} = [u_{f,x},u_{f,y}]$. The added force term ![]() $\boldsymbol {f}$ accounts for FSI.
$\boldsymbol {f}$ accounts for FSI.
Temporal discretization is realized by a third-order Runge–Kutta time stepping while the fluid is spatially discretized by a sixth-order finite difference scheme.
An unstructured grid is used for the discretization of the structural domain, which is solved by a finite element solver using the full elastodynamic equations:
with the structural density ![]() $\rho _{s}$, the displacement field
$\rho _{s}$, the displacement field ![]() $\boldsymbol {u}_{s}$ and the Piola–Kirchhoff stress tensor
$\boldsymbol {u}_{s}$ and the Piola–Kirchhoff stress tensor ![]() $\boldsymbol{\mathsf{P}}$.
$\boldsymbol{\mathsf{P}}$.
The interaction of fluid and structure motion is realized by a modified immersed boundary method based on variational transfer with the following interface conditions:
 \begin{equation} \left.\begin{gathered} \boldsymbol{u}_{f} = \frac{\partial \boldsymbol{u}_{s}}{\partial t} ,\\ J^{{-}1} \boldsymbol{\mathsf{P}} \boldsymbol{\mathsf{F}}^{\rm T} \boldsymbol{n} = {{{\boldsymbol{\sigma}}}}_{f} \boldsymbol{n}, \end{gathered}\right\} \end{equation}
\begin{equation} \left.\begin{gathered} \boldsymbol{u}_{f} = \frac{\partial \boldsymbol{u}_{s}}{\partial t} ,\\ J^{{-}1} \boldsymbol{\mathsf{P}} \boldsymbol{\mathsf{F}}^{\rm T} \boldsymbol{n} = {{{\boldsymbol{\sigma}}}}_{f} \boldsymbol{n}, \end{gathered}\right\} \end{equation}
including the Cauchy stress ![]() $\boldsymbol{\sigma} _{f}$ and the deformation gradient
$\boldsymbol{\sigma} _{f}$ and the deformation gradient ![]() $\boldsymbol{\mathsf{F}} = \boldsymbol {\nabla } \boldsymbol {u}_{s} + \boldsymbol{\mathsf{I}}$ with its associated determinant
$\boldsymbol{\mathsf{F}} = \boldsymbol {\nabla } \boldsymbol {u}_{s} + \boldsymbol{\mathsf{I}}$ with its associated determinant ![]() $J = \textrm {det} \boldsymbol{\mathsf{F}}$.
$J = \textrm {det} \boldsymbol{\mathsf{F}}$.
Details of the FSI solver as well as its experimental and numerical validation can be found in Nestola et al. (Reference Nestola, Becsek, Zolfaghari, Zulian, De Marinis, Krause and Obrist2019) and Becsek et al. (Reference Becsek, Pietrasanta and Obrist2020).
The two-dimensional, rectangular fluid domain is resolved with a structured grid of ![]() $2209 \times 897$ points on a domain of an extent of
$2209 \times 897$ points on a domain of an extent of ![]() $11.18r_{A} \times 4.55r_{A}$ with
$11.18r_{A} \times 4.55r_{A}$ with ![]() $r_A$ as the annular radius in order to resolve the onset of hydrodynamic instabilities. Grid stretching was applied which reduces the minimal mesh width to around
$r_A$ as the annular radius in order to resolve the onset of hydrodynamic instabilities. Grid stretching was applied which reduces the minimal mesh width to around ![]() $35\,\mathrm {\mu }$m in the immediate vicinity of the valve. The unstructured solid grid consists of approximately
$35\,\mathrm {\mu }$m in the immediate vicinity of the valve. The unstructured solid grid consists of approximately ![]() $11\,300$ triangular elements.
$11\,300$ triangular elements.
With a time step size of ![]() $1\,\mathrm {\mu }$s, the computational time for the simulation of the systolic acceleration (200 ms) amounts to around 1500 node hours on
$1\,\mathrm {\mu }$s, the computational time for the simulation of the systolic acceleration (200 ms) amounts to around 1500 node hours on ![]() $8$ nodes of a Cray XC40/XC50 high-performance computer.
$8$ nodes of a Cray XC40/XC50 high-performance computer.
3.2. Two-dimensional parametrized aortic model
The problem set-up in figure 7(a) is a model of an aortic root with an inserted bioprosthetic valve. The actual threefold symmetry of the three-dimensional aortic root with three sinus bulbs and corresponding valve leaflets is simplified to a two-dimensional problem by considering a mirrored longitudinal cut through the middle plane of a leaflet. Generally, the structural domain is divided into aortic wall, valve stent and valve leaflet and separated in the fluid regions as annulus (![]() $\delta \varOmega _{A}$), sinus (
$\delta \varOmega _{A}$), sinus (![]() $\delta \varOmega _{S}$) and AAo (
$\delta \varOmega _{S}$) and AAo (![]() $\delta \varOmega _{AAo}$). The aortic wall geometry is based on data of Haj-Ali et al. (Reference Haj-Ali, Marom, Ben Zekry, Rosenfeld and Raanani2012) and Reul et al. (Reference Reul, Vahlbruch, Giersiepen, Schmitz-Rode, Hirtz and Effert1990) and the curvature of the valve leaflets on the bioprosthetic aortic valve Edwards Intuity Elite 21 (Edwards Lifesciences, Irvine, CA, USA). Geometrical parameters are listed in table 1 which are constant throughout each analysed case.
$\delta \varOmega _{AAo}$). The aortic wall geometry is based on data of Haj-Ali et al. (Reference Haj-Ali, Marom, Ben Zekry, Rosenfeld and Raanani2012) and Reul et al. (Reference Reul, Vahlbruch, Giersiepen, Schmitz-Rode, Hirtz and Effert1990) and the curvature of the valve leaflets on the bioprosthetic aortic valve Edwards Intuity Elite 21 (Edwards Lifesciences, Irvine, CA, USA). Geometrical parameters are listed in table 1 which are constant throughout each analysed case.
Table 1. Constant parameters of the parametrized aortic model relative to the annular radius ![]() $r_A$.
$r_A$.

We additionally introduce the parameters sinus height (![]() $h_{STJ}$) and AAo radius (
$h_{STJ}$) and AAo radius (![]() $r_{AAo}$) in order to evaluate the influence of aortic wall geometry on instabilities in the aortic root. Parametrization values (table 2) were chosen according to realistic anatomical ranges extracted from various studies on aortic root morphology by Bahlmann et al. (Reference Bahlmann, Nienaber, Cramariuc, Gohlke-Baerwolf, Ray, Devereux, Wachtell, Kuck, Davidsen and Gerdts2011), Buellesfeld et al. (Reference Buellesfeld2013), Mirea et al. (Reference Mirea, Maffessanti, Gripari, Tamborini, Muratori, Fusini, Claudia, Fiorentini, Plesea and Pepi2013), Vriz et al. (Reference Vriz2014) and Boraita et al. (Reference Boraita, Heras, Morales, Marina-Breysse, Canda, Rabadan, Barriopedro, Varela, De La Rosa and Tuñón2016). As a result, we define three cases: initial configuration (indicated as case A), increased sinus height (indicated as case B) and decreased AAo radius (indicated as case C).
$r_{AAo}$) in order to evaluate the influence of aortic wall geometry on instabilities in the aortic root. Parametrization values (table 2) were chosen according to realistic anatomical ranges extracted from various studies on aortic root morphology by Bahlmann et al. (Reference Bahlmann, Nienaber, Cramariuc, Gohlke-Baerwolf, Ray, Devereux, Wachtell, Kuck, Davidsen and Gerdts2011), Buellesfeld et al. (Reference Buellesfeld2013), Mirea et al. (Reference Mirea, Maffessanti, Gripari, Tamborini, Muratori, Fusini, Claudia, Fiorentini, Plesea and Pepi2013), Vriz et al. (Reference Vriz2014) and Boraita et al. (Reference Boraita, Heras, Morales, Marina-Breysse, Canda, Rabadan, Barriopedro, Varela, De La Rosa and Tuñón2016). As a result, we define three cases: initial configuration (indicated as case A), increased sinus height (indicated as case B) and decreased AAo radius (indicated as case C).
Table 2. Variable parameters of the parametrized aortic model relative to the annular radius ![]() $r_A$ with the parameters sinus height
$r_A$ with the parameters sinus height ![]() $h_{STJ}$ and AAo radius
$h_{STJ}$ and AAo radius ![]() $r_{AAo}$. Evaluated configurations are indicated as initial configuration (A), increased sinus height (B) and decreased AAo radius (C).
$r_{AAo}$. Evaluated configurations are indicated as initial configuration (A), increased sinus height (B) and decreased AAo radius (C).

The opening phase of bioprosthetic aortic valves is completed after a duration of around 20 ms. Thereafter, the valve remains in the open position before the asynchronous closing starts at a third of the full cardiac cycle corresponding to a physical time of about 0.3 s (Vennemann et al. Reference Vennemann, Rösgen, Heinisch and Obrist2018). As we aim to investigate hydrodynamic instabilities initiating laminar–turbulent transition leading to turbulent flow during early systole as shown in Becsek et al. (Reference Becsek, Pietrasanta and Obrist2020), we limit our study to the systolic acceleration phase of a duration of about 0.2 s as defined in figure 7(b).
Inflow conditions are enforced by the fringe region technique described in Nordström, Nordin & Henningson (Reference Nordström, Nordin and Henningson1999) for a periodic fluid domain. A penalization term ![]() $\boldsymbol {f}_{{fringe}} (\boldsymbol {x})$ is added to the right-hand side of the Navier–Stokes equations within a fringe region located at the left ventricular outflow tract as described in Becsek et al. (Reference Becsek, Pietrasanta and Obrist2020). A physiological inflow profile at a defined cardiac output is ensured by tuning of the fringe function. By suppressing lateral velocity components within the fringe region, entering fluctuations due to the periodic fluid domain are damped. Here, we impose a pressure difference of 8 mmHg across the fringe region corresponding to the average systolic transvalvular pressure gradient.
$\boldsymbol {f}_{{fringe}} (\boldsymbol {x})$ is added to the right-hand side of the Navier–Stokes equations within a fringe region located at the left ventricular outflow tract as described in Becsek et al. (Reference Becsek, Pietrasanta and Obrist2020). A physiological inflow profile at a defined cardiac output is ensured by tuning of the fringe function. By suppressing lateral velocity components within the fringe region, entering fluctuations due to the periodic fluid domain are damped. Here, we impose a pressure difference of 8 mmHg across the fringe region corresponding to the average systolic transvalvular pressure gradient.
The fluid is modelled as incompressible and Newtonian with material properties similar to those of blood (![]() $\mu _{f}=0.004$ Pa s,
$\mu _{f}=0.004$ Pa s, ![]() $\rho _{f}=1050$ kg m
$\rho _{f}=1050$ kg m![]() $^{-3}$). The aortic wall and the valve stent are assumed to be rigid while we apply a hyperelastic, nonlinear neo-Hookean material model with a shear modulus of
$^{-3}$). The aortic wall and the valve stent are assumed to be rigid while we apply a hyperelastic, nonlinear neo-Hookean material model with a shear modulus of ![]() $\mu _{s}=5.0\times 10^{5}$ Pa to the flexible valve leaflets. The shear modulus was tuned in order to match leaflet oscillation amplitudes extracted from a less resolved three-dimensional case of a bioprosthetic valve with leaflets modelled by a fibre-reinforced Holzapfel–Gasser–Ogden model (Holzapfel, Gasser & Ogden Reference Holzapfel, Gasser and Ogden2000). Figure 8 shows the temporal evolution of the leaflet tip displacement for four shear moduli previously applied in studies of Hiromi Spühler & Hoffman (Reference Hiromi Spühler and Hoffman2020) (
$\mu _{s}=5.0\times 10^{5}$ Pa to the flexible valve leaflets. The shear modulus was tuned in order to match leaflet oscillation amplitudes extracted from a less resolved three-dimensional case of a bioprosthetic valve with leaflets modelled by a fibre-reinforced Holzapfel–Gasser–Ogden model (Holzapfel, Gasser & Ogden Reference Holzapfel, Gasser and Ogden2000). Figure 8 shows the temporal evolution of the leaflet tip displacement for four shear moduli previously applied in studies of Hiromi Spühler & Hoffman (Reference Hiromi Spühler and Hoffman2020) (![]() $\mu _{s}=3.3\times 10^{4}$ Pa), Chandra et al. (Reference Chandra, Rajamannan and Sucosky2012) (
$\mu _{s}=3.3\times 10^{4}$ Pa), Chandra et al. (Reference Chandra, Rajamannan and Sucosky2012) (![]() $\mu _{s}=1.2\times 10^{5}$ Pa), Bavo et al. (Reference Bavo, Rocatello, Iannaccone, Degroote, Vierendeels and Segers2016) (
$\mu _{s}=1.2\times 10^{5}$ Pa), Bavo et al. (Reference Bavo, Rocatello, Iannaccone, Degroote, Vierendeels and Segers2016) (![]() $\mu _{s}=3.4\times 10^{5}$ Pa) and De Hart et al. (Reference De Hart, Peters, Schreurs and Baaijens2000) (
$\mu _{s}=3.4\times 10^{5}$ Pa) and De Hart et al. (Reference De Hart, Peters, Schreurs and Baaijens2000) (![]() $\mu _{s}=5.0\times 10^{5}$ Pa) in comparison with the three-dimensional simulation.
$\mu _{s}=5.0\times 10^{5}$ Pa) in comparison with the three-dimensional simulation.

Figure 8. Temporal evolution of leaflet tip displacements perpendicular to the longitudinal aortic axis for four shear moduli according to two-dimensional studies for a neo-Hookean model of (a) Hiromi Spühler & Hoffman (Reference Hiromi Spühler and Hoffman2020), (b) Chandra, Rajamannan & Sucosky (Reference Chandra, Rajamannan and Sucosky2012), (c) Bavo et al. (Reference Bavo, Rocatello, Iannaccone, Degroote, Vierendeels and Segers2016) and (d) De Hart et al. (Reference De Hart, Peters, Schreurs and Baaijens2000) in comparison with a less resolved three-dimensional reference study using a Holzapfel–Gasser–Ogden (HGO) model.
3.3. Numerical results
3.3.1. The influence of FSI: rigid versus flexible leaflet
To assess the effect of FSI on laminar–turbulent transition, we compare the base configuration starting with closed leaflets (case A) from figure 7 with a rigid leaflet case fixed in open position (indicated as AR). The rigid leaflet shape of case AR is extracted from the flexible case A immediately after full valve opening. In particular, we pick the deformed leaflet shape prior to the onset of (a) leaflet motion and (b) non-zero transversal velocities within the shear layer created in the wake of the leaflet (hereafter referred to as ‘leaflet shear layer’).
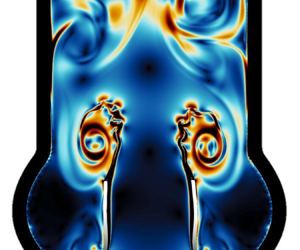
Figure 9 shows the instantaneous viscous shear stress magnitude ![]() $|{{{\tau }}}|$ at five time instances for the rigid leaflet case AR (top row) and the flexible leaflet case A (bottom row). Three main flow phenomena seem to occur sequentially for both rigid and flexible cases:
$|{{{\tau }}}|$ at five time instances for the rigid leaflet case AR (top row) and the flexible leaflet case A (bottom row). Three main flow phenomena seem to occur sequentially for both rigid and flexible cases:
(i) Starting vortex (figure 9a). Early during systolic acceleration, a distinct starting vortex is formed which is advected downstream.
(ii) Vortex–wall interaction (figure 9b–d). The starting vortex is advected and elongates in the streamwise direction. Due to the transversal confinement by the aortic wall and the associated no-slip boundary condition at the wall, a secondary vortex is created upstream of the starting vortex. This smaller vortex rebounds from the aortic wall and moves towards the leaflet shear layer. The ejection of a secondary vortex when a sufficiently strong primary vortex (here the starting vortex) impinges at a wall is well documented (Walker et al. Reference Walker, Smith, Cerra and Doligalski1987; Orlandi & Verzicco Reference Orlandi and Verzicco1993).
(iii) Shear layer instability (figure 9e). When the secondary vortex reaches the outer side of the shear layer, we observe growing shear layer instabilities.

Figure 9. Instantaneous viscous shear stress magnitude ![]() $| {{{\tau }}} |$ for (AR) rigid leaflet case and (A) flexible leaflet case for aortic wall configuration A at (a)
$| {{{\tau }}} |$ for (AR) rigid leaflet case and (A) flexible leaflet case for aortic wall configuration A at (a) ![]() $t=0.10$ s, (b)
$t=0.10$ s, (b) ![]() $t=0.1175$ s, (c)
$t=0.1175$ s, (c) ![]() $t=0.135$ s, (d)
$t=0.135$ s, (d) ![]() $t=0.1525$ s and (e)
$t=0.1525$ s and (e) ![]() $t=0.17$ s. Secondary vortical structures forming after the impingement of the starting (primary) vortex on the aortic wall are shown by the red arrows.
$t=0.17$ s. Secondary vortical structures forming after the impingement of the starting (primary) vortex on the aortic wall are shown by the red arrows.
Both cases show growing vortical structures within the shear layer at a similar time which suggests that the general mechanisms do not seem to be influenced by the open or closed starting position of the rigid or flexible leaflet, respectively. Moreover, the occurrence of shear layer instabilities seems to be independent of mechanisms related to FSI. This is further supported by the observation that the flexible leaflets of case A remain stable during the initial onset of vortical structures reminiscent of KH-like vortex roll-up within the shear layer. This is in agreement with the LSA predicting KH modes for this flow regime.
The impact of FSI on the downstream flow field starts to become relevant during the growth phase of the shear layer instability. Figure 10 shows instantaneous shear stress magnitudes for the flexible leaflet case at time instances after those displayed in figure 9. As predicted by LSA, we observe an FSI-related instability of the flexible leaflets. While figure 10(a) shows the onset of leaflet motion, we observe a stronger influence of leaflet motion on the downstream flow field by vortex shedding from the leaflet tips in figure 10(b). This is consistent with the repeated formation of vortex rings at the valve orifice associated with oscillatory leaflet motion shown for the three-dimensional model by Becsek et al. (Reference Becsek, Pietrasanta and Obrist2020). Eventually, figure 10(c) possibly indicates another instability leading to small-scale vortices within the larger vortex downstream of the leaflets.

Figure 10. Instantaneous viscous shear stress magnitude ![]() $|{{{\tau }}} |$ for aortic wall configuration A at (a)
$|{{{\tau }}} |$ for aortic wall configuration A at (a) ![]() $t=0.1875$ s, (b)
$t=0.1875$ s, (b) ![]() $t=0.1945$ s and (c)
$t=0.1945$ s and (c) ![]() $t=0.2$ s.
$t=0.2$ s.
3.3.2. Effect of aortic root geometry
To assess the influence of morphological features on instability mechanisms, we simulate the cases A (base configuration), B (increased sinus height) and C (decreased AAo radius) as defined in table 2. Instantaneous viscous shear stress magnitudes at multiple time instances throughout systolic acceleration are shown in figure 11. Cases A and B display similar temporal and spatial evolution of the starting vortex. In contrast, case C exhibits an early elongation of the starting vortex caused by the earlier vortex–wall interaction due to the narrower AAo. As described before, confinement of the downstream flow region causes the formation of a second smaller vortex approaching the leaflet shear layer (red arrows in figure 11) which is followed by instability in the leaflet shear layers. In case C, this shear layer instability appears earlier than in cases A and B (see figure 11b). Likewise, the second shear-related instability leading to smaller shear-layer vortices (green arrows) occurs also earlier for case C than for cases A and B.

Figure 11. Instantaneous viscous shear stress magnitude ![]() $|{{{\tau }}} |$ for aortic wall configurations (A) initial configuration, (B) increased sinus height and (C) decreased AAo radius at (a)
$|{{{\tau }}} |$ for aortic wall configurations (A) initial configuration, (B) increased sinus height and (C) decreased AAo radius at (a) ![]() $t=0.125$ s, (b)
$t=0.125$ s, (b) ![]() $t=0.15$ s, (c)
$t=0.15$ s, (c) ![]() $t=0.175$ s and (d)
$t=0.175$ s and (d) ![]() $t=0.20$s. Secondary vortical structures forming after the impingement of the starting (primary) vortex on the aortic wall are shown by the red arrows.
$t=0.20$s. Secondary vortical structures forming after the impingement of the starting (primary) vortex on the aortic wall are shown by the red arrows.
Figure 12 shows the evolution of the transversal velocity at six leaflet thicknesses, ![]() $x=6t_L$, downstream of the instantaneous leaflet position as well as the transversal leaflet tip velocity. First, we observe the initial opening of the leaflet (completed at
$x=6t_L$, downstream of the instantaneous leaflet position as well as the transversal leaflet tip velocity. First, we observe the initial opening of the leaflet (completed at ![]() $t\approx 0.08$ s) which is almost identical for all three aortic configurations. After the opening phase, the leaflet remains in a stable position until the onset of transversal leaflet and fluid motion. For cases A and B, this occurs at
$t\approx 0.08$ s) which is almost identical for all three aortic configurations. After the opening phase, the leaflet remains in a stable position until the onset of transversal leaflet and fluid motion. For cases A and B, this occurs at ![]() $t\approx 0.13$ s, while we observe an earlier onset of leaflet and fluid motion for case C (
$t\approx 0.13$ s, while we observe an earlier onset of leaflet and fluid motion for case C (![]() $t\approx 0.11$ s). After this onset, we find growing oscillations of leaflet tip and fluid at a frequency of approximately 55 Hz. These oscillations are reminiscent of leaflet fluttering observed in BHVs in experimental studies (Vennemann et al. Reference Vennemann, Rösgen, Heinisch and Obrist2018).
$t\approx 0.11$ s). After this onset, we find growing oscillations of leaflet tip and fluid at a frequency of approximately 55 Hz. These oscillations are reminiscent of leaflet fluttering observed in BHVs in experimental studies (Vennemann et al. Reference Vennemann, Rösgen, Heinisch and Obrist2018).

Figure 12. Temporal evolution of transversal fluid velocities extracted at ![]() $x=6t_L$ downstream of the instantaneous leaflet tip position (blue) and transversal leaflet tip velocity (black) for aortic wall configurations (a) initial configuration (case A), (b) increased sinus height (case B) and (c) decreased AAo radius (case C) with the onset of transversal oscillations indicated by the red arrow.
$x=6t_L$ downstream of the instantaneous leaflet tip position (blue) and transversal leaflet tip velocity (black) for aortic wall configurations (a) initial configuration (case A), (b) increased sinus height (case B) and (c) decreased AAo radius (case C) with the onset of transversal oscillations indicated by the red arrow.
Although the same qualitative sequence of flow phenomena shows for every aortic wall configuration, there are major differences in the timing and onset of the different mechanisms. In particular, a shorter distance between leaflet tip and aortic wall appears to lead to earlier shear layer perturbations.
4. Comparison of numerical results and LSA
Finally, we compare the results from LSA (§ 2) with flow patterns observed in numerical simulations (§ 3). Previously, we already confirmed in both approaches the consistent presence of KH and FSI instabilities for the investigated flow regime at ![]() ${\textit {Re}}=3318$.
${\textit {Re}}=3318$.
Figure 13(a) displays the temporal evolution of transversal velocity profiles that were obtained along the leaflet shear layer downstream of the valve for case AR (rigid leaflet). In this figure, we can identify the onset and propagation of the KH instability as ‘ridges’. The red line in figure 13(a) indicates the phase speed ![]() $c_{r,2}(\alpha _2)$ of KH instabilities according to the LSA for the configuration
$c_{r,2}(\alpha _2)$ of KH instabilities according to the LSA for the configuration ![]() $b_2$ (free jet). There is a reasonably good agreement between the propagation speed of the ridges and the phase speed
$b_2$ (free jet). There is a reasonably good agreement between the propagation speed of the ridges and the phase speed ![]() $c_{r,2}$ especially before
$c_{r,2}$ especially before ![]() $t\approx 0.17$ s when the amplitude of the instability is still small.
$t\approx 0.17$ s when the amplitude of the instability is still small.

Figure 13. (a) Case AR: transversal velocity profiles over time along the leaflet shear layer. Red line: phase speed ![]() $c_{r,2}(\alpha _2)$ for base flow
$c_{r,2}(\alpha _2)$ for base flow ![]() $b_2$ (pure shear flow). (b) Case A: transversal velocity profiles over time along the leaflet shear layer (top row) and leaflet shape over time (bottom row). Red line: phase speed
$b_2$ (pure shear flow). (b) Case A: transversal velocity profiles over time along the leaflet shear layer (top row) and leaflet shape over time (bottom row). Red line: phase speed ![]() $c_{r,3}(\alpha _3)$ for base flow
$c_{r,3}(\alpha _3)$ for base flow ![]() $b_3$ (flexible wall). Black lines indicate the upstream propagation of velocity ‘ridges’. (c) Streamwise velocity field in the leaflet wake at
$b_3$ (flexible wall). Black lines indicate the upstream propagation of velocity ‘ridges’. (c) Streamwise velocity field in the leaflet wake at ![]() $t=0.14$ s. (d) Envelope
$t=0.14$ s. (d) Envelope ![]() $G(t)$ of transversal velocity at
$G(t)$ of transversal velocity at ![]() $x=6t_L$ for case AR (
$x=6t_L$ for case AR (![]() $G_{AR}|_{x=6t_L}$) and case A (
$G_{AR}|_{x=6t_L}$) and case A (![]() $G_{A}|_{x=6t_L}$) and of the leaflet tip for case A (
$G_{A}|_{x=6t_L}$) and of the leaflet tip for case A (![]() $G_{A}|_{x=0}$). Dashed lines show
$G_{A}|_{x=0}$). Dashed lines show ![]() $\exp (\omega _{i,2,max}t)$ of base flow
$\exp (\omega _{i,2,max}t)$ of base flow ![]() $b_2$ (shear flow) and
$b_2$ (shear flow) and ![]() $\exp (\omega _{i,3,max}t)$ of base flow
$\exp (\omega _{i,3,max}t)$ of base flow ![]() $b_3$ (flexible wall).
$b_3$ (flexible wall).
Figure 13(b) shows the transversal velocity profiles in the leaflet shear layer of case A (flexible leaflet) and the deformation of the leaflet beneath. The phase speeds ![]() $c_{r,2}(\alpha _2)$ (free jet) and
$c_{r,2}(\alpha _2)$ (free jet) and ![]() $c_{r,3}(\alpha _3)$ (jet with flexible wall) are added as red lines. At the onset of the shear layer instabilities, the perturbations seem to propagate with a phase speed comparable to
$c_{r,3}(\alpha _3)$ (jet with flexible wall) are added as red lines. At the onset of the shear layer instabilities, the perturbations seem to propagate with a phase speed comparable to ![]() $c_{r,2}(\alpha _2)$. However, after the onset of leaflet motions, which appear to propagate with phase speed
$c_{r,2}(\alpha _2)$. However, after the onset of leaflet motions, which appear to propagate with phase speed ![]() $c_{r,3}(\alpha _3)$, the shear layer perturbations appear to accelerate somewhat towards the phase speed
$c_{r,3}(\alpha _3)$, the shear layer perturbations appear to accelerate somewhat towards the phase speed ![]() $c_{r,3}(\alpha _3)$.
$c_{r,3}(\alpha _3)$.
Furthermore, figure 13(a,b) reveals that the shear layer instability also grows in the upstream direction (indicated by thin black lines). This is reminiscent of an absolute instability (Huerre & Monkewitz Reference Huerre and Monkewitz1990; Schmid & Henningson Reference Schmid and Henningson2001) which may be facilitated by the lower streamwise velocities in the wake of the leaflet (figure 13c). Furthermore, this could suggest that the shear layer instability, which starts downstream of the leaflets, is triggering the FSI instability when it reaches the leaflets.
The growth rates of FSI-DNS and LSA results are compared in figure 13(d). Solid lines show the envelope of transversal velocity oscillations over time within the leaflet shear layer for case AR (![]() $G_{AR}|_{x=6t_L}$) and case A (
$G_{AR}|_{x=6t_L}$) and case A (![]() $G_{A}|_{x=6t_L}$) and for the leaflet tip of case A (
$G_{A}|_{x=6t_L}$) and for the leaflet tip of case A (![]() $G_{A}|_{x=0}$). For comparison with growth rates obtained by LSA, we display the maximum temporal growth of KH instabilities of base flow
$G_{A}|_{x=0}$). For comparison with growth rates obtained by LSA, we display the maximum temporal growth of KH instabilities of base flow ![]() $b_2$ (
$b_2$ (![]() $\exp (\omega _{i,2,max}t)$) and of FSI instabilities of base flow
$\exp (\omega _{i,2,max}t)$) and of FSI instabilities of base flow ![]() $b_3$ (
$b_3$ (![]() $\exp (\omega _{i,3,max}t)$). The initial growth of the shear layer instabilities in the FSI-DNS is in very good agreement with the predicted growth rate of configuration
$\exp (\omega _{i,3,max}t)$). The initial growth of the shear layer instabilities in the FSI-DNS is in very good agreement with the predicted growth rate of configuration ![]() $b_2$ (free jet). Likewise, the growth of the leaflet instabilities agrees well with the growth rate from configuration
$b_2$ (free jet). Likewise, the growth of the leaflet instabilities agrees well with the growth rate from configuration ![]() $b_3$ (jet bounded by flexible wall). For better comparison, the different onsets of instability growth are marked by circles in figure 13(a,b), although the small initial amplitudes are not evident in this figure.
$b_3$ (jet bounded by flexible wall). For better comparison, the different onsets of instability growth are marked by circles in figure 13(a,b), although the small initial amplitudes are not evident in this figure.
Finally, we study the leaflet shape in figure 13(b) in comparison with wavelengths determined by LSA. In the numerical simulations, the leaflet mostly exhibits an S-shaped travelling wave pattern. In LSA, this leaflet form corresponds approximately to the wavenumber ![]() $\alpha _0 = 5.55$ resulting in one full wave per leaflet length. As illustrated in figure 3, the eigenmodes at this wavenumber show a decoupled behaviour where only one shear layer (or flexible wall) is affected by the instability, whereas the other shear layer (flexible wall) is not affected. This suggests individual, decoupled dynamics for each leaflet, which agrees well with experimental studies of leaflet kinematics which indicate asynchronous motion of the leaflets (Vennemann et al. Reference Vennemann, Rösgen, Heinisch and Obrist2018).
$\alpha _0 = 5.55$ resulting in one full wave per leaflet length. As illustrated in figure 3, the eigenmodes at this wavenumber show a decoupled behaviour where only one shear layer (or flexible wall) is affected by the instability, whereas the other shear layer (flexible wall) is not affected. This suggests individual, decoupled dynamics for each leaflet, which agrees well with experimental studies of leaflet kinematics which indicate asynchronous motion of the leaflets (Vennemann et al. Reference Vennemann, Rösgen, Heinisch and Obrist2018).
5. Conclusions
In this study, we investigated instability mechanisms which may contribute to laminar–turbulent transition downstream of a BHV. We used two conceptionally different approaches: LSA and numerical FSI simulations.
In the first part of this study (LSA) we derived modified Orr–Sommerfeld equations with an FSI extension term. We constructed a simplified one-dimensional model with a central jet and a zero-flow region surrounding the jet. The jet was confined either by a rigid wall (modelling the flow through a valve with fixed leaflets) or by a flexible wall (flow through a valve with flexible leaflets). In a third configuration, there was no wall between the jet and the zero-flow region (modelling the free aortic jet flowing into the AAo). The confined jet (fixed leaflets) was linearly stable for a physiological Reynolds number of ![]() ${\textit {Re}}=3318$. The configuration with a flexible wall exhibited FSI instabilities beyond a critical Reynolds number of
${\textit {Re}}=3318$. The configuration with a flexible wall exhibited FSI instabilities beyond a critical Reynolds number of ![]() ${\textit {Re}}_{FSI}=184$. For the configuration without separating wall, we found KH instabilities for a somewhat wider range of wavenumbers and a slightly higher critical Reynolds number (
${\textit {Re}}_{FSI}=184$. For the configuration without separating wall, we found KH instabilities for a somewhat wider range of wavenumbers and a slightly higher critical Reynolds number (![]() ${\textit {Re}}_{KH}=299)$. At
${\textit {Re}}_{KH}=299)$. At ![]() ${\textit {Re}}=3318$, the KH instabilities had a higher maximum growth rate and slower phase speeds than the FSI instabilities. For low wavenumbers, the unstable modes had either sinous or varicose character such that the associated displacements of the flexible walls were either in phase or out of phase, respectively. For higher wavenumbers, however, the unstable modes were decoupled such that the two flexible walls could move independently from each other.
${\textit {Re}}=3318$, the KH instabilities had a higher maximum growth rate and slower phase speeds than the FSI instabilities. For low wavenumbers, the unstable modes had either sinous or varicose character such that the associated displacements of the flexible walls were either in phase or out of phase, respectively. For higher wavenumbers, however, the unstable modes were decoupled such that the two flexible walls could move independently from each other.
Second, we conducted FSI simulations for a two-dimensional symmetric model of the aortic root comprising valve leaflets, a valve stent and a parametrized aortic wall model immersed in a fluid domain. To study the influence of FSI on the onset of instabilities, we ran simulations for rigid as well as flexible leaflets. Both models showed qualitatively similar flow phenomena. First, a starting vortex is formed which is advected and elongated in the downstream direction. The interaction of this starting vortex with the aortic wall leads to a secondary vortex. This vortex moves towards the leaflet shear layer and perturbs it. We suspect that this triggers the KH shear layer instability. This sequence is observed in the shear layers behind rigid and flexible leaflets which indicates that this part of the instability mechanism is independent of FSI. Only after the onset of KH instabilities do the flexible leaflets start moving with growing amplitude which results in repeated shedding of vortices from the leaflet tips. These vortices eventually break down and contribute to the chaotic nature of the fully developed flow field downstream of the valve. Simulations in a model with a narrower AAo exhibited an earlier onset of the KH instabilities. This supports the interpretation that the onset of the KH instability is triggered by the secondary vortex, because this vortex has to travel a shorter distance (in the narrow aorta case) before it reaches the shear layer. Furthermore, this indicates that the spanwise distance between aortic wall and leaflet shear layer is an important parameter for the temporal evolution of the instabilities.
The study is concluded by a combined analysis of the numerical data and the results from LSA. The results of both approaches are in good agreement. The combined analysis supports the higher growth rate of the KH instabilities in the shear layer and the higher phase speeds of FSI instabilities on the leaflets. The wavelength of the leaflet oscillations corresponds to a modal wavenumber for which the LSA indicates decoupled eigenmodes. This could offer an explanation for the experimental observation that valve leaflets tend to move independently from each other. Additionally, the investigation of the spatio-temporal evolution of the KH instability suggests that it has the character of an absolute instability. This could mean that the onset of the leaflet oscillation (FSI instability) is triggered by the KH instability which initiates somewhat downstream of the leaflets and propagates upstream towards the leaflet.
By investigating the fundamental instability mechanisms in the flow field downstream of a BHV, our results could be useful for valve design optimization. We have shown that both KH and FSI instabilities are present at a physiologically realistic Reynolds number of ![]() ${\textit {Re}}=3318$. The critical Reynolds numbers for both instabilities are significantly smaller than physiological Reynolds numbers. Therefore, it is likely that transition to turbulence will occur in any aortic valve regardless of its specific design. At the same time, this means that complete suppression of transition is probably not possible. However, a better understanding of the transition mechanisms may help to find ways to modify the transition process which could contribute to improving hydraulic valve performance, increasing valve durability or reducing blood trauma. Additionally, we showed the relevance of aortic wall geometry (e.g. spanwise distance between leaflet shear layer and aortic wall) for the onset of instabilities. Therefore, patient-specific assessment of this geometrical parameter may allow for a more favourable positioning of the valve with respect to the aortic wall which could result in a delayed KH instability. This could even help to mitigate unfavourable haemodynamic mechanisms such as shear-induced thrombosis. Furthermore, optimized leaflet rigidity might dampen the FSI instability and contribute to reduced leaflet fluttering. Thereby, not only could the cyclic stresses contributing to leaflet fatigue be lowered, but also vortex shedding after the onset of oscillatory leaflet motion could be reduced which further mitigates adverse haemodynamic effects.
${\textit {Re}}=3318$. The critical Reynolds numbers for both instabilities are significantly smaller than physiological Reynolds numbers. Therefore, it is likely that transition to turbulence will occur in any aortic valve regardless of its specific design. At the same time, this means that complete suppression of transition is probably not possible. However, a better understanding of the transition mechanisms may help to find ways to modify the transition process which could contribute to improving hydraulic valve performance, increasing valve durability or reducing blood trauma. Additionally, we showed the relevance of aortic wall geometry (e.g. spanwise distance between leaflet shear layer and aortic wall) for the onset of instabilities. Therefore, patient-specific assessment of this geometrical parameter may allow for a more favourable positioning of the valve with respect to the aortic wall which could result in a delayed KH instability. This could even help to mitigate unfavourable haemodynamic mechanisms such as shear-induced thrombosis. Furthermore, optimized leaflet rigidity might dampen the FSI instability and contribute to reduced leaflet fluttering. Thereby, not only could the cyclic stresses contributing to leaflet fatigue be lowered, but also vortex shedding after the onset of oscillatory leaflet motion could be reduced which further mitigates adverse haemodynamic effects.
It is very likely that a full three-dimensional configuration of a real heart valve prosthesis features many more instability phenomena, e.g. azimuthal modes of vortex ring breakdown as present in figure 5 of Becsek et al. (Reference Becsek, Pietrasanta and Obrist2020). Regarding the structural side of the FSI problem, the influence of radial tension within the actual three-dimensional, curved leaflet shape might influence the leaflet motion as well as its impact on downstream flow features. Therefore, the proposed instability mechanism (starting vortex ![]() $\to$ secondary vortex at the aortic wall
$\to$ secondary vortex at the aortic wall ![]() $\to$ KH instability in the shear layer
$\to$ KH instability in the shear layer ![]() $\to$ FSI instability on the leaflets) is only a first hypothesis and requires further investigation and confirmation.
$\to$ FSI instability on the leaflets) is only a first hypothesis and requires further investigation and confirmation.
Funding
This work was supported by a grant from the Swiss National Supercomputing Centre (CSCS) under project ID s1121.
Declaration of interests
The authors report no conflict of interest.
Appendix A. Definition of base flows
Base flow profiles are extracted from numerical results as presented in § 3. After the initial outward leaflet deflection (opening of the valve), the leaflets remain stable for a certain time period. We define the time instance just prior to the onset of leaflet oscillations as a quasi-steady base flow solution and assume locally parallel flow. The flow profile is then extracted between the leaflet tips in the spanwise direction as shown in figure 1 (green line). With inflow conditions tuned to achieve a physiological cardiac output at rest, dimensional analysis of the base flow at the orifice yields a Reynolds number of ![]() ${\textit {Re}}=3318$.
${\textit {Re}}=3318$.
Appendix B. Derivation of the material constant  $\xi$
$\xi$
To determine the material constant ![]() $\xi$ in the formulation of the force density
$\xi$ in the formulation of the force density ![]() $\tilde {\boldsymbol {f}}_{{FSI}}$, we assume proportionality of the restoring force density of the structure to the squared wavenumber
$\tilde {\boldsymbol {f}}_{{FSI}}$, we assume proportionality of the restoring force density of the structure to the squared wavenumber ![]() $\alpha ^2$ (Lebbal et al. Reference Lebbal, Alizard and Pier2022). In order to ensure the transferability of FSI-DNS and LSA results, we conduct purely structural finite-element simulations for a single leaflet considering its thickness and neo-Hookean material model applied in numerical simulations. As shown in figure 14, a defined displacement amplitude
$\alpha ^2$ (Lebbal et al. Reference Lebbal, Alizard and Pier2022). In order to ensure the transferability of FSI-DNS and LSA results, we conduct purely structural finite-element simulations for a single leaflet considering its thickness and neo-Hookean material model applied in numerical simulations. As shown in figure 14, a defined displacement amplitude ![]() $\hat {\eta }$ at varying wavelengths
$\hat {\eta }$ at varying wavelengths ![]() $\lambda$ is imposed from alternating sides to map the restoring force resulting in a non-dimensionalized material-specific constant of
$\lambda$ is imposed from alternating sides to map the restoring force resulting in a non-dimensionalized material-specific constant of ![]() $\xi = 2\times 10^{-7}$.
$\xi = 2\times 10^{-7}$.

Figure 14. (a) Imposition of fixed value displacement amplitude ![]() $\hat {\eta }$ at varying distances
$\hat {\eta }$ at varying distances ![]() $\lambda$. (b) Determination of material-specific spring constant
$\lambda$. (b) Determination of material-specific spring constant ![]() $\xi$ (blue line) by evaluating the horizontal restoring force
$\xi$ (blue line) by evaluating the horizontal restoring force ![]() $f_y/\hat {\eta }\alpha ^2$ for different wavenumbers
$f_y/\hat {\eta }\alpha ^2$ for different wavenumbers ![]() $\alpha =2{\rm \pi} /\lambda$.
$\alpha =2{\rm \pi} /\lambda$.
Appendix C. Sensitivity analysis
Figure 15 summarizes the sensitivity of the LSA and the numerical FSI simulations to variations in element size. Maximum growth rates ![]() $\omega _{i,max}$ converge at
$\omega _{i,max}$ converge at ![]() $400$ grid points for both
$400$ grid points for both ![]() $b_2$ and
$b_2$ and ![]() $b_3$ base flows. Sensitivity analysis regarding the fluid mesh width of the FSI simulations was conducted for minimal mesh widths of 35, 70 and
$b_3$ base flows. Sensitivity analysis regarding the fluid mesh width of the FSI simulations was conducted for minimal mesh widths of 35, 70 and ![]() $140\,\mathrm {\mu }$m. Results were compared at the STJ and within the leaflet shear layer at a critical time
$140\,\mathrm {\mu }$m. Results were compared at the STJ and within the leaflet shear layer at a critical time ![]() $t=0.13$ s which marks the onset of transversal fluid oscillations. Also, the temporal evolution of leaflet tip displacements was assessed to investigate the sensitivity of structural motion to fluid mesh widths. In general, a fluid mesh width of
$t=0.13$ s which marks the onset of transversal fluid oscillations. Also, the temporal evolution of leaflet tip displacements was assessed to investigate the sensitivity of structural motion to fluid mesh widths. In general, a fluid mesh width of ![]() $70\,\mathrm {\mu }$m is found to be sufficient for converged results. However, better numerical performance (i.e. fewer spurious oscillations at the FSI, more stable numerical convergence) is reached for smaller mesh widths. Therefore, a minimum mesh width of
$70\,\mathrm {\mu }$m is found to be sufficient for converged results. However, better numerical performance (i.e. fewer spurious oscillations at the FSI, more stable numerical convergence) is reached for smaller mesh widths. Therefore, a minimum mesh width of ![]() $35\,\mathrm {\mu }$m was used for this study. For this mesh width, a maximum time step of
$35\,\mathrm {\mu }$m was used for this study. For this mesh width, a maximum time step of ![]() $1\,\mathrm {\mu }$s is necessary to achieve numerical stability.
$1\,\mathrm {\mu }$s is necessary to achieve numerical stability.

Figure 15. Sensitivity analysis of LSA: (a) maximum growth rate ![]() $\omega _{i,max}$ for base flows
$\omega _{i,max}$ for base flows ![]() $b_2$ (shear flow, blue) and
$b_2$ (shear flow, blue) and ![]() $b_3$ (flexible wall, green). A number of grid points of
$b_3$ (flexible wall, green). A number of grid points of ![]() $400$ (indicated by the red line) was chosen for this study. Sensitivity analysis of numerical FSI simulations: (b) transversal (
$400$ (indicated by the red line) was chosen for this study. Sensitivity analysis of numerical FSI simulations: (b) transversal (![]() $u_{f,y}$) and streamwise (
$u_{f,y}$) and streamwise (![]() $u_{f,x}$) velocity profiles at the STJ (left) and within the leaflet shear layer (right) for minimal fluid mesh widths 35, 70 and
$u_{f,x}$) velocity profiles at the STJ (left) and within the leaflet shear layer (right) for minimal fluid mesh widths 35, 70 and ![]() $140\,\mathrm {\mu }$m at time instant
$140\,\mathrm {\mu }$m at time instant ![]() $t=0.13$ s; (c) temporal evolution of the leaflet tip displacement
$t=0.13$ s; (c) temporal evolution of the leaflet tip displacement ![]() $u_{s,y}$ for minimal fluid mesh widths 35, 70 and
$u_{s,y}$ for minimal fluid mesh widths 35, 70 and ![]() $140\,\mathrm {\mu }$m.
$140\,\mathrm {\mu }$m.