Introduction
By the end of 2020, about 300,000 infants may be born in the United States to mothers infected by the severe acute respiratory syndrome virus 2 (SARS-CoV-2) sometime during their pregnancy. Millions more will be born to mothers and families who have experienced tremendous stress and change in their daily lives and environments due to the pandemic. Postnatal effects of in utero exposure to SARS-CoV-2 from pregnant women with Coronavirus Disease 2019 (COVID-19) are mostly unknown, but are suggested from the 1918 Influenza pandemic which had lifelong effects on health and achievement. We discuss how maternal infections and in utero exposure to the pandemic environment may affect postnatal development and lifetime cardiovascular, metabolic, and neurodevelopmental health. The effects of SARS-CoV-2 on pregnant women and neonates are compared to other coronaviruses, SARS (severe acute respiratory syndrome) and MERS-CoV (Middle East Respiratory Syndrome). We then suggest indicators of maternal, neonatal, and later life health that should be monitored following in utero exposure to SARS-CoV-2. Lastly, we consider how to disentangle the effects of maternal infection versus the effects of prenatal exposure to the stress of the pandemic environment, both positive and negative.
Lifetime effects of the 1918–1919 influenza pandemic
The 1918 Influenza pandemic (Influenza A, H1N1 subtype) had multiple health consequences for the cohort that was in utero during the pandemic.Reference Almond 1 , Reference Mazumder, Almond, Park, Crimmins and Finch 2 The U.S. cohort in utero during the peak pandemic period, experienced more depression after age 50, diabetes and ischemic heart disease after age 60, and mortality after age 65, with some variation in estimated effects.Reference Mazumder, Almond, Park, Crimmins and Finch 2 – Reference Schnittker 5 The Taiwanese cohort exposed in utero in 1919 had more renal disease, circulatory and respiratory morbidities, and diabetes after age 60.Reference Lin and Liu 6 The corresponding Swedish cohort had higher morbidity at ages 54–87, indicated by excess hospitalization and male mortality from heart disease and cancer.Reference Helgertz and Bengtsson 7 The effect on late life health varied by trimester of development at the pandemic peak. Elevated heart disease in the U.S. was associated with second trimester exposure at the peak for the 1918–1919 cohort; while diabetes was associated with third trimester exposure at the peak.
No data on birth weight are available for the 1918 Influenza cohort; however, there are many indications that early life physical health and neurodevelopment were directly affected either by in utero exposure or indirectly by its multifarious stresses. Men in the 1918–1919 U.S. flu cohort were shorter at WWII enlistment than flanking cohorts,Reference Mazumder, Almond, Park, Crimmins and Finch 2 while children and adolescents in Taiwan were shorter than surrounding cohorts.Reference Lin and Liu 6 U.S. women exposed in utero married men with less education.Reference Fletcher 3 Educational deficits in the U.S. and Taiwan for these cohorts could be related to early cognitive deficits.Reference Almond 1 , Reference Lin and Liu 6 Lower socioeconomic status (SES) as adults for those in utero during the 1918 epidemic was also confirmed in the parents of the Wisconsin Longitudinal Study participants,Reference Cook, Fletcher and Forgues 8 but was not found in Sweden.Reference Helgertz and Bengtsson 7
These historical associations for the cohort in utero in 1918–1919 are based solely on birth dates and cannot identify individuals whose mothers actually experienced infections. Thus, the analysis is restricted to population data on timing of infections and birth dates related to outcomes many decades after the pandemic. Thus we cannot readily distinguish direct effects on long-term health and well-being due to exposure to the infection itself versus the stress effects due to exposure to the pandemic environment. These socio-environmental stressors include potentially increased levels of uncertainty, undernutrition, under- and unemployment, poverty, and loss of loved ones. Despite this, the findings from the 1918 flu pandemic of lasting consequences for those exposed prenatally warrants study of similar programming effects from the current pandemic. Unlike the earlier pandemic, the current pandemic provides opportunity to study individuals with known in utero exposure to SARS-CoV-2 throughout their life based on known maternal infection and socio-environmental stresses. We can add further critical comparisons to individuals exposed in utero to the pandemic environment but with no maternal infection, which potentially allows disentanglement of the effects of exposure to infection versus pandemic environment.
Long-term consequences of maternal and fetal exposure to viral infections
Maternal viral infections can affect the fetus or neonate through multiple pathways. Maternal infections can directly infect the fetus as well as the placenta.Reference Raciot and Mor 9 Viral species differ markedly in their impact on pregnant women and fetuses. For instance, HIV and hepatitis B virus are vertically transmitted in up to 40% of cases without the successful interventions that have almost eliminated direct transmission in the U.S. Fortunately, maternal transmission is rare for the coronaviruses MERS-CoV (2012) and SARS-CoV (2002)Reference Rodríguez-Blanco, Vegara-Lopez, Aleo-Giner and Tuells 10 and the 2009 H1N1 influenza virus.Reference Mosby, Rasmussen and Jamieson 11 And, no severe birth defects have been associated with prior coronaviruses, MERS-CoV (2012) and SARS-CoV (2002). In general, pregnancy increases virus-associated morbidity and mortality, as shown for influenza H1N1 in 2009 and SARS-CoV.Reference Alfaraj, Al-Tawfiq and Memish 12 , Reference Giles, Krishnaswamy, Macartney and Cheng 13 These infections also caused more preterm delivery and low birth weight.Reference Giles, Krishnaswamy, Macartney and Cheng 13
Virus-related maternal inflammatory processes can impact the placenta and disturb in utero metabolism to cause intrauterine growth restriction (IUGR).Reference Maldonado 14 Long-term consequences include impaired glucose and insulin metabolism and hyperactivity of the hypothalamic–pituitary–adrenal (HPA) axis.Reference Kesavan and Devaskar 15 Historically, Barker and colleagues showed that IUGR and low birth weight which could be related to maternal infection or poor nutrition are associated with later life cardiovascular disease and obesity.Reference Barker, Osmond, Kajantie and Eriksson 16 In the Helsinki Birth Cohort (1934–1944), which suffered a suboptimal nutritional environment, smaller placentas predicted larger childhood body mass index (BMI) and increased adult cardiovascular disease.Reference Thornburg and Marshall 17 Maternal immune response to viruses and bacterial coinfections can impact fetal development with multi-generational behavioral and cognitive consequences.Reference Pollak and Weber-Stadlbauer 18
Effects of COVID-19 on pregnant women and neonates
We summarize the main points of the COVID-19 literature published thus far, bearing in mind that these findings are preliminary as they are based on small numbers, specific locations, and, often, more severely ill patients.
COVID-19 in pregnant women
Pregnant women do not appear to be at increased risk of contracting SARS-CoV-2, as their rates of infection seem to parallel the rates of infection in their surrounding communities. When pregnant women do contract the SARS-CoV-2 virus, the majority experience a similar clinical course as age-matched non-pregnant women; however, reports increasingly show need for more hospitalization, mechanical ventilation, and intensive care.Reference Ellington, Strid and Tong 19 , Reference Trocado, Silvestre-Machado and Azevedo 20 , Reference Delahoy, Whitaker and O’Halloran 21 Thus far, the overall mortality rate from COVID-19 in pregnant women is not significantly different from non-pregnant women.Reference Ellington, Strid and Tong 19
As in the general population, a minority of pregnant patients develop severe and critical illness, with cardiopulmonary compromise, and even multi-organ failure. SARs-CoV-2 can cause an exaggerated inflammatory response and coagulation activation in some individuals, causing worse outcomes. Whether the immunologic changes of pregnancy affect the exaggerated inflammatory response is unknown. The limited data suggests that COVID-19 pregnancies have similar elevations of cytokines (IL-6, TNFα) and chemokines (CCL2, CXCL10) as other COVID-19 patients.Reference Ur and Verma 22 Some postulate that the anti-inflammatory state of pregnancy required to prevent rejection of the fetus may actually help fight the inflammatory cascade caused by COVID-19.Reference Berhan 23 Severe COVID-19 disease is also associated with increased rates of thromboembolic events, despite prophylactic anticoagulation.Reference Bilaloglu, Aphinyanaphongs, Jones, Iturrate, Hochman and Berger 24 Although pregnancy increases the risk of thromboembolic events, and COVID-19 could further increase thromboembolic events in pregnancy, this possibility has not been studied.
Little is known about the impact of the SARS-CoV-2 virus on the placenta and the impact of the associated inflammatory and thromboembolic responses on the placenta. There are some reports of neonatal infections from SARs-CoV-2 infection of the placenta and its transplacental transmission.Reference Vivanti, Vauloup-Fellous and Prevot 25 The inflammatory and thromboembolic responses related to maternal COVID-19 disease may affect placental growth, vascular perfusion, and hypertensive disorders of pregnancy. One study of third trimester placentas from women infected with SARS-CoV-2 showed a significant increase in features of maternal vascular malperfusion, which may be related to the inflammatory and thromboembolic response.Reference Shanes, Mithal and Otero 26 Importantly, these patients had moderate-to-severe COVID-19, but none were intubated. Together, the risks of these pathological markers was 3.3-fold above reference non-exposed population.
Birth outcomes
Rates of preterm birth may be increased by maternal SARS-CoV-2 infections, with estimates ranging from 12% to 27%.Reference Huntley, Huntley, Di Mascio, Chen, Berghella and Chauhan 27 , Reference Panagiotakopoulos, Myers and Gee 28 These may be overestimates because they over-represent the more severely ill pregnant women. The increased rates of preterm delivery may be related to fever and hypoxemia which increase risk for preterm labor, premature rupture of membranes, and abnormal fetal heart rates. However, asymptomatic but infected pregnant women also showed more preterm delivery than non-infected pregnant women. Estimates of low birth weight range from 12% to 20%.Reference Trocado, Silvestre-Machado and Azevedo 20 A meta-analysis reported 15.6% low birth weight which did not significantly differ by maternal COVID-19 status.Reference Cavalcante de Melo and Machado de Araújo 29 Importantly, studies from Ireland and Denmark as well as anecdotal reports by doctors from several regions around the world suggest decreasing levels of preterm birth/birth of very low birthweight infants in the general population during the pandemic.Reference Philip, Purtill and Reidy 30 , Reference Hedermann, Hedley and Baekvad-Hansen 31 This suggests that for some, the measures taken to control spread of the virus may have had some positive externalities.
Additionally, rates of C-section delivery are increased in pregnant women with SARS-CoV-2 infections. In a systematic review, C-sections occurred in 52%–85% of COVID-19 deliveries, which may also be overestimated.Reference Huntley, Huntley, Di Mascio, Chen, Berghella and Chauhan 27 Early in the pandemic, C-section was the primary mode of delivery in some hospitals; given the lack of information about vertical transmission, there was concern that vaginal delivery might increase risk of infection in the neonate. C-section rates may also be increased due to abnormal fetal heart rate tracings related to maternal hypoxia and fever. Additionally, C-section may be chosen to relieve severe maternal disease, resulting in preterm birth.Reference Easterlin, De Beritto and Yeh 32
Stillbirths among women with COVID-19 so far have been rare and seem to have been related to very severe maternal illness. Infected mothers in one prospective study had significant several-fold increased rates of stillbirth.Reference Marian, Kathryn and Nicola 33 In another study, there was a general increase in stillbirths in the pandemic period in Britain.Reference Khalil, von Dadelszen, Draycott, Ugwumadu, O’Brien and Magee 34
Data on effects of first and second trimester maternal infections is very limited, as is data for spontaneous abortions. There is a theoretical concern that fever in the first trimester may increase risk for miscarriage and congenital anomalies. Further studies of the outcomes of maternal infections, especially in the first and second trimesters are needed.
Neonatal outcomes
Most newborns born to mothers with COVID-19 disease have been healthy, and most commonly suffered from sequelae of prematurity rather than the effects of SARS-CoV-2. The rate of congenital infection from SARS-CoV-2 at this time is estimated at <3%, approximating the rates of other congenital infections.Reference Kotlyar, Grechukhina and Chen 35 In utero transmission needs further study to substantiate reports of transmission, based on polymerase chain reaction assay for SARs-CoV-2 in the neonate and/or placenta, or elevated IgM antibodies.Reference Vivanti, Vauloup-Fellous and Prevot 25 The few case reports of potential in utero transmission are complicated by the initial lack of criteria defining vertical transmission. Horizontal spread of the disease to neonates from family members or other household contacts occurs and is generally mild.Reference Feld, Belfer and Kabra 36
Ongoing/future studies
The COVID-19 cohort provides a natural experiment to examine the effects of maternal viral infection while infants were in utero. Such effects may span the lifecycle of these babies; during this time it may be possible to intervene to prevent later life problems. Cohort studies include the UCSF PRIORITY: Pregnancy Coronavirus Outcomes Registry and the American Academy of Pediatrics Society of Neonatal and Perinatal Medicine (AAP SoNPM) – National Perinatal COVID-19 (NPC-19) Registry, a collaboration of the AAP SoNPM with the Vermont Oxford Network (VON). Neither of these registries are currently supported for the long-term follow-up which is warranted by important scientific and clinical reasons.
We suggest that to capture the consequences of viral exposure in utero for childhood development and adult health COVID-19 birth cohort studies consider immediate collection of data from the mother, fetus, neonate, and placenta. These initial data should be followed by analysis of child growth and development and lifelong study of health, behavioral patterns, and cognitive functioning. Table 1 suggests multiple indicators for immediate measurement and measurement across the lifespan. Initial indications of disease presence, exposure, and severity are important including inflammatory cytokines in the mother and infant. Clinical data on the size and development of the infant both before and at birth and the placenta at birth should be routinely collected. Because relatively simple anthropometric measures routinely taken at birth serve only as a very crude proxy measure of the prenatal environment, we encourage studies using longitudinal ultrasound measurements of fetal development. Because hypocortisolemia was common in SARS-CoV-1, HPA axis activity should be studied in severe COVID-19 mothers (ChiCTR20000301150).Reference Pal 37 Maternal genetics may also influence vulnerability to infection and impact on the fetus, shown for adult carriers of ApoE alleles.Reference Finch and Kulminski 38 Molecular studies could include the placental transcriptome for genetic variants of gene expression (eQTLs) that predict childhood obesity and BMI.Reference Peng, Deyssenroth and Di Narzo 39 Epigenomic methylation of DNA and histones should be monitored across the lifespan of the infant. DNA methylation measures represented as epigenetic clocks that represent “aging” can be estimated in pediatric and then adult years.Reference McEwen, O’Donnell and McGill 40 Socioeconomic status and educational status of the mother and child should also be assessed, as causes of adverse outcomes can be social as well as biological. Additionally, COVID-19 infection appears to be more common and severe in racial and ethnic minorities in the U.S.Reference Kopel, Perisetti, Roghani, Aziz, Gajendran and Goyal 41 Moreover, preexisting conditions increase the severity of COVID-19 infection, which may have implications for transmission and neonatal outcomes. Our recommendations are oriented toward the United States as the situation may differ in low- and middle-income settings.
Table 1. Domains for evaluating effects of in utero exposure to COVID-19
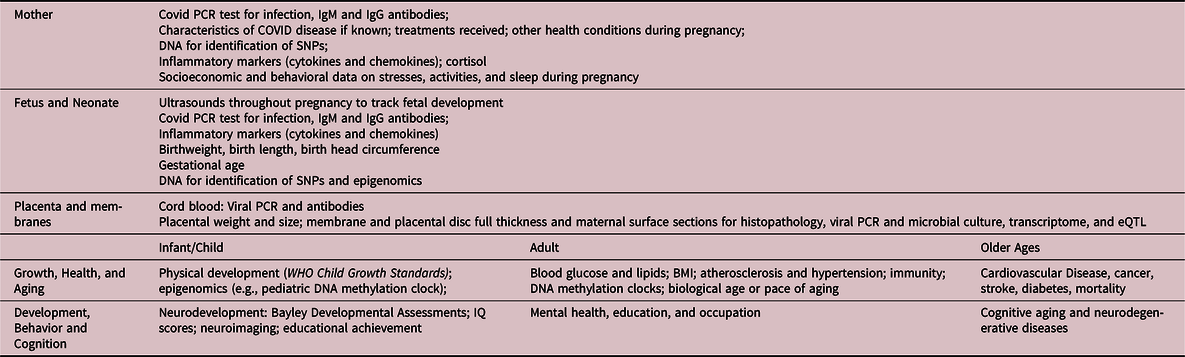
The child should be followed for indicators of growth, motor, and neurological development milestones. Throughout life, the standard blood-based indicators should be collected. Composite measures derived from clinical chemistry and physical exams can be used starting in childhood to categorize the “Pace of Aging.”Reference Belsky, Caspi and Houts 42 Follow-up should include information on development of both pediatric (e.g., leukemia, asthma) and adult diseases (e.g., heart disease, cancer, stroke).
The COVID-19 pandemic also provides an opportunity to study the effects of in utero exposure to the pandemic environment and the effects of different regional and national policies to address viral spread. The COVID-19 pandemic has increased levels of stress, unemployment, food insecurity, and domestic violence, and diminished or disrupted prenatal care. These factors may have programming effects and/or direct effects on neonatal health. The pandemic-related lockdown policies may benefit some individuals; pregnant women staying home who may rest more, and have decreased exposure to other infections, and women with job stability, may benefit from less stress from work and commuting time. These benefits are evidenced by reports of decreased rates of preterm birth for the general population during the pandemic.
Studies would include mother and child dyads and a selection of mothers with symptomatic and nonsymptomatic COVID-19 diagnosis, as well as a group of mothers and babies with no in utero exposure. We suggest the desirability of enrolling an additional child born either shortly before or shortly after the COVID-19 pandemic to the same mother. These study groups would allow comparison between infants who were exposed to maternal infection and those who were prenatally exposed to the pandemic without having experienced maternal infection. These infants can also be compared to those who were born before or conceived after the pandemic, providing further insight on the effects of the pandemic environment. The inclusion of information on social and economic stresses will allow comparisons between countries taking different measures to reduce spread of the virus, These types of comparisons may give us further insights beyond the effects of COVID, such as socioeconomic and social policies that may decrease risk of preterm birth, which has eluded the maternal-infant health community for decades. This should be balanced by further investigating reports of generally increased stillbirth and potential contributors.
Summary and conclusions
Maternal COVID-19 infections and exposure to the pandemic environment may have long-term effects on growth and aging for the cohort in utero during this pandemic based on the 1918 influenza birth cohort. From comparisons of the 1918 Influenza with the current COVID-19 pandemic, we suggest studies of markers from birth through adulthood that are indicators of the altered development and accelerated aging that could be experienced in the century ahead.
We need to evaluate whether the effects of COVID-19 can be generalized to other viruses. While the current pandemic is similar in some ways to the earlier, there are important differences. COVID-19 resembles the 1918 Flu in that many infections were relatively uncomplicated cases, but deadly for a small proportion of cases. Surprisingly, given the 100 year difference in time, the mortality during the two pandemics appears fairly similar in New York at the height of the pandemic; an increase over baseline of about 200 deaths per 100,000 population in the 1918 epidemic and an increase of about 150 per 100,000 in 2020.Reference Faust, Lin and Del Rio 43 A key difference between the 1918 pandemic and the current COVID-19 pandemic is the more significant role of secondary bacterial infections, in comparison to the current severe lung disease, multi-organ damage, inflammatory response, and thromboembolic tendency reported for the most serious cases of COVID-19. Secondary bacterial infections related to COVID-19 have mostly been effectively managed with antibiotics. Additionally, the 1918 flu was particularly deadly for people aged 20 to 40, or those in the childbearing years; in contrast, the SARS-CoV-2 virus causes higher mortality among older persons. While the long-term outcomes may not be the same as 1918, it is important to study the effects of SARS-CoV-2 during pregnancy in terms of consequences for later life health and aging.
Acknowledgements
The authors would like to thank Jennifer Cotter (M.D.) and Linda Szymanski (D.O.) of Children’s Hospital Los Angeles, Department of Pathology & Laboratory Medicine and the Keck School of Medicine, USC, for useful information on placental pathology and biobanking.
Financial Support
This work was supported by NIA (P30-AG017265) to E.M.C. and NIA (R01-AG05142, P01-AG055367) to C.E.F.
Conflicts of Interest
None.
Ethical standards
None.




