Introduction
Community engagement (CE) is the collaboration between institutions of higher education and their larger communities (local, regional, state, national, and global) for the mutually beneficial exchange of knowledge and resources in a context of partnership and reciprocity [Reference Ahmed and Palermo1]. As simple as this definition is and the principles encompassed by CE, the practice and landscape of CE have diverse practical methods of application. A variety of challenges exist in the field of CE, such as misunderstanding of methods by newcomers, or gaps in communication among practitioners due to differences in practice or terminology. Historically, there has been no formal model to contextualize all practical methods of applying CE. In efforts to create a common dialog about CE practices, we are proposing a comprehensive model for CE that outlines different components and provides a common reference for all types of CE practitioners. Academic health centers (AHCs) aim to improve the health of the surrounding community and advance research for better treatments and access to care [Reference Borden2]. Hence, developing a model for practicing CE at AHCs will help further clarify CE in the context of AHC missions and programs, spurring additional development in CE practices. Although CE is practiced at an international level, the authors focused the model on CE practices at US AHCs; accordingly, there are implications for a common model for all practitioners.
Background
The history and definitions of various terms used to describe CE are important to understanding the diverse approaches at different institutions (the definitions and history have been covered at length in other papers [Reference Ahmed and Palermo1, Reference Wallerstein and Duran3, Reference Israel4]). In the USA, CE was initially taken on as part of the mission of several land-grant universities; and in the 1990s it was further integrated into health promotion [Reference McCloskey5]. From the early 2000s to the present, the National Institutes of Health through the Clinical and Translational Science Awards (CTSAs) and the Centers for Disease Prevention and Control have had new interest in CE as an approach essential to resolving health disparities and improving the health of communities across the country [Reference Woollard6, Reference McLachlan7]. The practice of CE is relevant to various domains with numerous contexts and modes of implementation; leading to different names for CE, thereby making it difficult for practitioners of CE to share a common language [8, Reference Lazarus9].
Previous models address one or a few CE components, yet none that we could find address all components of CE (Community Outreach and Service, Education, Clinical Care, Research, and Policy and Advocacy). One logic model, specialized for the CTSAs, focuses on relationship types to measure the contributions of community-academic partnerships to research, aligning with the research and education CE components [Reference Eder10]. Other models have been developed to address the dynamics of individual CE components, such as publishing CE research [Reference Michener11]. A structure-process-outcomes framework for evaluating CE activity impact in academic medical centers was also developed that aligns with the CE component of research [Reference Michener11, Reference Szilagyi12]. Another model comes from the Carnegie Foundation’s Community Engagement Classification Framework (CFCECF). The CFCECF is an assessment tool which recognizes CE in multiple applications, but is primarily focused on assessing specific indicators with an emphasis on the types of CE activities most prevalent at undergraduate institutions, such as service learning [Reference O’Meara and Jaeger13]. Through review of these different models for CE, there is a central limitation mentioned for all—they lack the diversity in CE components necessary in order to accommodate all AHCs. To fully compare and account for each AHCs CE contributions, we need to look beyond the limited scope of research, education, and community service [Reference Ahmed and Palermo1, Reference Eder10, Reference Szilagyi12]. A more comprehensive model would offer the following benefits: provide a context for CE, facilitate practitioners’ ability to relate to each other, develop a common language through a shared reference, engage in advancing CE scholarship, and broaden the scope of CE activities considered in strategic planning, tracking and assessment, and evaluation of CE.
A More Comprehensive Context for CE at AHCs
CE Components
The types of CE activities that faculty, staff, and students engage in at AHCs vary. These CE activities can be categorized into 5 main components: (1) Community Outreach and Community Service, (2) Education, (3) Clinical Care, (4) Research, and (5) Policy and Advocacy. CE activities can focus on 1 component or incorporate any combination of these components, as reflected in the overlapping of areas in Fig. 1. CE programs are tailored to individual institutions and communities based on several factors including: the resources available; the primary mission and focus of the institution; and the interests, resources, and needs of the communities served by the institution [Reference Wallerstein and Duran3]. The diversity of CE programming is as unique as the communities and institutions that engage, which reinforces the challenge in developing a model that captures the full range of practices and activities. The CE Components Practical Model is specific to the context of CE at AHCs. All of these components are supported by essential administrative functions and infrastructure. These supporting elements are highlighted in the foundational box beneath the CE components in Fig. 1.
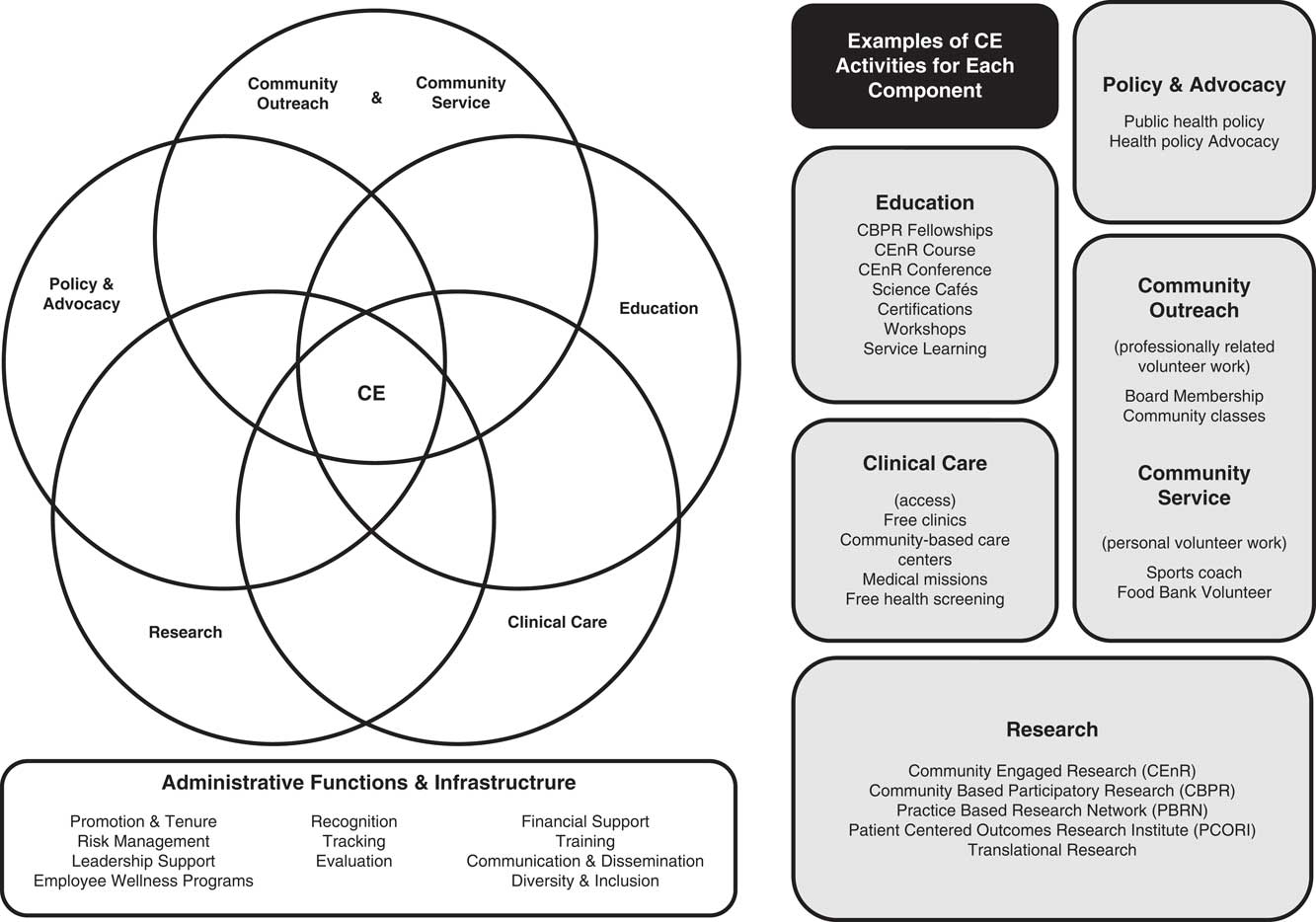
Fig. 1 The community engagement (CE) Components Practical Model.
Community Outreach and Community Service
Community service is a voluntary activity that faculty, staff, and students engage in unrelated to their professional appointment. Community service [14] is often a starting place for CE practitioners; it is an application of CE where professionals and academics start to connect with partner organizations and identify meaningful issues and causes. Community outreach is the way faculty, staff, and students collaborate in a manner consistent with the role and mission of their professional appointment with external groups in mutually beneficial partnerships that are grounded in scholarship [15]. Community outreach at AHCs often includes activities such as: faculty serving on the board of directors for local organizations or government committees as a health care industry representative; or faculty, staff, and students providing classes on health and nutrition to the community. Community outreach is one way for institutions to engage with the community, as it does not require the community to make a request or commitment, rather, it is an opportunity to make personal connections with the community, offer the community a benefit, and develop a shared understanding of the community’s needs. Community outreach is often the most commonly identified application of CE. For example, results from the Medical College of Wisconsin’s CE Surveys in 2014 and 2015 showed that community outreach activities were reported at least 2.5 times more often than any other type of CE activity included in the survey, including CE educational courses, publications and presentations, research projects, and awards and fundraising [16].
Education
Service learning (SL) [17] is one of the primary forms of CE application within the education component. SL focuses on student participation and volunteerism and influences how CE is practiced at undergraduate institutions. SL, while applicable to AHCs, is not the main application of CE in the context of education [17]. CE scholarship, of primary interest to faculty, is also included in this context, which focuses on learning new methods and practices for partnering with the community. This could include virtual ways of connecting with the community [Reference Sandy and Franco18]. CE education also includes traditional courses for both community-academic partners and academics on the methodology and principles of community-based participatory research, community engagement in research (CEnR), and practice-based research networks, but may not involve “practicing” CE. Education programs and courses designed because of collaborations between medical professionals, institutions, and the community, are also a part of CE education. The educational programs and courses identify the societal factor challenges related to improving health and health services; and educate communities and professionals about methods to better address those challenges. Educational components that are designed in partnership with the community are useful for educating both academics and community partners. For example, when developing a research project, community partners may need a course about Institutional Review Board (IRB) practices or other courses related to stages of research. Whereas academics may need to learn more about the culture of the community to be more receptive to what the community needs in the collaboration and partnership [Reference Foco19]. Other types of educational programs include workshops and conferences organized by faculty, staff, and community partners to address a mutual area of interest for learning and collaboration [Reference Ahmed20]. In addition, science cafés and certificate programs provide community-focused educational tools [Reference Ahmed21, 22] that are more focused in engaging the community in topics of community interest and offering value to community participants. HealthStreet, is another program that provides community-focused educational interactions based on community health workers engaging individual community members in discussions about research and clinical trial participation [Reference Cottler23].
Clinical Care
AHCs apply CE to the practice of health care delivery and access in a variety of ways. Although physicians, residents, and students engage with the community on a professional level when working directly with patients; clinical care in the context of CE involves more than fulfilling these standard professional obligations. Access to healthcare is a major challenge for improving the health of communities. AHCs deliver clinical care that is sensitive to and addresses the particular needs of the diverse populations served in order to improve credibility among the community [Reference Wilson-Stronks24]. Academics can learn the specific needs of the surrounding community through strong relationships with community groups, especially those groups representing underserved populations with the greatest health disparities. Through creating a healthcare setting that addresses the needs of the community, AHCs encourage community members to seek care. For example, in Dayton, Ohio, a program called “Reach Out: Physician’s Initiative to Expand Care to Underserved Americans” used a multidimensional approach to understand barriers to healthcare access in the community [Reference Ahmed and Maurana25, Reference Ahmed26]. Through door-to-door questioning of local community members in Dayton, the program found out that most residents lacked information about the local free clinics where they could seek care; and that transportation, child care, and inability to pay also were barriers to accessing care [Reference Ahmed and Maurana25, Reference Ahmed26]. Therefore, reasonable healthcare is still lacking in the community even if free clinics are available through AHCs, in the case of Reach Out the AHC informed the members of the community about the program after discovering the perceived barriers to accessing care. Additional examples of how CE is applied in the clinical care component include access programs that address financial and other barriers to healthcare, such as providing free clinics or community-based care centers [Reference Ahmed and Maurana25, Reference Ahmed26]. There is a recent increase in using Community Health Needs Assessments data to inform and direct community health programs, such as the University of Illinois Unison Health project [Reference Hospital27, 28]. Other examples of clinical care CE activities are volunteer medical missions, providing free health screenings, and providing care at reduced cost [Reference Hinojosa29, Reference Kharofa, Meurer and Nelson30].
Research
There are several applications that fall under CE research, ranging from research for improving CE methods and practices to improvements in the quality of clinical care in communities. Community-based participatory research incorporates community through all phases of the research process [Reference Israel4]. CEnR, another approach to research with communities involves community-academic partnership, with an emphasis on incorporating community identified needs and desires using the principles of CEnR [Reference Ahmed and Palermo1, Reference Ahmed31]. One study of over 100 community-academic partnerships demonstrates the capacity of the CEnR partnership approach to build sustainable programming in communities and to have a measurable impact that can be transformative for partnerships and communities [Reference Ahmed31]. Practice-based research networks are composed of primary care physicians working together to solve community-based health care problems and translating the physician’s findings and solutions into practice. This is a form of clinicians interacting with community and engaging in research [32, Reference Fink33]. Similarly, the Patient Centered Outcomes Research Institute, uses patient engagement to improve research protocols and ultimately the quality of healthcare and outcomes, this form of research closely resembles the principles of CE [Reference Frank, Basch and Selby34]. With the CTSA program through the National Center for Advancing Translational Science, there is a strong suggestion to incorporate CE at all levels of translational research, from phase 1 (T0) to phase 5 (T4), this is a sizeable challenge for all researchers from the bench to the clinic to integrate with existing and new research programs [35]. A program from the University of California, Los Angeles compared community-based interventions for the treatment of depression with technical services and found that community-based interventions are viable options for improving outcomes [Reference Chung36]. An example of a CTSA CE project is a community-academic partnership with veteran organizations that helped identify barriers to use of Veterans Affairs services [Reference Franco37]. One approach to evaluating community-academic partnerships for health and the impact of the network of social connections is Social Network Analysis, which has been useful for determining new directions for grant funding agencies [Reference Franco38]. It is important for CE institutions to innovate by developing evaluation tools to assess the impact and outcomes of programs, identify best practices, and determine what changes and investments are needed to support new and emerging CE applications. Although CE research activities are focused towards population health and medicine, CE research is also focused on furthering the art and science of CE itself.
Policy and Advocacy
Policy is essential to making larger changes to how healthcare is delivered or public health initiatives are developed. AHCs are frequently asked by local, regional, and state governments and communities to participate and partner in developing public health policy and procedures that may be used in broad application [Reference Nelson39]. Research findings may also have implications affecting current medical and research practice, such as developing new IRB training programs [Reference Solomon40]. Institutional leadership or faculty may therefore, become involved in policy making. As government has a significant impact on the healthcare sector, AHCs may send representatives to advocate for governmental health policies that impact patient care, the physician’s ability to provide care, and the communities served by AHCs. For example, for the “Reach Out: Physician’s Initiative to Expand Care to Underserved Americans” program needed to work with state legislators to enact legislation to make volunteer physicians caring for the underserved more risk free [Reference Ahmed and Maurana25]. In this situation, it would have been difficult to run free clinics for the underserved without the extension of Good Samaritan statutes and working with malpractice carriers. Most policy and advocacy work within AHCs is undertaken by institutional leadership and faculty. At other higher education institutions, advocacy and policy may be a primary focus for CE activities. As an essential area for CE, it is important to learn the best methods for increasing the impact from involvement in activities related to policy creation and implementation.
Administrative Functions And Infrastructure
All of these components are supported by essential administrative functions and infrastructure, which includes: promotion and tenure [Reference Bloomgarden and O’Meara41], risk management [Reference Jones and Wells42], leadership support, employee wellness programs, recognition, tracking [Reference Driscoll43], evaluation, financial support [Reference Driscoll43], training, communication, and dissemination [Reference Mendel44], and diversity and inclusion [Reference Tienda45]. These, among other administrative functions, are critical to the CE efforts at an institution, supporting the facilitation of systemic integration of CE, and the development of tools to track, measure, evaluate, and improve on practices in order to foster genuine and sustainable partnership with community [Reference Woollard6, 8, Reference Lazarus9, Reference Szilagyi12].
Overlap
CE programs are ideally developed in partnership between the community and the institution, leveraging the resources of both groups to address community needs and align with institutional priorities. There are times when “bridges” need to be built in order to span 2 disciplines [Reference Ahmed20]. Such a process may generate unique ideas, solutions, and programs that do not serve the purposes of tidy, silo-ed categories, and may incorporate elements of several components within the CE Components Practical Model. For example, the Medical College of Wisconsin’s Saturday Free Clinic for the Uninsured Program increases clinical care access for underserved populations, while also providing an education and training experience for the medical students who are managing day-to-day operations [46]. Several other AHCs offer a similar experience for their medical students serving underserved populations [47]. Another example includes a community-based clinical program that not only sought feedback from the community, but did so in a way that was aligned with the community to maximize the impact of the research [Reference Nelson48].
Conclusions and Future Implications
CE application in AHCs has evolved as more institutions have become involved and adapted its application. Currently, other models exist that address individual parts of the CE components, yet the CE Components Practical Model presents a more comprehensive approach to CE. The CE Components Practical Model also addresses one of the major limitations encountered by the other models—flexibility to tailor to each institution and situation. The broader spectrum of CE activities in the CE Components Practical Model provides AHC’s a widened scope through which they can identify CE activities that align with institutional strengths, priorities, and existing programs. The model is not meant to imply that institutions need to have activities within all components, but to build awareness about the possibilities and allow institutions to define, with their communities, how best to develop and orient CE activities. Beyond AHC consideration, which includes a focus on health and clinical care, other institutions may apply the CE Components Practical Model by reconsidering the component focused on clinical care, and consider their own specialties, applied sciences, and unique assets in its place.
With this model, we hope to reduce confusion about CE among practitioners at AHCs and other academic institutions. The CE Components Practical Model is a systematic and inclusive model to contextualize and recognize the diverse application of CE components at AHCs, including: Community Outreach & Community Service, Education, Clinical Care, Research, and Policy & Advocacy. The model may provide insights, as CE practitioners seek to collaborate in CE activities, strategic planning, administration, evaluation and assessments, and although they may differ the practitioners can find ways to be more inclusive by taking into consideration the full scope of programs and priorities in the CE domain. The model also brings attention to the essential role of administration functions and infrastructure to support these activities. Where academic institutions in general, and AHC’s specifically, are strongly rooted in more traditional practices and methodologies, this model highlights that institutions need to integrate and invest in CE with the same strategies and supportive structures as it pursues other central missions. This foundational understanding of the field of CE will increase the ability of CE practitioners to relate to and to learn from each other by setting a common model to refer to.
The foundation created by the presented model will spur greater discussion among CE practitioners, catalyze research that will determine best practices for all CE components, and support AHCs in practicing CE with increased understanding. As each institution is able to understand the breadth of CE there is an opportunity for AHCs to engage in meaningful ways that align with institutional priorities that are also reciprocal to community priorities and needs. Meaningful discussions can take place that improve and increase the expertise of AHCs in CE and the sophistication with which they integrate CE in their missions.
In addition to how the CE Components Practical Model informs CE practice and program application, the foundation in understanding CE in this broader context can help develop frameworks, metrics, and methods to further the development of assessment and evaluation of CE activities. All practitioners of CE share a commonality in needing to measure and evaluate their work, regardless of how they engage with the community. It is often the common need for measurement and evidence of impact of CE practices that brings practitioners together. Through these conversations, practitioners can be more aware of the limitations of current models of CE for understanding and the resulting tracking, evaluation, and assessment tools. The model presented can inform the development of a comprehensive framework, and evaluation and assessment tools that encompass all types of CE at AHCs and other institutions.
On a national level, developing metrics for CE is an ongoing initiative. Thus far, gathering baseline information about current methods of measuring CE in AHCs has been done in several studies. A study by the University of Rochester-Medical Center discusses how to evaluate CE in academic medical centers, because so many implement new CE activities as part of the CTSA awards and the increasing importance of CE [Reference Szilagyi12]. A recent study by Haldeman et al., looks at biobanks and how CE is understood and implemented [Reference Haldeman49]. Essentially, staff and faculty at biobanks think that CE is important for developing trust with community and gathering participants, yet they fail to know which of their CE activities are the most impactful or how to change their approach to obtain better results [Reference Haldeman49]. Another example is the CFCECF, which collects information on CE achievements, yet the framework gives significant attention to particular CE activities [Reference Pearl50]. A more balanced framework would be more inclusive of all CE activities, and provide the data and evidence required for each CE component, as well as the weight given to the individual components.
Apart from this foundational understanding, more work needs to be done to study current CE activity tracking and evaluation for all components. There is much work to be done to reach the point where all areas of CE have well-founded best practices established for all CE components, and evaluation tools that integrate this full spectrum of CE practice. We put forward The CE Components Practical Model to provide the necessary foundation for a broader perspective of CE practice; and to encourage practitioners and researchers to use it as a basis for development of more comprehensive conversation about CE and evaluation and assessment tools for CE activities.
Financial Support
Funding for this work was supported by: National Clinical and Translational Science Awards 5UL1TR000055-05 and UL1TR001436, NIH and MCW Community Engagement Core Implementation Initiative FP00009037, Advancing a Healthier Wisconsin Research and Education Program.
Disclosures
The authors have no conflicts of interest to declare.



