Introduction
Overweight and obesity are the major risk factors for many chronic diseases, particularly for diabetes, cardiovascular diseases, and cancer (WHO, 2020a). These diseases, namely non-communicable diseases (NCDs), are not only the cause of premature mortality, but also of long-lasting morbidity. Moreover, overweight/obesity in children is linked with impairments in quality of life (Tsiros et al., Reference Tsiros, Olds, Buckley, Grimshaw, Brennan, Walkley, Hills, Howe and Coates2009; Williams et al., Reference Williams, Wake, Hesketh, Maher and Waters2005) and a high risk of teasing and bullying (Lobstein et al., Reference Lobstein, Baur and Uauy2004). One of the major concerns on the subject is that childhood overweight/obesity is likely to continue throughout the adulthood of the individual (Rooney et al., Reference Rooney, Mathiason and Schauberger2011). Thus, the increasing prevalence of obesity poses a significant threat to future demands for healthcare. Eventually, prevention of childhood obesity becomes a priority for reducing the financial and general burden on healthcare.
The prevalence of childhood overweight/obesity has increased significantly in most high-income countries, and is also increasing rapidly in low- and middle-income countries (Sahoo et al., Reference Sahoo, Sahoo, Choudhury, Sofi, Kumar and Bhadoria2015). WHO reported (2020b) that 39 million children under the age of five worldwide were overweight in 2019. The number of overweight preschool children has increased by almost 24% since the year 2000 in Africa. And approximately half of the children under five who were overweight/obese in 2019 lived in Asia (WHO, 2020b). As such, halting the rise in diabetes and obesity in children and adults became one of the global health targets set by the World Health Assembly in 2013 (WHO, 2013). Improving nutrition occupies a substantial place in the Sustainable Development Goals (SDG) for 2015–2030 (WHO, 2016).
In the SDG framework, it is stated that improving nutrition plays a key role in health, education, empowerment of women, employment, progress in poverty, and inequality of a society. Issues such as: poverty and inequality, water, sanitation and hygiene, education, food systems, climate change, social protection, and agriculture have also been reported to have significant effects on the outcomes of nutrition (United Nations, 2015). Economic, genetic, cultural, behavioural, and psychosocial factors are related to excess weight, making this a complicated and multifaceted context (Franks and Ling, Reference Franks and Ling2010; Pérez et al., Reference Pérez, García and Herrera2013). To determine the most powerful strategies for reducing the burden of overweight/obesity and sustainable development, the prevalence and determinants of overweight/obesity must be known (Mohsena et al., Reference Mohsena, Goto and Mascie-Taylor2016). WHO highlights the importance of monitoring levels and trends of overweight/obesity in children (De Onis et al., Reference De Onis, Blössner and Borghi2010). However, in Turkey, preschool childhood obesity is not yet perceived as an emerging health issue and receives inadequate attention and the data related to overweight/obesity trends among preschool children is inadequate. Few studies that have been conducted are cross-sectional, and the data are limited to one year (MOH/HUBDB/NH, 2010; Santas & Santas, Reference Santas and Santas2018). There is a need to conduct studies using world-standard anthropometric measures and shed light on factors associated with overweight/obesity in preschool children in Turkey. This study is one of the first studies to use world-standard anthropometric measures in Turkey with the following objectives: firstly, to describe the prevalence and trends of overweight/obesity among preschool children based on population body mass index-for-age Z-score (BMI-for-age), which is the globally preferred anthropometric measure instead of weight-for-length and -height or weight-for-age. In this way, the worldwide data would be comparable with Turkey. Secondly, to identify the 25-year trends of overweight/obesity in preschool children in Turkey using the recent 2006 WHO standards instead of the National Center for Health Statistics (NCHS) reference. And lastly, to examine whether the maternal/household and individual-level factors are associated with overweight/obesity in preschool children using TDHS 2003, 2008, and 2013 datasets.
Methods
Data source
Demographic and Health Surveys (DHSs) are regularly carried out in over 90 countries worldwide and provide for the major basic demographic indicators and the health status in those countries to be measured by validated questionnaires. DHS uses a weighted, multi-stage, stratified cluster sampling methodology that represents the general population. In this study, the data provides the prevalence and trends of overweight and obesity among preschool children, and is obtained from the last five TDHSs conducted by the Hacettepe University Institute of Population Studies (HIPS) in 1993, 1998, 2003, 2008, and 2013. To examine whether the maternal/household and individual-level factors are associated with overweight/obesity in preschool children, a pooled data of TDHS 2003, 2008, and 2013 is utilized. The prevalence of overweight/obesity was doubled beginning from TDHS 2003 when compared to the previous two TDHSs. The main reasons why only the last three TDHS studies were used are; a) it is possible to get more feasible results with contemporary data, b) to add comparability to the results of this study under a high-prevalence overweight/obesity setting. Moreover, a larger set of data is obtained by pooling the last three surveys which led to the increased number of observations and more reliable estimations. More details about TDHS surveys are available in the survey reports (HIPS, 2020).
The dataset included information from children under five years old and their mothers aged between 15 and 49 years old. Children with no anthropometric measurements or who have had implausible measurements were excluded. The children with pregnant mothers were also excluded because variables such as maternal BMI and maternal employment status were affected by pregnancy and could mislead the results. Among the total of 14,231 eligible children to identify the overweight/obesity prevalence, the contribution of the TDHS 1993, 1998, 2003, 2008, and 2013 was 2872, 2547, 3704, 2528, and 2580 children, respectively. When the TDHS 1993 and TDHS 1998 were excluded, the pooled data of 8,812 children under five years old were included in the analysis to examine the factors associated with overweight/obesity (Figure 1).

Figure 1. The study flowchart of the selection of the final study population from the TDHS datasets.
Anthropometric measurements and outcome variables
Weight and height/length were measured by trained staff contracted by the DHS survey, using standardized measuring equipment. The supine length was measured for children below 24 months and standing height was measured for children over 24 months. Details on anthropometric measurement in DHS can be found in (ICF International, 2012). Overweight was defined as body mass index-for-age more than 2 standard deviations (SD) above the median of the reference population (BMI-for-age >+2) and obesity was defined as BMI-for-age more than 3 SD. Children with BMI-for-age Z-score above 2 SD were categorized as overweight/obese and 2 SD or below as normal. Implausible values beyond +/- 5 SD were excluded based on recommendations by WHO (2019a).
Multicentre Growth Reference Study and 2006 WHO Child Growth Standards
Standard implementation for examining anthropometric data is the comparison of the population studied with a reference population based on the properties of the normal distribution. It enables to compare the changes between the anthropometric indicators of different groups in the community and the changes that may occur in nutritional status over time. It is worth mentioning that the reason for using the reference group is that well-nourished children in all communities follow almost the same growth patterns before puberty (HIPS, 2014).
In 2006, the WHO released the most recent WHO Child Growth Standards (WHO Multicentre Growth Reference Study Group & De Onis, Reference De Onis2006) based on a multi-country study involving breastfed infants and young children from 6 geographically distinct countries (Brazil, Ghana, India, Norway, Oman, and the United States). However, in TDHS-1993, TDHS-1998, and TDHS-2003 databases, the analyses were based on estimates derived from NCHS growth references (Hamill et al., Reference Hamill, Drizd, Johnson, Reed and Roche1977), which were recommended for international use. But the recent WHO Child Growth Standards differ substantially from the NCHS reference, therefore, the NCHS and recent WHO standards are not comparable and compatible (De Onis et al., Reference De Onis, Onyango, Borghi, Garza and Yang2006). This study aimed to describe the national prevalence and trends of early childhood overweight/obesity using the recent WHO Child Growth Standards because these standards provide better statistical depth and lead to more robust information out of data in hand. Thus, Z-scores and the prevalence of overweight for 1993, 1998, and 2003 databases were computed using a syntax file provided by WHO (2006). DHS data experts at www.dhsprogram.com were also contacted and requested anthropometric indicators for TDHS 1993, 1998, and 2003 calculated according to the recent WHO standards. Either way, the obtained BMI-for-age indicators gave the same results. Thus, the BMI-for-age from 1993 to 2013 became comparable at both national and global levels.
Independent variables
Independent variables were identified using the standard questionnaires and the DHS recoding manual (ICF International, 2018). Children, mothers, and household characteristics that were considered to be relevant based on the literature were chosen amongst the existing variables in the databases.
Household and maternal characteristics: Region comprised five categories: North, West, Middle, East, and South. Place of residence was urban or rural. Wealth index quintile, a variable indicating an economic well-being score based on housing characteristics and ownership of sustainable goods (Rutstein and Kiersten, Reference Rutstein and Kiersten2004), initially comprised five quintiles: poorest, poorer, middle, richer, richest. For mother’s marital status, the initial categories “married” and “living with a partner” were regrouped into “couple” category; the other initial categories (“never in union”, “widowed”, “divorced” and “separated”) were put together in the “single parent” category. Mother’s age, initially a quantitative variable was recoded into three categories: 15-19, 20-29, ≥30 years. Mother’s BMI, initially a quantitative variable was recoded into four categories, based on the international classification of adult overweight and obesity: underweight (<18.5kg/m2), normal weight (18.5–24.9kg/m2), overweight (25–29.9kg/m2) and obese (≥30kg/m2). Weight and height were measured by trained staff, using standardized measuring equipment. Mother’s mother tongue the initial categories were “Turkish” and “Kurdish”; the other categories (mainly “Arabic” and other languages) were put together in the “Other” category. Mother’s education and father’s education comprised four categories: no/incomplete primary school, primary school, secondary school, high school, and higher. Mother’s employment status comprised three categories: not employed, employed without social security, employed with social security.
Child characteristics: Age of the child was recoded in months’ groups: 0–11, 12–23, 24–35, 36–59 months. Sex of the child was female and male. Type of birth was normal and caesarean. Duration of breastfeeding, initially a quantitative variable, was recoded into three categories: the child is less than 6 months old and is still breastfeeding, <6 months, ≥6 months. Bottle-feeding derived from drank from the bottle with a nipple yesterday/last night variable and comprised two categories: yes, and no. Birth weight was categorized into three groups, based on clinical cut-off points of birth weight: low (<2500g), middle (2500g-4000g), and high birth weight (>4000g). Stunting was defined as height-for-age less than 2 SD below the median of the reference population. Extreme values beyond +/- 6 SD were excluded according to recommendations by WHO (2010). Therefore, stunted, initially a quantitative variable, was recoded into two categories: yes, and no.
Data analysis
The TDHS surveys collect data at the national level, with rural-urban distinction, and at the regional level. Detailed information on all other control variables came from the relevant modules of the survey household and individual questionnaire forms. While the sample designs and questionnaires of the surveys were the same, their sample sizes differed. Consequently, the number of women interviewed and the number of children whose information was collected through birth histories were different. Therefore, to prevent possible biases in the analyses stemming from the different number of observations in different surveys, weighting factors obtained from the equation
![]() $1/\left( {a \times nc/nT\;} \right)$
were used (Marriott et al., Reference Marriott, Campbell, Hirsch and Wilson2007), where a is the total number of surveys, nc is the total number of respondents for the survey c, and nT is the total number of respondents for all surveys. Weighting factors were multiplied by sample weight to obtain a new weight variable and final weights. Using the final weights, the prevalence of overweight and obesity was adjusted and the multilevel analysis was done.
$1/\left( {a \times nc/nT\;} \right)$
were used (Marriott et al., Reference Marriott, Campbell, Hirsch and Wilson2007), where a is the total number of surveys, nc is the total number of respondents for the survey c, and nT is the total number of respondents for all surveys. Weighting factors were multiplied by sample weight to obtain a new weight variable and final weights. Using the final weights, the prevalence of overweight and obesity was adjusted and the multilevel analysis was done.
Categorical variables were compared using the chi-square test. Maternal/household and individual-level factors associated with overweight/obesity were investigated using generalized linear mixed-effects models with canonical link (logit). The group-level variable in this study was the clusters in which the sampling frame was divided; they were called primary sampling units. After the sample size per domain was determined, the sample size was converted to the number of primary sampling units or clusters that would be selected. TDHS surveys included 700, 634, and 642 clusters in 2003, 2008, and 2013, respectively. First, the null model (Model 1-random intercept model) was fitted with no predictors, considering cluster-specific random effects on being overweight/obese. It was then observed that the between-cluster variance was non-zero, and random-intercept fixed slope models were fitted by adding maternal/household and individual level explanatory variables. The second model (Model 2) included maternal/household variables, and the third model (Model 3) included individual-level variables. The final model (Model 4) was fitted for each maternal/household and individual-level variable. The survey year was fitted as a fixed effect in all multivariate models. Between-cluster effects were presented with an intra-class correlation coefficient (ICC, %), a proportional change in variance (PCV, %), and median odds ratios (MOR). The ICC represents the proportion of the total observed individual variation in the outcome that was attributable to between-cluster variation. It was calculated by the formula
![]() ${\tau ^2}\;/\left( {{\tau ^2} + {\pi ^2}/3} \right)$
where
${\tau ^2}\;/\left( {{\tau ^2} + {\pi ^2}/3} \right)$
where
![]() ${\tau ^2}$
denotes the between-cluster variation. PCV represented the proportional change in cluster variation between the null model and model 2, model 3, model 4, respectively. MOR was the median distribution of odds ratios comparing two randomly selected subjects with the same covariate patterns, but in different clusters, comparing the higher risk subject to the lower risk subject. The fixed effects of explanatory variables were provided as adjusted odds ratios (aOR) and their 95% confidence intervals (95% CI). Statistical analyses were performed in R version 3.6.1 (a language and environment for statistical computing, R Foundation for Statistical Computing, Vienna, Austria. URL: https://www.R-project.org) using lme4 package. The significance level was defined at the double-sided p-value of less than 0.05.
${\tau ^2}$
denotes the between-cluster variation. PCV represented the proportional change in cluster variation between the null model and model 2, model 3, model 4, respectively. MOR was the median distribution of odds ratios comparing two randomly selected subjects with the same covariate patterns, but in different clusters, comparing the higher risk subject to the lower risk subject. The fixed effects of explanatory variables were provided as adjusted odds ratios (aOR) and their 95% confidence intervals (95% CI). Statistical analyses were performed in R version 3.6.1 (a language and environment for statistical computing, R Foundation for Statistical Computing, Vienna, Austria. URL: https://www.R-project.org) using lme4 package. The significance level was defined at the double-sided p-value of less than 0.05.
Results
Descriptive statistics
In 1993, 1998, 2003, 2008, and 2013 the prevalence of overweight (BMI-for-age >+2) was 5.3%, 4.9%, 10.0%, 11%, and 11.6%, and that of obesity (BMI-for-age >+3) 1.3%, 0.5%, 1.6%, 2.2%, and 2.8%, respectively. The prevalence of overweight in preschool children had more than doubled over 25 years and the prevalence was higher in males than females each year (Figure 2).
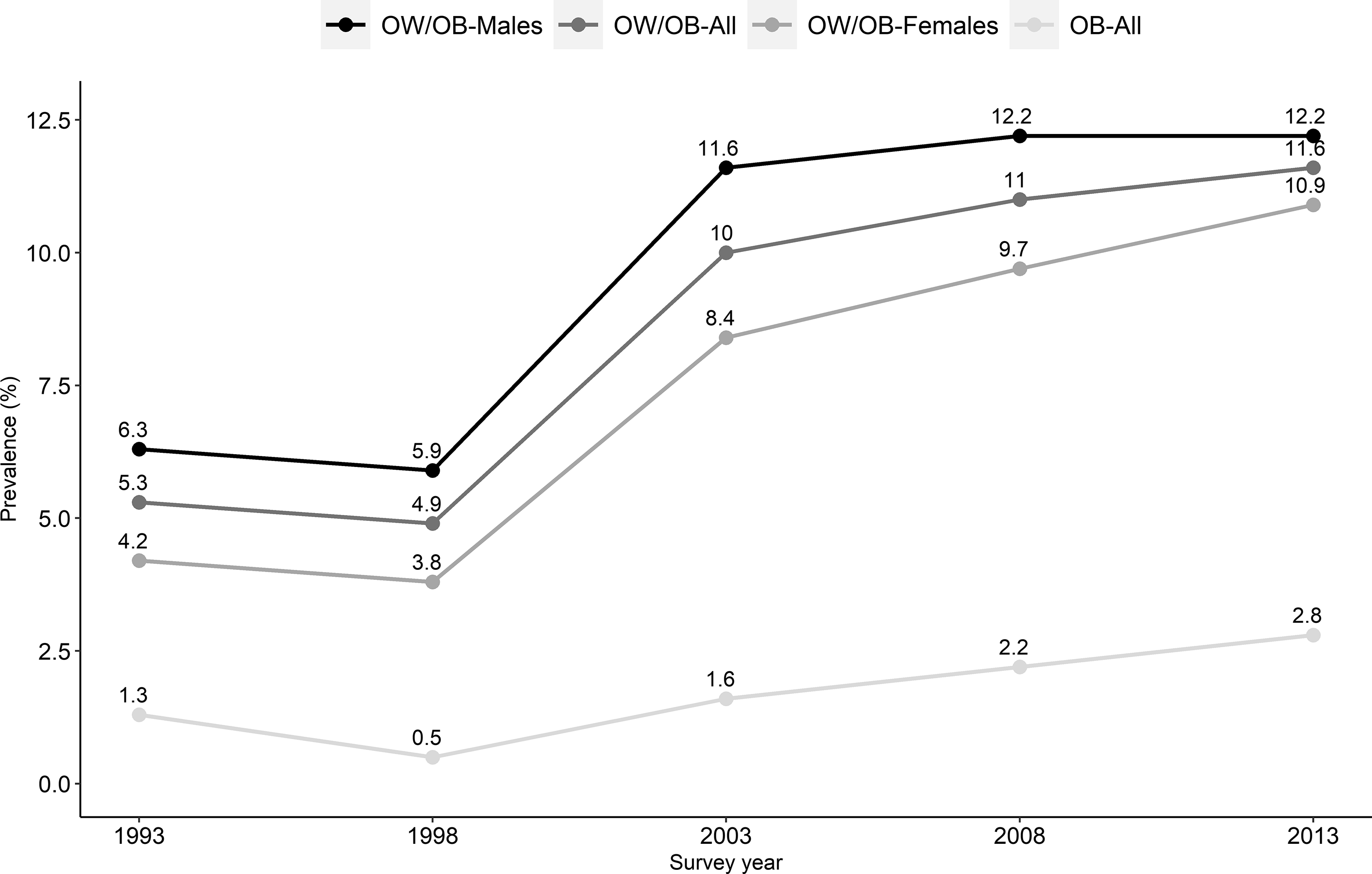
Figure 2. Trend in overweight (OW) and obesity (OB) prevalence among children under five years, Turkey Demographic and Health Survey 1993, 1998, 2003, 2008 and 2013.
Figure 3, TDHS-2003, TDHS-2008, and TDHS-2013 data sets generated by the pooled data sets by region shows the prevalence of overweight children in Turkey. The highest prevalence was in West Anatolia with 13.8%, the lowest in Central East Anatolia with 5.9%, and the average prevalence in all regions was 10.9%.

Figure 3. Prevalence of child overweight across the regions; pooled data from TDHS-2003, TDHS-2008 and TDHS-2013.
Various characteristics of preschool children are presented in Table 1. Data shows that, based on the mother’s education variable, urban settlement has increased, the percentage of adolescent pregnancy has decreased; the percentage of high school and higher education graduates has increased (from 14.6% to 25.9%). A large proportion of mothers (46.5%) were graduates of primary school. Stunting in children decreased from 14.5% in 2003 to 9.6% in 2013. High birth weight has also decreased throughout the years (Table 1).
Table 1. Percentage and frequency distribution of the characteristics of children under five years in Turkey (Weighted)

* : Overweight
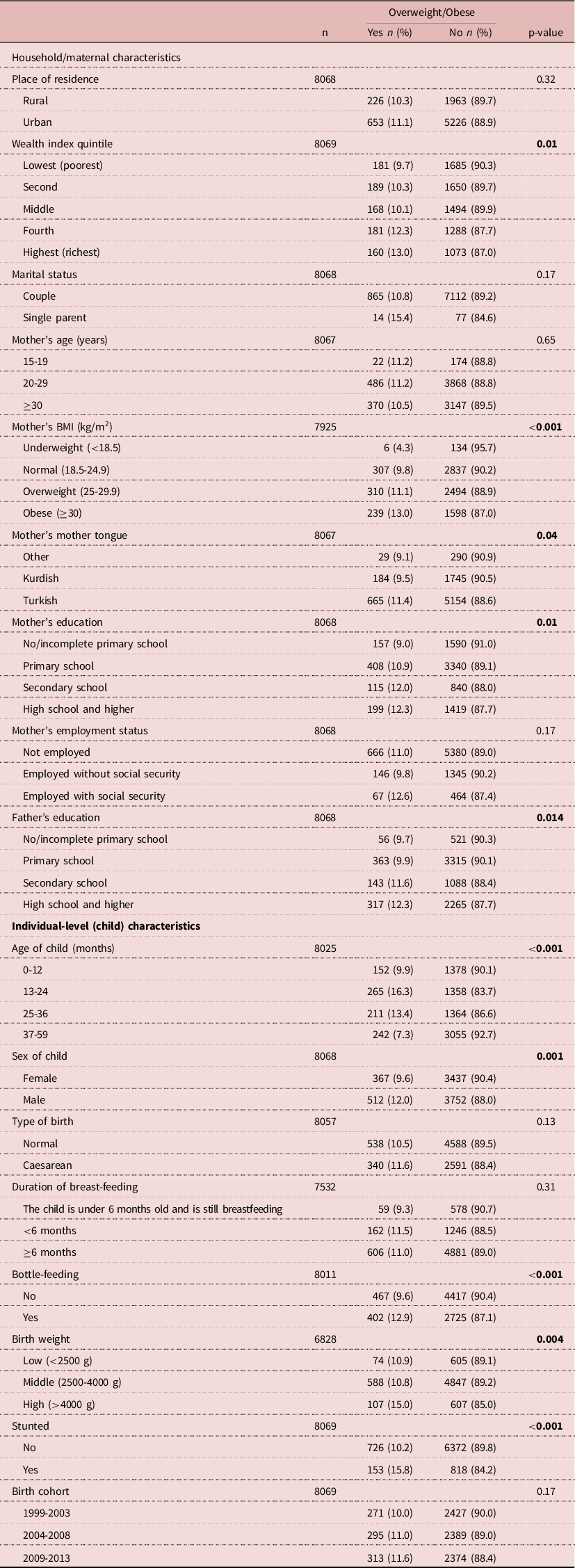
Bivariate associations of outcomes with independent variables
Table 2 shows the descriptive statistics indicating the relationship between overweight status of preschool children and household/maternal- and individual-level factors. No difference was observed in the prevalence of overweight/obesity between children from urban and rural areas. The prevalence of obesity was lowest in the poorest quintile with 9.7%. The difference between the poorest and the richest quintiles (13%) was significant; as well as the difference between the poorest and fourth quintiles (12.3%). Around 24% of mothers were overweight/obese. The prevalence of overweight/obesity among preschool children was the highest among children born to mothers with BMI≥30. The significance was due to the difference between underweight-obese and normal-obese groups. Overweight/obesity was higher in children of women whose mother tongue was Turkish (11.4%), and women who were graduated from a high school or higher education level (12.3%). The statistical significance was due to the difference between no/incomplete primary school and high school or higher education level. As the education level of the father increased, the overweight/obesity status of the child increased, and the significance was due to the difference between primary (9.9%) and high school or higher education graduates (12.3%). The prevalence was the highest in male children (12%), children of age 13-24 months (16.3%), and children who were bottle-fed (13%). Also, the prevalence was higher among children who had high birth weight (15%). The significance was due to the difference between the low-high birth weight and middle-high birth weight groups. Stunting was also more common among overweight children (16% of stunted children were overweight).
Table 2. Relationship between overweight of children under five years in Turkey and household/maternal and children characteristics’; pooled data from Turkey Demographic and Health Survey 2003, 2008 and 2013 (Weighted)
Results of the multilevel logistic regression models
Table 3 shows the summary measures of between-cluster effects. The ICC derived from the null model was 15.36%, which implies that 15.36% of the individual variation in the odds of childhood overweight/obesity was due to the effect of clusters, while the remaining 84.6% was due to unmeasured differences between the children. When comparing MOR with the ORs for the maternal/household (model 2) and individual (model 3) characteristics, the median effect of clustering on childhood overweight/obesity was high. Results of the pooled-data multilevel logistic regression models were presented in Table 4.
Table 3. Summary measures of between-cluster effects on overweight and obesity in children under five years
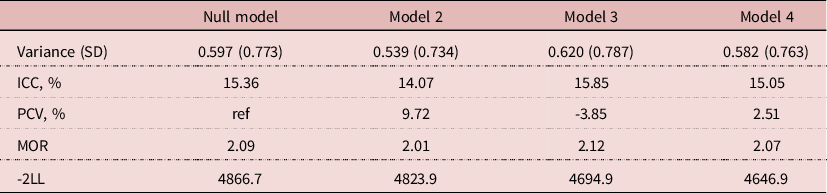
variance: cluster-level variance, SD: standard deviation, ICC: intra-class correlation coefficient, PCV: Proportional change in variance, MOR: Median odds ratio, -2LL: -2×log-likelihood; null model (model 1) is random intercept the only model with no predictors, model 2 included household/maternal variables, model 3 included individual-level variables, model 4 is a final model with both household/maternal and individual-level variables
Table 4. A multilevel analysis of overweight in children under five years by household/maternal and individual-level characteristics; pooled data from Turkey Demographic and Health Survey 2003, 2008, and 2013 (Weighted)
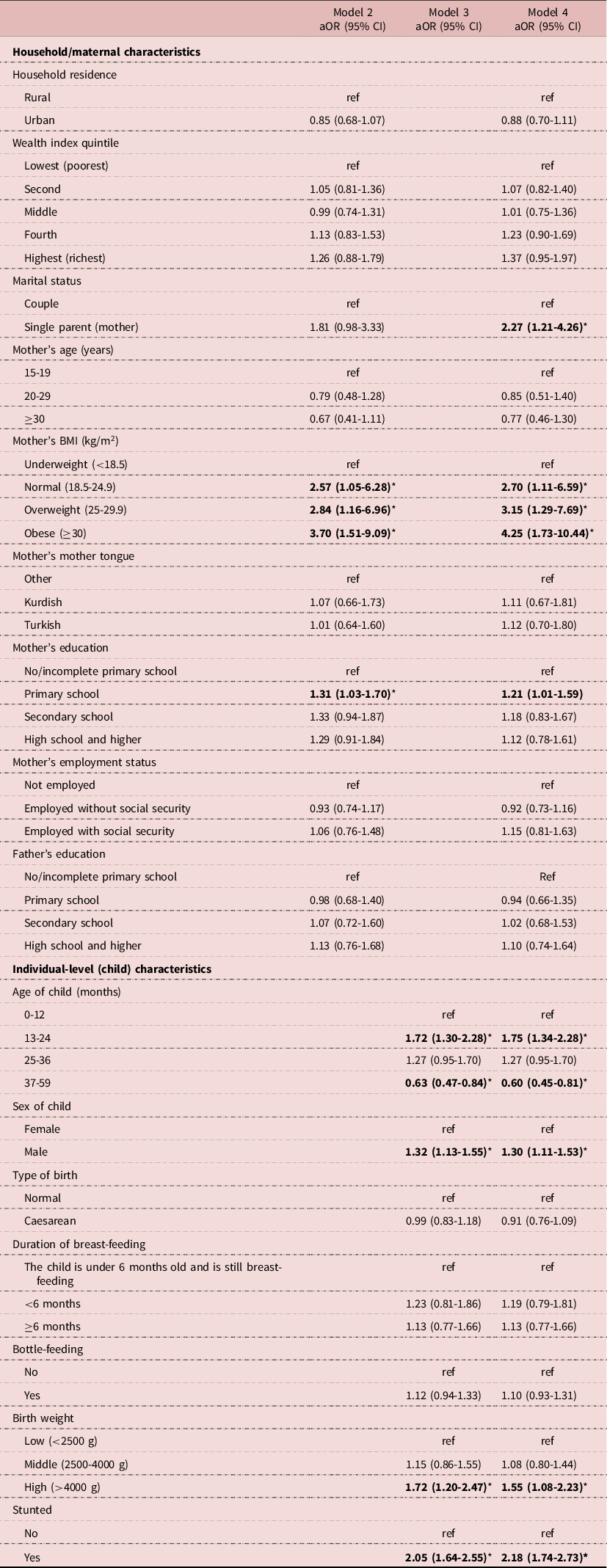
* p<0.05
Model 2 was a multilevel model adjusted for maternal/household level characteristics. The probability of having an overweight/obese child was higher among all the three maternal BMI groups compared to underweight women. Maternal BMI was associated with childhood overweight/obesity - having an obese mother (aOR = 3.70, 95% CI = 1.51–9.09), overweight mother (aOR = 2.84, 95% CI = 1.16–6.96) and normal-BMI mother (aOR = 2.57, 95% CI = 1.05–6.28) compared to having an underweight mother.
In Model 3 - comprising the individual-level characteristics - one-year-old children were more prone to be overweight/obese – 72% (95% CI = 1.30–2.28), compared to zero-year-old children. Also, children over 36 months old had lower odds (aOR = 0.63, 95% CI = 0.47–0.84) of being overweight. When examined by sex, overweight/obesity in male children was 1.32 (95% CI = 1.13–1.55) times higher than in females. Children having high birth weight were 1.72 (95% CI = 1.20–2.47) times more likely to be overweight/obese compared to children having low birth weight. Overweight/obesity in stunted children was 2.05 (95% CI = 1.64–2.55) times higher than children who weren’t stunted.
Model 4 included both maternal/household and individual-level characteristics. Overweight/obesity was 2.27 (95% CI = 1.21–4.26) times more common among children living in single-parent households compared to those living in dual-parent households. As the mother’s BMI increased, the frequency of overweight/obesity increased in children. Children having normal-BMI mothers were 2.70 (95% CI = 1.11–6.59), having overweight mothers were 3.15 (95% CI = 1.29–7.69), and having obese mothers were 4.25 (95% CI = 1.73–10.44) times more likely to be overweight/obese compared to children having an underweight mother. Overweight was higher among children of mothers who have completed primary school (aOR = 1.21, 95% CI = 1.01 to 1.59) than children of mothers who have not completed primary school. One-year-old children had a 75% higher risk (95% CI = 1.34–2.28) of being overweight/obese than children aged 0-12 months. Conversely, children over the age of three had a 40% lower probability of being overweight/obese than children aged 0-12 months. In addition, overweight/obesity in male children was 1.30 (95% CI = 1.11–1.53) times higher than females. Children with high birth weight had a 55% (95% CI = 1.08–2.23) higher probability of being overweight/obese compared to children with low birth weight. Stunting in preschool children was a constituent that accompanied overweight/obesity. Stunted children were 2.18 (95% CI = 1.74–2.73) times more overweight/obese compared to children who weren’t stunted.
Discussion
This study examined the relationship between selected socio-economic, bio-demographic variables and the overweight status of under-five-year-old children in three consecutive TDHSs between 2003 and 2013; and identified the 25-year prevalence of overweight/obesity using TDHS 1993, 1998, 2003, 2008, and 2013 datasets. There is extensive literature in examining the factors of child nutritional status in a wide range of countries, utilizing different analytical methods. However, previous studies have mostly used standard multiple linear or logistic regressions. DHS data have a hierarchical structure, with children nested within women, women clustered within households, and households nested within communities. Observations from the same group are expected to be more alike at least in part because they share the common characteristics or have been exposed to a habitual set of conditions, thus violating the standard assumption of independence of observations native in conventional regression models. As a result, in terms of analysing such data, standard statistical methods are expected to lead to valid results unless some allowance for clustering is made (Duncan et al., Reference Duncan, Jones and Moon1998; Rasbash et al., Reference Rasbash, Steele, Browne, Goldstein and Charlton2013). Multilevel models are technically stronger as well as provide an analytical structure with a much greater capacity for generality when compared to the conventional single-level statistical methods (Raudenbush & Bryk, Reference Raudenbush and Bryk2002). For example, in a recent study using logistic regression in the TDHS-2013 data set, Santas and Santas (Reference Santas and Santas2018) found that, contrary to the findings in this study, overweight/obesity was found to be significantly more common among female children than males. In two studies using similar anthropometric criteria in the same data set, the reason for finding different overweight/obesity-related factors could be due to the use of statistically different methods. Therefore, taking the clustered data structure into account, in this study, multilevel logistic regression models are fitted to assess the relationship between bio-demographic, socioeconomic variables, and overweight status.
Childhood obesity is associated with critical health problems and the risk of early NCDs. Studies have highlighted that the body weight of children under five years is a substantial predictor of health at older ages (Brophy et al., Reference Brophy, Cooksey, Gravenor, Mistry, Thomas, Lyons and Williams2009; Deckelbaum & Williams, Reference Deckelbaum and Williams2001). Monitoring related trends are important for combating obesity in early childhood. The findings of this study show that the prevalence of overweight/obesity in preschool children in Turkey was 5.3% in 1993; 4.9% in 1998; 10.0% in 2003; 11% in 2008; and 11.6% in 2013. Preschool children’s overweight/obesity in Turkey were presented for the first time in 2013 TDHS. In this report, children who were two standard deviations above the median weight-for-height were considered overweight/obese and 11% of children under the age of five were found to be overweight/obese. The WHO recommends assessing obesity in preschool children with the BMI-for-age which is also the globally preferred measurement (WHO, 2008). This study identified overweight/obesity based on BMI-for-age instead of weight-for-length/height and weight-for-age. Nevertheless, weight-for-length/height and BMI-for-age yield close results, which suggests comparability between indicators for assessing overweight/obesity in children aged under five (De Onis et al., Reference De Onis, Blössner and Borghi2010). This study has already shown that the 2013 results were similar to the weight-for-height measurement in the TDHS-2013 report (11.6% vs 10.9%).
On a large scale, Turkey Nutrition and Health Survey (TNHS) conducted in 2010, which included 2567 preschool children, found the rate of overweight/obesity (BMI-for-age Z-score ≥ + 2 SD) as 8.5%. In TNHS, the researcher or the mother might have chosen the healthier child and therefore the actual prevalence might have been higher (MOH/HUBDB/NH, 2010). The results of this study are consistent with the results of other studies in Turkey. For example, in a 2003 study conducted in Izmir (Ucar et al., Reference Ucar, Dizdarer, Darcan, Korkmaz, Ergudenler, Asilsoy, Bilgili, Ozcan, Simsek and Coker2009) - one of the larger cities in Turkey - found the prevalence of overweight among children aged 2-6 years as 10.3%. Also, in a cross-sectional study (Kondolot et al., Reference Kondolot, Balcı, Ozturk, Mazıcıoglu, Hatipoglu, Kurtoglu and Ustunbas2011) conducted in Kayseri, Turkey, in 2010, the prevalence of overweight among children aged 0-84 months was found as 10%.
In another study of Santas and Santas (Reference Santas and Santas2018), which was an advanced analysis performed with TDHS-2013 data, the frequency of overweight/obesity under the age of five, based on weight-for-height indicator, was found to be 8.6%. Z scores based on both the NCHS reference and the recent WHO reference are presented in the 2013-TDHS data set. When the data set in the study of Santas and Santas were examined, it was determined that obesity was evaluated according to the NHCS references, which was used before 2006. In this study, Z scores for TDHS-1993, TDHS-1998, and TDHS-2003 were revised in accordance with 2006 WHO Child Growth Standards, which is the current reference system instead of NCHS references. For the TDHS-2008 and TDHS-2013, Z scores that were based on the recent WHO reference was used. Thus, overweight levels that are comparable globally and between TDHS series were obtained. WHO reports that the current obesity epidemic could be detected earlier in many developed countries if new international standards were applied 20 years ago (WHO, 2019b).
In this study, a doubled prevalence of overweight/obesity among preschool children was found in the early 2000s. The prevalence, which was around 5% before 2000, increased to 10% in 2003. De Onis and Blössner (Reference De Onis and Blössner2000) reported on the prevalence of overweight among preschool children based on data from 94 countries from 160 nationally representative samples. The worldwide prevalence of overweight was 3.3%, and it was found to have increased in 16 of the 38 countries. In 2010, another study by De Onis et al., reported that the global prevalence of preschool children overweight/obesity increased from 4.2% in 1990 to 6.7% in 2010, for a relative increase of 60%. The observed increase in the prevalence of preschool childhood overweight/obesity after 2000 is a likely result of a change in nutrition and physical activity patterns over time. Modernization, urbanization, and the occurrence of contemporary problems such as screen addiction as a result of technological development have led to a decrease in physical activity. This behavioural change is influenced by plural environmental and social factors, including community, national policies, interpersonal, and interaction with biological processes (Huang and Glass, Reference Huang and Glass2008).
The prevalence of overweight is lowest in Central East Anatolia (5.9%) and highest in Western regions (%13.8 and 13.4%) and Istanbul (13.2%) where urbanization is high. In the TDHS reports, the Eastern region has been defined as the least developed region of the country (HIPS, 2014). This finding indicates the inequality between regions, and the need for regional priority for intervention planning.
In the present study, maternal BMI showed strong associations with childhood overweight/obesity, even after controlled for all other socioeconomic and demographic variables. The findings of this study indicate the child of an obese mother is at a greater risk - 4.5 times more - for being overweight than an underweight mother, and this increase in risk correlates positively with the increase in the mother’s BMI. The observed relationship is similar to the results from other studies (Danielzik et al., Reference Danielzik, Czerwinski-Mast, Langnäse, Dilba and Müller2004; Portela et al., Reference Portela, Vieira, Matos, De Oliveira and Vieira2015). Armoon and Karimy’s (2019) also showed that, in Iran, the mother’s obesity increased the risk of the child’s obesity by 4 times. In a similar survey on 3 to 5-year-old children, mother’s obesity was one of the important associated factors of childhood obesity (Gewa, Reference Gewa2010). Familial patterns of obesity result from genes, environment, and behavioural factors working in harmony, especially for young children growing up within the family. It is unlikely that these factors can be considered to work independently. That is, family members with a genetic tendency for obesity are likely to share similar environments, including high fat diets and low levels of activity, that lead to overweight (Birch and Davison, Reference Birch and Davison2001). Some studies have shown high dietary fat intake to be a significant predictor of obesity among women only when there was familial propensity (Pérusse and Bouchard, Reference Pérusse and Bouchard2000). Due to mothers and children exposed to an obesogenic environment that may predispose them to increased risks for the development of overweight, children whose parents consumed high levels of total fat, saturated fat, and cholesterol have been shown to consume high levels of these nutrients (Oliveria et al., Reference Oliveria, Ellison, Moore, Gillman, Garrahie and Singer1992). Overweight mothers are also inclined to not practice in breastfeeding, which leads to their children not benefiting from any preventive impact that breastfeeding may provide (Hediger et al., Reference Hediger, Overpeck, Kuczmarski and Ruan2001). Research studies have also shown that children born to obese mothers are at an increased risk of macrosomia and congenital abnormalities, as well as being obese later in life (Leddy et al., Reference Leddy, Power and Schulkin2008; Sorrie et al., Reference Sorrie, Yesuf and Gebremichael2017).
The results of this study indicate that the overweight rate is higher among children who live in a single parent household. These findings are similar to previous conclusions of some studies (Duriancik and Goff, Reference Duriancik and Goff2019). Schmeer (Reference Schmeer2012) examined the impacts of family structure on obesity among children of age from 3 to 5. Schmeer found that single parenthood resulted in higher BMI scores among the children compared to those children in dual-parent households. Chen and Escarce (Reference Chen and Escarce2010) also concluded that children in single-parent households were at the greatest risk for childhood obesity. Possible explanations for this relationship are that children in single-parent households typically consume foods higher in saturated fat and sugar; have less access to vegetables and fruits; watch more TV (Byrne et al., Reference Byrne, Cook, Skouteris and Do2011; Huffman et al., Reference Huffman, Kanikireddy and Patel2010); and do less physical activity (Augustine and Kimbro, Reference Augustine and Kimbro2017; Duriancik and Goff, Reference Duriancik and Goff2019) than children from two-parent households. Also, financial constraints, greater instability, and unshared responsibilities in housework in single-parent families may be other potential challenges (Duriancik and Goff, Reference Duriancik and Goff2019; Sisson et al., Reference Sisson, Sheffield-Morris, Spicer, Lora and Latorre2014; Yelick, Reference Yelick2017). A current study (Irvin et al., Reference Irvin, Fahim, Alshehri and Kitsantas2018) illustrated that children in single-parent houses had a higher percentage of unmet health-care needs compared to children in dual-parent houses.
This study also implied that the maternal education level and the children’s overweight status are related. Overweight is higher among children of mothers who have completed primary school than children of uneducated mothers. It seems that there is a trend in this relationship when the bivariate analysis is considered; as the mother’s education level increases, the percentage of children that are overweight increases (Table 2). Even though no significant evidence was found in multilevel regression analysis, a similar relationship was also discovered for the education level of the father, in the bivariate analysis. As the father’s education level increases, the percentage of children that are overweight increases. On the other hand, research on the association between maternal education level and overweight/obesity in early childhood did not lead to a definite conclusion. Recent studies across 11 European countries have shown that low maternal education could yield a significant risk of early childhood obesity (Ruiz et al., Reference Ruiz, Goldblatt, Morrison, Porta, Forastiere, Hryhorczuk, Antipkin, Saurel-Cubizolles, Lioret and Vrijheid2016). Interestingly, the relationship between maternal education and children’s overweight status in China and Kenya is different from that in western countries. In the case of China and Kenya, the overweight rate among children with a high maternal education level is higher than that of lower maternal education level (Gewa, Reference Gewa2010; Liu et al., Reference Liu, Liu, Lin, Li, Pallan, Cheng and Adab2016). The possible explanation could be that in the given social conditions, mothers who received higher education could find a better position of employment and command higher incomes. Evaluating this relationship with wealth status may yield more accurate results. Also, it should be noted that, while in high-income countries, children living in low socioeconomic level households have higher obesity rates, in developing countries children living in higher socioeconomic levels have higher obesity rates (Han et al., Reference Han, Lawlor and Kimm2010; McCormick et al., Reference Mccormick, Sarpong, Jordan, Ray and Jain2010).
Another important finding in this study the relationship between age and overweight among children. This study showed an increase in the likelihood of being overweight at 13-23 months of age than children aged 0-12 months. Previous studies reported that overweight was more common in infants (McCormick et al., Reference Mccormick, Sarpong, Jordan, Ray and Jain2010; Tchoubi et al., Reference Tchoubi, Sobngwi-Tambekou, Noubiap, Asangbeh, Nkoum and Sobngwi2015). TBSA-2010, a national study conducted in Turkey, the prevalence of overweight under 5 years of age was the highest in the 19-24-month age group (15%) (MOH/HUBDB/NH, 2010). In addition, the present study showed that children over 36 months old had significantly lower odds of being overweight. After the age of 3, there may be a relationship due to the increase in physical activity, with the development of children’s motor skills to a great extent and the ability to go out and play games.
The analyses showed that males had a greater chance of being overweight compared to females. The link between sex and overweight in children is inconsistent across the literature but male predominance was observed in many studies (Benedict et al., Reference Benedict, Hong, Winichagoon, Tejativaddhana and Kasemsup2020; Chen et al., Reference Chen, Chen, Zeng and Li2016; El-Gamal et al., Reference El-Gamal, Babader, Al-Shaikh, Al-Harbi, Al-Kaf and Al-Kaf2020; Kurspahić-Mujčić and Mujčić, Reference Kurspahić-Mujčić and Mujčić2020; Tchoubi et al., Reference Tchoubi, Sobngwi-Tambekou, Noubiap, Asangbeh, Nkoum and Sobngwi2015). However, in some studies female predominance (Jouret et al., Reference Jouret, Ahluwalia, Cristini, Dupuy, Nègre-Pages, Grandjean and Tauber2007), or no difference was observed (Gewa, Reference Gewa2010; Ogden et al., Reference Ogden, Carroll, Kit and Flegal2012; Reilly et al., Reference Reilly, Armstrong, Dorosty, Emmett, Ness, Rogers, Steer and Sherriff2005), supporting the theory that overweight was an outcome of interactions between genetics, behaviour, and environmental factors.
Birth weight is a strong factor related to the occurrence of overweight/obesity among preschool children studied. Not surprisingly, birth weight higher than 4000 grams involved a high risk for the occurrence of overweight in preschool years. These findings are consistent with previous reports (Armoon and Karimy, Reference Armoon and Karimy2019; Gewa, Reference Gewa2010; Oppitz et al., Reference Oppitz, Cesar and Neumann2014; Tchoubi et al., Reference Tchoubi, Sobngwi-Tambekou, Noubiap, Asangbeh, Nkoum and Sobngwi2015; Yu et al., Reference Yu, Han, Zhu, Zhu, Wang, Cao and Guo2011). The relation between high birth weight and the increased risk of childhood overweight/obesity was attributed to endocrine and metabolic pathways. Moreover, the high birth weight indicated the danger of obesity not only at the preschool-ages but also during the rest of the childhood (Qiao et al., Reference Qiao, Ma, Wang, Li, Katzmarzyk, Chaput, Fogelholm, Johnson, Kuriyan and Kurpad2015; Rugholm et al., Reference Rugholm, Baker, Olsen, Schack-Nielsen, Bua and Sørensen2005; Yu et al., Reference Yu, Han, Zhu, Zhu, Wang, Cao and Guo2011). The report of a meta-analysis-based study indicates with high consistency that the high birth weight may lead to a doubling of the long-term overweight risk, regardless of sex, socio-economic status, geographic/ethnic origin, parental weight status, etc. Accordingly, prenatal overfeeding is a key risk factor leading to long-term obesity predisposition (Schellong et al., Reference Schellong, Schulz, Harder and Plagemann2012).
The results of the multilevel regression showed that, in stunted children, the chance of becoming overweight was more than 2 times higher than non-stunted children. This phenomenon has been found consistently in many countries (El-Gamal et al., Reference El-Gamal, Babader, Al-Shaikh, Al-Harbi, Al-Kaf and Al-Kaf2020; Gewa, Reference Gewa2010; Mamabolo et al., Reference Mamabolo, Alberts, Steyn, Delemarre-Van De Waal and Levitt2005; Said-Mohamed et al., Reference Said-Mohamed, Bernard, Ndzana and Pasquet2012; Steyn et al., Reference Steyn, Labadarios, Maunder and Nel2005; Tzioumis and Adair, Reference Tzioumis and Adair2014; Wang et al., Reference Wang, Höjer, Guo, Luo, Zhou and Wang2009). Similar circumstances, whether behavioural or environmental factors favour the growth of stunting and overweight in the same household. The mechanism of the association between stunting and overweight is still not conclusive. It has been assumed that nutritional stunting is related to impaired fat oxidation (Hoffman et al., Reference Hoffman, Sawaya, Verreschi, Tucker and Roberts2000b). Secondly, another theory is that stunted children may have a damaged regulation of energy intake, which results in the risk of being overweight (Hoffman et al., Reference Hoffman, Roberts, Verreschi, Martins, De Nascimento, Tucker and Sawaya2000a). Thirdly, mild stunting might be related to a greater sensitivity to the effects of high-fat diets (Sawaya et al., Reference Sawaya, Grillo, Verreschi, Carlos Da Silva and Roberts1998). Furthermore, low physical activity is a substantial risk factor for stunting and being overweight (Said-Mohamed et al., Reference Said-Mohamed, Bernard, Ndzana and Pasquet2012). The double burden should be noteworthy in preschool children in Turkey because the focus of health services should also be overweight as well as undernutrition.
This study implies that, as the household’s wealth index increases, the percentage of obesity in children increases slightly (Table 2). Although this relationship was statistically significant in bivariate analysis, it was not significant in multilevel analysis. Wealth status has been related to health outcomes such as nutritional status, as it is directly linked to the accessibility of nutrition-rich food and living in a healthful environment. This difference may be related to the fact that poor households in high-income countries have easy access to carbohydrate and fat-rich, non-nutritious, obesogenic foods, and in developing countries, the increase in purchasing power and the shift to richer households in access to obesogenic foods.
Although BMI is the main indicator of obesity, various methods are available for the determination of body fat content, such as bioelectrical impedance analysis (BIA), skinfold thickness (SFT), isotope dilution method, measurement of dual energy X-ray absorption (DEXA), and measurement of body K. However, measurement of BMI alone may have limitations in some populations and ethnicities, as it does not distinguish between increases in body weight attributed to increased muscle mass and those attributed to fat (Tascilar et al., Reference Tascilar, Bilir, Akinci, Kose, Akcora, Inceoglu and Fitoz2011; Yilmaz et al., Reference Yilmaz, Inan, Karakas, Buyukozturk-Karul and Sonmez2012). It is important to understand that although BMI and body fat percentage often change simultaneously, a considerable proportion of individuals of certain ethnicities may have a normal BMI but a high body fat content (Kapoor et al., Reference Kapoor, Furler, Paul, Thomas and Oldenburg2019; Kryst et al., Reference Kryst, Żegleń, Wronka, Woronkowicz, Bilińska-Pawlak, Das, Saha, Das and Dasgupta2019). This phenotype is known as ‘normal weight obesity’ and is commonly described in individuals of Asian descent. The prevalence of normal-weight obesity varies widely among different populations, with the highest prevalence found in Korean women (Kapoor et al., Reference Kapoor, Furler, Paul, Thomas and Oldenburg2019; Kim et al., Reference Kim, Han, Kwon, Song, Yim, Lee and Park2014; Franco et al., Reference Franco, Morais and Cominetti2016). At this point it may be useful to use other available methods to estimate body fat content besides BMI. Two methods most widely used in clinical practice in countries like India are DEXA scanning and BIA (Kapoor et al., Reference Kapoor, Furler, Paul, Thomas and Oldenburg2019). In a study (Yilmaz et al., Reference Yilmaz, Inan, Karakas, Buyukozturk-Karul and Sonmez2012) comparing the methods used in the assessment of obesity in Turkish children, BMI measurement is recommended as a useful, easily performed, and reproducible method. Moreover, in this study, it was observed that BIA may prevent the false diagnosis of obesity, which is possible when using BMI measurement alone, particularly in boys during the pubertal term. Therefore, although there is a good correlation between body fat percentage and BMI, the limitations of BMI measurements in terms of ethnicity and gender should be considered. It is recommended that researchers consider the use of these indicators not individually, but in conjunction with each other (Kapoor et al., Reference Kapoor, Furler, Paul, Thomas and Oldenburg2019).
The limitation of this study was the cross-sectional design of the DHS dataset which limits the capacity to infer causality. This requires further research using longitudinal data. Another limitation of the present study included a lack of data on nutritional status and physical activity, which are important components in the prediction of overweight status due to the unavailability of variables in the dataset.
Despite these limitations, it is necessary to underline the strengths of the study. Firstly, the DHS data produce a nationally representative prediction of overweight among children in Turkey using appropriate weighting techniques. For the first time in this study, the prevalence of overweight in 25 years and the trend of pre-school children in Turkey were examined. As TDHS is repeated every 5 years, all children born from 1988 to 2013 were represented. Secondly, recent studies show that the choice of growth standard is important for identifying the onset of becoming overweight in children (Evellen Vandijk and Inni, 2009). In this study, Z scores were revised according to the recent WHO Child Growth Standards, which is the current reference system instead of NCHS references. Consequently, globally comparable overweight/obesity prevalence was obtained. Thirdly, factors associated with overweight were examined by multilevel analysis, which is appropriate to the nature of the data set.
In conclusion, the rise in overweight/obesity in preschool children since the early 2000s has been dramatic in Turkey. This result points to the need for urgent and effective interventions to reverse worsening trends. Multilevel analyses indicate a relationship between birth weight and overweight gradient, so, affected children should be assessed for becoming overweight in routine health follow-ups from birth. The strong relationship between overweight and stunting indicates the need to clarify the risk factors for the double burden. This study pointed to the relationship between overweight in preschool children and family structures as an important finding. There is a need to focus on identifying potential challenges in single-parent families to help improve family-based interventions. In this study, besides the characteristics of the child such as age and sex, some factors belonging to the household and the parents were found to be associated with being overweight. These findings indicate that interventions that target reducing childhood overweight/obesity should be handled with parents and communities as well as children. The first thing to do for proper intervention programs is to monitor the trend of overweight. Findings are expected to contribute to the plan of prevention strategies to address the rising burden of preschool children’s overweight/obesity and its considerable morbidity and mortality in adulthood in Turkey.
Acknowledgments
The authors would like to thank the anonymous reviewers and editor of this journal for their comments, which considerably improved the manuscript. The authors also acknowledge the Hacettepe University Institute of Population Studies and all women and children who participated in TDHS. The authors would also like to thank Ali Görçin and Veene Sulaivany for English language editing.
Ethical Approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Funding
This research received no specific grant from any funding agency, commercial entity, or not-for-profit organization.









