Introduction
Worldwide, socioeconomic transitions have shaped the trajectory of human reproduction, and in general, have predicted reproductive behaviour and fertility change (Bongaarts, Reference Bongaarts2009). However, unlike global trajectories of fertility transition, in India, changes in fertility have not been entirely driven by progress in socioeconomic and health status. The country has been experiencing an unusual process of fertility transition, where a rapid decline in fertility levels occurs irrespective of slow socioeconomic development (Goli et al., Reference Goli, James, Singh, Srinivasan, Mishra, Rana and Reddy2021). Fertility decline in India has occurred even in many socioeconomically less-developed regions with relatively high infant mortality rates (IMR). Demographic research in India has reported that the women from economically weaker and illiterate sections of society with relatively low age at marriage have significantly contributed to fertility decline in the country (Drèze & Murthi, Reference Drèze and Murthi2001; Bhat, Reference Bhat2002; McNay et al., Reference McNay, Arokiasamy and Casses2003; Dommaraju & Agadjanian, Reference Dommaraju and Agadjanian2009; James, Reference James2011; Basu & Desai, Reference Basu and Desai2016). Thus, the convergence of India’s TFR towards replacement level fertility is majorly attributed to the success of the intensive family planning (FP) programme initiated in the late 1960s and continued up to the mid-1990s, which resulted in a tremendous decline in fertility levels (Alagarajan, Reference Alagarajan2003; Spoorenberg & Dommaraju, Reference Spoorenberg and Dommaraju2012; James & Goli, Reference James and Goli2016).
This peculiar process of fertility transition has invited considerable attention from many researchers, especially to find out the reasons behind such a process. Several factors have been discussed as likely pathways to fertility decline in India, including improved health outcomes, mortality decline, policy and programmes promoting late marriages, delayed childbearing, birth spacing and sterilization (James, Reference James2011; Spoorenberg & Dommaraju, Reference Spoorenberg and Dommaraju2012; De Oliveira et al., Reference De Oliveira, Dias and Padmadas2014; Dharmalingam et al., Reference Dharmalingam, Rajan and Morgan2014; Vlassoff et al., Reference Vlassoff, Rao and Vishnu Lale2016). In this direction, studies have also reported that a key reason for the changes in reproductive behaviour of women of lower socioeconomic status is the diffusion of institutionalized FP policies and, thereby, the increased use of female sterilization (Bhat, Reference Bhat2002; McNay et al., Reference McNay, Arokiasamy and Casses2003; Dommaraju & Agadjanian, Reference Dommaraju and Agadjanian2009; Srinivasan, Reference Srinivasan2017).
In the Indian context, several studies have identified the defining factors of FP use. Alongside programme factors (incentive and disincentive policies), female education, employment, age at marriage, exposure to mass media and autonomy have been suggested to be significantly related to the use of contraception among married women (James, Reference James1999; Dharmalingam et al., Reference Dharmalingam, Rajan and Morgan2014; Basu & Desai, Reference Basu and Desai2016; Srinivasan, Reference Srinivasan2017). The adoption of contraception is also associated with age at first birth, sex composition of children as well as the regional and residential status of women (Jayaraman et al., Reference Jayaraman, Mishra and Arnold2009). Some studies have argued that the government in some states is involuntarily enforcing women to opt for sterilization through denial of government entitlements on having more than two children (Sharma, Reference Sharma2014; Goli, Reference Goli2021). The majority of these states have limited outreach of diverse FP methods, especially spacing methods. However, a few studies have suggested that the high popularity of female sterilization in some demographically advanced states is related to cultural and contextual factors such as son preference (Rajaretnam & Deshpande, Reference Rajaretnam and Deshpande1994; Clark, Reference Clark2000; Ghosh & Chattopadhyay Reference Ghosh and Chattopadhyay2017), religious norms (Srikanthan & Reid, Reference Srikanthan and Reid2008), women’s domestic power (León Reference León2011) and familial power relations (Saavala, Reference Saavala2013). Also, women’s inclination towards contraceptive use, particularly female sterilization, depends on a range of correlates from individual factors to social- and community-level factors (Dyson & Moore, Reference Dyson and Moore1983; Moursand & Kravdal, Reference Moursand and Kravdal2003). Although voluminous literature has provided sufficient evidence on the association of socioeconomic and cultural variables with female sterilization, the contribution of bio-demographic factors such as C-section births has been largely ignored.
Global studies that have tested the linkages between mode of delivery and subsequent fertility intentions almost unanimously agree that women who undergo C-section delivery for a previous birth are less likely to have subsequent live births than women who previously had a vaginal birth (Oral & Elter, Reference Oral and Elter2007; Ma et al., Reference Ma, Norton and Lee2010; Evers et al., Reference Evers, McDermott, Blomquist and Handa2014). Empirical evidence across the world suggests that C-section birth is highly associated with the increased use of contraception and lowered fertility compared with vaginal birth (Murphy et al., Reference Murphy, Stirrat and Heron2002; O’Neill et al., 2013). Another study by Smith et al. (Reference Smith, Wood, Pell and Dobbie2006) based in Scotland found an increased risk of women who had a history of C-section birth not opting for a second birth. They also found C-section births to be associated with longer inter-pregnancy intervals. In the context of the United Kingdom, previous studies reported that a higher rate of C-section births among women is associated with an increased risk of delayed pregnancy or high inter-pregnancy interval (Murphy et al., Reference Murphy, Stirrat and Heron2002). In the specific context of Scotland, women who underwent C-sections were found to have compromised subsequent pregnancy and experienced involuntary sterilization to avoid risks in future pregnancies (Mollison et al., Reference Mollison, Porter, Campbell and Bhattacharya2005). In the USA, the rate of C-section is high but the trend of tubal litigations following C-section births had decreased as women are increasingly opting for effective reversible contraception over permanent sterilization. However, female sterilization was found to be common among the women living in the South, among Black and Hispanic women, and women with lower income, lower education and higher parity (Chan & Westhoff, Reference Chan and Westhoff2010). In contrast to the USA, demand for female sterilization following C-section was found to be high in Brazil among women from higher socioeconomic status. Even though female surgical sterilization is not officially accepted in the country, it is performed at a high rate during C-section surgeries (Barros et al., Reference Barros, Victora, Vaughan and Huttly1991; Faúndes & Cecatti, Reference Faúndes and Cecatti1993). However, in countries of sub-Saharan Africa, C-section is associated with lowered natural fertility and increased use of contraception. In particular, female sterilization was found to be much more prevalent among women whose delivery of previous birth was through C-section mode compared with vaginal births (Collin et al., Reference Collin, Marshall and Filippi2006). India also highly relies on female sterilization as the primary mode of contraception, rather than modern reversible birth control measures. The National Family Health Survey (NFHS) reported that the prevalence of female sterilization was 35.7% in 2015–16, which accounts for about 62.4% of the total contraceptive use in India (IIPS & ICF, 2017). Many studies have also reported that the poor quality of female sterilization facilities, such as inadequate sterilization of instruments, bacterial infections, no use of anaesthesia, unhygienic hospital wards, and so on, is causing serious health risks or even deaths of women undergoing tubal litigations. This raises serious concerns about the increased rates of female sterilization, and particularly the increased rate of undesirable C-section-led female sterilization, which is the primary focus of this paper. Although it has been speculated that C-section births are increasingly contributing to lower fertility intentions, as indicated by the increase in female sterilizations and lower mean CEB, there is a paucity of empirical evidence on this subject from India.
Over the last few decades, there has been a dramatic increase in the rate of C-section births across the world, including in India (Betran et al., Reference Betran, Merialdi, Lauer, Bing-Shun and Thomas2007). According to NFHS-4 data from 36 Indian states and UTs, the rate of C-section births in some states was as high as 57.7% in 2015–16. Data from successive NFHS rounds have shown an increasing trend in the percentage of women having C-section births – from a low level of 2.9% in 1992–93 to 9.0% in 2005–06, doubling to 17.2% in 2015–16 (IIPS & ICF, 2017; Guilmoto & Dumont, Reference Guilmoto and Dumont2019). The current C-section levels in the country in 2015–16 were way higher than the WHO recommended 10–15% (WHO, 2015). The recent NFHS (2015–16) also reported state-level variation in the occurrence of C-section births, and higher rates in many demographically advanced southern states compared with northern states, with Telangana having the highest rate (58%) followed by Andhra Pradesh (40.1%), Tamil Nadu (34.1%), Puducherry (33.6%) and Goa (31.4%).
A largely under-researched phenomenon in human reproduction in India is the role of bio-demographic factors, such as C-section births, in shaping subsequent reproductive behaviour and how this influences overall fertility decline. The main aim of this study was to identify the likelihood of female sterilization after C-section birth among married women in India. The study hypothesized that the high rate of female sterilization in India cannot be attributed to individual and social factors alone, but that bio-demographic factors such as C-section also contribute significantly and is a key factor linked to the higher rate of female sterilizations and consequent smaller family size in the advanced states of India. If the hypothesis holds, this would indicate a lack of choice for women in terms of methods of FP and an intentional over-reliance on female sterilization for fertility decline in India.
Against this backdrop, this study attempted to test for the association between C-section births and fertility decline using data from a pooled sample of Indian states with data available about C-section births, female sterilization and CEB.
Methods
Data
The study used a cross-sectional perspective to estimate the association between C-section and subsequent reproductive behaviour in women. The data for this analysis came from NFHS-4 – a nationwide survey conducted in India during 2015–16 by the Ministry of Health and Family Welfare (MoHFW) and the International Institute for Population Science (IIPS). It used multi-stage stratified random sampling, and the sample size was sufficient to perform robust statistical analyses. This study was based on 255,726 currently married women from demographically advanced and less-advanced states of India. Information on family planning, type of birth and CEB, along with socioeconomic and demographic characteristics, were used in the analyses. NFHS data are available in the public domain, so ethical approval was not required for this study.
Statistical analysis
Bivariate tabulations, correlation plots and multivariate regression models were carried out to investigate: (i) the association between C-section births and female sterilizations, and (ii) the association of C-section births and female sterilization with CEB. The bivariate distribution of using any FP method or female sterilization after last birth was shown with disaggregation of C-section and non-C-section births and by order of last birth. The robustness of the estimates was checked through their distribution within the 95% confidence interval. Adjusted predicted probabilities of having female sterilization for C-section and non-C-section births were estimated through logistic regression, and post-regression estimates were performed to measure the predicted probabilities. Given the distribution of births data, the study used Poisson regression to estimate the relative effect of C-section birth compared with non-C-section birth of the preceding birth on CEB net of other socioeconomic covariates.
Poisson regression is a generalized linear model where the outcome variable is linked with logarithmic function. The natural logarithm of mean CEB is expressed as the linear function of a set of independent variables. In this model, birth is assumed to be a Poisson process whose probability of occurrence is constant at any point in time and the mean number of CEB and its variance are equal:
Mathematical proofs of the models are reported below following Engelhardt et al. (Reference Engelhardt, Kohler and Prskawetz2009). It is postulated that the mean CEB depends on a set of predictors
![]() ${x_1},\,{x_2}, \ldots {x_p}$
such that:
${x_1},\,{x_2}, \ldots {x_p}$
such that:
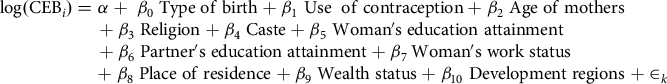 $${\matrix{ {{\rm{log}}\left( {{\rm{CE}}{{\rm{B}}_i}} \right) = \alpha + \;{\beta _0}\;{\rm{Type}}\;{\rm{of}}\;{\rm{birth}} + {\beta _1}\;{\rm{Use}}\;\;{\rm{of}}\;{\rm{contraception}} + {\beta _2}\;{\rm{Age}}\;{\rm{of}}\;{\rm{mothers}}} \cr {{\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} \hskip 2pt+ {\beta _3}\;{\rm{Religion}} + {\beta _4}\;{\rm{Caste}} + {\beta _5}\;{\rm{Woman's}}\;{\rm{education}}\;{\rm{attainment}}} \cr {{\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} \hskip 6pt+ {\beta _6}\;{\rm{Partner's}}\;{\rm{education}}\;{\rm{attainment}} + {\beta _{7\;}}{\rm{Woman's}}\;{\rm{work}}\;{\rm{status}}} \cr {{\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} \hskip 58pt+ {\beta _8}\;{\rm{Place}}\;{\rm{of}}\;{\rm{residence}} + {\beta _9}\;{\rm{Wealth}}\;{\rm{status}} + {\beta _{10}}\;{\rm{Development}}\;{\rm{regions}}} {{\mkern 1mu} + { \in _k}} \cr }} $$
$${\matrix{ {{\rm{log}}\left( {{\rm{CE}}{{\rm{B}}_i}} \right) = \alpha + \;{\beta _0}\;{\rm{Type}}\;{\rm{of}}\;{\rm{birth}} + {\beta _1}\;{\rm{Use}}\;\;{\rm{of}}\;{\rm{contraception}} + {\beta _2}\;{\rm{Age}}\;{\rm{of}}\;{\rm{mothers}}} \cr {{\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} \hskip 2pt+ {\beta _3}\;{\rm{Religion}} + {\beta _4}\;{\rm{Caste}} + {\beta _5}\;{\rm{Woman's}}\;{\rm{education}}\;{\rm{attainment}}} \cr {{\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} \hskip 6pt+ {\beta _6}\;{\rm{Partner's}}\;{\rm{education}}\;{\rm{attainment}} + {\beta _{7\;}}{\rm{Woman's}}\;{\rm{work}}\;{\rm{status}}} \cr {{\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} {\mkern 1mu} \hskip 58pt+ {\beta _8}\;{\rm{Place}}\;{\rm{of}}\;{\rm{residence}} + {\beta _9}\;{\rm{Wealth}}\;{\rm{status}} + {\beta _{10}}\;{\rm{Development}}\;{\rm{regions}}} {{\mkern 1mu} + { \in _k}} \cr }} $$
where i = 1, 2, 3,…., n and j = 1, 2, 3,…., p. Also, the β
i
values indicate the regression coefficients corresponding to each covariate included in the study and
![]() ${ \in _k}$
is the error term, which is independently and identically normal-distributed:
${ \in _k}$
is the error term, which is independently and identically normal-distributed:
Figure 1 shows the analytical plan and sample selection process for all the models estimated in the study.
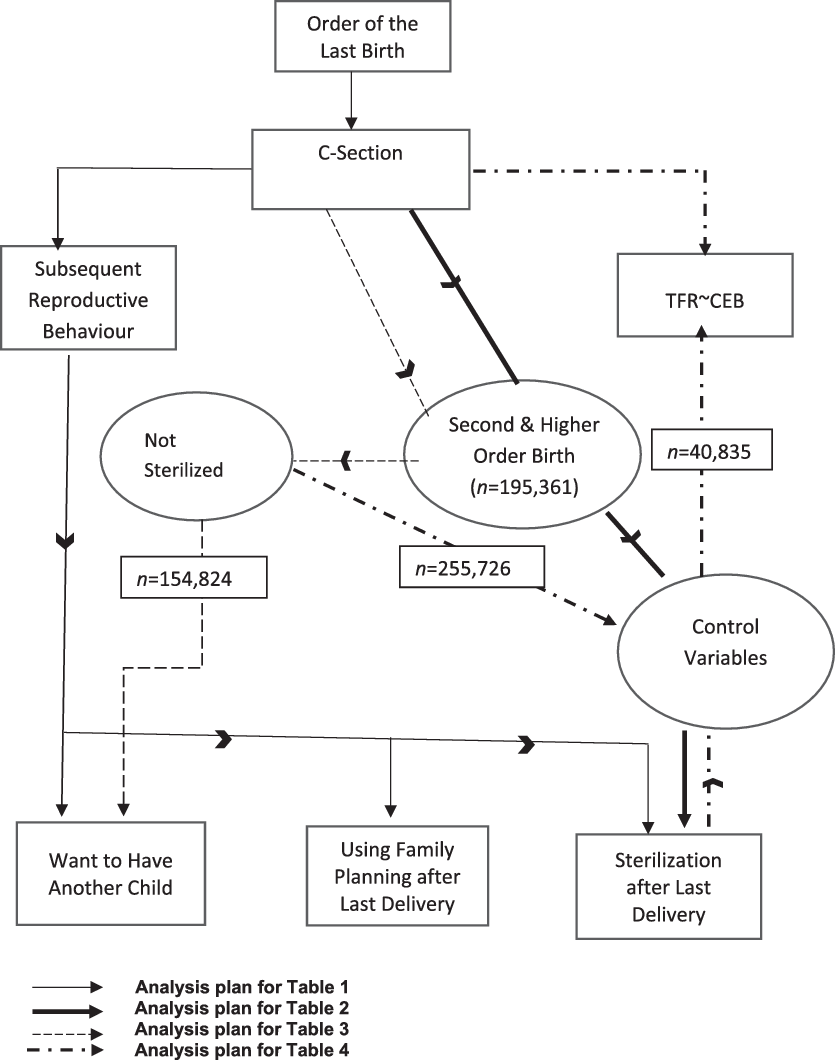
Figure 1. Analysis plan for assessing association between C-section and fertility behaviour.
Results and Discussion
The analysis by state (Table 1) presents alarming levels of C-section births in India in 2015–16, whereby eighteen states and Union Territories (UTs) had levels way above the global threshold of 10–15% designated by the World Health Organization (WHO, 2015). The rate of C-section births was higher in most south Indian states and UTs where fertility levels were already below the replacement level. In addition, several states with below replacement fertility level had conspicuously higher levels of C-section births than WHO guidelines, including Jammu Kashmir, Gujarat, Punjab, West Bengal, Himachal Pradesh and Delhi. Also, a noteworthy share of sterilization was seen in the states and UTs with higher levels of C-section births and below replacement level fertility, especially in south India for second- or higher-order births. Thus, the relationships between C-section births, female sterilization (a fertility-limiting behaviour) and fertility levels are examined in the next section.
Table 1. Percentage of C-section deliveries at the last birth, female sterilization rate and total fertility rate (TFR) by state, India, 2015–2016

a Based on weighted cases.
b Unweighted samples.
Association between C-section births and female sterilizations
The macro (state) level analysis of the association between C-section births and female sterilizations shows a positive linear relationship (r = 0.57). In other words, an increasing trend in C-section births is related to a monotonically increasing trend in female sterilizations (Figure 2). However, the incidence of sterilization following C-section at the last birth presents an incomplete picture of overall reproductive behaviour. Fertility levels and corresponding stopping behaviour are mostly guided by future fertility intentions and type of delivery at the previous birth. Thus, an explicit quantitative assessment of the association between C-section births and sterilizations by birth order can provide more insight into the mechanisms defining completed fertility.
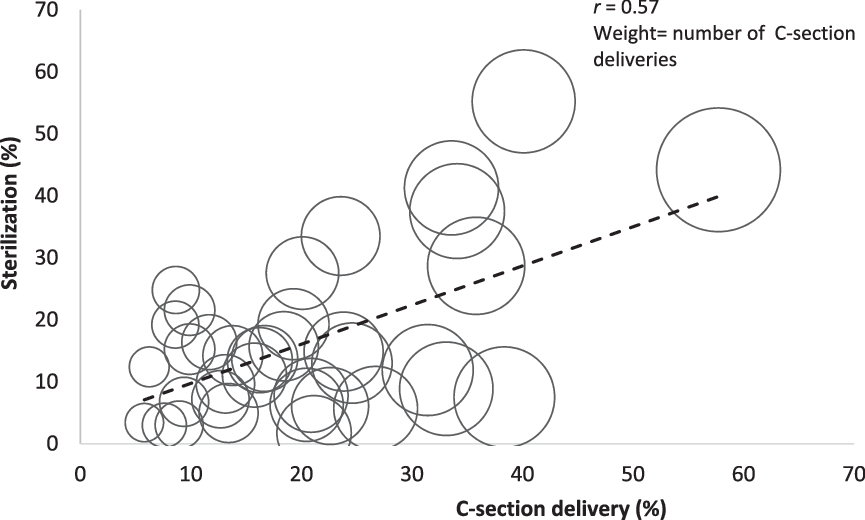
Figure 2. Association between C-section delivery and female sterilization by state.
This section presents plausible empirical evidence through bivariate differences in female sterilization and CEB by type of birth at specific birth order. Irrespective of the order of birth, women who had a C-section delivery had a higher prevalence of sterilization than women who had a normal delivery, except for first-order births (Figure 3). Furthermore, female sterilization was higher in women with C-section births compared with non-C-section births; the difference was large for second and higher-order births (Table 2). For women with birth order second and above, the female sterilization rate was 45.3% (95% CI 44.7–45.9) compared with 22.3% (95% CI 22.3–22.5) in non-C-section births. Similarly, the intention to have an additional child was also significantly less in women with C-section births (13%, 95% CI 12.6–13.4) than non-C-section births (20.5, 95% CI 12.6–13.4) for the preceding birth. This noteworthy difference in sterilization may be an indication of stopping behaviour after two or higher-order births.
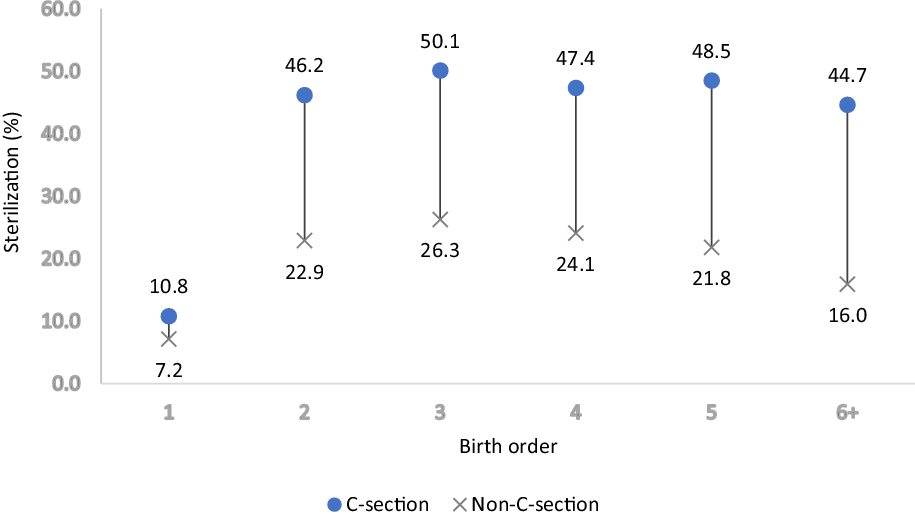
Figure 3. Female sterilization by birth order and type of delivery for last birth.
Table 2. Future fertility intention and sterilization of women after last delivery by type of delivery and birth order of last birth
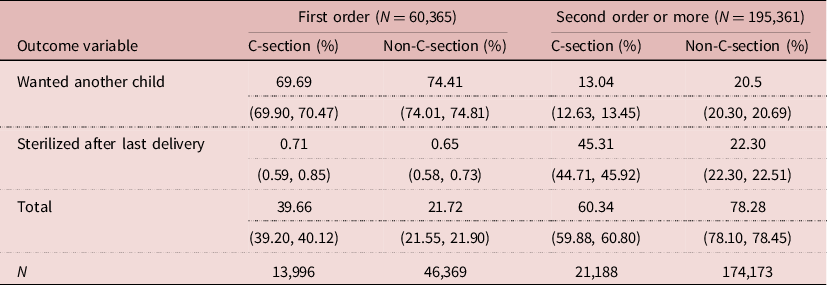
Figures in parentheses are 95% confidence intervals.
Besides the estimation of crude differences in sterilization and future fertility intentions by C-section births, an exercise to explore the relationship between C-section births and sterilization after first birth was carried out. Logistic regression was applied to estimate the net effect of C-section birth on sterilization at two or higher-order births. The adjusted results are in sync with the unadjusted estimates (Table 3). The predicted probability (PP) of female sterilization after second and higher-order births was nearly doubled in the case of C-section births (PP = 0.37, p<0.001) compared with non-C-section births (PP = 0.19, p<0.001) after controlling for socio-demographic factors and regions. The results also indicate that C-section births in India lead to female sterilizations independent of socio-demographic factors.
Table 3. Logistic regression estimates of predicted probability (PP) of having sterilization in women with second or higher order delivery by type of last delivery and other covariates, India, 2015–16
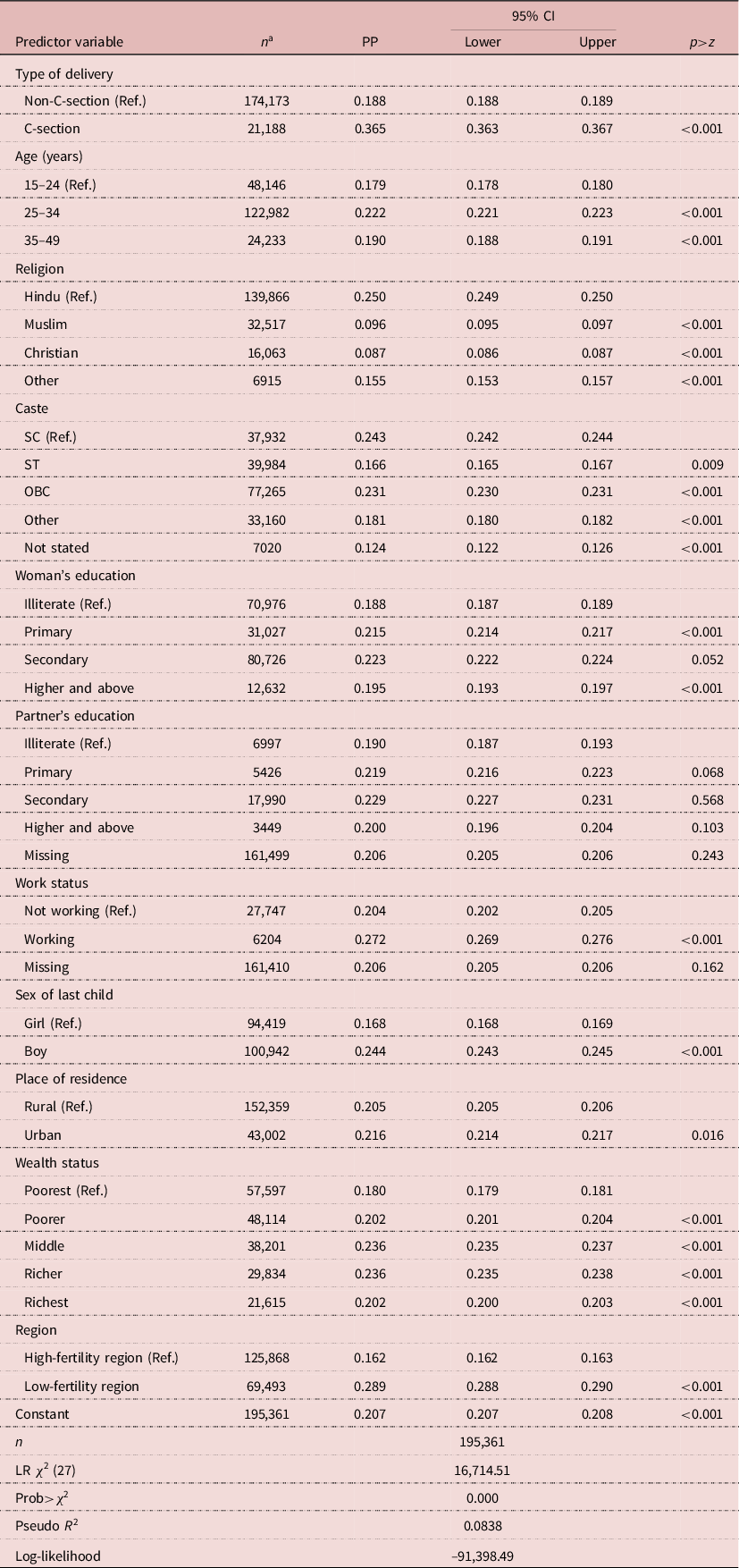
a Includes women whose last delivery was second order or more.
Ref.: reference category.
In the Indian context, explanations of pathways to C-section-induced sterilization may include both medical and non-medical factors. In a global context, there is evidence that women of low body mass index (BMI) and of shorter height should not have more than two or three C-section births – and this probably applies to India (Stulp et al., Reference Stulp, Verhulst, Pollet, Nettle and Buunk2011; Xiong et al., Reference Xiong, Zhou, Cao, Zhang, Qiu and Yao2016). Most often, a low BMI in women raises their risk of emergency obstetric complications and consequently the rate of C-section births (Sebire et al., Reference Sebire, Jolly, Harris, Regan and Robinson2001; Ehrenberg et al., Reference Ehrenberg, Dierker, Milluzzi and Mercer2003). There is evidence that the rise in institutional births in India under the Safe Motherhood Scheme has also contributed to increasing the rate of C-section births (Mishra & Ramanathan, Reference Mishra and Ramanathan2002). Thus, if a woman opts for a C-section birth, it is easier to convince them to accept sterilization as a cost-effective strategy – both for the state and the woman’s household.
The association between C-sections and female sterilizations can be attributed to the affordability of C-section birth. Females from lower socioeconomic backgrounds may opt for sterilization soon after a C-section birth as the cost is lower if it is performed then. Thus, C-section-led sterilization may prevent even wanted subsequent births and contributes to involuntary fertility decline. Women with low socioeconomic backgrounds tend to have low level of education and are therefore, less likely to be able to give their informed consent to sterilization. Other factors explaining the high level of post-C-section sterilization among women in the demographically advanced states of India include increased awareness and a strong policy supporting sterilization (Baveja et al., Reference Baveja, Buckshee, Das, Das, Hazra and Gopalan2000) and women’s ambitions (Saavala, Reference Saavala2013). Institutional factors such as a shortage of emergency obstetric care and trained surgeons in public hospitals (Evans et al., Reference Evans, Maine, McCloskey, Feeley and Sanghvi2009), the trauma experienced during a previous birth and FP pressure on women (Bhattacharya et al., Reference Bhattacharya, Porter, Harrild, Naji, Mollison and Teijlingen2006) are the main reasons for other states. These arguments also explain the finding that advanced C-section births induce subsequent female sterilization, which has significantly contributed to an augmented fertility decline in India, even at lower levels of socioeconomic development and higher childhood mortality rates compared with the standards of developed countries during the peak of their fertility transition (James & Goli, Reference James and Goli2016).
Furthermore, the results indicated that the predicted probability of sterilization was higher for a male child (PP = 0.24, p<0.001) compared with a female child at the last birth (PP = 0.17, p<0.001). This shows that sterilization works as an instrument of Meta preference for sons in India when the analysis is controlled for type of last delivery and other covariates. The predicted probability of sterilization for women with two or higher parity is substantially higher in the case of low-fertility regions (PP = 0.29, p<0.001) compared with high-fertility regions (PP = 0.16, p<0.001). This finding corroborates the hypothesis that a region with a lower level of fertility has considerably higher C-section births as well as female sterilizations. Working women (PP = 0.27, p<0.001) also have a significantly higher probability of undergoing sterilization under the controlled effects of type of birth, region and women’s other socioeconomic characteristics.
Future fertility intentions and C-section birth
It has been argued that women who have a C-section at their previous birth have a lesser chance of progression to higher parity births (Norberg & Pantano, Reference Norberg and Pantano2016). This is because of the misconception prevailing in society that having a C-section birth means that subsequent births will have to be by C-section. However, an examination of this hypothesis was not possible using the available dataset as the NFHS does not list all births to a mother by corresponding modes of birth (i.e. C-section or vaginal delivery). Information on type of birth was available for the latest birth only. However, using available information, a significant transition in fertility behaviour was noted among women who had a C-section at their latest birth, especially second- and higher-order births (Table 4). Importantly, in the Indian context, where fertility level has reached replacement level, the role of C-section becomes critical to future fertility intentions, specifically around second-order births. In this context, a net association between C-section births and future fertility intentions was explored for unsterilized women. The results indicate a lower progression to higher-order births for women who had delivered any previous birth through abdomen incision (PP = 0.25, p<0.001). This means that unsterilized women with a previous C-section birth tended to have a lower intention to have an additional birth, but increased practice of FP. The practice of FP for birth spacing also increased notably for women (PP = 0.30, p<0.001) who desired more than two births under the influence of a C-section birth. These findings corroborate those of previous studies, which showed that C-section birth is associated with the birth spacing behaviour of women (Smith et al., Reference Smith, Wood, Pell and Dobbie2006; O’Neill et al., Reference O’Neill, Khashan, Henriksen, Kenny, Kearney and Mortensen2014).
Table 4. Logistic regression estimates of predicted probability (PP) of future fertility intentions of women with second-order delivery who were not sterilized and wanted to have an additional child by type of last delivery and other covariates, India, 2015–16
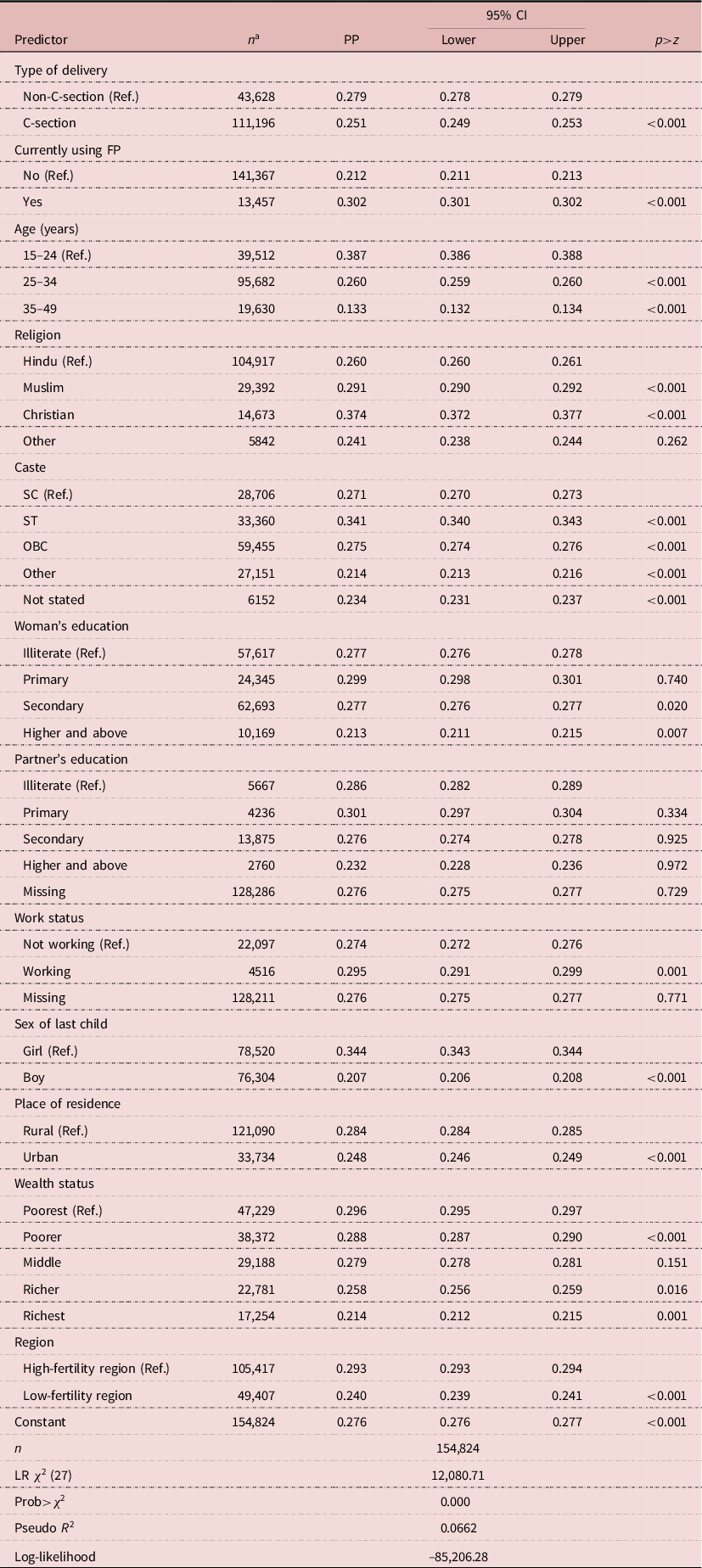
a Includes non-sterilized women whose last delivery was second-order or more.
Ref.: reference category.
The desire for more births decreases substantially when the sex of the last child was male (PP = 0.21, p<0.001) rather than female (PP = 0.34, p<0.001). Socioeconomic indicators such as women’s education and household wealth status considerably limit future fertility desire on moving vertically from the most vulnerable to the affluent category. Most importantly, the predicted probability for future intentions to have more than two children in the low-fertility region (PP = 0.24, p<0.001) was significantly lower than that of the high-fertility region (PP = 0.29, p<0.001). These findings indicate that future fertility intention in both the high- and low- fertility regions is guided by the controlled effect of type of births in India.
The important takeaway message from this is that the sex of the child at last birth and type of birth critically determine the fertility choices and behaviours of unsterilized women in India. Nevertheless, pathways by which C-section birth influence completed fertility are only partially explained in the previous analyses. To account for this, a correlation analysis between C-section births and total fertility rate (TFR) was performed (Figure 4). The correlation coefficient obtained from state-level analysis depicted a significant inverse linear relationship between C-section births and TFR. Conspicuously, the states with TFR below 2.1 had a high share of C-section births (Table 1). Similarly, a high rate of C-section births was also seen among the states and UTs that were on the verge of replacement level fertility. This implies that fertility levels and C-section births reciprocally affect each other. However, there was significant heterogeneity in the level of association at the state level. Spatial disparity in factors, such as availability of modern health technology, and access to and use of antenatal care services, especially in private health institutions, partly explains the increase in C-section births, as well as the pathways of fertility decline, at the sub-national level.
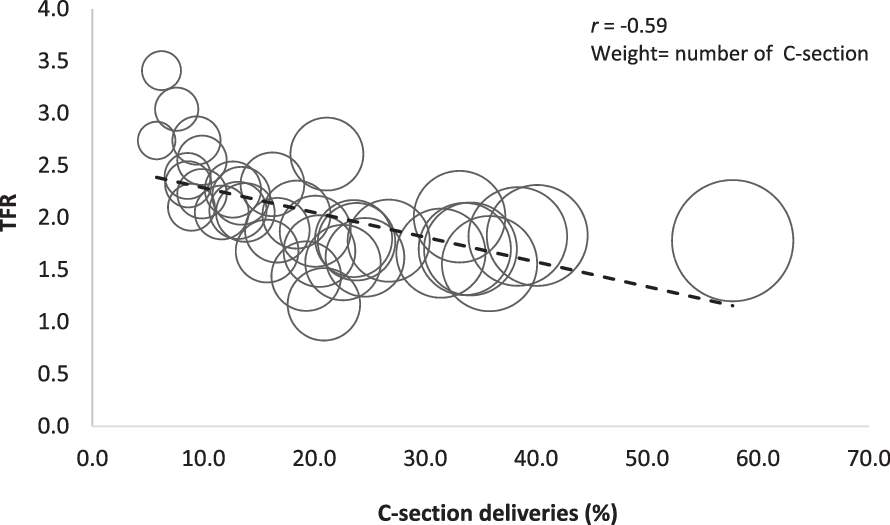
Figure 4. State-level association between level of C-section delivery and TFR.
Table 5. Poisson regression estimates showing the effect of type of delivery and other covariates on CEB to women, India
Ref.: reference category.
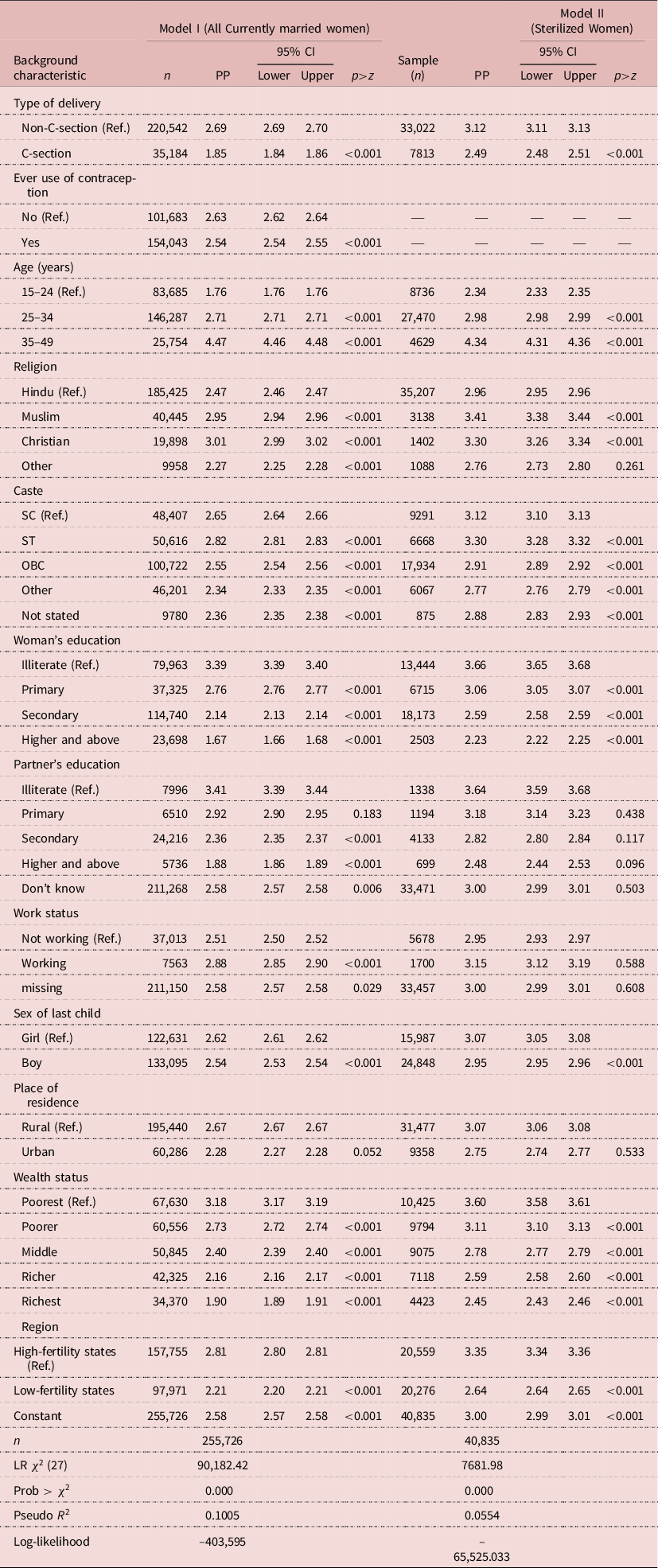
To understand the effect of type of birth on fertility, CEB was used as a proxy for completed fertility. The association of C-section births with fertility was exercised for two sets of samples: a ‘sterilized women’ sample and ‘currently married women’ sample. Table 5 shows the results of the net association between C-section births and CEB after controlling for contraception use and other socio-demographic factors. The results revealed that CEB was significantly lower in women with C-section birth (PP = 1.85, p<0.001) compared with non-C-section birth (PP = 2.69, p<0.001). Separate analyses for sterilized women also indicated that the CEB is significantly lower in women with C-section births (PP = 2.49, p<0.001) than those with non-C-section births (PP = 3.12, p<0.001). This indicates that the completed fertility rate for women under the effect of C-section births is relatively lower than that for their counterparts. A similar gap in completed fertility was observed between the low-fertility (PP = 2.64, p<0.001) and high-fertility regions (PP = 3.35, p<0.001) when the analysis was controlled for type of birth and other socioeconomic and demographic covariates. Furthermore, the completed fertility was lower among higher educated women, women belonging to urban areas and those with improving economic status compared with their counterparts.
C-section delivery, female sterilization and the violation of reproductive rights
Sterilization is a limiting method of FP and needs a surgical procedure for its implementation. Being an irreversible method of contraception, it mandates service providers to adequately inform women of the consequences of undergoing sterilization, especially when births occur in health facilities. However, the estimates from NFHS-4 manifest that three in every five currently married women who were sterilized 5 years preceding the survey were not informed about the side-effects and their management (IIPS & ICF, 2017). There is well-documented evidence of inadequate counselling and advice about other forms of contraceptives and about the side-effects of the sterilization process (Verma & Roy, Reference Verma, Roy, Koenig and Khan1999; Koenig, Reference Koenig2003; Jain, Reference Jain2016). It is noteworthy to mention that sterilization regret has nearly doubled in India is last decade. A study by Bansal and Dwivedi (Reference Bansal and Dwivedi2020) substantiated this observation and noted that one in every five women regret sterilization in resource-poor settings. Importantly, quality-of-care factors such as provider competence, inter-personal relationship between service providers and women and availability of appropriate constellation of services are severely lacking in India (Gupta, Reference Gupta1993; Nataraj, Reference Nataraj1994; Ganatra et al., 1999; Singh et al., Reference Singh, Ogollah, Ram and Pallikadavath2012; Bansal & Dviwedi, Reference Bansal and Dwivedi2020). When aligned with excess C-section deliveries and attributable risk of sterilization, these observations suggest a glaring violation of women’s reproductive rights. The study analysis precisely explains how the rate of sterilization is enhanced in the presence of C-section deliveries (Figure 3). The gap between sterilization among C-section and non-C-section deliveries is high at all birth orders. It can be concluded that C-section deliveries instil an involuntary channel of adopting coercive measures of fertility regulation. This finding corroborates previous studies from other geographies (Sifris, Reference Sifris2010).
Another factor that is typical of patriarchal societies like India is the lack of involvement of women in decision-making regarding FP methods. Women usually have little autonomy and control over their fertility and contraceptive choices (Jeejebhoy, Reference Jejeebhoy1995; Raj et al., Reference Raj, Saggurti, Balaiah and Silverman2009; Oliveira et al., Reference Oliveira, Dias and Padmadas2014) and therefore the decision to undergo sterilization is often not a personal choice. Conspicuously, Figure 5a shows higher sterilization regret among women who were not involved in decision-making on FP. It was observed that among women who were not primary decision-makers on FP method use, sterilization regret was 11.8% for those who had a C-section delivery previously compared with their counterparts who had a normal delivery (6.9%). It is intriguing to note that among women who were involved in the decision-making on FP method use, the share of sterilization regret was nearly the same irrespective of type of delivery. This indicates that C-section delivery positively correlates with ill-informed decisions to undergo sterilization and consequently to higher involuntary sterilization leading to regret of opting for sterilization (Figure 5b).

Figure 5. Female sterilization regret by a) women’s involvement in decision-making on family planning (FP) and b) type of delivery.
Robustness checks
Estimates for sub-samples among high- and low-fertility states were checked for consistency and robustness. The analyses suggest that robustness checks were in tune with findings that emerged based on the total sample (Table 6). The findings from both sub-samples suggest a significant negative relationship between C-section births and CEB, even after controlling for several other determinants of fertility. Women’s education attainment and husband’s education level were also significantly related to lower CEB, which indicates that educated couples plan their fertility even with a previous C-section birth. The results corroborate the findings from a range of other studies which have established that C-section birth reduces the likelihood of subsequent birth compared with spontaneous vaginal delivery (Collin et al., Reference Collin, Marshall and Filippi2006; Smith et al., Reference Smith, Wood, Pell and Dobbie2006; O’Neill et al., Reference O’Neill, Khashan, Henriksen, Kenny, Kearney and Mortensen2014; Norberg & Pantano, Reference Norberg and Pantano2016). However, the results are in contrast with findings from other studies that indicate no association between the occurrence of C-section births and fertility levels (Gurol-Urganci et al., Reference Gurol-Urganci, Cromwell, Mahmood, Van Der Meulen and Templeton2014). This might be due to different contextual factors involved with those studies, which might contrast with the Indian scenario.
Table 6. Robustness checks: estimates based on sub-samples of high-fertility (TFR≥2.1) and low-fertility (TFR<2.1) states, India, 2015–16
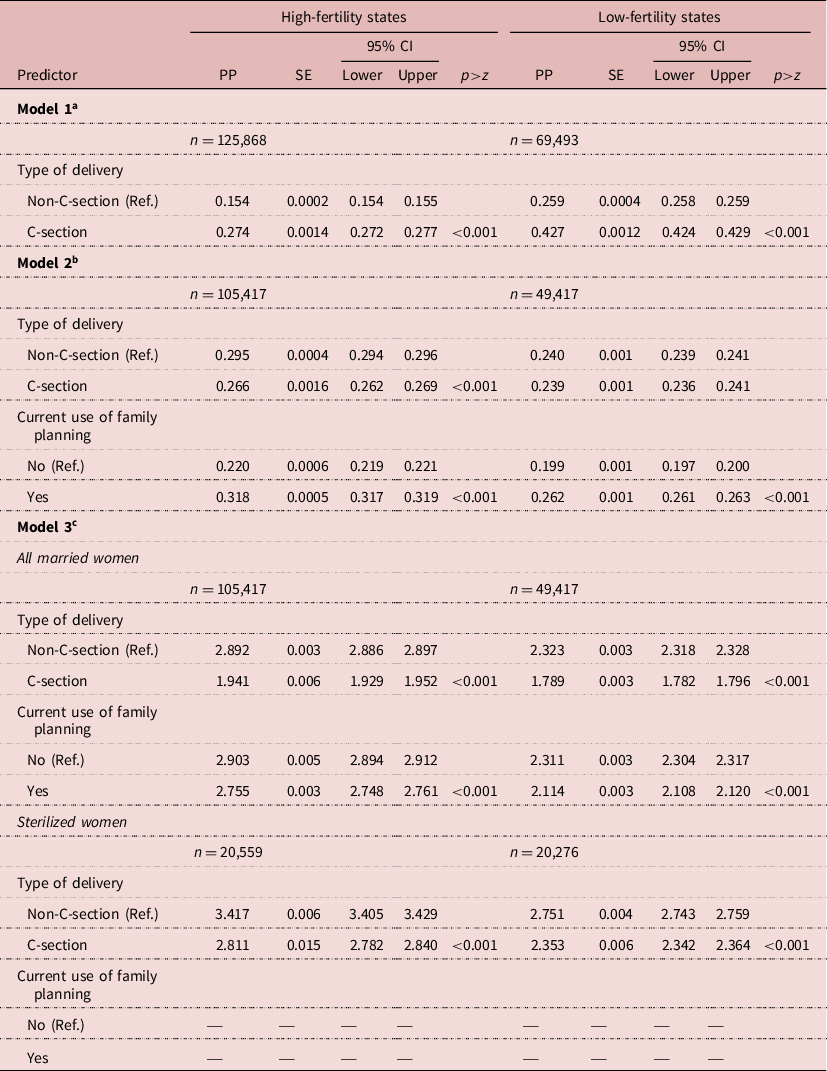
The analysis was controlled for demographic, socioeconomic and biomedical covariates included in the previous models. Ref.: reference category.
a Model 1: logistic regression estimates of predicted probability of having sterilization in women with second-order delivery by type of last delivery.
b Model 2: logistic regression estimates of predicted probability of future fertility intentions: women with second-order delivery but not sterilized and wanted to have an additional child by type of last delivery.
c Model 3: Poisson regression showing the effect of type of delivery and other covariates on CEB in women.
Conclusion
This study attempted to understand and differentiate the nature of the relationship between type of birth and consequent fertility performance among females in India using robust empirical investigation through macro- and micro-level approaches. The macro-level evaluation indicated a positive association between C-section births and female sterilizations. In contrast, it also showed a reciprocal relationship between C-section births and TFR, meaning that an increase in C-section births increases the chance of female sterilization as well as a reduction in overall fertility level. Equivalent findings were noted in the micro-level analyses, which implied lower completed family size among women who experienced C-section births compared with those with non-C-section births. Interestingly, C-section has led to a fertility decline among both sterilized and non-sterilized married women in India. It has contributed to significantly smaller family sizes among sterilized women, while among non-sterilized women it increased use of contraception and a higher intention to have another child was observed.
The study found that females with C-section births had a relatively higher probability of having sterilization, especially after the second birth. Thus, it can be concluded that number of children, progression to higher-order births and the adoption of sterilization are significantly affected by C-section births. In turn, C-section births are affected by the number and sex composition of children at the last birth. There could be two crucial pathways through which C-section affects subsequent fertility levels in India. The first takes the pattern of the more affluent section of society where sterilization followed by C-section is understood as an instrument of wilfully reaching desired fertility goals by bypassing successive physiological pain and the risk of unwanted births. In the second scenario, for poor and rural women, post-C-section sterilization is not always a deliberate decision of women, but an involuntary choice made out of compromises or lack of awareness of other FP methods.
C-section births are widely regarded as life-saving interventions for women with emergency obstetric complications. They are crucial to reducing maternal and infant mortality. However, an excessive prevalence of C-section births is a regressive indicator of public health and maternal health care in any country (WHO, 2015). The over-utilization of C-section shifts resources away from other important medical interventions such as improving maternal health outcomes, maternal and child undernutrition and poor BMI, and inadequate access to other basic health care facilities. The excessive utilization of interventions for medically non-required cases may be harmful to maternal and neonatal outcomes. In most cases, physicians may impose it on women to get higher remuneration or implement state directives (Jou et al., Reference Jou, Kozhimannil, Johnson and Sakala2015). Due to the unreasonable economic burden of C-section deliveries, women’s postnatal care and child care might be affected (Goli et al., Reference Goli, Rammohan and Moradhvaj2018). At the same time, it disproportionately influences fertility desires and reproductive behaviour in a country at various disaggregated levels.
This study suggests that sterilization regret for post-C-section delivery is higher than for normal deliveries, especially when women are not involved in contraception decision-making. Other studies have also reported an overall rise in sterilization regret in India and associated it with quality-of-care issues in the health system (Singh, Reference Singh2018; Bansal & Dwivedi, Reference Bansal and Dwivedi2020). Thus, the C-section deliveries inflate fertility-limiting behaviour through the involuntary imposition of sterilizations as viable FP options among potential users, thereby violating reproductive rights (Sifris, Reference Sifris2010). In particular, the astonishing rise in C-section births pushing an increased rate of unwanted female sterilization is a matter of policy concern. Therefore, this study has broader policy implications in addressing high C-section rates by revisiting intervention strategies towards reducing its over-utilization and preventing involuntary, uninformed or coercive female sterilizations, especially in the demographically advanced states of India.
Although replacement level of fertility is a desired demographic goal for India, the way states are achieving this goal needs rethinking (Sharma, Reference Sharma2014; Goli, Reference Goli2021). Attainment of lower fertility rates without making substantive progress in socioeconomic development, improvement in health and women status has received substantial criticism from the Bucharest and Cairo conferences on Population and Development (Cohen & Richards, Reference Cohen and Richards1994; McIntosh & Finkle, Reference McIntosh and Finkle1995; Goli, Reference Goli2021). Similarly, female sterilization’s involuntary and coercive nature has received strong criticism worldwide (Beckett, Reference Beckett2005; Del Aguila, Reference Del Aguila2006; Schoen, Reference Schoen2001; Goli, Reference Goli2021). Thus, FP programmes in India need to advocate counselling sessions for women before providing postpartum sterilization, which must include providing comprehensive information on the surgical procedure and its associated risks, safety concerns, informed consent, quality of care and choice of modern reversible contraception. Fertility decline in a country should happen through informed choice on FP and must uphold women’s reproductive rights.
Acknowledgments
The authors thank the research assistance and contribution by Deepti Singh and Deepshikha Singh to the previous version of this manuscript.
Funding
This research received no specific grant from any funding agency, commercial entity or not-for-profit organization.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Ethical Approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. NFHS data are available in the public domain, so ethical approval was not required for this study.













