Introduction
The World Health Organization (WHO) defines anaemia as the condition of having a low number of red blood cells or a low amount of haemoglobin (Hb) (WHO, 2020). Anaemia is diagnosed when the concentration of Hb falls below established cut-off values; therefore, the capacity of the blood to carry oxygen to tissues is compromised (WHO, 2017). There are three main mechanisms through which anaemia develops in a human body namely: (a) when the body makes too few red blood cells, known as ineffective erythropoiesis, (b) when red blood cells are destroyed, known as haemolysis, and (c) blood loss (WHO, 2017). The three common contributors to anaemia are nutritional deficiencies, diseases, infections, and genetic Hb disorders (Milman, Reference Milman2011). The prevalence of anaemia caused by nutritional deficiency, particularly iron, is the widest and most common among all other forms of anaemia (Kotecha, Reference Kotecha2011; Abalkhail & Shawky, Reference Abalkhail and Shawky2002; Johnson-Wimbley et al., Reference Johnson-Wimbley and Graham2011). Anaemia diminishes physical and mental capabilities, heightens health risks, and significantly impacts quality of life and work capacity, with symptoms including fatigue, reduced physical stamina, and breathlessness (WHO, 2020; Milman, Reference Milman2011; Jimenez et al., Reference Jimenez, Kulnigg-Dabsch and Gasche2015).
It has been found in several studies that anaemia is a leading cause of adverse pregnancy outcomes and significantly increases the risk factor of maternal mortality, especially in developing countries (Rush, Reference Rush2000; Rahman et al., Reference Rahman, Abe, Rahman, Kanda, Narita, Bilano, Ota, Gilmour and Shibuya2016). In the case of women of reproductive age, anaemia can significantly increase the risk of postpartum haemorrhage, infection, and maternal mortality. On the other hand, it can cause low birth weight and poor neurocognitive and motor development in children (Daru, Reference Daru2022). It is necessary to control anaemia among women in the reproductive age group to prevent low birth weight, perinatal and maternal mortality, and the prevalence of diseases later in life (WHO, 2014). In this regard, the WHO endorsed a comprehensive implementation plan on maternal, infant, and young child nutrition in the World Health Assembly Resolution, 2012, and set a target to reduce anaemia by 50% among women of reproductive age by 2025 (WHO, 2014).
It has been estimated that globally 613 million (33%) women of reproductive age (15–49 years) are affected by anaemia. The countries in Asia and Africa have the highest prevalence rate with a share of more than 35% (WHO, 2017). It was found that every fourth person in the world (27%) has anaemia, whereas the developing countries alone account for more than 89% of the burden of anaemia (Kassebaum et al., Reference Kassebaum2016). The previous studies have identified several socio-economic determinants of anaemia in India. These studies have highlighted that vegetarianism, micronutrient deficiencies, and low intake of iron folate and vitamin B12 are significantly associated with severe anaemia (Ghosal et al., Reference Ghosal, Bal, Ranjit, Das, Behera, Satpathy, Dutta and Pati2023; Thomas et al., Reference Thomas, Chandra, Sharma, Jain and Pemde2015; Swaminathan et al., Reference Swaminathan, Ghosh, Varghese, Sachdev, Kurpad and Thomas2019). The commonly referred risk factors for anaemia in literature include age, marital status, educational attainment, place of residence, family income, poverty, access to healthcare services, and substandard sanitation conditions (Goswmai & Das, Reference Goswmai and Das2015; Ghosh, Reference Ghosh2009; Bharati et al., Reference Bharati, Shome, Chakrabarty, Bharati and Pal2009; Bharati et al., Reference Bharati, Pal and Bharati2020). Several studies have also identified factors such as access to drinking water, intake of animal-based protein, gender dynamics, societal norms, and preferences regarding contraception methods as key determinants influencing anaemia prevalence in India (Mog et al., Reference Mog, Neogi, Bharadwz, Panda and Sil2023; Nguyen et al., Reference Nguyen, Scott, Avula, Tran and Menon2018; Sedlander et al., Reference Sedlander, Talegawkar, Ganjoo, Ladwa, DiPietro, Aluc and Rimal2021).
According to the latest National Family and Health Survey (NFHS-5) (2019–2021), anaemia has affected 67.1% of children (06–59 months), 57.0% of all women (15–49 years), 52.2% of pregnant women (15–49 years), and 25.0% men (15–49 years) in India. In addition, the NFHS-5 (2019–21) indicates a significant rise in the prevalence of anaemia in all the categories compared to the previous round of the survey (NFHS-4) conducted in 2015–2016 (NFHS, 2019–2021). However, anaemia has been studied predominantly among women of reproductive age groups and children (Sidhu et al., Reference Sidhu, Kumari and Uppal2002; Arlappa et al., Reference Arlappa, Balakrishna, Laxmaiah and Brahmam2010; Kotecha, Reference Kotecha2011; Ghosh, Reference Ghosh2023; Ghosh, Reference Ghosh2023b, Ghosh et al., Reference Ghosh, Hossain and Sarkar2023; Nguyen et al., Reference Nguyen, Scott, Avula, Tran and Menon2018; Bharati et al., Reference Bharati, Pal and Bharati2020). There are also a few studies on the prevalence of anaemia exclusively in men (Didzun et al., Reference Didzun, De Neve, Awasthi, Dubey, Theilmann, Bärnighausen, Vollmer and Geldsetzer2019; Kumar et al., Reference Kumar, Sharma and Sinha2021; Singh et al., Reference Singh, Ram, Singh and Tripathi2022). In addition, most of these studies have understood and considered women or children as homogeneous groups.
There are several studies which have explored anaemia from a specific analytical framework that considers caste, ethnicity, or gender as individual factors. These single-axis frameworks are based on the premise that gender, economic class, ethnicity, and caste can be distinguished from one another and are mutually exclusive (Mukhopadhyay, Reference Mukhopadhyay2015). These studies have delved into the understanding of anaemia by examining these factors separately and independently. Similarly, a number of studies have analyzed the association between anaemia and caste (Vart et al., Reference Vart, Jaglan and Shafique2015; Sidhu et al., Reference Sidhu, Kumari and Uppal2002; Sudhagandhi et al., Reference Sudhagandhi, Sundaresan, William and Prema2011), anaemia and ethnicity (De et al., Reference De, Halder, Chakraborty, Das, Paul, De, Banerjee, Chatterjee and De2011; Rohisha et al., Reference Rohisha, Jose and Chakrabarty2019), and anaemia and gender (Sedlander et al., Reference Sedlander, Talegawkar, Ganjoo, Ladwa, DiPietro, Aluc and Rimal2021; Alvarez-Uria et al., Reference Alvarez-Uria, Naik, Midde, Yalla and Pakam2014) independently. However, anaemia does not affect every person in the strata of society in the same way. It is argued that anaemia indicates poor nutrition and health, which varies with socioeconomic factors, such as gender norms, race, income, and living conditions (WHO, 2014; WHO, 2017). It is difficult to draw a clear distinction or understand societal inequality exclusively based on caste, class, or gender as these identities often intersect and collectively contribute to the produce inequality (Iyer et al., Reference Iyer, Sen and Östlin2008). Therefore, it is important to note that social identities such as gender, class, ethnicity, and caste are interconnected and cannot be separated or regarded as mutually exclusive categories (Nair & Vollhardt, Reference Nair and Vollhardt2020).
Despite extensive research on anaemia in India, there is a notable gap in studies that adopt an intersectional theoretical framework to understand the complex interplay of class, caste, and gender in shaping anaemia prevalence. The existing studies adopt a single-axis framework focusing on caste, class, or gender to analyse social inequality and thus fail to provide an accurate and comprehensive understanding of the overall situation. Thus, there is a dearth of scientific studies based on large-scale data on anaemia from an intersectional theoretical framework in India.
The objective of this study is to fill the research gap by examining the intersections of class, caste, and gender to provide a theoretical understanding of anaemia prevalence and its determinants in the Indian context. The study attempts to understand how socio-economic factors such as class, caste, and gender intersect to influence anaemia prevalence. Moreover, by utilising the latest NFHS-5 (2019–21) data, this study seeks to identify the associations between anaemia prevalence and various demographic and socio-economic factors, including religion, geographical region, education, and household characteristics. Ultimately, this study contributes to the literature by offering insights into the complex social dynamics underlying anaemia in India and informing comprehensive interventions to address this alarming public health challenge.
Inequity in health and intersectionality
The achievement in health equity, which provides a clear intuition to understand the level of social justice, is the best sign of the well-being of a society (Sen, Reference Sen2002; Subramanian et al., Reference Subramanian, Ackerson, Subramanyam and Sivaramakrishnan2008). However, the growing evidence of health inequities from different corners of the world suggests the failure of ensuring health for all (Mishra, Reference Mishra, Nambiar and Muralidharan2017). It is well-documented that the inequities in different socio-economic indicators and health outcomes have widened over the decades across different population groups in India since the 1990s with the introduction of neoliberal economic policies (Uddin et al., Reference Uddin, Acharya, Valles, Baker and Keith2020; Borooah, Reference Borooah, Thorat and Newman2010). The intersection of different social gradients shapes an individual’s life experiences and determines an individual’s quality of life. This intersection also positions the privileges and oppressions that people have to live with in the society. Health disparity arises from such social inequalities and social arrangements in lived experiences of individuals (Weber, Reference Weber2010). Indian society is highly stratified based on social identities such as caste, class, gender, ethnicity, and religion (Khamis et al., Reference Khamis, Prakash and Siddique2012; Patnaik & Jha, Reference Patnaik and Jha2020). These social identities are the determining factors of exclusion and discrimination and result in inequity in access to healthcare, limited utilization of health services, and poor health outcomes in India (Borooah, Reference Borooah, Thorat and Newman2010; Baru et al., Reference Baru, Acharya, Acharya, Kumar and Nagaraj2010; Shaikh et al., Reference Shaikh, Miraldo and Renner2018; Das et al., Reference Das, Hossain and Roy2022).
Kimberlé Crenshaw, a feminist scholar, introduced the theory of intersectionality, which aims to understand, address, and represent the complexities present due to the interplay of different kinds of social dimensions and retrospective economic and social inequalities (Crenshaw, Reference Crenshaw1989). The analytical framework of intersectionality has become the principal way of conceptualizing the relation between systems of oppression which construct multiple identities and social locations in hierarchies of power and privilege (Carastathis, Reference Carastathis2014). In other words, it aims to understand how a person’s social and political identities combine to create multiple forms of discrimination and privileges (Cole, Reference Cole2009; Purdie-Vaughns & Eibach, Reference Purdie-Vaughns and Eibach2008). The emerging theoretical framework of intersectionality provides a critical analytic lens to examine the racial, ethnic, class, and gender disparities and challenges existing ways of understanding these structures of inequality (Dill & Zambrana, Reference Dill, Zambrana, McCann, Kim and Ergun2020; Kapilashrami et al., Reference Kapilashrami, Hill and Meer2015). During the initial years, the scholarship on intersectionality was largely predominated by feminist literature. Eventually, intersectionality theory was broadened to be applied to different studies to understand the complexity of social and economic dimensions beyond the feminist perspective.
The concept of intersectionality is often criticised for its Western origin and does not reflect the complexity of the Indian experience. The debates on the concept of intersectionality are that it must not deduce a group or posit a person to a ‘stable’ or ‘homogenous category’; rather, it shall be able to analyse different levels of social divisions and identities (Menon, Reference Menon2015). Therefore, intersectionality requires the ability to include any group of people beyond the traditional framework (Yuval-Davis, Reference Yuval-Davis2006). However, intersectionality can be critically examined and applied in many different ways as long as it provides insights into our challenges and dilemmas and creates solidarity across the subjects often lost between agendas and movements (John, Reference John2015).
The theoretical framework of intersectionalityFootnote 1 provides an analytical approach to understanding and looking into the complex ways in which social identities determine the access and utilisation of health services and the health outcomes within the stratified society. The intersectionality framework is important for understanding health inequities in India, considering the complex interaction of social identities such as caste, gender, religion, class, and ethnicity, which shape individuals’ access to healthcare and experiences (Kapilashrami et al., Reference Kapilashrami, Hill and Meer2015; Roy et al., Reference Roy, Bhatta and Burnette2020). For instance, Dalit women in rural areas may face discrimination due to their caste, gender, and socio-economic status, leading to limited healthcare access and poorer outcomes. Similarly, tribal communities encounter unique health challenges due to isolation and historical marginalisation. By adopting an intersectional approach, Indian policymakers can craft inclusive policy interventions that cater to the needs of marginalised groups, thereby fostering more effective and equitable health policies that acknowledge the diversity within the country. Thus, the application of the analytical framework of intersectionality in health equity and inequality research becomes critical (Harari & Lee, Reference Harari and Lee2021).
Mahapatro et al. (Reference Mahapatro, James and Mishra2021) found that poorer women face more unmet healthcare needs compared to wealthier women, based on class, caste, and gender dynamics from the National Sample Survey (2017–2018). Conversely, men from lower and middle classes exhibit higher unmet healthcare needs than women in the same economic class. The study on the interplay of gender and class in determining access to healthcare for long-term ailments evinced that there is a differential outcome in accessing healthcare for long-term ailments among different social groups, genders, and economic classes (Sen et al., Reference Sen, Iyer and Mukherjee2009). The studies on child health and nutrition based on the concept of intersectionality show that children belonging to the poorest, Scheduled Tribes (ST), Scheduled Castes (SC), and girls (class, caste, and gender) have worse stunting outcomes than group belonging to non-poor, non-SC/ST, and boys (Mukhopadhyay, Reference Mukhopadhyay2015).
However, the literature on health inequity, especially on the prevalence of anaemia, is predominated by studies based on a single-axis analytical framework of social power. Nevertheless, multiple social identities and associated power relations do not act separately but often operate simultaneously and produce complex interactions (Iyer et al., Reference Iyer, Sen and Östlin2008). The complex interrelationships between caste, class, and gender determine the utilization and access to public goods and services for certain social groups differently than others in India (Patnaik & Jha, Reference Patnaik and Jha2020). Therefore, intersectionality can be a useful tool to examine different dimensions of social inequality and hence a practical approach to addressing health disparities that the traditional single-axis analytical framework lacked (Sen et al., Reference Sen, Iyer and Mukherjee2009; Para-Medina & Weber, Reference Para-Medina, Weber, Texler Segal, Demos and Kronenfeld2003). This study attempts to understand the anaemia status in India through an intersectionality approach in the framework of health inequity.
Materials and methods
Data and ethical statement
This study is based on the recent NFHS-5 conducted in 2019–2021, which is a large-scale, multi-round, cross-sectional, and household-level data on population, health, and nutrition collected from all over the country. The survey is conducted by the International Institute for Population Sciences in Mumbai, under the guidance of the Ministry of Health and Family Welfare, Government of India (IIPS and ICF International Inc., 2021). The fieldwork was done in two phases (17 June 2019 to 30 January 2020 and 2 January 2020 to 30 April 2021) in all the states and union territories in India as it was done in the midst of COVID-19 pandemic. The NFHS-5 collected data from 636,699 households, 724,115 women, and 101,879 men. The NFHS-5 was developed to be representative of each of India’s over 707 districts for key indicators, including anaemia. The survey was carried out utilising a two-stage sampling technique. The household response rate was 98%, while the individual response rate for males was 92%, and for women, it was 97%. The detailed methodology for the survey design can be found in the NFHS-5 national report (IIPS and ICF International Inc., 2021). The NFHS-5 received approval from the Institutional Ethical Review Board (IERB) at IIPS, Mumbai, India, as well as the ICF International Review Board. The survey ensured that participants provided written consent before being interviewed and confidentiality was strictly upheld ensuring the anonymity of survey respondents (IIPS and ICF International Inc., 2021). The data of the NFHS-5 is publicly accessible to registered users and it is the Indian version of the Demographic and Health Surveys (DHS) Program.
Sample size
The anaemia status of both the sex in the reproductive age range is the primary focus of the research; the NFHS-5 collects data from women aged 15–49 and men aged 15–54. However, male samples older than 49 were eliminated to harmonise the dataset and simplify the analysis process. Then, observations missing information about the anaemia status of the respondents were discarded. Thus, a total sample size of 788,458 individuals (699,966 female and 88,522 male) was compiled for statistical analysis.
Outcome variables
This current study uses data on anaemia collected by the NFHS-5 (2019–21). The anaemic status of respondents has been generated as a binary variable, categorised as non-anaemic (coded as 0) and anaemic (coded as 1) for the analysis. The health investigators of the NFHS collected capillary blood Footnote 2 samples from a finger prick in order to measure the concentration of Hb. The surveyors collected blood samples from women aged 15–49 years and men aged 15–54 years who were eligible and provided their consent to take the test. The Hb measurement in NFHS-5 was conducted using the HemoCue system, which includes a portable, battery-operated photometer (Hb201+), along with disposable cuvettes treated to collect blood (NFHS, 2019). The HemoCue system utilises the cyanmethemoglobin method, which is a reliable and widely used quantitative method recommended by WHO (2001). The respondents with a Hb level less than 11.0 g/dl for non-pregnant women, 12.0 g/dl for pregnant women, and 13.0 g/dl for males were recorded as anaemic. The Hb levels were adjusted according to the respondent’s smoking habits and the enumeration areas with an altitude above 1,000 metres.
Explanatory variables
The primary focus of this study is to examine the intersection of gender, caste, and class as a predictor of anaemia among the reproductive population (between 15 and 49 years of age) in India. Therefore, the primary independent variables for this research are gender, caste, and class, which were further categorised into different categories (Table 1). The respondents were categorised according to their gender identity (male and female), caste or social group (SC, ST, and Others comprising General and Other Backward Classes), and class or economic status (poorest, poorer, middle, richer, and richest as per their position in the wealth quintile from lowest to highest). It is worth mentioning that the wealth quintile was constructed based on the household’s availability of various consumer products (such as vehicles, bicycles, radio, and television) and dwelling features (drinking water, sanitation facilities, and housing materials). The respondents were given a score based on principal component analysis, which was then divided into five quintiles, each representing 20% of the respondents and ranging from low (value 1) to high wealth (value 5).
Table 1. Description of the explanatory variables
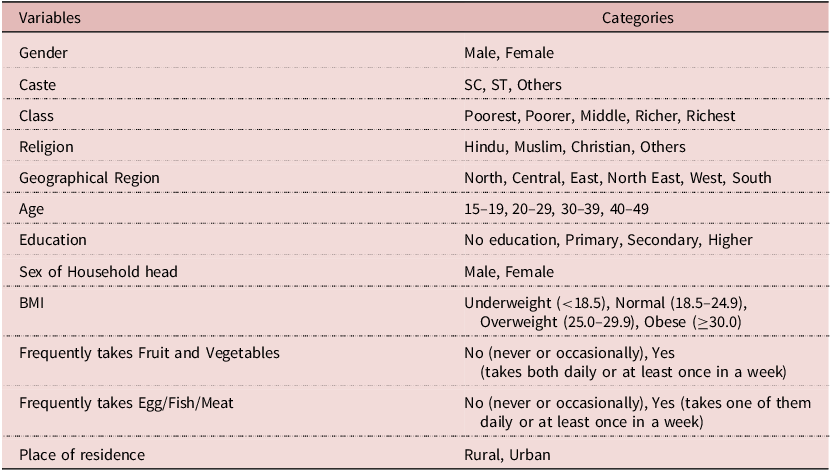
Source: Tabulated from NFHS-5 data.
Covariates
The other covariates used in this study have been selected after reviewing the research papers based on the different versions of NFHS data (Mukhopadhyay, Reference Mukhopadhyay2015; Vart et al., Reference Vart, Jaglan and Shafique2015; Srinivasan et al., Reference Srinivasan and Mohanty2004; Sharif et al., Reference Sharif, Das and Alum2023; Ghosh, Reference Ghosh2023). The covariates selected for the present study include the respondents’ age, educational level, Body Mass Index (BMI), sex of the household head, intake of fruits and vegetables, intake of eggs, fish, and meat, and place of residence (Table 1).
Statistical approach
This study uses bivariate cross-tabulations to show the anaemic status by social dimensions such as gender, class, and caste. Additionally, bivariate crosstabulation has been employed after applying specific conditions to focus on particular sub-dimensions, examining the intersectionality of gender, class, and caste. For example, bivariate tabulation was performed using the variables ‘anaemic status’ and ‘gender’ to analyse the anaemic status of males in the poorest class who belong to the SC community. While performing the tabulation, an ‘if’ condition was applied to extract data from the sub-sample of the poorest and SC population. During the analysis, appropriate sample weights were used separately for the male and female populations, as NFHS-5 provides different sample weights for each. A binary logistic regression model was also utilised since the nature of the dependent variable of the study is dichotomous, as stated in the outcome variable section above. This model assessed how the selected social dimensions (gender, class, and caste) are associated with anaemic status. The place of residence (rural or urban) was included as a covariate in the model and showed significant contributions. Further, the interaction of the place of residence with the selected social dimensions was explored. Four different models were performed in the study. Model 1 illustrated the association of the selected social dimensions (gender, class, and caste) with anaemic status while controlling for other covariates, including place of residence. In model 2, the place of residence was introduced as an intersecting variable. Thus, the intersection of residence with gender was shown in model 2A, caste in model 2B, and class in model 2C. All analyses were performed using Stata version 14.1 (StataCorp., 2015).
Whereas,
p is the likelihood of anaemia; x
1
, x
2
, x
3
, …x
i
refers to the independent variables; β
0
, β
1
, β
2
, β
3
…β
i
refer to the coefficients, or effects of the independent variables in the prevalence of anaemia; and
![]() $\varepsilon $
is the error term.
$\varepsilon $
is the error term.
A multicollinearity assessment was performed for the regression model to ensure the independence of the predictor variables. The variance inflation factor value of 1.20 indicates that the variance of the coefficients is only minimally inflated, indicating low multicollinearity. Furthermore, the condition number of 36.21 is relatively low, suggesting that the design matrix is reasonably well-conditioned. Therefore, the results indicate that the logistic regression model is robust in terms of multicollinearity and numerical stability, and the independent variables used in the analysis are relatively independent, allowing for more reliable estimates of the regression coefficients.
Results
This paper categorised the population into different social stratifications according to class, caste, and gender identities to examine the prevalence of anaemia in India. Table 2 shows that the highest percentage of anaemia is found among the poorest class (58.99%) in India, followed by the poorer class (53.92%), middle class (51.82%), then the richer class (49.85%), and the richest class (47.39%), respectively. The result indicates that economically poor households are more likely to suffer from anaemia than those with better economic states. It has been found that the female population suffers more from anaemia (57.09%) than the male (25.47%). Table 2 records highest prevalence of anaemia among STs (61%) population, followed by SC (55.28%) and Other population groups (51.76%) in India. Table 2 also represents prevalence of anaemia at the household level across the intersections of class, caste, and gender. It has been found that the occurrence of anaemia is higher in case of women across the three social dimensions of class, caste, and gender. Interestingly, there is a presence of an indirect proportionality between the prevalence of anaemia and the hierarchy of social position. In other words, the higher the social and economic order, the lesser the prevalence of anaemia in society and vice versa. Table 2 shows that within the poorest class, women in ST communities have the highest percentage of anaemia (69.29%), followed by SC communities (63.45%), and then the women of Other communities (61.41%). The anaemic trend remains consistent even with males within the poorest class across three caste groups. The highest prevalence of anaemia is found among ST males (39.78%), followed by the males of SC communities (35.26%), and then males in Other communities (35.21%). The prevalence of anaemia among males and females decreases with higher order in the caste and class hierarchy. The percentage of anaemic females in ST decreases consistently from the poorest class (69.29%), the lowest in the economic hierarchy, to the richest class (49.95%), and the highest in the economic hierarchy. A similar trend of decrease in the percentage of anaemic from the lower economic class to the upper economic class has been observed among males and females across the different caste groups. The prevalence of anaemia among the ST men also decreased from the poorest (39.78%) to the richest class (28.02%). Similarly, the percentage of females in the SC being anaemic decreased from the poorest class (63.45%) to the richest class (55.60%). The prevalence of anaemia among the SC men decreased from the poorest class (35.26%) to the richest class (19.57%). In the same way, the percentage of females in the Other communities being anaemic decreased from the poorest class (61.41%) to the richest class (50.16%). However, there is a contradiction of this decreasing trend of prevalence of anaemia based on caste hierarchy in the case of the richest class and females. The prevalence of anaemia among women within the richest class is the highest in SC communities (55.60%) than in the Other communities (50.16%), followed by STs (49.95%). However, this contradiction is not in the case of males in the richest class across the three castes. In Table 2, the ratio of anaemic females to anaemic males for different castes and classes has been calculated. Table 2 shows that ST women in the poorest class (69.23%) have the highest prevalence of anaemia, followed by ST women in the poorer class (64.77%), SC women in the poorest class (63.45%), ST women in the middle class (60.99%), and SC women in poorer class (59.83%). In other words, the ST and SC women in the lower economic classes are more likely to suffer from anaemia than the women in wealthier categories and men across the different class and caste groups.
Table 2. Anaemic status (%) in India by caste, class, and gender
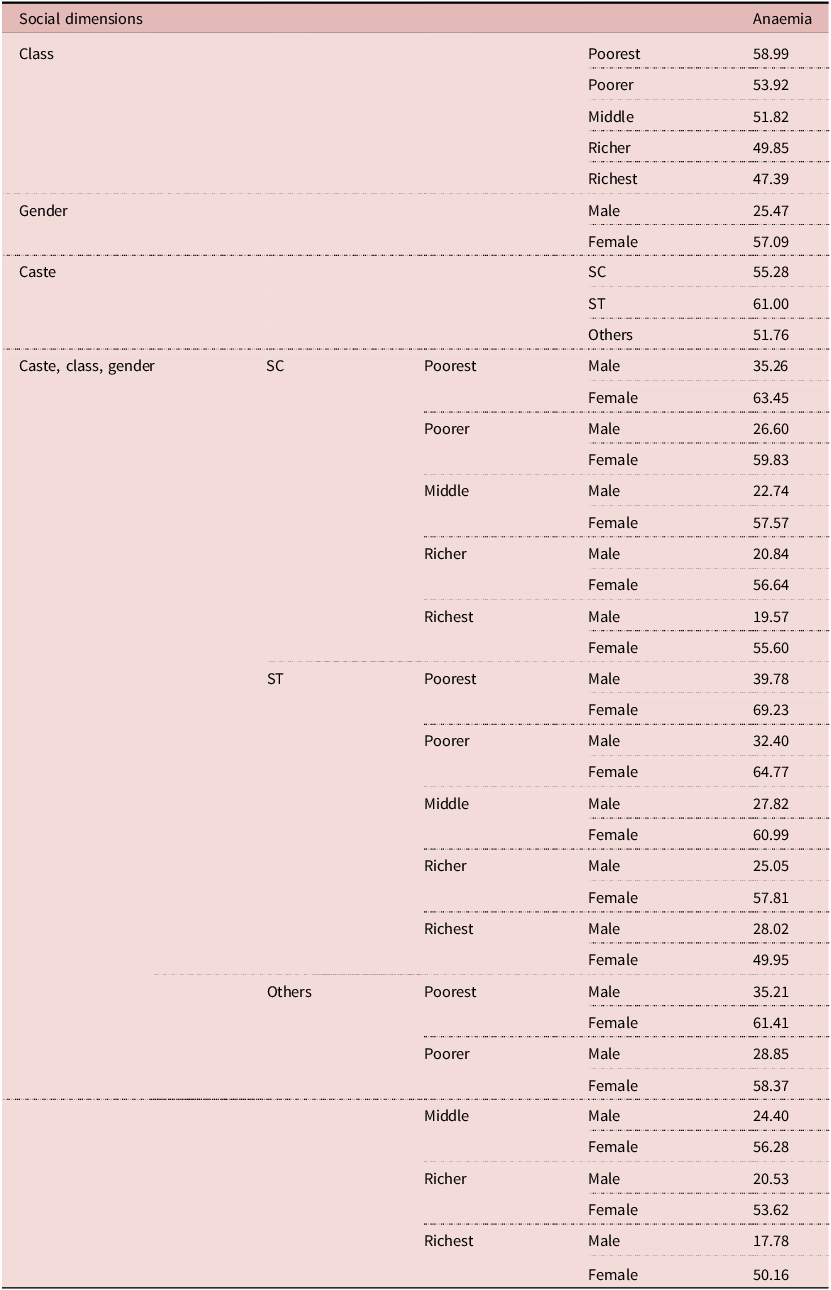
Source: Calculated from NFHS-5 data.
In Table 3, model 1 analyses who will likely have anaemia among different social dimensions. In model 2, the place of residence was introduced due to the significant variation in the functionality of socio-economic parameters such as gender, class, and caste, depending on whether a person resides in a rural or urban environment. Model 1 shows that females have significantly higher prevalence of anaemia than males in India. It has been found that anaemia rates drop significantly in female-headed households (OR: 0.98; CI: 0.965–0.990). The prevalence of anaemia is found across people of different economic classes and caste groups. However, it was observed that the likelihood of being anaemic is inversely related to income. The poorest category is the most vulnerable, with being more anaemic. On the other hand, along the caste categories, the respondents from the ST category are more likely to be anaemic than all castes. In Model 1, the prevalence of anaemia among different religions is observed. In India, there is a substantial prevalence of anaemia among Muslims (OR: 1.04; CI: 1.026–1.057) compared to the other religious communities. It has been found that Muslims are more likely to be anaemic, followed by Hindus, Others (OR: 0.90; CI: 0.882–0.923), and Christians (OR: 0.54; CI: 0.528–0.552), respectively.
Table 3. Odds ratio of being anaemic in India: Intersection of place of residence with gender, caste, and class
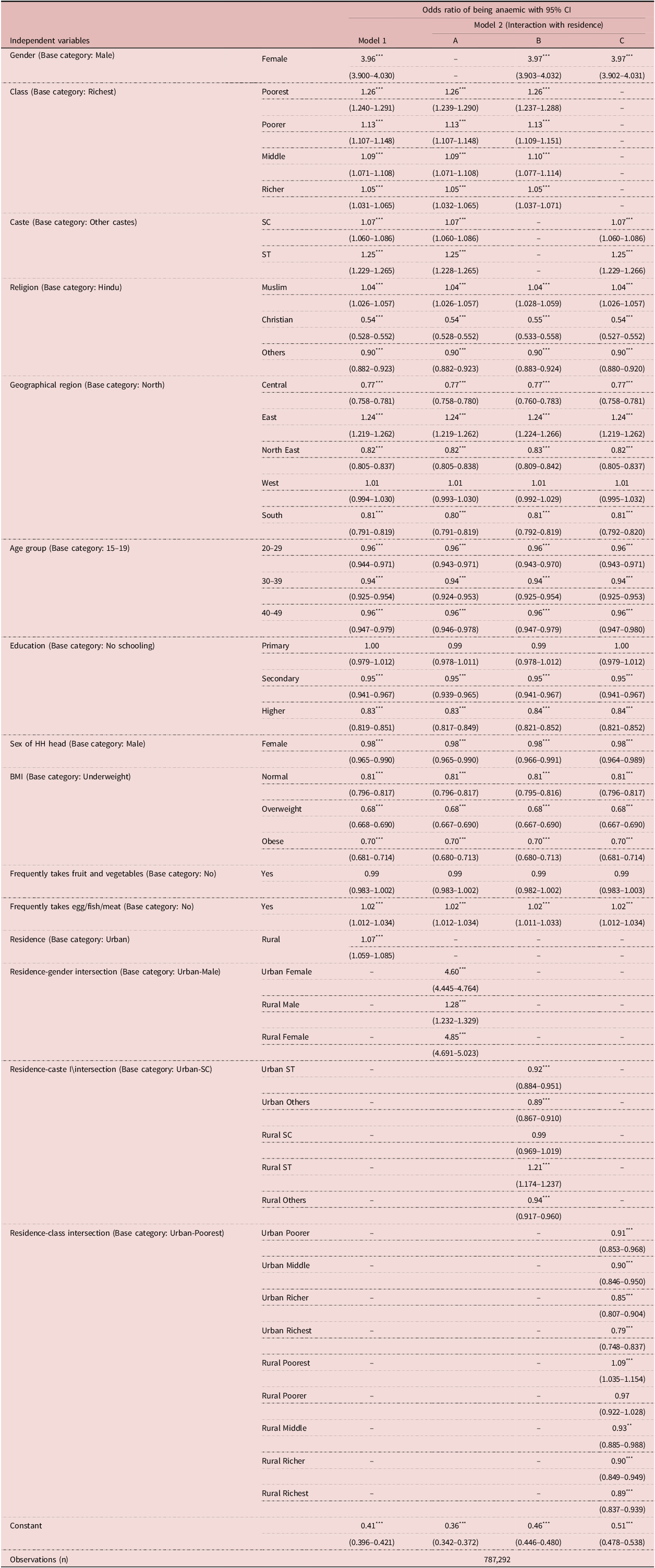
Model 1 includes place of residence as a covariate and finds it to be significant; Model 2 considers the intersection of residence with gender (Model 2A), caste (Model 2B), and class (Model 2C)
Source: Calculated from NFHS-5 data.
*P < 0.1.
**P < 0.05.
***P < 0.01.
Model 1 shows an interesting trend in the prevalence of anaemia across five different geographic regions (Central, East, Northeast, West, and South) in India. It has been found that the prevalence of anaemia is significantly lower in the Central region (OR: 0.77; CI: 0.758–0.781), followed by the Northeast (OR: 0.82; CI: 0.805–0.837) and South regions (OR: 0.81; CI: 0.791–0.819). The Eastern region (OR: 1.24; CI: 1.219–1.262), the Western region (OR: 1.01; CI: 0.994–1.030), and Northern region, respectively, have a significant prevalence of anaemia in India. Model 1 does not record a clear trend of the likelihood of being anaemic in different age groups. However, 30–39 years old respondents are better off than other age groups. The variance between the likelihood of being anaemic is minimal in these categories. Nevertheless, respondents with a higher level of education show a lower likelihood of being anaemic (OR: 0.83; CI: 0.819–0.851). In the case of the Body Mass Index (BMI), as one progresses across the categories from normal to overweight and then to obese, the likelihood of being anaemic decreases. Interestingly, the respondents with ‘Normal’ BMI (OR: 0.81; CI:0.769–0.817) have a higher chance of being anaemic than ‘Obese’ BMI. (OR: 0.70; CI: 0.681–0.714) The perplexity of anaemia with better BMI (only in the case of Normal BMI) is observed. The respondents who frequently consume fruits and vegetables are less likely to be anaemic than their counterparts. Model 1 shows that the respondents living in rural areas have 7% more chances of being anaemic than the urban residents.
In Model 2A, further decomposition by intersecting residence and gender reveals that the likelihood of females being anaemic is very high in both urban (OR: 4.60; CI: 4.445–4.764) and rural areas (OR: 4.85; CI: 4.691–5.023) compared to males. However, the probability of being anaemic for rural males (OR: 1.28; CI: 1.232–1.329) is also high compared to urban males but nominal to females in both areas. This shows the vulnerable state of females in terms of health (anaemia) irrespective of place of residence. Model 2B analyses the intersection of caste and place of residence with anaemia. It has been found that the Urban Others (OR: 0.89; CI: 0.867–0.910) respondents are less likely to be anaemic, followed by Urban ST (OR: 0.92; CI: 0.884–0.951), Rural Others (OR; 0.94: CI: 0.917–0.960), Rural SC (OR:0.99; CI: 0.969–1.019), and Rural ST (OR: 1.21; CI: 0.969–1.019) among all the castes-residence groups. The results reflect that Urban Others are better off than their counterparts in the rural area and also across other residence-social categories. Compared to the Urban SC category, Urban Others (OR: 0.89; CI: 0.867–0.910) and Urban ST (OR: 0.92; CI: 0.884–0.951) areas are less likely to be anaemic. How does wealth or economic status determine health? In other words, if it is assumed that the one with higher income shall have better health and lesser anaemic, then this holds true for model 2C. The intersection of place of residence with various economic groups is examined in model 2C in Table 3, which shows that the probability of anaemia decreases with better economic status in both urban and rural areas. It has been found that among all residence-economic groups, the urban richest (OR: 0.79; CI: 0.748–0.837) is better off than all other categories in urban areas. Similarly, rural richest (OR: 0.89; CI: 0.837–0.939) is better off across all categories in rural areas. Therefore, the rural poorest (OR: 1.09; CI: 1.035–1.154) category is more likely to be anaemic than any other residence-income group. This displays the combined effect of income and place of residence on the prevalence of anaemia. The results suggest that gender, place of residence, income, and social group among all the variables affect the sampled respondents’ anaemia level significantly.
Discussion
The present study has delineated the prevalence of anaemia among people belonging to different classes, social strata, caste affiliations, and genders within India. Utilising recent NFHS-5 data, the study employed bivariate cross-tabulations and binary logistic regression models to analyse the prevalence of anaemia and its association with socio-economic dimensions, demographic indicators, and geographical location. The present study highlights that women belonging to ST and SC communities, particularly those in lower economic classes, exhibit a higher likelihood of suffering from anaemia compared to other social groups. Therefore, the result of this present study shows an unequal prevalence of anaemia suggesting higher health inequity among the different social groups in India. The STs (also known as Tribals, Indigenous people, and Adivasis) and the SCs (also known as Dalits) are the most socio-economically disadvantaged communities who share a disproportionate burden of anaemia in India. The high prevalence of anaemia among the ST and SC population in India follows the trend of the earlier studies (Arlappa et al., Reference Arlappa, Balakrishna, Laxmaiah and Brahmam2010; Kaur et al., Reference Kaur, Bains and Kaur2018; Ghosh, Reference Ghosh2023). The Muslim population have a higher prevalence of anaemia compared to the Hindus, Christians, and other religious groups. The higher prevalence of anaemia among Muslims has also been found in the previous studies (Sekhar, Reference Sekhar, Sudhir, Bari, Khan and Shaban2021). The health of Muslim communities is affected by poverty, inadequate services like clean water, healthcare, and sanitation. The Sachar Committee Report (2006) reveals limited education, social security access, employment opportunities, visibility, and identity-based discrimination among Muslims, especially Muslim women, leading to poor health outcomes (Parveen, Reference Parveen2014). On the other hand, class and gender have remained significant determinants of the prevalence of anaemia in India. The present study confirms that economically poor households are more likely to suffer from anaemia than those with better economic states and people with a higher level of education are comparatively less prone to anaemia (Mog et al., Reference Mog, Neogi, Bharadwz, Panda and Sil2023). Furthermore, building upon prior research (Biradar, Reference Biradar2022; Ghosh, Reference Ghosh2023; Ghosh et al., Reference Ghosh, Hossain and Sarkar2023; Sharif et al., Reference Sharif, Das and Alum2023), the present study identifies class, caste, gender, religion, education, female-headed household, and BMI as significant determinants of anaemia prevalence in India. The present study also identifies geographical location and place of residence as determinants of anaemia in India, indicating that the rural poor women are particularly susceptible. The percentage share of the female population in the total anaemic patients remained significantly higher than the male population. Interestingly, female-headed households have less prevalence of anaemia than male-headed households. This result is similar to the previous study’s findings, which show that female-headed households are associated with better nutritional and health outcomes than male-headed households in India (Gaiha & Kulkarni, Reference Gaiha and Kulkarni2005). It is argued that women in the female-headed households are more empowered with a greater voice in financial decision-making at the household level (Abbas et al., Reference Abbas, Isaac, Zia, Zakar and Fischer2021; Ghosh & Vinod, Reference Ghosh and Vinod2017). Female-headed households experience higher decision-making autonomy and stronger social support networks, potentially reducing anaemia prevalence through improved nutrition, healthcare access, and other factors such as education, labour force participation, and healthcare utilisation (Annan et al., Reference Annan, Donald, Goldstein, Martinez and Koolwal2021; Vijay & Patel, Reference Vijay and Patel2021). Furthermore, women’s autonomy in matters of fertility decisions is correlated with better health outcomes, while early marriages often result in adverse effects such as frequent pregnancies and low birth weights ultimately leading to ill health among women (Gaiha & Kulkarni, Reference Gaiha and Kulkarni2005).
The result of the present study shows that women are more anaemic than men is consistent with other studies on anaemia carried out in India and different parts of the world (Didzun et al., Reference Didzun, De Neve, Awasthi, Dubey, Theilmann, Bärnighausen, Vollmer and Geldsetzer2019; Kumar et al., Reference Kumar, Sharma and Sinha2021). However, there exists a problematic inclination towards generalizing all women as a unified and homogeneous group, disregarding the diverse inequalities in health status and social realities experienced by women of different races, classes, sexual preferences, and geopolitical backgrounds, thereby necessitating the rejection of the notion of ‘universal sisterhood’ (Doyal, Reference Doyal1995). In this regard, the theory of intersectionality is important to understand the ways in which different intersections of socio-economic and geographical identity combine together and determine health and illness among women in different stratas of the society. Indian society is marked by significant stratification based on caste, class, gender, ethnicity, and religion (Khamis et al., Reference Khamis, Prakash and Siddique2012; Patnaik & Jha, Reference Patnaik and Jha2020). These intersecting social identities shape individuals’ experiences and quality of life, determining privileges and oppressions (Weber, Reference Weber2010). Social inequalities result in exclusion, discrimination, and inequitable access to healthcare, limiting utilization of services and contributing to poor health outcomes in India (Borooah, Reference Borooah, Thorat and Newman2010; Das et al., Reference Das, Hossain and Roy2022). Therefore, women’s marginalized position and subordination must be understood and linked with the caste and ethnicity question within the feminist discourse in India (Guru, Reference Guru1995; Chakravarti, Reference Chakravarti2018). Therefore, the present study analysed the intersections of caste, class, and gender to understand the prevalence of anaemia in the Indian context. The results indicate that SC and ST women, especially those in the lowest economic strata, are more vulnerable and likely to have the highest anaemia prevalence rate compared to their counterparts.
There is a broad consensus that anaemia serves as a significant indicator of inadequate nutrition and overall poor health. Additionally, anaemia is closely connected to the five global nutrition targets, namely stunting, low birth weight, childhood overweight, exclusive breastfeeding, and wasting (WHO, 2014). A broad spectrum of socioeconomic factors, such as discrimination based on gender norms or race, lack of sufficient income, low education level, poor living conditions, and inadequate access to water, sanitation, and hygiene, significantly contribute to the prevalence of anaemia (WHO, 2017). Therefore, the underprivileged population groups with a lower level of education, limited access to healthcare services, and inadequate dietary diversity are more prone to being anaemic (Yadav et al., Reference Yadav, Ghimire, Amatya and Lamichhane2021).
It has been found in the present study that the socially disadvantaged groups (ST and SC) who live in rural areas are more like to be anaemic than others. Studies have observed that women in the reproductive age groups from the STs and SC communities who are poor and live in rural areas have a higher prevalence of anaemia (Biradar, Reference Biradar2022). This trend has been consistent through nationally representative data NFHS-2 (1998–1999), NFHS-3 (2005–2006) (Balarajan et al., Reference Balarajan, Fawzi and Subramanian2013), and NFHS-5 (2019–2021) (Sharif et al., Reference Sharif, Das and Alum2023). Studies have observed a similar pattern that the under-five aged children of STs communities are found to have the highest prevalence of anaemia than other children in NFHS-3 (2005–2006) (Vart et al., Reference Vart, Jaglan and Shafique2015). This trend of a high prevalence of anaemia among ST children remained unchanged for the next ten years as observed from NFHS-4 (2015–2016) (Ghosh, Reference Ghosh2023). Therefore, the finding of the present study confirms previous research indicating a greater prevalence of malnutrition, morbidity, and anaemia among indigenous populations and socio-economically disadvantaged groups in India, attributed to factors such as poverty, restricted access to food and healthcare, poor nutritional and health status, limited educational opportunities, and reduced healthcare utilisation among mothers (Ghosh, Reference Ghosh2023; Maity, Reference Maity2017; Maharatna, Reference Maharatna2011; Ghosh et al., Reference Ghosh, Hossain and Sarkar2023). These conditions lead to a higher prevalence of anaemia among women from socio-economically disadvantaged ST and SC communities in India.
In India, anaemia is highly associated with caste identity (Kaur et al., Reference Kaur, Bains and Kaur2018), even after accounting for demographic factors, including adult education and household wealth (Vart et al., Reference Vart, Jaglan and Shafique2015). In addition, the socioeconomic inequities manifested in caste, class, and gender differentials determine the availability, utilization, and affordability of health services in India (Baru et al., Reference Baru, Acharya, Acharya, Kumar and Nagaraj2010). Consequently, there are significant differences among different population groups in health status determined by caste, class, and regional inequalities (Jungari & Chauhan, Reference Jungari and Chauhan2017).
The SCs and STs constitute most socio-economically marginalised populations, facing exclusion, widespread poverty, landlessness, precarious employment, and discrimination at multiple levels for being at the bottom of the social stratification of Indian society (Das et al., Reference Das, Hossain and Roy2022; Baru et al., Reference Baru, Acharya, Acharya, Kumar and Nagaraj2010; Patel et al., Reference Patel, Das and Das2018). This exclusionary process revolves around social relationships and institutions, perpetuating the marginalisation, isolation, and deprivation of certain communities in terms of political participation, civil rights, and socio-cultural and economic opportunities (Thorat, Reference Thorat2002; Throat, Reference Thorat2013). In India, a significant portion of the SC and STs population resides in rural areas and works as landless agricultural labourers (Baru et al., Reference Baru, Acharya, Acharya, Kumar and Nagaraj2010). These communities often face poverty, as they fall below the poverty line (Patnaik & Jha, Reference Patnaik and Jha2020). Furthermore, they experience marginalisation in terms of access to basic social and physical amenities within their households (Srinivasan & Mohanty, Reference Srinivasan and Mohanty2004). Consequently, the SC and STs population endure multiple social and economic inequalities compared to other communities in India (Das et al., Reference Das, Hossain and Roy2022). The exclusion resulting from their social identities also leads to social vulnerability, limiting their access to healthcare services and contributing to health disparities and overall poor health outcomes (Borooah, Reference Borooah, Thorat and Newman2010; Fiorati et al., Reference Fiorati, Arcêncio and Souza2016; Patnaik & Jha, Reference Patnaik and Jha2020). The disadvantaged caste groups are exposed to poor living conditions, poor diets, adverse caste-based discrimination, and limited access to health care and food supplements. Therefore, they are more vulnerable to infectious diseases and iron deficiency, significantly increasing anaemia (Vart et al., Reference Vart, Jaglan and Shafique2015). However, it has been found that within these two marginalised groups, the ST population has been suffering from adverse health outcomes in terms of anaemia than the SC communities in India. It has also been confirmed in the study by Maity (Reference Maity2017) that the STs consistently performed poorly in the prevalence of anaemia and utilisation of healthcare services such as the use of modern contraceptives, antenatal and postnatal healthcare, and child immunisation. The STs in India have experienced greater marginalisation due to the lack of political mobilisation and leadership and a slower poverty alleviation rate compared to the SC population (Xaxa, Reference Xaxa2001; Maharatna, Reference Maharatna2011). Therefore, it is clear from the above discussion that intersections of multiple factors such as caste, class, gender, and place of residence significantly determine ‘who is anaemic in India’.
Limitations and strengths of the study
While diligent efforts have been made, the present study acknowledges certain limitations, particularly in relation to methodological issues. Firstly, a debate revolves around whether Hb concentration in capillary blood is better suited for measuring Hb than venous blood. A few studies suggest that Hb levels obtained from capillary samples may be higher than those from venous samples, potentially leading to false-negative outcomes (De la Cruz-Góngora et al., Reference De la Cruz-Góngora, Méndez-Gómez-Humarán, Gaona-Pineda, Shamah-Levy and Dary2022; Garcia-Casal et al., Reference Garcia-Casal, Dary, Jefferds and Pasricha2023). However, the NFHS and other DHS surveys worldwide collect capillary blood samples from a finger prick, considering its convenience, affordability, and user-friendliness. Secondly, the study’s limitations include its reliance on cross-sectional rather than cohort data, limiting the ability to establish causality relationships, and only allowing for identifying associations. Thirdly, given the absence of a fieldwork-based qualitative dataset to supplement this study, there are limitations in comprehensively understanding social dynamics and power relations in everyday lives, cultural practices, and the intricate interplay of various factors influencing the prevalence of anaemia.
Nevertheless, the paper has humbly justified addressing the prevalence of anaemia in India vis-à-vis health inequity. The present study only prioritised the intersection of the three prominent variables – class, caste, and gender – but also prioritised other relevant variables such as age, urban-rural, religion, and food habits in determining the prevalence of anaemia. Such variables are an instrumental part of the diverse culture of India. Therefore, the intersectionality approach with the applicability of all these variables has been adopted in this study. Consequently, the paper deduces the homogeneity of entities at different levels, thus minimising the demerits of intersectionality by addressing the disparity between well-defined groups and within the group. Thus, the paper contributes to the literature on the prevalence of anaemia in India by employing an intersectionality framework alongside quantitative health data.
Conclusion
One of the most critical indications of a nation’s social well-being and justice can be assessed by the state of health (in)equity among the different sections of society. However, the growing evidence suggests that the inequities in health and other socio-economic indicators have been widened across different population groups in India. The present study sheds light on the complex interplay of various factors, such as caste, class, gender, and place of residence, in determining ‘who is anaemic in India’. The study underscores that the high prevalence rate of anaemia among the SC and ST has remained a significant challenge in India. It has been found that economic class, caste and gender identity, and place of residence significantly determine the prevalence of anaemia in India. The existing social and economic inequalities determine the varied prevalence of anaemia across different social groups, genders, regions, and urban and rural dwellers in India. The present study highlights that the SC and ST women who are economically marginalised and live in the rural parts of the country share a disproportionate burden of anaemia. Consequently, comprehending the intersections of various social positions and privileges tied to socio-political identities becomes imperative in analysing the prevalence of diseases such as anaemia, thereby facilitating the formulation of effective policy measures. In India, the current approach of the state to eradicate anaemia focuses primarily on promoting antenatal care and the use of iron and folic acid supplements. However, this one-size-fits-all measure ignores the social context of the disease. It overlooks the importance of implementing a food-based approach to provide local nutritious foods with multiple nutritional benefits. Therefore, a comprehensive understanding of the prevalence and determinants of anaemia from a theoretical intersectionality perspective is crucial for crafting inclusive policy interventions to address the disparities in anaemia prevalence and improve the health outcomes of marginalised communities. This paper undertakes a significant endeavour to identify demographic groups with elevated anaemia prevalence, which is crucial for implementing policy-level interventions given India’s diverse demographics and geography. In addition, it is also important to strengthen the public distribution system and nutrition and supplement programmes at public institutions and household levels. There is a serious need to ensure food security and primary healthcare across class, caste, and gender, along with ensuring proper employment to women from marginalised communities with a focus on inclusive development so that no one is left behind.
Data availability statement
The paper is based on National Family Health Survey data, which is the Indian version of the DHS Program, and is publicly accessible to registered users.
Acknowledgements
The researchers express their sincere gratitude for the insightful comments and valuable suggestions offered by the anonymous reviewers of the Journal of Biosocial Sciences. The suggestions have significantly enhanced the quality of the paper.
Funding statement
This study did not receive any funding from any agency.
Competing interests
There are no known conflicts of interest/competing interests to declare.
Ethical standard
This paper uses the secondary data from the NFHS-5 conducted by the International Institute for Population Sciences in Mumbai, under the guidance of the Ministry of Health and Family Welfare, Government of India. This survey received approval from the IERB at IIPS, Mumbai, India, as well as the ICF International Review Board. The survey ensured that participants provided written consent before being interviewed and confidentiality was strictly upheld ensuring the anonymity of survey respondents (IIPS and ICF International Inc., 2021).





