Introduction
There are 10.35 million people held in penal establishments worldwide (Walmsley, Reference Walmsley2016). Recent large-scale systematic reviews have established that prisoners suffer multiple vulnerabilities including mental disorder, substance misuse and homelessness. Fazel & Seewald (Reference Fazel and Seewald2012), in a systematic review of the international literature, found that mental illness is over-represented in prisoners. They identified a pooled 6-month prevalence of psychosis of 3.6% in male prisoners and 3.9% in female prisoners. The pooled prevalence of major depression was 10.2% in male prisoners and 14.1% in female prisoners. No significant differences in rates of psychosis and depression between remand and sentenced prisoners were identified. The authors further found high levels of heterogeneity in the review, partly explained by higher rates of psychosis in low-middle-income countries. Fazel & Danesh (Reference Fazel and Danesh2002), in an earlier review of 6-month prevalence data from 12 countries, found that 3·7% of men [95% confidence interval (CI) 3.3–4.1] had psychotic illnesses and 10% major depression. Rates in women were 4.0% with psychotic illnesses and 12% major depression. Older prisoners, in addition, may have significantly higher rates of affective disorder, with one study reporting a prevalence of 30% for depressive disorder (Fazel et al. Reference Fazel, Khosla, Doll and Geddes2001). These prison estimates are significantly higher than international population point prevalence estimates for psychotic illness, which have been reported as 4.6/1000 (Saha et al. Reference Saha, Chant, Welham and McGrath2005) and major depressive disorder reported as 4.7% (Ferrari et al. Reference Ferrari, Somerville, Baxter, Norman, Patten, Vos and Whiteford2013).
Suicides are also over-represented in the prison population. A study (Fazel et al. Reference Fazel, Grann, Kling and Hawton2011) reviewing data from 12 countries found that in men, crude relative rates of suicide were at least three times higher than the general population. Western European countries had similar rates of prisoner suicide, which were mostly higher than those in Australia, Canada and New Zealand. In women, inmate suicide rates varied widely and were raised compared with rates in the general population.
Substance and alcohol misuse are associated with the significant economic burden (Rehm et al. Reference Rehm, Taylor and Room2006) and are risk factors for offending (Grann & Fazel, Reference Grann and Fazel2004). Their prevalence in marginalised communities such as homeless populations and prisons is of international concern. A systematic review evaluating substance abuse and dependence (Fazel et al. Reference Fazel, Bains and Doll2006) across 13 prison-based studies, found that estimates of prevalence for alcohol abuse and dependence in male prisoners ranged from 18% to 30% and 10% to 24% in female prisoners. The prevalence estimates of drug abuse and dependence varied from 10% to 48% in male prisoners and 30% to 60% in female prisoners. This review excluded studies citing only lifetime prevalence rates. Compared with US general population estimates (Kessler et al. Reference Kessler, McGonagle, Zhao, Nelson, Hughes, Eshleman, Wittchen and Kendler1994), this review noted that male prisoners have a slight excess of alcohol dependence and a two- to 10-fold excess of drug dependence whilst estimates for female prisoners noted a two to a fourfold excess of alcohol dependence and 13-fold increase in drug dependence.
Incarceration is associated with homelessness, and homelessness can be a cause or consequence of incarceration (McCann, Reference McCann2003). Homelessness is in itself associated with higher levels of mental illness and substance misuse (Fazel et al. Reference Fazel, Hope, O’Donnell and Jacoby2008) with both these vulnerabilities affected by trends towards the closure of long-stay psychiatric hospitals or ‘asylums’ (Paulson, Reference Paulson2012). McNiel et al. (Reference McNiel, Binder and Robinson2005) found that 16% of those incarcerated in the San Francisco penal system were homeless. Greenberg & Rosenheck (Reference Greenberg and Rosenheck2008), in a national study of US inmates, found that 12.4% had been homeless in the previous year, although not at the time of incarceration; and 2.9% were homeless at the time of incarceration. A United States Bureau of Justice Statistics study (Hughes et al. Reference Hughes, Wilson and Beck2001) representing a nationwide survey of state prisoners expecting to be released in 1999, found that 12% reported being homeless at the time of their arrest. Estimates in the United Kingdom for homelessness at the time of committal are 15% (Williams et al. 2012).
The Irish Penal Reform Trust (2017) reported that there were 3674 people in prison custody in Ireland as of December 2016, with a rate of imprisonment of 79 per 100 000 of the population. The Irish prison population increased by 400% from 1970 to 2011. The 14 institutions in the Irish prison system consists of 11 traditional ‘closed’ institutions, two open centres and one ‘semi-open’ facility. Female prisoners are accommodated in two prisons nationally. The Irish Prison service (2015) reported of those sent to prison, 79.4% were male and 20.6% were female. Approximately one-sixth of the total prison population comprised remand prisoners.
Mental disorder, substance misuse (Council of Europe, 2015) and homelessness (McCann, Reference McCann2003) have been highlighted as key areas of need amongst Irish prisoners. Whilst the prevalence of these vulnerabilities are studied by health services, governmental and non-governmental organisations, they have not been systematically reviewed.
Whilst reviews of international literature often report a lifetime prevalence of these vulnerabilities, an analysis of need informing resource management requires estimates of point prevalence – What proportion of prisoners actively suffer from a psychotic, major affective disorder or substance misuse disorder at the time of assessment? What proportion are homeless at the time of committal to prison? This is in contrast to those that have a history of these vulnerabilities, which although relevant to their long-term needs, may be less pertinent when estimating immediate care needs. In this study, we systematically review published studies which estimate the reported point prevalence of major mental illness, alcohol and substance misuse at the time of assessment, and that of homelessness on committal in Irish prisoners.
Aims
To systematically analyse published data pertaining to three questions:
a. What is the reported point prevalence of psychotic illness and major affective disorder in Irish prisoners?
b. What is the reported point prevalence of alcohol or substance misuse disorder in Irish prisoners?
c. What was the reported point prevalence of homelessness on committal in Irish prisoners?
Methods
PRISMA Guidelines (Moher et al. Reference Moher, Liberati, Tetzlaff and Altman2009) were followed in the conduct of this review. A research librarian (ID) conducted searches of PsycINFO, MEDLINE, PubMed, EMBASE and Google Scholar (1 January 1966 to 31 December 2016) for publications citing Irish data (Republic of Ireland) on point prevalence of major mental illness, substance misuse/dependence and homelessness amongst prisoners using the search terms ‘mental*, psych*, prevalence, disorder, prison*, substance*, alcohol, drug*, misuse, dependen*, abuse, home*, nfa, no fixed abode, prison*, inmate, jail, sentenced, remand, detainee’ and also combinations of those.
We additionally searched websites of the Irish Prison Reform Trust, Mental Health Commission, Irish Prison Service and the Council of Europe. We augmented searches by reviewing research repositories including Lenus (a repository specific to the Irish health service), Scopus and reviewing governmental reports.
As overarching general inclusion criteria, studies were required to (1) be drawn from the general prison population, (2) relate to adult (>18 years) males and/or females in an Irish prison, and (3) cite quantitative data with a clear numerator and denominator.
Additional specific inclusion/exclusion criteria included:
1. For the purpose of this study, ‘major mental Illness’ included psychosis (schizophrenia, schizoaffective disorder, delusional disorder, psychotic depression, mania with psychosis, drug-induced psychosis) and affective disorder (major depressive disorder, bipolar affective disorder). Inclusion required the use of standardised diagnostic classification and/or psychiatric assessment. Studies based solely on self-reported symptoms were excluded, as were those drawn from select prison subpopulations (Giblin et al. Reference Giblin, Kelly, Kelly, Kennedy and Mohan2012) and hospitalisation samples (O’Connor & O’Neill Reference O’Connor and O’Neill1990; Linehan et al. Reference Linehan, Duffy, Wright, Curtin, Monks and Kennedy2002). Data on point prevalence were extracted, as opposed to lifetime prevalence. Therefore, samples reporting historical diagnoses based on retrospective chart review (Davoren et al. Reference Davoren, Fitzpatrick, Caddow, Caddow, O’Neill, O’Neill and Kennedy2015) were excluded.
2. Studies on substance misuse and alcohol misuse were included where diagnoses were made using a standardised diagnostic classification and/or psychiatric assessment. For the purpose of this study, ‘misuse’ was defined as harmful use or dependence. Studies based solely on self-reported symptoms or drug testing (Long, Reference Long2008) were excluded, as were those drawn from prison subpopulations such as hospitalisation samples or screened sub samples where the screening tool used did not target substance misuse (McInerney et al. Reference McInerney, Davoren, Flynn, Mullins, Fitzpatrick, Caddow and O’Neill2013; O’Neill et al. Reference O’Neill, Smith, Caddow, Duffy, Hickey, Fitzpatrick, Caddow, Cronin, Joynt, Azvee, Gallagher, Kehoe, Maddock, O’Keefe, Brennan, Davoren, Owens, Mullaney, Keevans, Maher and Kennedy2016). Data on point prevalence were extracted, as opposed to lifetime prevalence (O’Mahony, Reference O’Mahony1997). Therefore, samples reporting historical diagnoses based on retrospective chart review (Davoren et al. Reference Davoren, Fitzpatrick, Caddow, Caddow, O’Neill, O’Neill and Kennedy2015) were excluded.
3. For the purpose of this study, homelessness was defined as included those living ‘homeless and roofless’ and in ‘unsettled accommodation’. Data on homelessness at the time of incarceration were extracted, as opposed to a lifetime history of homelessness. Studies drawn from prison subpopulations such as screened samples where the screening tool used did not assess homelessness (McInerney et al. Reference McInerney, Davoren, Flynn, Mullins, Fitzpatrick, Caddow and O’Neill2013; O’Neill et al. Reference O’Neill, Smith, Caddow, Duffy, Hickey, Fitzpatrick, Caddow, Cronin, Joynt, Azvee, Gallagher, Kehoe, Maddock, O’Keefe, Brennan, Davoren, Owens, Mullaney, Keevans, Maher and Kennedy2016) and hospitalisation samples were excluded.
Data were independently extracted by two researchers (G.G., a Consultant Psychiatrist and N.K., a Senior Registrar in Psychiatry) for each included publication. There was no disagreement in data extracted by the two researchers.
Statistical analysis
For each outcome (psychosis, affective disorder, alcohol use, substance use, homelessness upon committal) a proportion meta-analysis was conducted to calculate the pooled percentage of prisoners who were suffering from each outcome. Inconsistency was measured across studies using the I 2 statistic, which reflects the percentage of variability in effect estimates due to heterogeneity, rather than sampling error; 30–60% is considered moderate levels of heterogeneity, 50–90% substantial heterogeneity and 75–100% considerable heterogeneity (Higgins & Green, Reference Higgins and Green2011). Heterogeneity in meta-analysis refers to when the true effects being evaluated differ between studies. If the variation between the studies’ results is above that expected by chance, there is evidence of heterogeneity. The Cochrane Q test was used to test heterogeneity, where random effects models were used where there was evidence of significant heterogeneity and fixed effects models where there was no evidence of significant heterogeneity. Meta-analysis calculations were performed and graphical plots were created using the StatsDirect software.
Study quality
For each included study, the quality of the study was assessed using the adapted Newcastle–Ottawa scale (Wells et al. Reference Wells, Shea, O’Connell, Robertson, Peterson, Welch, Losos and Tugwell2014). This is a commonly used quality assessment tool for non-randomised studies including case control and cohort designs. It has previously been adapted to use in cross-sectional studies (Herzog et al. Reference Herzog, Álvarez-Pasquin, Díaz, Del Barrio, Estrada and Gil2013). However, due to the lack of validation for cross-sectional studies, we have used this as a descriptive indicator of study quality and not in statistical weighting.
Results
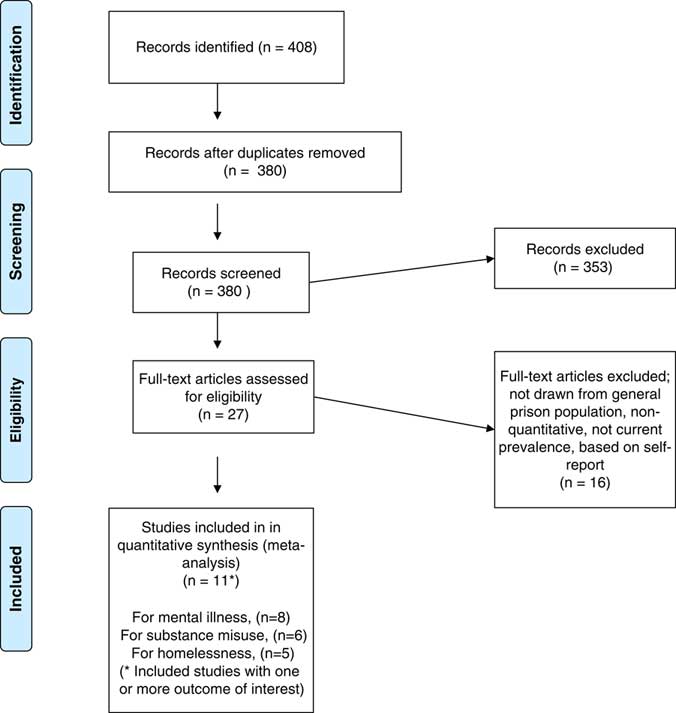
We reviewed 408 abstracts of which inclusion criteria were met for eight, six and five studies reporting the prevalence of major mental illness, substance misuse and homelessness on committal, respectively (Fig. 1). Study quality is reported using the adapted Newcastle–Ottawa scale in Table 1. Based on the evidence of significant heterogeneity in our review, random effects models were used for proportion meta-analyses.

Fig. 1 Study inclusion flowchart.
Table 1 Study quality assessment (adapted Newcastle–Ottawa Scale)

Legend for rating: representativeness of sample (0–1)+sample size (0–1)+non-respondents (0–1)+use of validated tool (0–2)+assessment of outcome (0–2)+statistical methods (0–1), maximum score=8.
Psychotic disorder
Eight studies, with a total sample size of 28 012 prisoners, reported suffering from a psychotic disorder (Table 2). The pooled percentage suffering from a psychotic disorder, from a random effects model, was 3.6% (95% CI=3.0–4.2%) (Fig. 2a). There was substantial heterogeneity in the percentage of prisoners diagnosed with a psychotic disorder across studies (I 2=54.8%; Cochran’s Q p=0.03).
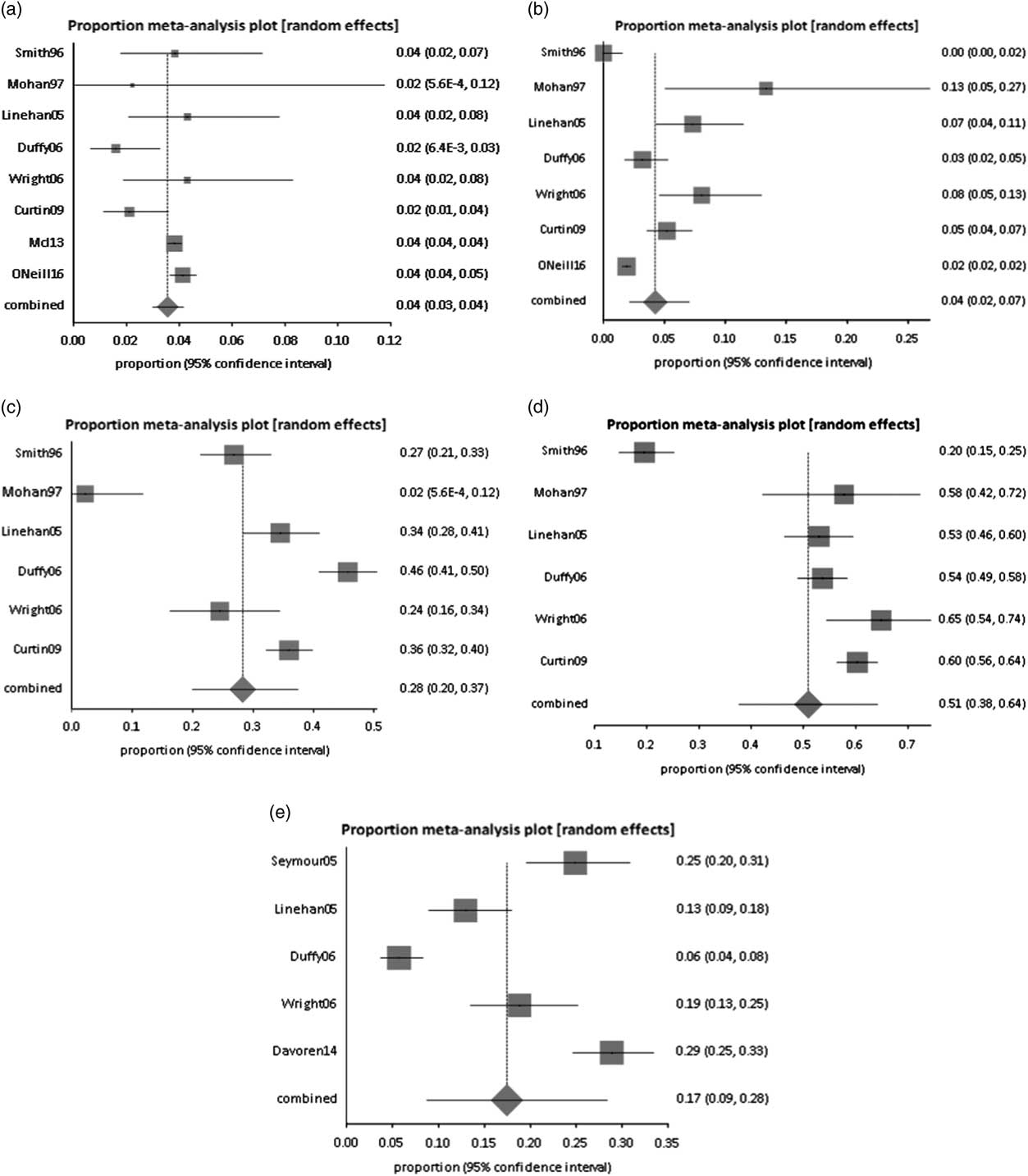
Fig. 2 Forest plot of studies with prisoners (a) diagnosed with a psychotic disorder, (b) diagnosed with an affective disorder, (c) diagnosed with an alcohol use disorder, (d) diagnosed with a substance use disorder and (e) homeless on committal.
Table 2 Prevalence of psychotic disorder
CI=confidence interval; DSM=Diagnostic and Statistical Manual of Mental Disorders; ICD=International Classification of Disease.
The prevalence in male samples was 3.81% (n=1060/27 781). Only two studies (Mohan et al. Reference Mohan, Scully, Collins and Smith1997; Wright et al. Reference Wright, Duffy, Curtin, Linehan, Monks and Kennedy2006) evaluated prevalence in a purely female sample and estimates for females were 3.9% (n=9/231). Estimates of prevalence in purely remand samples could be extracted from four studies (Linehan et al. Reference Linehan, Duffy, O’Neill and Kennedy2005; Curtin et al. Reference Curtin, Monks, Wright, Duffy, Linehan and Kennedy2009; McInerney et al. Reference McInerney, Davoren, Flynn, Mullins, Fitzpatrick, Caddow and O’Neill2013; O’Neill et al. Reference O’Neill, Smith, Caddow, Duffy, Hickey, Fitzpatrick, Caddow, Cronin, Joynt, Azvee, Gallagher, Kehoe, Maddock, O’Keefe, Brennan, Davoren, Owens, Mullaney, Keevans, Maher and Kennedy2016) and were 3.9% (n=1043/26 806).
Major affective disorder
Seven studies, with a total sample size of 7928 prisoners, reported an affective disorder (Table 3). The pooled percentage suffering from an affective disorder, from a random effects model, was 4.3% (95% CI=2.1–7.1%) (Fig. 2b). There was considerable heterogeneity in the percentage diagnosed with an affective disorder across studies (I 2=91.9%; Cochran’s Q p<0.001).
Table 3 Prevalence of major affective disorder

CI=confidence interval; DSM=Diagnostic and Statistical Manual of Mental Disorders; ICD=International Classification of Disease.
Prevalence from male samples was 2.33% (n=180/7697). Only two studies (Mohan et al. Reference Mohan, Scully, Collins and Smith1997; Wright et al. Reference Wright, Duffy, Curtin, Linehan, Monks and Kennedy2006) evaluated prevalence in a purely female sample and estimates for females were 9.1% (n=21/231). Estimates of prevalence in purely remand samples could be extracted from two studies (Linehan et al. Reference Linehan, Duffy, O’Neill and Kennedy2005; O’Neill et al. Reference O’Neill, Smith, Caddow, Duffy, Hickey, Fitzpatrick, Caddow, Cronin, Joynt, Azvee, Gallagher, Kehoe, Maddock, O’Keefe, Brennan, Davoren, Owens, Mullaney, Keevans, Maher and Kennedy2016) and were 2.1% (n=134/6409).
Alcohol and substance use disorders
Six studies, with a total sample size of 1659 prisoners, reported alcohol or substance use disorders (Table 4). The pooled percentage suffering from alcohol disorder across the six studies, from a random effects model, was 28.3% (95% CI=19.9–37.4%) (Fig. 2c). There was considerable heterogeneity in the percentage suffering from alcohol use disorder across studies (I 2=92.9%; Cochran’s Q p<0.0001). The pooled percentage of prisoners reporting a substance use disorder across the studies, from a random effects model, was 50.9% (95% CI=37.6–64.2%) (Fig. 2d). There was considerable heterogeneity in the percentage suffering from substance use disorder across studies (I 2=96.4%, Cochran’s Q p<0.001).
Table 4 Prevalence of alcohol and substance use disorders
CI=confidence interval; DSM=Diagnostic and Statistical Manual of Mental Disorders; ICD=International Classification of Disease.
Prevalence in male only samples was 37.1% (n=564/1520) for alcohol use disorder and 51% (n=775/1520) for substance use disorder. Two studies (Mohan et al. Reference Mohan, Scully, Collins and Smith1997; Wright et al. Reference Wright, Duffy, Curtin, Linehan, Monks and Kennedy2006) evaluated prevalence in a purely female sample and estimates for females were 17.2% (n=24/139) for alcohol use disorder and 62.6% (n=87/139) for substance use disorder. Estimates of prevalence in purely remand samples could be extracted from only one study (Linehan et al. Reference Linehan, Duffy, O’Neill and Kennedy2005) and were 34.5% (n=80/232) for alcohol use disorder and 53% (n=123/232) for substance use disorder.
Homelessness on committal
Five studies, with a total sample size of 1523 prisoners reported homelessness at time of committal (Table 5). The pooled percentage of homelessness from a random effects model was 17.4% (95% CI=8.7–28.4%) (Fig. 2e). There was considerable heterogeneity in the percentage of homelessness in comital across studies (I 2=96.2%; Cochran’s Q p<0.001).
Table 5 Prevalence of homelessness on committal
CI=confidence interval.
Prevalence in purely male samples was 8.2% (n=55/670). Only one study (Wright et al. Reference Wright, Duffy, Curtin, Linehan, Monks and Kennedy2006) evaluated prevalence in a purely female sample and estimates for females were 18.8% (n=35/186). Estimates of prevalence in purely remand samples could be extracted from two studies (Linehan et al. Reference Linehan, Duffy, O’Neill and Kennedy2005; Davoren et al. Reference Davoren, Fitzpatrick, Caddow, Caddow, O’Neill, O’Neill and Kennedy2015) and were 23.2% (n=153/658).
Discussion
Prisoners can experience a range of barriers to successful re-entry into society (Sarma, Reference Sarma2014). Homelessness, mental illness and substance misuse are three such barriers, which our study shows as being prevalent in Irish prisons. To our knowledge, this is the first systematic review estimating the current prevalence of these vulnerabilities amongst Irish prisoners.
Implications
A number of implications arise from these findings. This study confirms that a significant proportion of Irish prisoners present with a current psychotic or major affective disorder, which are potentially treatable mental illnesses. From a clinical view point, effective treatment of mental illness may reduce morbidity as well as potentially reduce mortality through suicide (Kapur, Reference Kapur2009), and potentially impact recidivism rates (Lovell et al. Reference Lovell, Gagliardi and Peterson2002). This finding strengthens the argument for the development of diversion services which, to date, are geographically variable and still evolving in Ireland (Gulati & Kelly, Reference Gulati and Kelly2018). Ireland has the lowest per capita secure psychiatric bed availability in developed countries (Kennedy, Reference Kennedy2016). Diversion services need an expansion of bed capacity within Irish mental health services (Kennedy, Reference Kennedy2006; Gulati & Kelly, Reference Gulati and Kelly2018) and changes in attitudes towards mentally disordered offenders (Duffy et al. Reference Duffy, Lenihan and Kennedy2003). Rates for psychotic disorders are in keeping with international estimates of prison morbidity (Fazel & Seewald, Reference Fazel and Seewald2012), which are significantly higher than general population estimates (Saha et al. Reference Saha, Chant, Welham and McGrath2005).
Rates for affective disorders in our study were higher, as would be expected in purely female samples, but low for remand samples in Ireland. The overall rates were lower than international comparisons and this may be due to the skewing of results based on one study where no prisoner was found to be suffering from a major affective disorder (Smith et al. Reference Smith, O’Neill, Tobin, Walshe and Dooley1996) or the use of point prevalence estimates in our study as opposed to period prevalence estimates in international comparisons. However, this would not explain why the rates in remand samples were low and may inform the need to review whether current screening processes for affective disorder in remand prisons (Grubin et al. Reference Grubin, Carson and Parsons2002) are adequate.
The burden of harmful use or dependence on alcohol and substances in Irish prisons is substantial. One in three prisoners had a current alcohol misuse or dependence and one in two, a problem with current substance misuse or dependence. This is in keeping with international prison estimates (Fazel et al. Reference Fazel, Bains and Doll2006) and substantially higher than Irish general population estimates (Irish Medical Organisation, 2015). Substance and alcohol misuse are seen as key risk factors for recidivism. Prison and probation services have invested in treatment programmes, but availability remains variable geographically. In the Irish context, treatment programmes for women, those specific to alcohol misuse as well as those focussed on novel drugs of misuse are seen as gaps in provision (Clarke & Eustace, Reference Clarke and Eustace2016). The co-occurrence of severe mental illness and substance use or abuse disorder are common (Buckley, Reference Buckley2006) with causes including self-medication, genetic vulnerability or lifestyle. The consequences include self-neglect, poor physical health, poor medication adherence, increased suicide risk and increased recidivism. There may be value in integrated treatment plans for that address both the addiction disorder and the mental illness (Minkoff, Reference Minkoff1989).
Our study found that over one in six Irish prisoners is homeless at the point of committal. This is higher than prison estimates in the United States (Hughes et al. Reference Hughes, Wilson and Beck2001; Greenberg & Rosenheck, Reference Greenberg and Rosenheck2008) but only slightly higher than a comparative UK prison estimate (Williams et al. 2012). However, it is significantly higher than the prevalence of homelessness in the general Irish population (Central Statistics Office, 2016). McCann (Reference McCann2003) concluded that homelessness was both a cause and consequence of imprisonment. Hickey (Reference Hickey2002) qualitatively studied the experience of ex-offenders. Nearly half of those participating in Hickey’s study highlighted homelessness as one of the key contributory factors leading them to re-offend on release. Recidivism rates in Ireland are often used as a proxy for the success of rehabilitation programmes (Martynowicz & Quigley, Reference Martynowicz and Quigley2010). Analysing data relating to over 19 000 prisoners in Ireland, O’Donnell et al. (Reference O’Donnell, Baumer and Hughes2008) found that 49.2% of prisoners were re-imprisoned within 4 years with 27.4% within the first year. Addressing homelessness would potentially impact recidivism and imprisonment rates over and above the obvious humanitarian impact.
The coexistence of severe mental illness, substance misuse and homelessness has been studied in international literature (Drake et al. Reference Drake, Osher and Wallach1991) and these often go hand in hand, interacting in ways that amplify the vulnerability of an individual. Homeless individuals with mental illness are unlikely to seek help and treatment, and those that also have an active substance misuse often excluded from temporary accommodation, with the consequent further social decline and increased risk of imprisonment. It would follow that efforts to find suitable accommodation through resettlement services should be undertaken in conjunction with treatment of mental illness and/or substance misuse in prisoners.
In summary, the extent of psychiatric and psychosocial morbidity in worldwide prisons is of international concern as they are significantly higher than general population prevalence. Our review found that levels of psychiatric and psychosocial morbidity in Irish prisons are largely in keeping with worldwide prison estimates, and recommends improved screening for affective disorders, the development of diversion services and the consideration of integrated treatment plans addressing the psychiatric and psychosocial need.
Strengths and limitations
The strengths of this review include the search criteria which led to the identification of multiple samples for each outcome of interest within a relatively small jurisdiction.
The key limitation of this study is the high level of heterogeneity. While pooled prevalences are reported, and random effects model used to account for heterogeneity, we recommend interpreting these results with caution. Such a high level of heterogeneity would be expected in such a study in view of differences in study designs, study periods, sampling, diagnostic criteria (International Classification of Disease v. Diagnostic and Statistical Manual of Mental Disorders), category of prisoners (remand v. sentenced v. mixed) and gender differences, as has been seen in previous meta-analyses (Fazel & Seewald, Reference Fazel and Seewald2012). Furthermore, two included studies (McInerney et al. Reference McInerney, Davoren, Flynn, Mullins, Fitzpatrick, Caddow and O’Neill2013; O’Neill et al. Reference O’Neill, Smith, Caddow, Duffy, Hickey, Fitzpatrick, Caddow, Cronin, Joynt, Azvee, Gallagher, Kehoe, Maddock, O’Keefe, Brennan, Davoren, Owens, Mullaney, Keevans, Maher and Kennedy2016) used case ascertainment through screening. In McInerney et al.’s study (Reference McInerney, Davoren, Flynn, Mullins, Fitzpatrick, Caddow and O’Neill2013), screening consisted of selecting all committals who on reception disclosed a history of previous psychiatric contact or prescription of psychiatric medication, a history of deliberate self-harm, who exhibited unusual or disturbed behaviour, those charged with homicide and individuals with a known history of treatment by prison psychiatric services. In O’Neill et al.’s study (Reference O’Neill, Smith, Caddow, Duffy, Hickey, Fitzpatrick, Caddow, Cronin, Joynt, Azvee, Gallagher, Kehoe, Maddock, O’Keefe, Brennan, Davoren, Owens, Mullaney, Keevans, Maher and Kennedy2016), this was undertaken using the Grubin screening tool questions (Grubin et al. Reference Grubin, Carson and Parsons2002) which has a reported sensitivity and specificity of 97% and 84%, respectively, in a UK sample. The use of screening for case ascertainment has the potential to bias prevalence estimates.
Future research may usefully be aimed at re-evaluating point prevalence of these vulnerabilities through an up to date nationwide cross-sectional study with robust study design and standardised outcome measures to limit heterogeneity.
Acknowledgements
The authors would like to thank Dr Anna Zornoza, St Hugh’s College, University of Oxford, Dr Valerie Murphy, University College Cork and Professor Ailish Hannigan, University of Limerick for their assistance.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
All authors have no conflicts of interest.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008. The authors assert that ethical approval for publication of this paper was not required by their local REC.