Introduction
Sleep problems are common in children and adolescents with autism spectrum disorder (ASD) (Richdale & Schreck, Reference Richdale and Schreck2009; Mannion & Leader, Reference Mannion and Leader2013; Wiggs & Stores, Reference Wiggs and Stores2004). Several studies have reported settling problems with some children with ASD taking more than an hour to fall asleep (Angriman et al. Reference Angriman, Caravale, Novelli, Ferri and Bruni2015; Cortesi et al. Reference Cortesi, Giannotti, Ivanenko and Johnson2010; Kotagal & Broomall, Reference Kotagal and Broomall2012). The reported prevalence of sleep problems in ASD has varied in the research from 33% (Goldman et al. Reference Goldman, McGrew, Johnson, Richdale, Clemons and Malow2011) to 80% (Mannion et al. Reference Mannion, Leader and Healy2013). Sleep problems have been found to persist over time in children and adolescents with ASD (Mannion & Leader, Reference Mannion and Leader2016). Prevalence of sleep problems in children with ASD is much higher than in typically developing children (Souders et al. Reference Souders, Mason, Valladares, Bucan, Levy and Mandell2009), with research finding sleep problems were more than twice as common in children with ASD as in the general population (Reynolds et al. Reference Reynolds, Soke, Sabourin, Hepburn, Katz, Wiggins and Levy2019).
Impact of sleep problems on the child
Sleep problems in children with ASD have a negative impact on various other aspects of the child’s life. Many children with ASD and other developmental disorders experience other comorbid conditions such as behaviour problems, toileting problems, attention-deficit/hyperactivity disorder, overselectivity, epilepsy and gastrointestinal symptoms (Devlin et al. Reference Devlin, Healy, Leader and Reed2008; Francis et al. Reference Francis, Mannion and Leader2017; Kelly et al. Reference Kelly, Leader and Reed2015); Leader et al. Reference Leader, Francis, Mannion and Chen2018; Leader & Mannion, Reference Leader, Mannion and Matson2016a; Reference Leader, Mannion and Matson2016b; Mannion & Leader, Reference Mannion and Leader2014a; Reference Mannion and Leader2014b; Newman et al. Reference Newman, Leader, Chen and Mannion2015). Research has begun to investigate the relationships between sleep problems and other comorbid conditions in ASD.
Positive correlations have been found between sleep problems and daytime challenging behaviour (Adams et al. Reference Adams, Matson, Cervantes and Goldin2014; Goldman et al. Reference Goldman, McGrew, Johnson, Richdale, Clemons and Malow2011; Sikora et al. Reference Sikora, Johnson, Clemons and Katz2012; Tudor et al. Reference Tudor, Hoffman and Sweeney2012). Correlations have also been found between sleep problems and hyperactivity, and compulsive and ritualistic behaviours, compared to children without sleep problems (Goldman et al. Reference Goldman, Surdyka, Cuevas, Adkins, Wang and Malow2009). Research has found significant positive associations between sleep problems, anxiety and challenging behaviour, with medication, anxiety and sleep problems accounting for 42% of the variance in challenging behaviour (Rzepecka et al. Reference Rzepecka, McKenzie, McClure and Murphy2011). Sleep problems have been shown to be a predictor of anxiety in children and adolescents with ASD (Williams et al. Reference Williams, Leader, Mannion and Chen2015).
Research has found that fewer hours of sleep per night predicted overall autism severity scores and social skills deficits (Adams et al. Reference Adams, Matson, Cervantes and Goldin2014; Schreck et al. Reference Schreck, Mulick and Smith2004). Stereotypic behaviour was predicted by fewer hours of sleep per night and screaming during the night, and poor sleepers with ASD have a higher percentage of behavioural problems than good sleepers with ASD (Schreck et al. Reference Schreck, Mulick and Smith2004).
Impact of sleep problems on parents
Sleep problems that affect children with ASD also affect parent’s sleep quality and quantity. Children waking during the night usually need parental help and/or attention, resulting in sleep loss for one or both parents (McCann et al. Reference McCann, Bull and Winzenberg2015; Meltzer & Mindell, Reference Meltzer and Mindell2007). Parent sleep can be affected by other factors, such as stress. Parents of children with developmental disabilities reported poorer sleep quality than parents of typically developing children, and that the strongest predictor of poor sleep quality was parental stress (Gallagher et al. Reference Gallagher, Phillips and Carroll2010).
Research has found that children’s sleep problems have a negative impact on parent anxiety and depressive symptoms levels. Children’s sleep behaviours have been shown to place a strain on marital relationships and financial insecurity (Kirkpatrick et al. Reference Kirkpatrick, Gilroy and Leader2019). Research has shown that maternal sleep quality was a significant predictor of maternal mood, stress and fatigue (Bar et al. Reference Bar, Efron, Gothelf and Kushnir2016; Kouros & El-Sheikh, Reference Kouros and El-Sheikh2017; Meltzer & Mindell, Reference Meltzer and Mindell2007). Children with ASD who had significant sleep disruptions were significantly more likely to have mothers with more depressive symptoms, fatigue and daytime sleepiness (Delahaye et al. Reference Delahaye, Kovacs, Sikora, Hall, Orlich, Clemons and Kuhlthau2014; Hodge et al. Reference Hodge, Hoffman, Sweeney and Riggs2013). Mothers of children who had significant sleep disruptions reported greater feelings of parenting stress and care-giving overload. Greater sleep and behaviour problems in children had a significant association with disturbed sleep and increased depressive symptoms, anxiety and stress levels in mothers (Chu & Richdale, Reference Chu and Richdale2009).
Children’s sleep significantly predicted maternal mental health, maternal sleep and maternal stress, and maternal sleep and maternal stress each predicted maternal mental health (Hodge et al. Reference Hodge, Hoffman, Sweeney and Riggs2013). Children’s sleep and maternal sleep were more closely related to maternal stress for mothers of typically developing children, and it was concluded that this may be because stress related to sleep is minor relative to other sources of stress relating to their child’s disability (Hodge et al. Reference Hodge, Hoffman, Sweeney and Riggs2013).
Actigraph for monitoring and tracking sleep
Strong evidence would support the use of the actigraph to objectively monitor and track sleep (Adkins et al. Reference Adkins, Molloy, Weiss, Reynolds, Goldman, Burnette and Malow2012; Meltzer et al. Reference Meltzer, Montgomery-Downs, Insana and Walsh2012; Wiggs & Stores, Reference Wiggs and Stores2004). The actigraph device can be used at home and is considered a reliable and an objective method for measuring sleep–wake patterns, onset of sleep, continuity and sleep duration (Wiggs & Stores, Reference Wiggs and Stores2004), making the actigraph suitable for the current study.
Current study
The current pilot study aimed to expand on existing research in critical ways. We primarily sought to extend current literature using objective sleep measurements through the use of actigraphy. In doing so, we sought to assess sleep in children with ASD and their parents. We also examined subjective measures of sleep, including further measures associated with well-being, namely parental stress, anxiety, depressive symptoms and overall quality of life. This pilot study sought to address several limitations in existing research at this critical research intersection, while providing a basis for future research in this area.
Method
Participants
Families of children with ASD were recruited for the current study if they had a child aged between 3 and 18 years and were recruited through special schools, schools with ASD units and from parent support groups. Once an interested individual contacted the researchers, and it was confirmed that their child had an independent diagnosis of ASD, and were aged between 3 and 18 years, they were recruited for the study.
The study sample comprised of nine children and adolescents with a diagnosis of ASD in accordance with DSM-IV-TR criteria (American Psychiatric Association, 2000). Diagnoses were provided by a licenced psychologist or paediatrician independent of the study. The participants received their diagnosis as a result of the formal diagnostic protocol which employs multiple diagnostic measures. Caregiver information on professional diagnosis, diagnostic setting/organisation and professional(s) who made the diagnosis was obtained.
The final sample consisted of a total of 21 participants (nine families – nine mothers, three fathers and nine children). Selection bias may have occurred. We attempted to address this by advertising that we were looking to recruit families where the child did not have sleep problems also. However, it is possible that only families where the child had sleep problems chose to participate in the study. Some children were not able to tolerate the use of actigraphs, which impacted upon the attrition rate. The descriptive statistics for participants are presented in Table 1.
Table 1. Descriptive statistics of participants

ADHD, attention-deficit/hyperactivity disorder.
Standard deviations appear in the parentheses beside the mean score.
Measures
The questionnaire booklet consisted of a demographic questionnaire, the below questionnaires and sleep diaries for the parent(s) and child. The demographic questionnaire consisted of questions on the child’s age, gender, diagnosis, comorbidity, education and medication.
Sleep diary
Participants completed a sleep diary for 7 days, for themselves and their children. They recorded when the actigraph was removed, and what time it was replaced, the start and end time of any naps taken, time got into bed and time turned out lights, time woke up in the morning, time turned on lights and time got out of bed. Research has suggested that it is useful to use a sleep diary, as it has been shown to be an important adjunct to actigraphy when used to edit data and remove artefacts (Wiggs & Stores, Reference Wiggs and Stores2004).
The Pittsburgh Sleep Quality Index (PSQI)
The participants (mothers and fathers) completed the Pittsburgh Sleep Quality Index (PSQI) (Buysse et al. Reference Buysse, Reynolds, Monk, Berman and Kupfer1989). The 19-item self-report questionnaire assesses sleep quality and sleep disruption. Seven dimensions of sleep: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications and daytime dysfunction were measured. The component scores are summed to give a total sleep quality score, which ranges from 0 to 21. A total score of ≥5 has been recommended as clinically significant in terms of poor sleep quality. The scale has acceptable internal consistency and good test–retest reliability (Buysse et al. Reference Buysse, Reynolds, Monk, Berman and Kupfer1989).
The Parenting Stress Index-Short Form (PSI/SF-4)
The Parenting Stress Index-Short Form (PSI/SF-4) (Abidin, Reference Abidin2012) is a standardised measure used to evaluate stress in parents that are at risk for parenting problems or child behavioural problems. The questionnaire consists of 36 items pertaining to parental feelings and experiences, comprising 3 scales: Parental Distress, Parent–Child Dysfunctional Interaction and Difficult Child Characteristics. Parents rate their agreement for each statement on a five-point Likert scale, ranging from 1 (strongly agree) to 5 (strongly disagree). The scales have shown high internal consistency and adequate test–retest reliability and have been used widely in studies of parents of children with disabilities (Dardas & Ahmad, Reference Dardas and Ahmad2014).
Multidimensional Scale of Perceived Social Support (MSPSS)
The Multidimensional Scale of Perceived Social Support (MSPSS) (Zimet et al. Reference Zimet, Dahlem, Zimet and Farley1988) is a 12-item self-report measure that evaluates a person’s perceived social support, from three subscales – family, friends and significant other. It was utilised as an additional variable to analyse parent stress. The MSPSS has demonstrated good internal and test-retest reliability, with high levels of social support associated with low levels of depressive symptoms and anxiety (Canty-Mitchell & Zimet, Reference Canty-Mitchell and Zimet2000; Zimet et al. Reference Zimet, Dahlem, Zimet and Farley1988).
The Hospital Anxiety and Depression Scale (HADS)
The Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, Reference Zigmond and Snaith1983) was used to assess parent levels of anxiety and depressive symptoms. The scale consists of 14 items, 7 assessing anxiety and 7 assessing depressive symptoms. It yields a total depressive symptoms score and a total anxiety score. A score of 0–7 is classified as normal for each score, 8–10 is classified as borderline abnormal (borderline case) and 11–21 is classified as abnormal. It has demonstrated good internal validity and concurrent validity and has been found to perform well in assessing the symptom severity and cases of anxiety disorders and depressive symptoms in somatic, psychiatric and primary care patients and in the general population (Bjellend et al. Reference Bjellend, Dahl, Haug and Neckelmann2002).
WHOQOL-BREF (World Health Organization’s Quality of Life Questionnaire-BREF)
Parent’s quality of life was assessed using the WHOQOL-BREF (World Health Organization; The WHOQOL Group, 1998), an abbreviated version of the WHOQOL-100. The questionnaire consists of several demographic questions at the beginning, followed by 26 items which are rated on a 5-point scale. These items assess four domains: physical health, psychological, social relationships and environment. The mean score of items within each domain is used to calculate the domain score. The scale has been shown to have good reliability and validity in adult populations (Krägeloh et al. Reference Krägeloh, Kersten, Billington, Hsu, Shepherd, Landon and Feng2013).
Actigraphy
All participants (mothers, fathers and children) were asked to wear an actigraph (Actiwatch 2, Philips Respironics, Norfolk, UK) for 7 consecutive days and nights, worn on the non-dominant wrist. The actigraphs were configured using a 1-minute epoch, with medium threshold, as this is the most widely used epoch length in sleep research (Meltzer et al. Reference Meltzer, Montgomery-Downs, Insana and Walsh2012). Parents were instructed to press the event marker button on the side of the actigraph to mark sleep onset and sleep offset on their own actigraphs, and to do so on their child’s actigraph also. Objective sleep quantity was measured by total sleep time (TST, total time within rest intervals scored as sleep). Additional data gathered and their definitions are as follows: (1) bedtime (time when the subject went to bed with the intent to sleep); (2) get-up time (time when the subject rose from bed for the final time); (3) time in bed (period of time between bedtime and get-up time); (4) onset latency (period of time between bedtime and sleep start time); (5) sleep efficiency (percentage of time in bed actually spent sleeping); (6) wake after sleep onset (WASO; the number of waking minutes between sleep start and sleep end times); and (7) #Awak (the number of continuous blocks of wake). A validated Philips Actiware software (Version 6, Philips Respironics) algorithm was used to estimate sleep parameters, based on thresholds for wake and sleep (Adkins et al. Reference Adkins, Molloy, Weiss, Reynolds, Goldman, Burnette and Malow2012). Actigraphy has been widely used in recent years in sleep studies with both children and adults and has demonstrated good reliability and validity (Sadeh, Reference Sadeh2011).
Procedure
A home visit was arranged at a time convenient for the family. Data collection took place during the summer holidays. Informed consent was obtained from the parents, and verbal assent from the children. Parents were then given the actigraphs and shown how to use them and given instructions on proper care of them. They were also instructed on the use of the daily sleep diary. They were also given the questionnaire booklet, containing the questionnaires listed above. After 7 days, a second home visit was made to collect the actigraphs, sleep diaries and questionnaires.
Results
Parenting Stress Index-Short Form (PSI-SF)
The majority of parents scored highly on the PSI-SF, indicating high parenting-related stress. The means, standard deviations, range, minimum and maximum scores are presented in Table 2 below.
Table 2. Descriptive statistics for WHOQOL-BREF, HADS, PSI-SF and MSPSS questionnaires

Multidimensional Scale of Perceived Social Support (MSPSS)
The majority of participants scored highly on the MSPSS. The means, standard deviations, range, minimum and maximum scores are presented in Table 2 above.
Hospital anxiety and depression scale (HADS)
The majority of participants scored highly on both the anxiety and depressive symptoms subscales of the HADS. The means, standard deviations, range, minimum and maximum scores are presented in Table 2 above.
WHOQOL-BREF
The raw scores calculated for each of the four domains were transformed into a 0–100 scale score. Lower scores indicate lower quality of life. The majority of participants had lower than average quality of life scores. Hawthorne et al. (Reference Hawthorne, Herrman and Murphy2006) investigated population normative values for the WHOQOL-BREF. The normative values they found were 73.5 for Domain 1, 70.6 for Domain 2, 71.5 for Domain 3 and 75.1 for Domain 4, with an average for the four subscales of 72.66. The means, standard deviations, range, minimum and maximum scores are presented in Table 2 above.
Subjective sleep quality
The mean PSQI total score was higher for mothers (Mean = 8.56, S.D. = 3.36) than for fathers (Mean= 7.00, S.D. = 4.00), with a high mean total score for parents (Mean= 8.17, S.D. = 3.41). Meltzer (Reference Meltzer2008) stated that a total score of ≥5 on the PSQI is recommended as clinically significant in terms of poor sleep quality. Two parents (17%) had a total score of <5 on the PSQI, while 10 parents (83%) had a total score of ≥5, indicating that the majority of parents had self-reported sleep problems. The means, standard deviations and range of scores are presented in Table 3 below.
Table 3. Means, standard deviations and range for subjective sleep variables for parent

PSQI = Pittsburgh Sleep Quality Index.
Standard deviations appear in the parentheses beside the mean score.
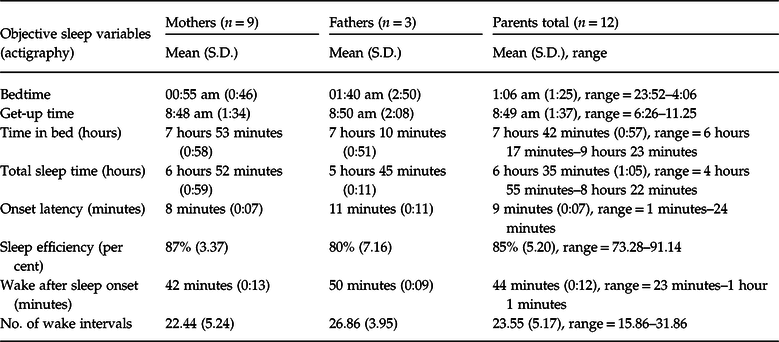
Actigraphy
A week (7 days and nights) of actigraph measurement produced an average for each of the sleep variables for both parents and children. The means and standard deviations for the range of sleep variables for parents are presented in Table 4. Souders et al. (Reference Souders, Mason, Valladares, Bucan, Levy and Mandell2009) stated that the Children’s Hospital of Philadelphia’s (CHOP) Sleep Centre recommends a sleep efficiency of <85% and a sleep-onset latency of >30 minutes as a cut-off for defining poor sleep quality. The majority of participants did not have poor sleep quality as indicated by poor sleep efficiency, with three participants (25%) having a sleep efficiency of <85%, while nine participants (75%) had a sleep efficiency of ≥85%. TST was less than recommended, with nine participants (75%) having ≤7 hours of sleep, with three participants (25%) having >7 hours.
Table 4. Means, standard deviations and range for objective sleep variables for parents
The means and standard deviations for the range of sleep variables for children were included in Table 5. Eight children (89%) had a TST of ≤8 hours, with one child (11%) getting >8 hours sleep. Four children (44%) had ≤7 hours of sleep, with five children having >7 hours of sleep per night, indicating less than recommended sleep time. Five children (56%) had <85% sleep efficiency, while four children (44%) had >85% sleep efficiency. The mean sleep efficiency of 83% is lower than the recommended cut-off of 85% indicating poor sleep quality.
Table 5. Means, standard deviations and range for objective sleep variables for children and adolescents with ASD

Correlation analyses
Subjective and objective sleep measures
Pearson’s correlations were used to test for associations between the subjective and objective sleep variables. No significant relationships were found between the subjective sleep measures (PSQI) and any of the objective (actigraph) sleep variables.
Sleep issues and stress
Pearson’s correlations were conducted to determine if there was a relationship between self-reported sleep quality (PSQI total score) and parent stress (PSI total stress), and between actigraph variables and parent stress. There were no significant correlations between parent stress and subjective sleep quality, or between parent stress and any of the child actigraph variables. There was only one significant correlation for the parent actigraph variables, a positive association between PSI total stress and sleep efficiency (as measured by actigraph), (r (12) = .61, p = .04), with a large effect size.
Sleep issues and parent depressive symptoms
Pearson’s correlations were conducted to determine if there was a relationship between self-reported sleep quality and parent depressive symptoms, and between actigraph variables and parent depressive symptoms. A large positive correlation was found between the global PSQI score and HADS depressive symptoms score, (r (12) = .70, p < .05). A significant negative correlation was found between HADS depressive symptoms score and parent sleep latency, (r (12) = -.70, p = .01, with a large effect size. Of the child actigraph variables, one significant correlation was found, between child WASO and HADS depressive symptoms score, (r (12) = .63, p = .03), with a large effect size.
Sleep issues and parent anxiety
Pearson’s correlations were conducted to determine if there was a relationship between self-reported sleep quality and parent anxiety, and between actigraph variables and parent anxiety, with no significant correlations found.
Sleep issues and quality of life
Pearson’s correlations were conducted to determine if there was a relationship between self-reported sleep quality and parent quality of life, and between actigraph variables and parent quality of life. One significant positive correlation was found between average WHOQOL-BREF scores and sleep efficiency (actigraphy), (r (12) = .60, p = .04, with a large effect size.
Parent sleep variables and child sleep variables
Pearson’s correlations were conducted to determine if there was a relationship between parent actigraph variables and child actigraph variables, with no significant correlations found.
Discussion
The current pilot study was the first study to use a multi-method approach to examine both child and parent sleep, and their relationship with parent stress, anxiety, depressive symptoms and quality of life. The current study diverges from previous findings that report child sleep disruption affects parent sleep, in that within the current sample child shorter TST, lower sleep efficiency and waking after sleep onset did not impact on parent sleep. One possible reason is that the child may not have sought parental attention, which is a factor which may warrant further investigation.
A significant association was found between parent depressive symptoms and self-reported subjective sleep quality, consistent with previous research (Chu & Richdale, Reference Chu and Richdale2009; Hall et al. Reference Hall, Moynihan, Bhagat and Wooldridge2017; Meltzer, Reference Meltzer2011). A significant positive association was found between parent depressive symptoms and child WASO, that is, that higher parent depressive symptoms were associated with child sleep disruptions during the night. In addition to depressive symptoms, research has indicated that sleep disturbance and sleep disorders could be linked to alcohol use and abuse in alcoholics and non-alcoholics (Roehrs & Roth, Reference Roehrs and Roth2001). Caffeine consumption has also been reported as having a detrimental impact on sleep patterns, especially in adolescents (Snel & Lorist, Reference Snel and Lorist2011). Evidence also suggests that nicotine influences sleep and mood and that smoking increased sleep-related respiratory disorders which negatively impact on sleep quality and increased daytime tiredness (Jaehne et al. Reference Jaehne, Loessl, Bárkai, Riemann and Hornyak2009). It is possible that parent self-reported reduced quantity and good quality of sleep could have been linked to alcohol use or abuse, caffeine and or nicotine consumption. Although beyond the scope of the current study, the measurement of the aforementioned sleep problem contributors would be considered beneficial to future research.
A positive correlation was found between quality of life and parent sleep efficiency, that is, lower quality of life scores was associated with lower sleep efficiency. This may be because individuals with a lower quality of life have many worries, for example, money, work, children, lack of social support, etc., which impact on their sleep quality. Although lower quality of life may not have an impact physically, it has an impact on psychological well-being, therefore contributing to the poorer sleep quality.
A significant negative association was found between parent depressive symptoms and parent’s sleep-onset latency, indicating that higher parent depressive symptoms was associated with shorter sleep-onset latency. No significant correlations were found between the subjective sleep measures (PSQI) and the objective sleep measures (actigraphy). This may suggest that subjective measures of sleep may be unreliable compared to objective measures such as actigraphy, and that self-report measures may overestimate or exaggerate sleep problems. It may also suggest that parents feel frustrated or burnt out. The subjective and objective measures of sleep did not match well, which indicates that subjective measures of sleep should be improved in the future. The concordance between subjective sleep measures and actigraphy should be addressed in future research.
The main findings of the study indicate that parental depressive symptoms may be linked to self-reported sleep quality, and child sleep disruptions. Parental self-reported depressive symptoms were higher than average normative values (Hinz & Brähler, Reference Hinz and Brähler2011), as was self-reported anxiety. No associations were found between parent anxiety and parent or child sleep, which may suggest that parental anxiety is linked to other child issues, for example, child behaviour problems, symptom severity, etc. Certain sleep issues were apparent in the children in this study, including TSTs that are less than recommended for children, with 89% of the children in the study getting less than 8 hours of sleep on average per night, and 44% getting less than 7 hours per night. Sleep recommendations indicate that children aged between 7 and 12 years of age should get 10 to 11 hours of sleep per night, and that children aged 12–18 years should get 8 to 9 hours of sleep (National Sleep Foundation, 2015). The average sleep efficiency was lower than the recommended cut-off of 85% (Souders et al. Reference Souders, Mason, Valladares, Bucan, Levy and Mandell2009), indicating less than recommended sleep quality. WASO was also an issue for children.
The sleep patterns of parents in this study did not appear abnormal. Bedtimes, get-up times and TSTs were wide ranging. Sleep-onset latency was short, with an average latency of 9 minutes, and average sleep efficiency was 85%, indicating that the sleep quality was quite good. The high PSQI scores did not appear to correlate with the actigraph variables, apart from less than recommended TST, with parents getting an average of 6 hours 35 minutes of sleep per night (7–8 hours is recommended for adults), and WASO was quite high, with parents spending an average of 44 minutes awake each night, with 92% of parents awake for longer than 30 minutes each night.
Results were found that also contradict previous research on parent stress and sleep, with a positive correlation found between parent stress and parent sleep efficiency, indicating that higher parent stress was linked to greater parent sleep efficiency. The results indicated that parents with high stress and/or depressive symptoms levels may be more tired and sleep better as a result. This result is in contrast to previous results (Gallagher et al. Reference Gallagher, Phillips and Carroll2010), which found that parental stress was associated with poorer sleep quality. However, this result was based on subjective sleep measures, which may not be as reliable as actigraphy. Similar results have been found as the current study, where child and parent sleep were more closely linked to parent stress for parents of typically developing children than for parents of children with ASD (Hodge et al. Reference Hodge, Hoffman, Sweeney and Riggs2013). This may be because stress related to sleep is minor relative to other sources of stress relating to their child’s disability.
Parent stress, anxiety and depressive symptoms were all higher than average, with quality of life lower than average. The mean PSI stress score was in the 86th percentile, indicating very high stress levels for parents. As no associations were found between parent stress and parent or child sleep problems, it would appear that parent stress may be linked to other factors not examined in the current study, for example, child behaviour or child functioning. Furthermore, 89% of mothers and 67% of fathers scored above average for both self-reported anxiety and depressive symptoms. In support of this, previous research has found that 83% of parents reported lower than average quality of life (Hawthorne et al. Reference Hawthorne, Herrman and Murphy2006), which again was not found to be linked to parent or child sleep problems.
The current study had several methodological strengths, including objective measurement (actigraphy) of both parent and child sleep, which has been used in very few studies. The questionnaires used in the study have been validated and shown to be reliable. The study examined several relationships between parent sleep and parent issues, and child sleep and parent issues.
There were also several limitations. Firstly, this was a very small study, where the small sample size limited the statistical analyses that could be conducted on the data, as well as the generality and validity of the study. The failure to find relationships could be due to several uncontrolled factors or to the small sample size. Non-tolerance of the actigraphs was a major issue in this study, with several participants having to pull out due to being unable to tolerate the actigraphs. Tactile sensitivity is a major issue for many children with ASD; therefore, asking a child to wear a watch-like device can be difficult for many children. Data collection took place during the summer holidays, which may have affected the availability of families to participate in the research. The absence of a control group is also a limitation of the present study. A control group would have allowed comparisons to be drawn between the groups for each of the variables examined. A final limitation was the lack of fathers who participated in the study, with only three out of the nine families having both mother and father. This made it difficult to compare maternal data with paternal data due to the limited numbers.
The present study raises important points for future research. No correlations were found between subjective and objective measures of sleep, highlighting the lack of reliability of subjective sleep measures, which can overexaggerate sleep problems. There was a lack of relationships found between parent stress, anxiety, depressive symptoms and quality of life and child and parent sleep in the current study; therefore, the factors that affect these variables should be examined in future research. Actigraphy is an emerging and more reliable method of sleep measurement. A multi-method approach to sleep measurement, which allows an examination of different aspects of sleep, should be used in all future sleep research. A replication of this study with a larger sample size and a typically developing control group should be conducted in the future.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
The author has no conflicts of interest to disclose.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all individual participants included in the study. The study protocol was approved by the ethics committee of the participating institution.







