The global coronavirus disease (COVID-19) pandemic poses new challenges to maintaining the safety of healthcare workers (HCWs) and increases occupational stressors. Reference Buselli, Corsi, Veltri, Baldanz, Chiumiento, DelLupo, Marino, Necciar, Caldi, Foddis, Guglielmi and Cristaudo1–Reference Willan, King, Jeffery and Bienz3 Early in the pandemic, contact transmission was considered as critical as droplet transmission, resulting in significant attention on safe doffing and cleaning of potentially contaminated personal protective equipment (PPE), Reference Cao, Qin, Jing, Cheng, Hui, Chunjie and Longjiang4–Reference Oksanen, Enni, Sampo, Veli-Jukka, Jussi, Maija, Lasse and Ahmed6 in part because cross contamination during PPE doffing has been a major and common risk (46%–90%) with other serious communicable diseases. Reference Casanova, Erukunuakpor, Kraft, Mumma, Durso, Ferguson, Gipson, Walsh, Zimring, DuBose and Jacob7–Reference Osei-Bonsu, Masroor, Cooper, Doern, Jefferson, Major, Adamson, Thomas, Lovern, Albert and Stevens12 With a better understanding of disease transmission, contact with potentially contaminated PPE is less critical for severe acute respiratory coronavirus virus 2 (SARS-CoV-2), but it is still important. Real-world factors complicating this process include HCW stress and fatigue, Reference Davey, Lee, Robbins, Randeva and Thake13,Reference Mehta, Machado, Kwizera, Papazian, Moss, Azoulay and Herridge14 high patient volumes and staff turnover, shifting supply-chain availability, and reuse or extended use of items previously considered single use. Reference Peters, Marnie and Butler15,Reference Singh, Naik, Soni and Puri16 In addition, PPE doffing varies among HCWs and is sometimes inadequate Reference Alberto, McCarthy, Hamilton, Shalkevich, Milestone, Izem, Fritzeen, Marsic, Sarcevic, O’Connell and Burd17 or occurs in spaces not designed for these activities and workflow. Reference Kang, O’Donnell, Colaianne, Bircher, Ren and Smith11,Reference Osei-Bonsu, Masroor, Cooper, Doern, Jefferson, Major, Adamson, Thomas, Lovern, Albert and Stevens12
To prevent infection and occupational stress in COVID-19 care, healthcare facilities usually focus on organizational strategies, whereas significantly less attention is directed to the built environment as a resource to improve adherence to safe workflows and behaviors. However, the design of spaces where doffing occurs can help reduce HCWs’ load (cognitive and physical) as well as contamination risks. Reference Wong, Matić, Campiglia, Zimring, Mumma, Kraft, Casanova, Durso, Walsh, Shah and Shane18–Reference Zimring, Matić, Sala, Mumma, Kraft, Casanova, Erukunuakpor, Durso, Walsh, Shah and Jacob20 Also, low-effort changes to existing spaces can make this process easier, safer, and faster. Reference Matić, Humphreys and DuBose21
Although some studies have briefly described how PPE doffing occurs in COVID-19 patient care environments, Reference Cheng, Chen, Xiao, Zhang, Cheng, Zhou, Peng and Liu22–Reference Agarwal, Ranjan, Saraswat, Kasi, Bharadiya, Vikram, Singh, Upadhyay, Baitha, Klanidhi and Chakrawarty25 research showing how design can improve COVID-19 doffing processes is lacking. In this study, we sought to better understand how the built environment of inpatient nursing units can affect HCW safety and efficiency during PPE doffing and considering workflow behaviors in the context of COVID-19 care.
Methods
The study was conducted in 4 phases from April to May 2021 at 3 hospitals of a single healthcare system using the same COVID-19 PPE donning–doffing protocol (Fig. 1). We selected 3 intensive care units (ICUs, sites 1 and 2) and 1 inpatient ward (site 3) designated for COVID-19 care based on availability and the ability to visualize behaviors inside patient rooms via either glass doors or large windows. All research protocols were approved by Institutional Review Boards at Emory University and the Georgia Institute of Technology.

Fig. 1. Overview of four study settings, with sites 2a and 2b being different units in the same hospital. Settings varied in layout and configuration of spaces allocated for doffing.
In phase 1, we scanned the literature to identify previously observed doffing behaviors, errors, and missteps that led to increased risk of self- and cross contamination among HCWs in the context of infectious diseases. Previous studies on COVID-19, Ebola virus disease, and fomite-mediated transmission identified several categories of behaviors that can put HCWs at increased risk: inadequate hand hygiene, Reference Mumma, Durso, Casanova, Erukunuakpor, Kraft, Ray, Shane, Walsh, Shah, Zimring and DuBose9,Reference Cheng, Chen, Xiao, Zhang, Cheng, Zhou, Peng and Liu22,Reference Connors23 excessive reach, Reference Mumma, Durso, Ferguson, Gipson, Casanova, Erukunuakpor, Kraft, Walsh, Zimring, DuBose and Jacob10,Reference Wong, Matić, Campiglia, Zimring, Mumma, Kraft, Casanova, Durso, Walsh, Shah and Shane18 rushing, Reference Muñoz-Leyva and Niazi26,Reference Pyrek27 improper disposal of non-reusable and contaminated items, Reference Wong, Matić, Campiglia, Zimring, Mumma, Kraft, Casanova, Durso, Walsh, Shah and Shane18,Reference Fan, Jiang, Hu, Chen, Xu, Qi, Yin, Gou and Liang24,Reference Pyrek27,Reference Neuwirth, Mattner and Otchwemah28 bumping into items or touching the environment, Reference Wong, Matić, Campiglia, Zimring, Mumma, Kraft, Casanova, Durso, Walsh, Shah and Shane18,Reference Connors23 touching PPE outer surfaces, Reference Cheng, Chen, Xiao, Zhang, Cheng, Zhou, Peng and Liu22,Reference Connors23,Reference Agarwal, Ranjan, Saraswat, Kasi, Bharadiya, Vikram, Singh, Upadhyay, Baitha, Klanidhi and Chakrawarty25–Reference Pyrek27 touching clothes or body under PPE, Reference Connors23,Reference Agarwal, Ranjan, Saraswat, Kasi, Bharadiya, Vikram, Singh, Upadhyay, Baitha, Klanidhi and Chakrawarty25 improper storing and cleaning of reusable PPE, 29 and not disinfecting the environment and items before or after doffing. Reference Connors23,Reference Agarwal, Ranjan, Saraswat, Kasi, Bharadiya, Vikram, Singh, Upadhyay, Baitha, Klanidhi and Chakrawarty25,Reference Neuwirth, Mattner and Otchwemah28 Combining results from the literature scan and interviews with 3 HCWs experienced in COVID-19 care (2 infection preventionists and a critical care nurse), we defined an initial list of survey questions and doffing behaviors to be observed. Adapting a previously used method, Reference Mumma, Durso, Ferguson, Gipson, Casanova, Erukunuakpor, Kraft, Walsh, Zimring, DuBose and Jacob10 we ranked and prioritized these behaviors by their severity index. Ultimately, we pretested observation and survey tools in a pilot study.
In phase 2, a 3-member research team observed HCWs performing PPE donning and doffing during routine patient care using an iPad-based tool kit. Observations lasted ∼1 hour in each unit and were conducted outside patient rooms and through room windows to minimize disruptions to patient care. Observer A recorded the frequency and types of shortlisted behaviors. Observer B recorded the sequence of doffing steps, and observer C documented the physical environment where these behaviors occurred, including the positioning of PPE storage, work surfaces, and supplies.
Following observations, HCWs completed 2 surveys. In survey 1, we assessed the prior experience and perceptions of HCWs regarding challenges during donning and doffing. In survey 2, we used a modified NASA task load index method Reference Hart and Staveland30 and asked HCWs to rate the perceived level of difficulty of doffing tasks using a 7-point scale across 6 workload dimensions: mental demand, physical demand, temporal demand, overall performance, effort, and frustration level.
In Phase 3, we conducted 2 virtual focus groups, each with a nurse and an infection preventionist. Focus groups were used to review and validate observation and survey results, and to identify the most significant safety and efficiency challenges within the doffing process.
For the first 3 phases, we synthesized data from observations, surveys, and focus groups qualitatively using pattern matching. Reference Yin31 Also, 2 researchers independently coded all survey comments and summative statements from focus groups. The overall workload score of doffing tasks was calculated based on individual ratings across workload dimensions (survey 2). We compiled the results from both analyses in a framework summarizing major challenges and HCW preferences in relation to physical elements and environments involved in doffing.
In phase 4, we used this framework to guide a virtual workshop with 9 experts in healthcare facility design, infection prevention, and/or healthcare epidemiology: 3 researchers, 3 architects, 1 biomedical engineer, and 1 infection preventionist. This team of experts focused on opportunities identified in previous study phases to improve the design of doffing spaces. The outcome of this meeting was a set of design goals, guidelines, and strategies to improve HCW safety and efficiency during COVID-19 PPE doffing.
Results
We observed 11 unique individuals conducting 16 PPE donning–doffing events: 14 were performed by nurses, 1 by a physician, and 1 by a respiratory therapist. Doffing procedures varied considerably between sites, and even between individual HCWs in the same site, including differences in the number of doffing steps, the duration of doffing, the techniques used to clean and store PPE, and the frequency and type of hand hygiene. Most doffing tasks took place at or around the patient-room door (Fig. 2). The location of doffing was usually dictated by the placement of PPE supply elements such as mobile carts and wall-mounted PPE caddies, which were typically positioned near the door and outside the patient room. PPE cleaning tasks were always observed outside the room, in the corridor. Based on survey responses from 18 HCWs, doffing PPE was generally not perceived as burdensome after over a year of practice. Nevertheless, all participants rated gown removal as the most demanding task (mean, 4.0; median, 3.5), with hand hygiene being the least demanding (mean, 2.7; median, 1.3). The task with the highest mental demand was cleaning PPE (mean, 3.0; median, 3.0), and the least mentally demanding task was performing hand hygiene (mean, 1.6; median, 1.0).

Fig. 2. Number and location of doffing tasks in each site based on observations (16 donning-doffing events). The color intensity of each circle is proportionate to the number of doffing tasks done at that specific area.
We identified design patterns affecting doffing processes across sites (Tables 1 and 2). Patterns related to the size and layout of doffing spaces, the types of PPE used, and the type and location of PPE furniture and supplies (especially furniture used for storing, cleaning, and drying reusable PPE). All sites located PPE storage next to patient room doors, and most sites did not offer much space to wall-mount the storage. Across sites trash cans were close to the patient room door, and sinks were far from the doffing area, whether inside (∼4.5 m or 15 feet) or outside (>6 m or 20 feet) the patient room. We observed 7 different PPE storage configurations, 3 PPE cleaning station types, 2 methods to hang and dry items after cleaning, and 4 different formats to dispose of PPE after use (Fig. 3). PPE storage and cleaning methods largely depended on whether the items were for single or extended use. For instance, N95 masks were kept in designated containers to be reused, and face shields were hung on wall- or door-mounted hooks to dry after being cleaned. Some PPE types required additional steps during doffing, such as reusable masks made of hard materials (eg, elastomeric half-mask respirators that needed cleaning and drying after use).
Table 1. Design Features Relevant to COVID-19 PPE Doffing Across Sites: Size and Layout of Doffing Spaces

Table 2. Patterns Related to Types of PPE Furniture and Supplies Used in COVID-19 PPE Doffing Spaces

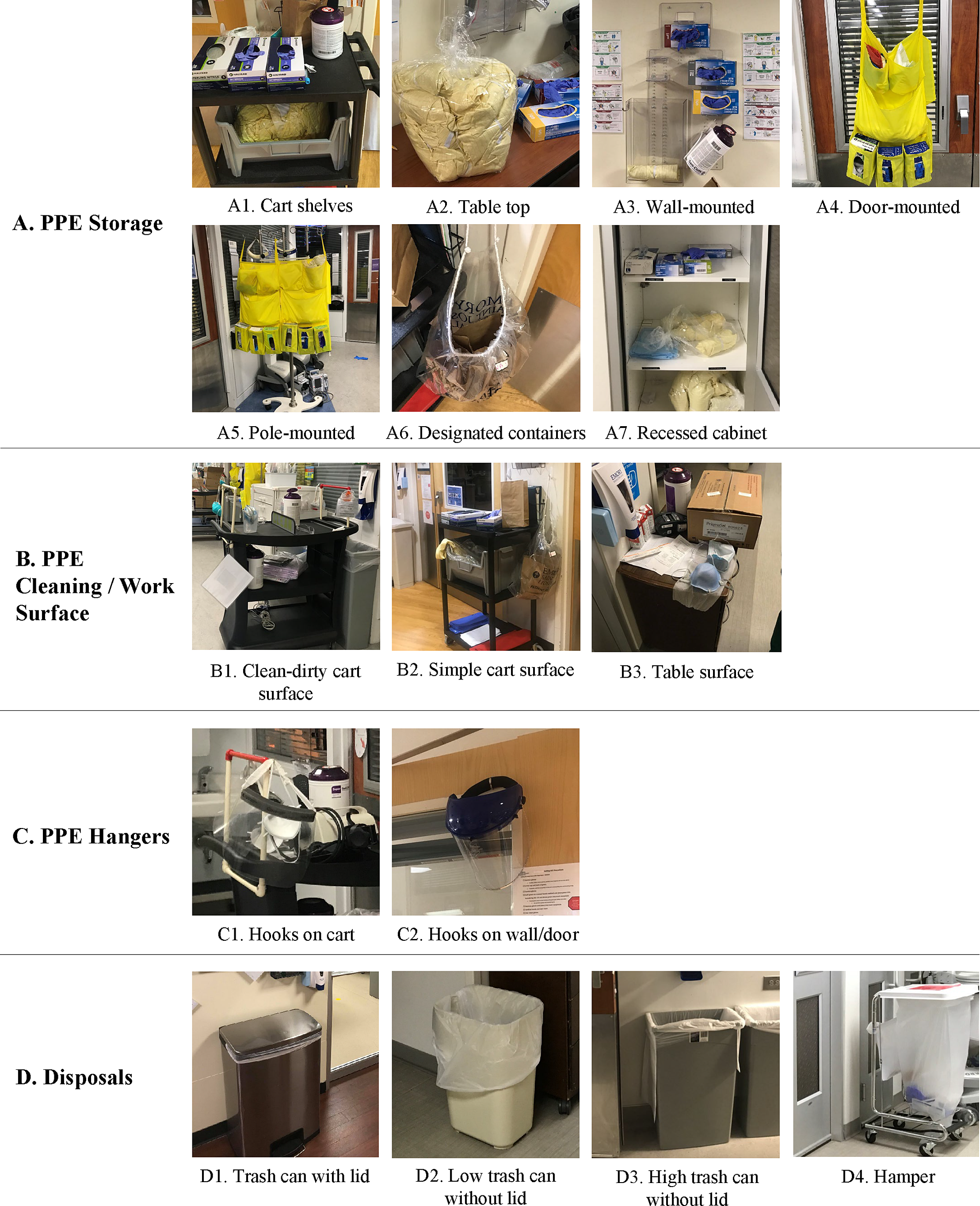
Fig. 3. Different types of PPE storage, work/cleaning surfaces, hangers, and disposals observed across sites: there were various wall-mounted or cart storage and disposal solutions depending on local practices and available wall space and floor space.
Risky behaviors, inefficiencies, and ergonomic issues
According to study participants, risks to contamination during doffing are greater when there is inadequate hand hygiene, inadequate doffing location, inadequate storing or staging of PPE, and touching contaminated items. Hand hygiene lasted <10 seconds during 69% (n = 11) of doffing events observed. Inadequate doffing location was observed once, when an HCW removed their gown at the patient bedside zone (as opposed to near the patient room door). We observed improper PPE storing or staging when HCWs placed reusable masks and eyewear on the dirty-designated side of surfaces after cleaning (eg, the tops of the carts were divided in dirty and clean sides) and when face masks were air drying without proper labeling or packaging. According to an infection preventionist focus-group participant, “Leaving PPE hanging on a cart without being labeled may be a risk because someone else could pick it up.” Touching contaminated PPE and overfilling hampers or trash cans after disposing of gloves and gowns was also observed and identified as “very concerning” from an infection control standpoint.
We also identified process inefficiencies such as staff performing tasks that were unnecessary. HCWs sometimes had to “walk around the unit to find a gown” (respiratory therapist, focus group) or pause their task to retrieve items that should be readily available, such as supplies to clean or dry PPE or a stock of clean gowns. According to an IP focus group participant, “going back and forth to get items” can result in HCW fatigue, which can contribute to “missteps during doffing.” Another inefficiency was the waste of both PPE and valuable patient-care space. According to a nurse, PPE was wasted more often when gloves were stored in vertical caddies (compared to tabletops), which often led to gloves falling on the floor during retrieval. On the other hand, corridor space occupied by PPE storage was considered a waste in cluttered units.
Although rare, we noted behaviors such as excessive reach or hindered access and visibility. We observed a few HCWs stretching to reach a hand-sanitizer dispenser or throwing PPE to trash cans placed far away from the doffing area. Focus-group participants and survey respondents highlighted difficulties with the suboptimal height of wall-mounted PPE storage and supplies. Infection preventionist focus-group participants reported challenges with access and visibility of “recessed cabinets [being] sometimes far and out of sight” and the “hand sanitizer too low, out of sight.” According to an infection preventionist, “Having it in sight helps to remind [me] of hand hygiene,” and a hand sanitizer located at “normal height, not obstructed, would be optimal for the eye-catching reminder.” A nurse participant mentioned that “the [door-mounted] PPE storage blocks the glass in the patient room door.”
Challenging and supportive environmental qualities
The inconsistency and variability in the layout of doffing areas were reported as challenging by study participants, considering that HCWs often work at >1 unit at the same hospital or healthcare organization. Study subjects also showed dissatisfaction with insufficient unit areas to allow for PPE storage, or inadequate PPE storage design. One respiratory therapist expressed the following needs: “something more fit for PPE,” “different PPE stations for different types of units,” “better wall-mounted PPE stations,” and “better receptacles to put the gown in.” Additionally, infection preventionists reported that “door-mounted caddies and clean/dirty separators in carts’ surfaces can be challenging to clean.” One participant noted their preference for “the wall-mounted PPE acrylic unit because it can be cleaned.”
On the other hand, focus groups conveyed aspects of the built environment that can support doffing in the context of general patient care, such as accessibility, no-touch, cleanability, and flexibility. According to an infection preventionist and a nurse, having easy access and proximity to a sink is preferred. An infection preventionist noted that easy access to PPE and cleaning supplies facilitates HCW tasks. Infection preventionists also mentioned easy visual access to reminders of expected and safe behaviors as supportive of keeping storage units stocked with sufficient amounts of PPE and avoiding cross contamination by touch (eg, no-touch reminders on trash cans or hampers and cleaning reminders on tabletops). Infection preventionists noted that the use of hooks was helpful to air dry PPE elements while protecting them from physically touching other potentially contaminated items. Finally, a spacious PPE storage that is wall-mounted and has designated clean and dirty areas was positively perceived. In contrast, mobile PPE storage (on wheels) was perceived as advantageous for being flexible and easy to move when not needed.
Design goals, guidelines and strategies for COVID-19 PPE doffing
Based on these findings, experts in the design-focused workshop discussing design opportunities to improve PPE doffing spaces (study phase 4) defined several design goals for doffing areas: minimize HCW contact with the environment; reduce HCW physical and cognitive load; improve accessibility to PPE; and encourage doffing process standardization (Fig. 4). Several design guidelines addressing these goals were also synthesized from the discussion: provide environmental cues; minimize physical obstructions; and design standardized and flexible doffing spaces. These ideas were then translated into concrete design strategies such as set and demarcate PPE doffing locations and using transparent materials for PPE storage.

Fig. 4. Summary of design goals, guidelines, and strategies for PPE doffing design.
Overall, some general themes emerged: (1) environmental implications of supply and staff shortages in healthcare facilities; (2) the need for clearly defined and organized doffing spaces in intensive and acute care settings; (3) the dilemma between using horizontal versus vertical space to store and clean PPE; and (4) the need to minimize touching surfaces and leverage the built environment to encourage and optimize hand hygiene.
Discussion
In our examination of doffing spaces used a year into the COVID-19 pandemic, healthcare facilities had developed improvised processes based on their available spaces to accommodate unexpected patient surges and an intensive routine of PPE donning–doffing imposed by COVID-19 care needs. Our study demonstrates how environmental features can affect HCW safety and occupational well-being in this context. Unlike the Ebola outbreak, where a small group of HCWs cared for fewer patients and doffed PPE in a dedicated space following a choreographed and supervised process, Reference Matić, Humphreys and DuBose32 our study showed that HCWs care for large volumes of COVID-19 patients in a short amount of time in areas previously designed for inpatient care, with significant variations in the PPE doffing process across the settings observed. Our findings highlight the importance of intentional and attentive design of areas around the patient room door, where most doffing tasks occur. We observed that spaces such as corridors were not sufficiently flexible to accommodate dedicated areas for doffing tasks and the various PPE supply stations involved.
Although standardizing sequences of PPE doffing tasks within institutions can be challenging, the size and layout of corridors and door areas should be defined and organized to support the general sequence of PPE doffing behaviors and to prevent clutter. This strategy therefore contributes to process consistency, helping reduce HCW cognitive load and potentially increasing compliance to safe and efficient behaviors. Our findings also underscore the importance of adequate location and ergonomic design of PPE storage and work areas in the units that reuse PPE. In turn, these factors affect the utilization and occupancy of corridor areas where critical healthcare workflows coexist.
Some of the behaviors identified in this study echoed the recent literature on COVID-19 PPE doffing Reference Connors23,Reference Agarwal, Ranjan, Saraswat, Kasi, Bharadiya, Vikram, Singh, Upadhyay, Baitha, Klanidhi and Chakrawarty25 and general findings of poor HCW compliance with adequate hand hygiene protocols. Reference Sands and Aunger33 We recognized many challenges associated with reusing PPE, such as PPE cleaning and drying that may not be needed for lower volumes of patients. We also noted a lack of designated personnel to supervise doffing (trained observers) or restock supplies, which may not be the case in other settings nor essential in safe care delivery when staffing is limited. Nevertheless, healthcare facilities should continue to plan for a pandemic-type scenario with a limited supply chain and staff constraints.
Design considerations regarding PPE supply, storing, and cleaning stations include whether they should be vertical or horizontal; fixed or mobile; made of porous, impermeable, transparent, or opaque materials; and separated into clean and dirty zones. For instance, wall-mounted vertical PPE storage units saved space. However, this option was not always available due to limited wall or door space around patient rooms. Vertical PPE often presented challenges such as ergonomics (inadequate mounting height), cleaning (hard-to-clean materials such as fabric), and limited visibility or physical access. Alternatively, horizontal surfaces often occupy valuable corridor areas and may impact doffing duration, with increased walking between tasks. In turn, horizontal surfaces on wheels (eg, mobile caddies) with clearly designated clean and dirty zones may encourage PPE cleaning and offer more flexibility for HCWs to stage frequently used patient-care items.
The design-focused workshop with experts provided opportunities for multidisciplinary dialogue and helped identify low-effort and low-cost strategies that can improve safety and efficiency and mitigate contamination risks. Coupled with insights provided by focus group participants, no-touch attributes were recommended to minimize cross contamination and the need for additional hand hygiene after touching doorknobs or handrails. Associated design and technology strategies could automate door opening, increase the availability of mobile sinks, and improve the visibility and ergonomics of hand hygiene stations to improve hand hygiene compliance. Other strategies may require more significant resources, like standardizing spaces to facilitate doffing consistency, and changing the configuration of corridor areas to reduce clutter.
This study had several limitations. We assessed inpatient settings at 4 sites, focusing on ICUs and acute-care units more than a year after the beginning of the pandemic, when there was still a significant focus on contact as a major mode of transmission. With changes in the understanding of transmission dynamics, including the importance of the airborne route, some of these processes will likely change in the future, though many of the design principles will still apply. Despite our modest sample size and the lack of generalizability of our qualitative results, we recorded considerable variations in the process, but we may not have captured all events because data collection and observations took place in corridor areas.
Our results emphasize how the built environment can be relevant during PPE doffing in the context of COVID-19 care in inpatient settings, where the design of doffing spaces around patient room doors may help reduce risks of cross contamination and occupational stress. To increase the strength of our findings, future research should operationalize and test our suggested design guidelines and strategies using an interdisciplinary approach that focuses on measuring actual improvements in PPE doffing, especially in terms of perceived HCW workload.
Acknowledgments
We thank all healthcare workers who participated in this study and facilities’ departments at study sites for providing architectural drawings. We thank our collaborators: Joel Mumma, Gabrielle Campiglia, Amanda Grindle and Anjali Joseph. We also thank Sharvari Tamhane, Fatemeh Motamed Rastegar and Yousef Bushehri for their assistance in data collectionand data visualization.
Financial Support
This work was supported by the Prevention Epicenters Program funded by the US Centers for Disease Control and Prevention (grant no. 6U01CK000554).
Conflicts of Interest
All authors report no conflicts of interest relevant to this report.









