To the Editor—The epidemiology of severe acute respiratory coronavirus virus 2 (SARS-CoV-2) variants has changed since the original outbreak strain to the SARS-CoV-2 (omicron) variant of concern. 1 Compared to previous variants, the (omicron) variant is more transmittable but less virulent. Reference Wolter, Jassat and Walaza2 During the SARS-CoV-2 (omicron)-variant wave in Thailand, the number of coronavirus disease 2019 (COVID-19) cases has been increasing exponentially as has the number of infected healthcare personnel (HCP), despite most HCP having received 3 or more COVID-19 vaccine doses. 3 These HCP COVID-19 cases have led to staff shortages and have added to the workload of healthcare personnel (HCP). Recently, international guidelines have recommended shortening the duration of quarantine to 7 days for HCP with high-risk exposure if the HCP has a negative reverse-transcription polymerase chain reaction (RT-PCR) or antigen-based diagnostic test administered by qualified personnel at day 7. 4,5 We report the feasibility and safety of a reduced quarantine duration for HCP with high-risk exposure to patients with COVID-19 in a Thai hospital.
We prospectively evaluated the feasibility and safety of reduced quarantine duration for HCP with high-risk exposure to COVID-19 in Thammasat University Hospital (Pathum Thani, Thailand). HCP with high-risk exposure (HR-HCP) were defined as having close contact (≤1 m for >15 minutes) with a patient with COVID-19 without the use of appropriate PPE. HCP were expected to comply with the hospital infection prevention and control (IPC) policy including mask wearing and maintaining physical distancing while eating or drinking and while attending all hospital activities. The quarantine policy for HCP with high-risk exposures during the SARS-CoV-2 α (alpha)-variant and δ (delta)-variant waves included quarantine for 14 days with RT-PCR tests on days 0–3, days 5–7, and days 13–14 after exposure. During the SARS-CoV-2 (omicron) wave, the hospital policy remained the same except that the quarantine for was reduced to 5 days, and when returning to work, HCP were required to strictly comply with hospital IPC policy for another 5 days. Furthermore, all HCP were required to report any symptoms and to undergo RT-PCR testing for SARS-CoV-2 on day 5 prior to returning to work and again on day 10.
The following HCP data were collected prospectively by the occupational health team: characteristics, underlying disease, working place, source of risk exposure, COVID-19 vaccination history, hospital transmission, and compliance with the hospital IPC policy. The primary outcome of this study was to evaluate hospital transmission among HR-HCP prior to and after the change in the quarantine policy. Hospital transmission was considered as exposed HCP who transmitted COVID-19 to patients and/or to other HCP both prior to and after the quarantine policy was implemented. The secondary outcome included compliance with quarantine policy including use of double masks, compliance with physical distancing, and the isolation policy. We used χ Reference Wolter, Jassat and Walaza2 tests to compare categorical variables. Independent t tests were used for continuous data. All P values were 2-tailed, and P < .05 was considered statistically significant.
From January 2021 to February 2022, 636 HCP had high-risk exposures: 440 during SARS-CoV-2 non-(omicron) waves (ie, α- and δ-variant waves) and 196 during the (omicron) wave. The median age of exposed HCP was 30 years (range, 26–36). Demographics and characteristics of exposed HCP are summarized in Table 1. Most HCP were female and had no underlying disease. We detected no significant differences between exposed HCP during SARS-CoV-2 non-(omicron) waves versus the (omicron) wave in terms of characteristics, type of contact, and working unit. During the entire study period, 173 (27%) of 636 transmission events occurred from exposed HCP to other HCP. Of 440 transmissions, 120 (27.3%) occurred during SARS-CoV-2 non-(omicron) waves and 53 (27%) of 196 transmissions occurred during the (omicron) wave (Table 1). All HCP developed infection prior to quarantine due to the delay in recognition of the index case. Notably, 143 (73%) of 196 exposed HCP tested negative on day 5 and returned to work during the SARS-CoV-2 (omicron) wave. No in-hospital transmission occurred after the entire follow-up period, and all exposed HCP tested negative on day 10. All HR-HCP were fully compliant with the hospital quarantine policy (Table 1). Also, vaccination among exposed HCP increased from the SARS-CoV-2 non-(omicron) periods to the (omicron) period.
Table 1. Characteristics of HR-HCP and COVID-19 Hospital Transmission Stratified by SARS-CoV-2 Variant
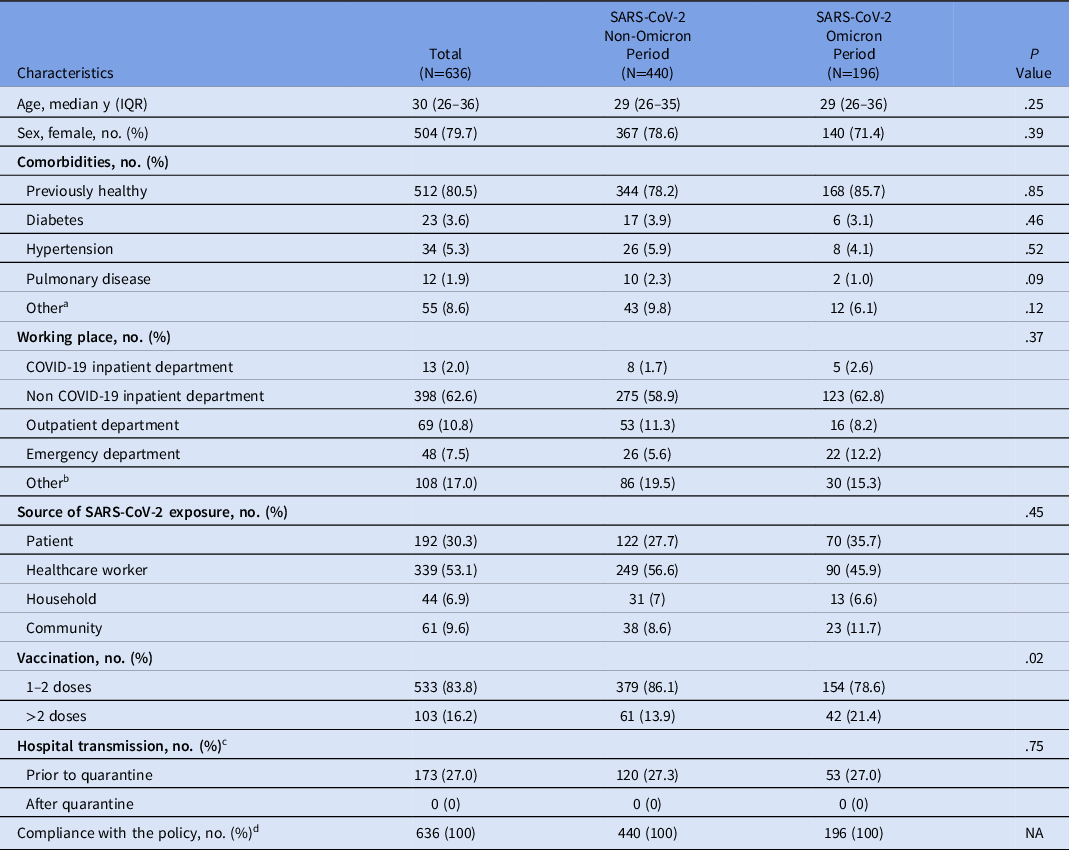
Note. HR-HCP, high-risk healthcare personnel; IQR, interquartile range; n, number; NA, not applicable.
a Dyslipidemia, thyroid disease, allergic rhinitis, chronic hepatitis B infection, gastroesophageal reflux disease, obstructive sleep apnea, systemic lupus erythematosus.
b Nursing department, physical therapy department, planning and finance department, medical supplies department.
c Transmission to patients and/or to other HCP.
d Compliance monitoring was performed by an infection control nurse for hand hygiene and use of double mask. Compliance to physical distancing was assessed by HCP self-report survey by the infection control division.
Our findings have demonstrated that the reduced quarantine time for HCP exposed to COVID-19 was safe and effective in preventing in-hospital transmission from HCP with high-risk exposure to patients and/or to other HCP and this may, in part, have been due to increased vaccinations among our HCP. Importantly, our policy was implemented without concerns by HR-HCP. Notably, of 623 exposed HCP, 173 (27%) developed COVID-19 prior to recognition of their exposure. This proportion was less than the pooled infection rate (51.7%) reported by a meta-analysis study of infection among frontline HCP during non-(omicron) waves. Reference Gholami, Fawad and Shadan6 The fact that HCP acquired COVID-19 prior to quarantine emphasizes that all HCP should be considered at risk for exposure and must strictly comply with IPC policies for COVID-19. Lastly, despite increases in COVID-19 vaccination, it is vital that HR-HCP adhere to hospital IPC policies.
Our study had several limitations. First, the data were collected from a single center, which may limit the generalizability of our findings. Second, we did not obtain the genotype of the variant; instead, we assumed the variant involved based on Thai Nation Institute of Health database. Reference Gholami, Fawad and Shadan6 Third, our sample size was relatively small. Despite these limitations, our data have demonstrated that the reduced quarantine time was safe and effective in Thai HR-HCP who generally received >3 vaccine doses. Additional studies are needed to evaluate an appropriate duration of quarantine for SARS-CoV-2–exposed HCP given the high rate of vaccination among HCP and that COVID-19 is now an endemic disease.
Acknowledgments
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.




