To the Editor—The emergence of carbapenemase-producing Enterobacteriaceae (CPE) is an important public health problem because the treatment of CPE is difficult; few options remain available for clinical use.Reference Nordmann, Cuzon and Naas 1 The New Delhi metallo-β-lactamase (NDM-1) is the most common class B carbapenemase among Enterobacteriaceae, and it has been detected increasingly frequently in several countries,Reference Johnson and Woodford 2 including Brazil.Reference Carvalho-Assef, Pereira and Albano 3 – Reference Carvalho-Assef, Pereira and Albano 8 The aim of this study was to evaluate the characteristics of transformants obtained from NDM-1–production in different bacterial species of Enterobacteriaceae identified in southern Brazil.
Isolates were selected from a surveillance study that evaluated Enterobacteriaceae with reduced susceptibility to carbapenems in Rio Grande do Sul State, southern Brazil. A total of 9 clinical NDM-producing isolates from 4 hospitals were selected for this study: 3 Klebsiella oxytoca, 2 Enterobacter clocae complex, 1 Klebsiella pneumoniae, 1 Morganella morganii, 1 Escherichia coli, and 1 Citrobacter freundii. These isolates were initially identified by the VITEK2 system (bioMèrieux, Marcy-l'Étoile, France) and confirmed by 16S rRNA sequencing. The bla NDM gene was detected by a multiplex real-time polymerase chain reaction (PCR), which also included primers for the bla KPC, bla VIM, bla GES, bla NDM, bla OXA-48, and bla IMP genes.Reference Quiles, Rocchetti and Fehlberg 9 The presence of bla NDM was further confirmed by conventional PCR, and the amplicons were purified and sequenced using a BigDye Terminator Kit (version 3.1, Thermo Fisher Scientific, Waltham, MA) and an ABI 3500 Genetic Analyzer (Applied Biosystems, Foster City, CA). GenBank was used to access the bla NDM sequences deposited to date, and the BioEdit program was used to compare similarities between sequences. The plasmids were extracted by alkaline lysis and were transformed into E. coli TOP10 electrocompetent cells by electroporation. Transformants were selected on Luria-Bertani agar containing 2 µg/mL ceftazidime. The transformants were evaluated for the bla NDM gene by conventional PCR with specific primers. The minimum inhibitory concentrations (MICs) of imipenem, meropenem, doripenem, piperacillin/tazobactam, ceftriaxone, cefepime, aztreonam, gentamicin, amikacin, polymyxin, and tigecycline were assessed by Etest (bioMèrieux, Marcy-l'Étoile, France). The modified Hodge test (MHT) and the combination-disc test (ie, meropenem and imipenem with and without ethylenediaminetetraacetic acid [EDTA]) were used as phenotypic methods for carbapenemase and metallo-β-lactamase detection, respectively.
It was possible to obtain transformants from all 9 clinical isolates. The transformants obtained from each isolate presented higher MICs than the original E. coli TOP10 for β-lactams. In fact, the MICs of transformants were similar to those of the donor NDM-positive clinical isolates, which showed high levels of resistance (Table 1).
TABLE 1 Phenotypic Characterization of Isolates and Transformants Obtained From NDM-1–Producers in Brazil
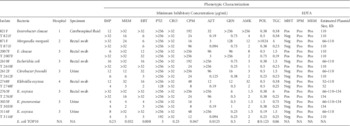
NOTE. T, transformant; MHT, modified Hodge test; EDTA, ethylenediaminetetraacetic acid; Neg, negative; Pos, positive; NA, not applicable; IMP, imipenem; MEM, meropenem; ERT, ertapenem; PTZ, piperacillin/tazobactam; CRO, ceftriaxone; CPM, cefepime; AZT, aztreonam; GEN, gentamicin; AMK, amikacin; POL, polymyxin B; TGC, tigecycline.
Notably, the combined-disc assay with EDTA proved to be positive (ie, EDTA inhibited the carbapenem activity) for all NDM-1–producing clinical isolates and transformants.
Plasmid analysis indicated that most transformants contained a 110-kb plasmid: 2 from the E. clocae complex and 1 each from K. oxytoca, M. morganii, E. coli, and C. freundii. However, it was also possible to identify the presence of a 52-kb plasmid in a transformant from K. oxytoca, a 154-kb plasmid from a K. oxytoca, and a K. pneumoniae (Table 1).
The in vitro transfer of plasmids containing the bla NDM-1 gene in our study confirms that this carbapenemase gene can be readily mobilized among different species of Enterobacteriaceae. Moreover, E. coli TOP10 transformants containing the bla NDM-1 gene presented similar characteristics of the original clinical isolate, with increased MIC to β-lactams and positive results of the combined-disc assay with EDTA. Although a plasmid of the same molecular weight (~110 bp) was observed in 6 of 9 transformants, the identification of other plasmids (~52 bp and ~154 bp) suggests that the bla NDM-1 gene is located in different mobile genetic elements.
Molecular investigations involving both the characterization of isolates of NDM-positive bacteria and the characterization of the plasmids containing bla NDM-1 genes reveal a highly complex picture. The plasmids encoding NDM also appear highly heterogeneous based on molecular size, incompatibility type, and linked antibiotic-resistance genes.Reference Johnson and Woodford 2 Moreover, our data support the findings from Brazil in which a variety of plasmids were found. The gene bla NDM-1 was identified on plasmid with an estimated size of 420–490 kb in Enterobacter hormaechei.Reference Carvalho-Assef, Pereira and Albano 8 In Enterobacter cloacae, Providencia rettgeri, and Klebsiella pneumoniae, the plasmid was reported to be ~230 kb.Reference Quiles, Rocchetti and Fehlberg 9 Escherichia coli and Enterobacter hormaechei had plasmid sizes of 70 kb and 90 kb, respectively.Reference Campos, da Silva and Dos Santos 10 The plasmid size in Acinetobacter baumannii was 100 kb.Reference Pillonetto, Arend and Vespero 7
In summary, the results of this study demonstrate the variety of plasmids observed in the transformants and suggests that strains producing bla NDM-1 harbor plasmids of different sizes, demonstrating the plasticity of these mobile genetic elements. These findings highlight the need for continuous monitoring of the presence of carbapenemases. Our results contribute to the understanding of carbapenem resistance in Enterobacteriaceae and to the molecular characterization of NDM-1–producing isolates in Brazil.
ACKNOWLEDGMENTS
Financial support: CAPES Foundation, Ministry of Education of Brazil, Brasília, Brazil. FIPE/HCPA (Research and Events Support Fund at Hospital de Clínicas de Porto Alegre). A.L.B. is a research fellow from the CNPq, Ministry of Science and Technology, Brazil (grant no. 458489/2014-0).
Potential conflicts of interest: All authors report no conflicts of interest relevant to this article.



