To the Editor—Much is still being discovered about coronavirus disease 2019 (COVID-19). Although originally described as viral pneumonia, reports of nonrespiratory manifestations of COVID-19 are increasing, including gastrointestinal, ocular, cardiac, and neurologic presentations. Reference Edirappuli and Venkatesh1–Reference Small and Beatty3 Hospitals restrict visitors with acute respiratory infections (ARIs), isolate and test all ARI patients for severe acute respiratory coronavirus virus 2 (SARS-CoV-2), and provide staff with full personal protective equipment when managing ARI patients. Reference Klompas4 Concerns about how to titrate infection control measures for asymptomatic, presymptomatic, and atypical infections Reference Arons, Hatfield and Reddy5 are heightened by fears of subsequent waves of COVID-19 from easing lockdowns. Transmission most likely occurs via droplets from infected individuals with respiratory symptoms, but it remains unclear whether SARS-CoV-2 is just as transmissible by patients who do not have respiratory symptoms.
Since January 23, 2020, the 1,600-bed Tan Tock Seng Hospital, co-located with the 330-bed National Centre for Infectious Diseases (NCID), has managed >9,000 COVID-19 patients. Reference Soh6 Contact tracing was immediately performed for every COVID-19 patient not managed at designated COVID-19 areas (fever zones) in the emergency department or clinic, or not pre-emptively admitted to an airborne infection isolation room (AIIR). In fever zones, all staff donned N95 respirators, gowns, gloves, and eye protection, while patients and visitors wore surgical masks. In non–fever zones, staff, patients, and visitors wore surgical masks and observed standard precautions.
Between January 23, 2020, and July 25, 2020, the hospital managed 5 COVID-19 patients without ARI symptoms who presented with gastrointestinal symptoms (n = 2), upper-limb swelling (n = 1), fever and muscle pain (n = 1), and anxiety symptoms (n = 1) (Table 1).
Table 1. Characteristics of Patients and the Exposed Contacts
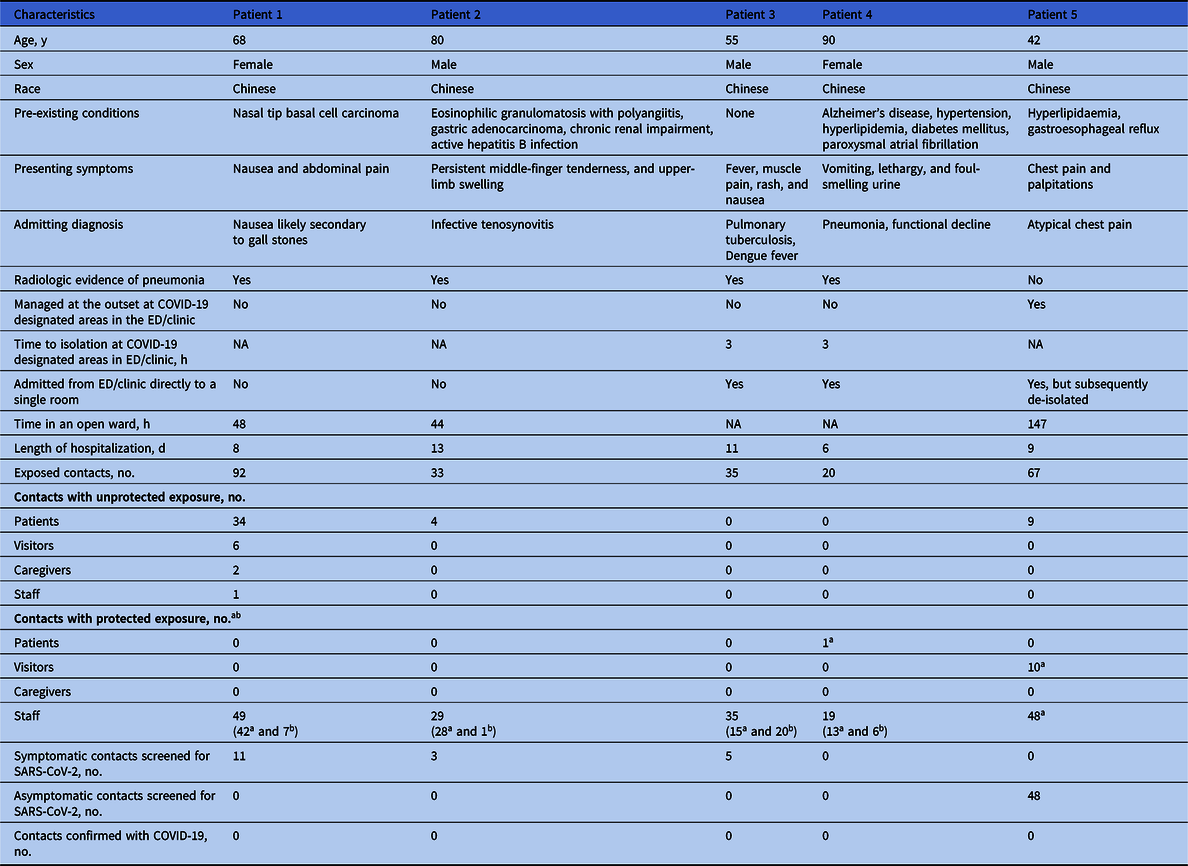
Note. ED, emergency department.
a Surgical mask.
b N95 respirator, gown, gloves, eye protection.
Patient 1
A 68-year-old woman presented to the emergency department non–fever zone on February 27, 2020, with a 2-week history of epigastric pain and nausea without fever or respiratory symptoms. She was admitted to a 5-bed cubicle in a general ward. On February 28, an abdominal/pelvic computed tomography scan revealed ground-glass changes in her bilateral lower lungs. She was immediately transferred to a single-bed room. SARS-CoV-2 was detected on the second nasopharyngeal swab taken on March 1. She was transferred to an AIIR, recovered uneventfully, and was discharged on March 5.
We identified 92 contacts (Table 1). Among them, 8 were inpatients who were moved to single-bed rooms. One staff member who had unprotected close contact developed ARI symptoms on March 1 and was admitted to the NCID, but 2 nasopharyngeal swabs collected 24 hours apart were negative for SARS-CoV-2. Moreover, 3 close patient contacts and a caregiver developed ARI symptoms, as well as another close patient contact whose chest x-ray showed worsening of air-space changes. They were screened for SARS-CoV-2, and the virus was not detected in ≥2 nasopharyngeal swabs taken 24 hours apart in these contacts. Also, 4 casual patient contacts and a staff member with protected exposure who became symptomatic also screened negative for SARS-CoV-2.
Patient 2
On March 20, 2020, an 80-year-old Chinese man with multiple comorbidities was admitted to a 5-bed cubicle from the rheumatology clinic for persistent left middle-finger tenderness and upper-limb swelling. A chest x-ray showed resolving right-lower-zone pneumonia. He had a fever (38.2°C) on March 22 and was transferred to a single-bed room. SARS-CoV-2 was detected on the nasal swab taken on the same day. He was transferred to an AIIR and was discharged on April 1 after recovering. He never developed respiratory symptoms.
We identified 33 contacts. All patient contacts remained asymptomatic, and 3 symptomatic staff contacts tested negative for SARS-CoV-2.
Patient 3
A 55-year-old Chinese man presented to the emergency department non–fever zone on March 24, 2020, with a 3-week history of intermittent fever, rash, nausea, and lethargy. The chest x-ray suggested an atypical infection or pulmonary tuberculosis. A Dengue Duo test showed IgM and IgG positivity. He was admitted to a single-bed room. SARS-CoV-2 was detected in the nasal swab taken on the same day, and he was transferred to an AIIR. Tuberculosis was ruled out by negative acid-fast bacilli smears and cultures. He did not develop any respiratory symptoms and was discharged on April 3 after recovering.
We identified 35 contacts, all staff. Among them, 5 developed symptoms but tested negative for SARS-CoV-2.
Patient 4
On April 20, 2020, a 90-year-old Chinese-woman with multiple comorbidities presented to the emergency department non–fever zone with a 1-day history of vomiting, lethargy, and foul-smelling urine. She had no fever or respiratory symptoms, but a chest x-ray revealed left-lower-zone air-space opacities and pleural effusion. She was admitted to a single-bed room. SARS-CoV-2 was detected on the second sample. She was immediately transferred to an AIIR and was discharged on April 25 after recovering. All 20 contacts remained asymptomatic until 14 days after exposure.
Patient 5
A 42-year-old Chinese man, a resident of a dormitory with COVID-19 transmission, presented with chest pain and palpitations on June 16, 2020. He was admitted to an AIIR but was transferred to a 5-bed cubicle for treatment of an anxiety disorder after testing negative for SARS-CoV-2. The day after his discharge on June 22, he was screened for SARS-CoV-2 in preparation for China travel and tested positive.
Of 3 in-hospital patient contacts, 1 was detected with SARS-CoV-2 on June 25. This patient had been admitted for congestive cardiac failure and suspected pneumonia. This patient contact and patient 5 had reactive SARS-CoV-2 serological tests taken on June 27 and 28, respectively; thus, it was improbable that the patient contact acquired COVID-19 from patient 5 while receiving care in the same cubicle.
In conclusion, we have reported 5 patients not initially suspected with COVID-19 and thus not managed at COVID-19–designated areas or AIIRs. In total, 247 contacts were identified from the hospital’s patient and visitor registration systems, staff rosters, electronic medical records, and closed-circuit television. Also, 56 contacts with unprotected exposure were quarantined or placed under phone surveillance for 14 days after exposure. Finally, 19 symptomatic contacts and 48 asymptomatic staff contacts were tested for SARS-CoV-2; none were positive for the virus.
Because the same vigilance for ARI patients cannot realistically be implemented for the smaller proportion of patients with atypical symptoms, the following measures are crucial for preventing nosocomial transmission of SARS-CoV-2: a robust hospital system with risk-based personal protective equipment, staff sickness surveillance, Reference Htun, Lim and Kyaw7 and rapid identification of COVID-19 patients with immediate contact tracing and management.
Acknowledgments
We would like to thank the staff members of the emergency department, clinics, general wards, Department of Clinical Epidemiology, Department of Infection Prevention and Control, and Occupational Health Clinic, whose efforts in contact tracing and management prevented any nosocomial transmission.
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.




