Impact statement
This research provides valuable insights into treatment-seeking behavior and barriers to seeking treatment for depressive symptoms and hazardous drinking in a resource-limited setting. The findings highlight the significant treatment gap for individuals with depressive symptoms and hazardous drinking. This low treatment-seeking behavior emphasizes the urgent need to improve both the demand for mental health treatment and the availability of mental health services in the studied population. Furthermore, we identified important preferences and sources of treatment for depressive symptoms. Both healthcare and non-healthcare settings were reported as valuable sources of treatment, with religious places being particularly helpful for almost 40% of treatment seekers. These findings suggest that incorporating mental health services into existing religious and traditional pathways could enhance treatment accessibility and coverage. The study also sheds light on the barriers hindering treatment-seeking behavior. Attitudinal and stigma-related barriers were identified as the top obstacles to seeking treatment from healthcare settings. These barriers were even more prevalent than structural barriers such as limited resources and financial costs. This highlights the crucial role of addressing mental health literacy, reducing stigma, and increasing public awareness and acceptance of mental health services to promote treatment-seeking behavior. The implications of this study extend beyond the study population, as the findings are relevant to other low-income settings facing similar challenges in mental health services. By addressing the identified barriers and promoting a wider range of treatment options, including religious and traditional healers, mental health services coverage and utilization can be increased, reducing the treatment gap and improving the well-being of individuals with depressive symptoms and hazardous drinking.
Background
Mental disorders are among the leading contributors of substantial health and economic burden worldwide (Arias et al., Reference Arias, Saxena and Verguet2022; GBD 2019 Mental Disorders Collaborators, 2022). Pre-COVID-19 pandemic in 2019, one in eight (970 million) people worldwide were living with mental disorders (GBD 2019 Mental Disorders Collaborators, 2022). Depression was the second most prevalent mental disorder, causing the largest proportion (37.3%) of mental disorder disability-adjusted life years (DALYs), with a 25% worldwide increase due to the early COVID-19 pandemic (GBD 2019 Mental Disorders Collaborators, 2022; WHO, 2022a). Similarly, alcohol use disorder was the most prevalent substance use disorder in the world in 2019 (Castaldelli-Maia and Bhugra, Reference Castaldelli-Maia and Bhugra2022), resulting in 3 million deaths every year (WHO, 2019). In addition to the health burden, poor mental health is projected to cost the world economy approximately $6 trillion by 2030 (Bloom et al., Reference Bloom, Cafiero, Jané-Llopis, Abrahams-Gessel, Bloom, Fathima, Feigl, Gaziano, Hamandi and Mowafi2012; The Lancet Global Health, 2020).
Lower- and middle-income countries (LIMCs) were estimated to bear 82% of people with mental disorders and 35% of the cost of poor mental health (Bloom et al., Reference Bloom, Cafiero, Jané-Llopis, Abrahams-Gessel, Bloom, Fathima, Feigl, Gaziano, Hamandi and Mowafi2012; The Lancet Global Health, 2020; GBD 2019 Mental Disorders Collaborators, 2022; WHO, 2022b). For instance, Sub-Saharan Africa had the highest prevalence of depressive disorders in the global burden of disease estimate (GBD 2019 Mental Disorders Collaborators, 2022), and the economic loss due to mental disorders in East Africa reached 4% of the gross domestic product (Arias et al., Reference Arias, Saxena and Verguet2022). In Ethiopia, mental illness, such as depression is the leading cause of years lived with disability (GBD 2019 Ethiopia Collaborators, 2022). The prevalence of depression ranged from 6.4% to 11.5% in Ethiopia (Bitew, Reference Bitew2014; Rathod et al., Reference Rathod, De Silva, Ssebunnya, Breuer, Murhar, Luitel, Medhin, Kigozi, Shidhaye, Fekadu, Jordans, Patel, Tomlinson and Lund2016). Hazardous alcohol use is also common in Ethiopia where the prevalence reached 8.9%–13.9% (Ayano et al., Reference Ayano, Yohannis, Abraha and Duko2019; Zewdu et al., Reference Zewdu, Hanlon, Fekadu, Medhin and Teferra2019).
Effective treatment options for mental illnesses exist. Pharmacological, psychosocial and community-based interventions are effective in treating mental disorders, including depression and alcohol use disorder in both high-income and low-income settings (Patel et al., Reference Patel, Araya, Chatterjee, Chisholm, Cohen, De Silva, Hosman, McGuire, Rojas and van Ommeren2007). Antidepressants (Cipriani et al., Reference Cipriani, Furukawa, Salanti, Chaimani, Atkinson, Ogawa, Leucht, Ruhe, Turner, Higgins, Egger, Takeshima, Hayasaka, Imai, Shinohara, Tajika, Ioannidis and Geddes2018), psychological interventions including cognitive behavioral therapy (Ijaz et al., Reference Ijaz, Davies, Williams, Kessler, Lewis and Wiles2018), and internet-based behavioral interventions (Karyotaki et al., Reference Karyotaki, Efthimiou, Miguel, FMg, Furukawa and Cuijpers2021) or a combination of them (Malhi and Mann, Reference Malhi and Mann2018; Cuijpers et al., Reference Cuijpers, Noma, Karyotaki, Vinkers, Cipriani and Furukawa2020) are effective in treating depression. A randomized controlled trial conducted in Zimbabwe demonstrated that problem-solving therapy, delivered by lay health workers, improved symptoms of common mental disorders (Chibanda et al., Reference Chibanda, Weiss, Verhey, Simms, Munjoma, Rusakaniko, Chingono, Munetsi, Bere, Manda, Abas and Araya2016). Likewise, a community-based rehabilitation intervention in Ethiopia, administered by lay health workers combined with facility-based care, has been demonstrated effective in reducing disability in patients with schizophrenia (Asher et al., Reference Asher, Birhane, Weiss, Medhin, Selamu, Patel, De Silva, Hanlon and Fekadu2022). Similarly, alcohol use disorder can be treated effectively using brief behavioral interventions in primary care, internet-based psychosocial interventions, psychological therapies, and pharmacological treatments (Connor et al., Reference Connor, Haber and Hall2016). There is growing evidence in Sub-Sharan Africa that psychosocial interventions, including brief intervention and motivational interviewing, are promising in reducing heavy episodic drinking (Sileo et al., Reference Sileo, Miller, Huynh and Kiene2020) and promoting abstinence (Sileo et al., Reference Sileo, Miller, Wagman and Kiene2021). Increasing treatment coverage is one of the effective ways to minimize the health and economic burden of mental disorders.
Despite the considerable disease burden and available effective interventions, treatment-seeking is very low for mental disorders, particularly for depression and alcohol use disorder. The low treatment-seeking behavior creates a large gap between the prevalence and treatment of the illness. The prevalence of treatment-seeking is widely variable across countries, but only one in six people with alcohol use disorder (Mekonen et al., Reference Mekonen, Chan, Connor, Hall, Hides and Leung2021a) and one-third of people with depression (Mekonen et al., Reference Mekonen, Chan, Connor, Hides and Leung2021b) have received treatment globally. Limited evidence indicated that the treatment gap is even larger in LMICs where only 17% of people with depression and 9% of people with alcohol use disorder received treatment (Mekonen et al., Reference Mekonen, Chan, Connor, Hall, Hides and Leung2021a,Reference Mekonen, Chan, Connor, Hides and Leungb). In Ethiopia, treatment-seeking was around 23% for depression (Hailemariam et al., Reference Hailemariam, Tessema, Asefa, Tadesse and Tenkolu2012; Rathod et al., Reference Rathod, De Silva, Ssebunnya, Breuer, Murhar, Luitel, Medhin, Kigozi, Shidhaye, Fekadu, Jordans, Patel, Tomlinson and Lund2016) and 13% for alcohol use disorder (Rathod et al., Reference Rathod, De Silva, Ssebunnya, Breuer, Murhar, Luitel, Medhin, Kigozi, Shidhaye, Fekadu, Jordans, Patel, Tomlinson and Lund2016; Zewdu et al., Reference Zewdu, Hanlon, Fekadu, Medhin and Teferra2019). The treatment rates for depression and alcohol use disorder are even lower than the treatment rate reported for psychotic disorders (40%) (Fekadu et al., Reference Fekadu, Medhin, Lund, DeSilva, Selamu, Alem, Asher, Birhane, Patel, Hailemariam, Shibre, Thornicroft, Prince and Hanlon2019). Moreover, even this low rate of help-seeking typically occurs after a prolonged delay, with health facilities often being the last resort (Senait et al., Reference Senait, Habtamu, Hailemariam and Mubarek2020; Baheretibeb et al., Reference Baheretibeb, Wondimagegn and Law2021).
Multiple reasons have been identified why people with depression and alcohol use disorder do not utilize mental health services. Barriers to mental health service utilization can be attitudinal (mostly cultural and at the individual level) and structural (mostly at the health facility and policy level) (Bruwer et al., Reference Bruwer, Sorsdahl, Harrison, Stein, Williams and Seedat2011; Andrade et al., Reference Andrade, Alonso, Mneimneh, Wells, Al-Hamzawi, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Florescu, Gureje, Hinkov, Hu, Huang, Hwang, Jin, Karam, Kovess-Masfety, Levinson, Matschinger, O’Neill, Posada-Villa, Sagar, Sampson, Sasu, Stein, Takeshima, Viana, Xavier and Kessler2014). Previous studies reported that attitudinal barriers were more critical in high-income settings and structural barriers were more likely in LMICs (Sareen et al., Reference Sareen, Jagdeo, Cox, Clara, ten Have, Belik, de Graaf and Stein2007; Roberts et al., Reference Roberts, Miguel Esponda, Krupchanka, Shidhaye, Patel and Rathod2018). However, available evidence suggested that both attitudinal and structural barriers are important in hindering or delaying treatment in low-resource settings (Andrade et al., Reference Andrade, Alonso, Mneimneh, Wells, Al-Hamzawi, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Florescu, Gureje, Hinkov, Hu, Huang, Hwang, Jin, Karam, Kovess-Masfety, Levinson, Matschinger, O’Neill, Posada-Villa, Sagar, Sampson, Sasu, Stein, Takeshima, Viana, Xavier and Kessler2014; Nadkarni et al., Reference Nadkarni, Gandhi, Bhatia and Velleman2023). For example, a previous Ethiopian study reported that major barriers to seeking treatment for alcohol use disorder included low perceived need and a lack of knowledge about where to seek help (Zewdu et al., Reference Zewdu, Hanlon, Fekadu, Medhin and Teferra2019). Similarly, another Ethiopian study reported that low perceived need and cost of treatment were the most common barriers to seek help for postpartum depression (Azale et al., Reference Azale, Fekadu and Hanlon2016).
Understanding factors associated with seeking mental healthcare is essential for planning mental health service coverage and reaching untreated cases. Identifying the barriers that can hinder, delay, or discourage people from seeking mental health treatment is an important step towards improving mental health services and reducing the treatment gap. The overall aim of this study was to assess treatment-seeking behavior for depressive symptoms and hazardous drinking among a community sample in Merawi town, Northwest Ethiopia. The specific objectives were to (1) estimate treatment rates, (2) identify barriers to mental healthcare, (3) explore the treatment preferences and (4) assess the roles of religious and traditional healers.
Methods
Study setting and design
A cross-sectional study was conducted in Merawi town, the capital of Mecha District. Merawi town is in Northwest Ethiopia, 30 km from Bahir Dar City, the capital of Amhara Regional State. The town is organized with three kebeles (the smallest administrative unit in Ethiopia) with an estimated population of 42,159 in 2022 (ESS, 2022). One health center and one primary hospital serve the town and the surrounding rural population in the district.
Participants
As part of a larger project, 1,785 participants were screened for depression and hazardous alcohol use. With a response rate of 97%, a total of 1,728 (52.4% females) adults aged 18 years and above were included in the screening process. Participants who were screened positive for depressive symptoms (n = 414) and/or hazardous drinking (n = 155) were used in the analysis of the current study which makes the final sample size 569.
Sampling and data collection
We used a systematic random sampling method to select every other household in Merawi town. In each included household, one adult participant was selected randomly using a lottery method. The sample was allocated proportionally for each of the three kebeles. Data were collected in the private dwelling of the participants by a computer-assisted face-to-face interview in August 2021. Five psychiatry nurses, under the supervision of one author (H.B.) collected the data using a pre-loaded questionnaire on a tablet device. Participants with a positive screen for depressive symptoms or hazardous drinking were automatically prompted with additional questions related to treatment-seeking behavior and barriers to seek treatment from healthcare settings. When participants reported severe depressive symptoms, anxiety symptoms, and hazardous drinking, an automatic prompt instructs the data collector to refer them to the nearest health facility. Data collectors were trained on the procedures of data collection and materials using a training manual.
Variables and measurement
Socio-demographic variables
Participants were asked to report on their socio-demographic characteristics including gender, age, marital status, religion, education, income, and relative income. Relative income was assessed by asking participants to rate their income as poor, average, or well-off in relation to their neighborhood. This method of measuring relative income has been used in previous studies to assess how participants perceived their income compared to their neighbors (Fekadu et al., Reference Fekadu, Medhin, Selamu, Hailemariam, Alem, Giorgis, Breuer, Lund, Prince and Hanlon2014; Mekonen et al., Reference Mekonen, Getnet, Belete, Menberu and Fekadu2020).
Psychosocial and related variables
Social support was assessed using the Oslo 3-item Social Support Scale (OSS-3). The OSS-3 is a widely used tool in Ethiopia (Fekadu et al., Reference Fekadu, Medhin, Selamu, Hailemariam, Alem, Giorgis, Breuer, Lund, Prince and Hanlon2014; Zewdu et al., Reference Zewdu, Hanlon, Fekadu, Medhin and Teferra2019; Mekonen et al., Reference Mekonen, Getnet, Belete, Menberu and Fekadu2020) to assess the perceived number of close companions, level of concern from others, and perceived ease of getting help from families/neighbors/friends. A previous study (Kocalevent et al., Reference Kocalevent, Berg, Beutel, Hinz, Zenger, Härter, Nater and Brähler2018) reported good reliability for OSS-3 (Cronbach’s alpha = 0.64) and it has acceptable internal consistency in the current study (Cronbach’s alpha = 0.59). Social support was categorized as poor (OSS score 3–8), moderate (OSS 9–11), and strong (OSS 12–14) based on the sum score of OSS-3 (Bøen et al., Reference Bøen, Dalgard and Bjertness2012).
Perceived quality of life and perceived general health were assessed using single-item questions adapted from WHO’s quality of life assessment tool (Skevington et al., Reference Skevington, Lotfy and O’Connell2004) and the Short Form-36 instrument (McHorney et al., Reference McHorney, Johne and Anastasiae1993), respectively. The original scales for both the WHO’s quality of life assessment tool and SF-36 are cross-culturally reliable assessments, with Cronbach’s alpha values exceeding 0.82 for the specific domains that our single-item questions adapted (Brazier et al., Reference Brazier, Harper, Jones, Cathain, Thomas, Usherwood and Westlake1992; Skevington et al., Reference Skevington, Lotfy and O’Connell2004). Participants were asked to rate their general health and quality of life as “very poor, poor, neither, good, very good.” The items were re-coded as “poor, neither, good” during data processing.
Internalized stigma (due to depression and hazardous drinking) was assessed using a brief form of Internalized Stigma of Mental Illness Inventory (ISMI) (Boyd Ritsher et al., Reference Boyd Ritsher, Otilingam and Grajales2003) adapted in the Ethiopian context (Assefa et al., Reference Assefa, Shibre, Asher and Fekadu2012). ISMI asked participants to rate their agreement (1 strongly disagree to 4 strongly agree) with statements related to self-stigma (e.g., “Having depression has spoiled my life”). ISMI is a reliable measure in the Ethiopian context (Cronbach’s alpha = 0.92) using its mean score as a cutoff point (Assefa et al., Reference Assefa, Shibre, Asher and Fekadu2012; Zewdu et al., Reference Zewdu, Hanlon, Fekadu, Medhin and Teferra2019). The Cronbach’s alpha for ISMI was 0.78 in the current study. Attitude towards mental illness was assessed using six items adapted from the Reported and Intended Behavior Scale (RIBS) (Evans-Lacko et al., Reference Evans-Lacko, Rose, Little, Flach, Rhydderch, Henderson and Thornicroft2011), the Community Attitude towards Mental Illness Scale (CAMI) (Taylor and Dear, Reference Taylor and Dear1981), and the Mental Health Knowledge Schedule (Evans-Lacko et al., Reference Evans-Lacko, Little, Meltzer, Rose, Rhydderch, Henderson and Thornicroft2010) as relevant to the Ethiopian context. The items for the attitude towards mental illness include “I would be willing to work with someone with a mental health problem” (RIBS), “The mentally ill should be isolated from the rest of the community” (CAMI). The internal consistency for the attitude towards mental illness items was good in the current study (Cronbach’s alpha = 0.70), with a scoring and categorization similar to ISMI.
Mental health
The nine-item Patient Health Questionnaire (PHQ-9) was used to screen for depressive symptoms. PHQ-9 is validated in the Ethiopian context and has demonstrated good psychometric properties with 86% sensitivity and 67% specificity (Gelaye et al., Reference Gelaye, Williams, Lemma, Deyessa, Bahretibeb, Shibre, Wondimagegn, Lemenhe, Fann, Vander Stoep and Andrew Zhou2013). Participants were asked to rate their experience of DSM-IV depressive symptoms in the past 2 weeks on a four-point scale (0 = not at all to 3 = nearly every day). The sum score for PHQ-9 ranged from 0 to 27, with higher scores showing severe depressive symptoms. PHQ-9 demonstrated high internal consistency in the current study (Cronbach’s alpha = 0.85). Mild to severe depressive symptoms are indicated by a PHQ-9 score ≥5 (Kroenke et al., Reference Kroenke, Spitzer and Williams2001). In addition to the PHQ-9, participants were also asked if they had experienced episodes of depressive symptoms in the last 12 months outside of the last 2 weeks (Luitel et al., Reference Luitel, Jordans, Kohrt, Rathod and Komproe2017). Generalized anxiety disorder was assessed using the 7-item Generalized Anxiety Disorder scale (GAD-7) (Spitzer et al., Reference Spitzer, Kroenke, Williams and Lowe2006). GAD-7 has demonstrated high internal consistency in the current study (Cronbach’s alpha = 0.83) and a total score of ≥10 is indicative of moderate to severe anxiety symptoms (Spitzer et al., Reference Spitzer, Kroenke, Williams and Lowe2006).
Substance use
The 3-item Alcohol Use Disorders Identification Test–Consumption (AUDIT-C) was used to assess hazardous drinking. The AUDIT-C uses the first 3 items about alcohol consumption from the 10-item AUDIT and has comparable validity for detecting alcohol abuse or dependence at a cut-off point of 3 for females (99.3% sensitivity and 77.8% specificity) and 4 for males (88.4% sensitivity and 86.6% specificity) (Bush et al., Reference Bush, Kivlahan, McDonell, Fihn and Bradley1998; Seth et al., Reference Seth, Glenshaw, Sabatier, Adams, Du Preez, DeLuca and Bock2015). AUDIT-C had high internal consistency in the current study (Cronbach’s alpha 0.85). We also asked participants if they had ever used tobacco products and khat (Catha edulis, an evergreen stimulant leaf commonly used in East Africa and the Middle East).
Treatment-seeking behavior
Treatment-seeking behavior was assessed by asking participants with depressive symptoms and/or hazardous drinking if they had ever sought treatment for their symptoms. Participants with an affirmative response for treatment-seeking were asked follow-up questions about the treatment source – healthcare settings (general medical care or specialized mental healthcare) or non-healthcare settings (religious places, traditional healers, sorcery, family/friend).
Barriers to seeking professional help
Barriers to seeking professional help were assessed using the Barriers to Accessing Care Evaluation (BACE) scale (Clement et al., Reference Clement, Brohan, Jeffery, Henderson, Hatch and Thornicroft2012). Participants were asked about a range of factors that hinder, delay, or discourage them from seeking or continuing professional help for depressive symptoms or hazardous drinking. The BACE scale has been modified to yes/no binary questions of 20 possible barriers and was previously used in the Ethiopian context (Azale et al., Reference Azale, Fekadu and Hanlon2016; Zewdu et al., Reference Zewdu, Hanlon, Fekadu, Medhin and Teferra2019). The BACE scale demonstrated good internal consistency in the current study (Cronbach’s alpha 0.82 for hazardous drinking and 0.74 for depressive symptoms).
Analysis
We described the participants’ characteristics. The proportion of participants with depressive symptoms (PHQ-9 positive or last 12 months depressive symptoms) and hazardous drinking were reported. We also reported the proportion of participants who had ever sought treatment for depression and hazardous drinking.
For participants with depressive symptoms, treatment-seeking was cross-tabulated with participants’ characteristics and other variables. Cross-tabulation and other further analyses were not conducted for participants who sought treatment for hazardous drinking because only two participants had reported treatment-seeking for their drinking problem. Proportions of barriers that hindered, delayed, or discouraged participants from seeking treatment for depressive symptoms and hazardous drinking were summarized.
Univariate logistic regression was used to estimate the unadjusted odds ratios of each variable in relation to treatment-seeking for depressive symptoms. Multivariable logistic regression was conducted to identify adjusted odds ratios for factors associated with treatment-seeking. Variables were entered into the final model using a backward elimination variable selection method. To adjust for the multiple comparisons, we used a 99.5% confidence interval and statistical significance was declared at a p-value less than 0.005 (Ioannidis, Reference Ioannidis2018). We use SPSS v.28 to perform the analysis.
Results
Participant characteristics
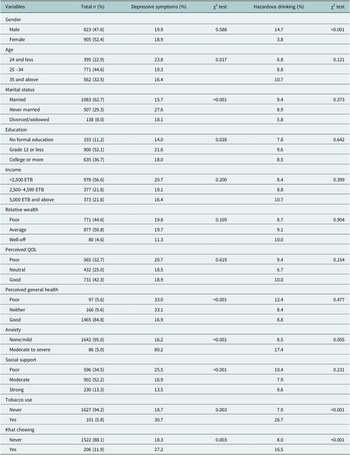
A total of 1,728 participants (52.4% female) were screened for depressive symptoms and hazardous drinking. The participants’ age ranged from 18 to 90 years with a median age of 29 years. The majority of the participants were married (62.7%) and reported good perceived general health (84.8%). PHQ-9 depressive symptoms were 19.4% (95% CI: 17.5–21.2%). Self-reported depressive symptoms within the last 12 months were 13% (95% CI: 11.4–14.5%). Participants with either PHQ-9 or last 12 months depressive symptoms were 24% (95% CI: 21.9–26.0%). Only 3.2% (n = 56) reported both depressive symptoms and hazardous drinking. A significant difference in depressive symptoms was observed based on the participants’ socio-demographic characteristics (age, marital status, and education), health-related (perceived general health and anxiety), and substance use (tobacco and khat) status (Table 1).
Table 1. Participant characteristics by depressive symptoms (PHQ-9 positive) and hazardous drinking status (n = 1,728)

Hazardous drinking was reported by 155 (9% [95% CI: 7.6–10.3%]) of participants. Participants with hazardous drinking were mostly males (78.1%), married (65.8%), and in the age group of between 25 and 34 years (43.9%). There was a significant gender difference in hazardous alcohol use where hazardous drinking was 14.7% in males and only 3.8% in females. Tobacco and khat use were also reported by 5.6% and 11.9% of participants, respectively. A significant difference in hazardous drinking was observed based on the participants’ substance (tobacco and khat) use status (Table 1).
Treatment-seeking behavior
Treatment-seeking behavior for hazardous drinking from any source was only 1.3%. No participant with hazardous drinking had sought help from healthcare settings. Only two participants (2/155) had sought help from their families/friends regarding their drinking problem.
Participants with depressive symptoms (PHQ-9 or last year depressive symptoms) (51.9% females) were mostly married (51.9%), in the age group of between 25 and 34 years (45.4%), maximum education of grade 12 (55.1%), and in the lower range of monthly income (58.7%). Among the 414 participants with depressive symptoms, 64.3% of them reported a high level of internalized stigma due to depression (Table 2).
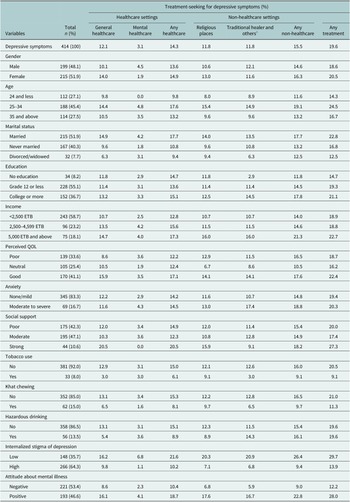
Table 2. Treatment-seeking for PHQ positive or last year depressive symptoms (n = 414)
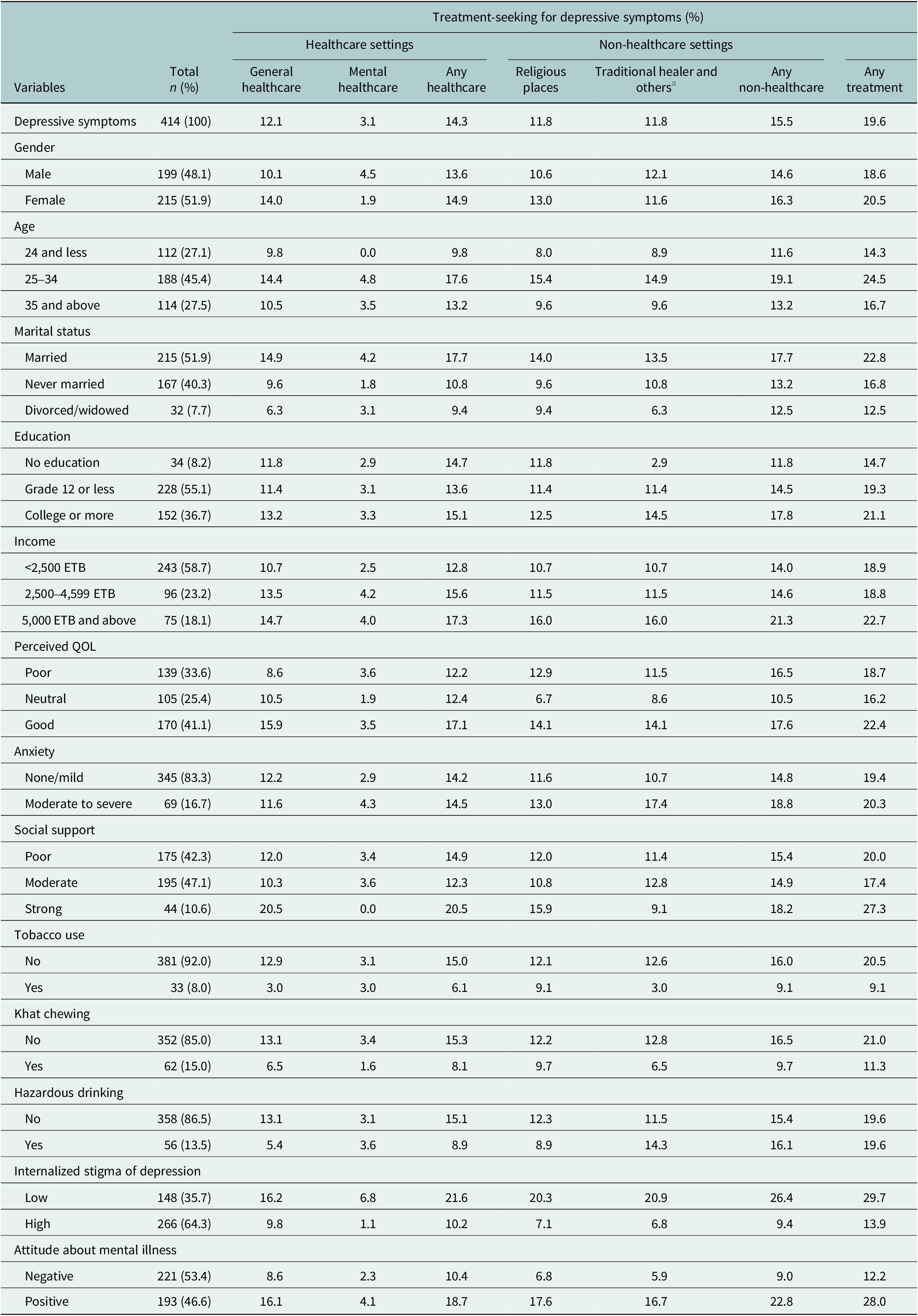
a Others = family/friends, wizard/sorcery; Any treatment = either healthcare or non-healthcare.
Treatment-seeking behavior for depressive symptoms was 14.3% (95% CI: 10.9–17.6%) from healthcare settings, 15.5% (95% CI: 12.0–18.9%) from non-healthcare settings, and 19.6% (95% CI: 15.7–23.4%) from any treatment source (either healthcare or non-healthcare). Treatment-seeking behavior from any source of treatment was higher among participants with low levels of internalized stigma (29.7%) and participants with a positive attitude towards mental illness (28%). While the help-seeking behavior from most sources was relatively similar, specialized mental healthcare was the least preferred (3.1%) source of treatment. The low treatment-seeking behavior from a mental healthcare setting was more pronounced among the younger age group, those who reported strong social support, and participants with a higher level of internalized stigma due to depression (Table 2).
Almost 40% of treatment seekers for depressive symptoms reported religious places were helpful treatment sources. One-fifth of the treatment-seeking participants reported none of the treatment sources were useful in treating their depressive symptoms (Figure 1).

Figure 1. Treatment sources considered as helpful in treating depressive symptoms (n = 81).
Unadjusted and adjusted estimates from logistic regression showed that attitudes about mental illness and internalized stigma of depression were important factors associated with treatment-seeking from any source of treatment. Participants with a positive attitude about mental illness (adjusted odds ratio (adj OR) = 2.84 [99.5% CI: 1.33–6.07) and lower level of internalized stigma (adj OR = 3.00 [99.5% CI: 1.41–6.42]) were three times more likely to seek treatment. Other variables including sociodemographic, clinical, and psychosocial variables did not show a statistically significant association with treatment-seeking behavior in both unadjusted and adjusted logistic regression models (Table 3).
Table 3. Factor associated with treatment-seeking (from any sources) for depressive symptoms (n = 414)

— variables excluded in the adjusted model based a backward elimination variable selection method.
* p-value <0.001.
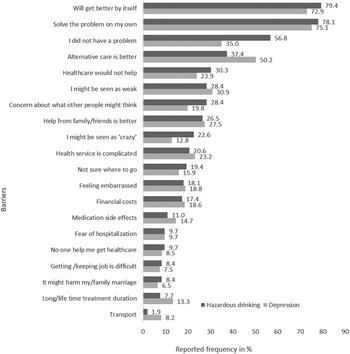
Barriers to seeking treatment from healthcare settings
Almost all participants with depressive symptoms (98.6%) and hazardous drinking (97.4%) reported at least one barrier to seeking treatment from healthcare settings. Most of the participants (more than 73%) believed the problem would get better by itself or that they could handle it themselves. The median number of barriers to seeking treatment for depression and hazardous drinking was 4 (interquartile ranges = 3 for depression and 5 for hazardous drinking). Three-fifths of participants (62.6% for depression and 59.4% for hazardous drinking) reported at least four barriers. Ten or more barriers were reported by 9% of participants with depressive symptoms and 14.2% of participants with hazardous drinking.
The top reported barriers to treatment-seeking for both depression and hazardous drinking were attitudinal and stigma-related barriers. The top three barriers to seeking treatment for depression were participants wanting to solve the problem by themselves (75.1%), perceiving the problem would get better by itself (72.9%), and prefer to get alternative forms of care from traditional or religious healers (50.2%). Similarly, the top three barriers to treatment seeking for hazardous drinking were participants’ perceptions that their drinking problem would get better by itself (79.4%), wanting to solve their problem by themselves (78.1%), and perceiving that they do not have a drinking problem (56.8%).
A substantial proportion of participants also reported structural barriers. The most frequently reported structural barriers were the perception that “the process of seeking health services is complicated” (23.2% for depression and 20.6% for hazardous drinking) and “financial costs involved in treatment-seeking” (18.6% for depression and 18.1% for hazardous drinking) (Figure 2).
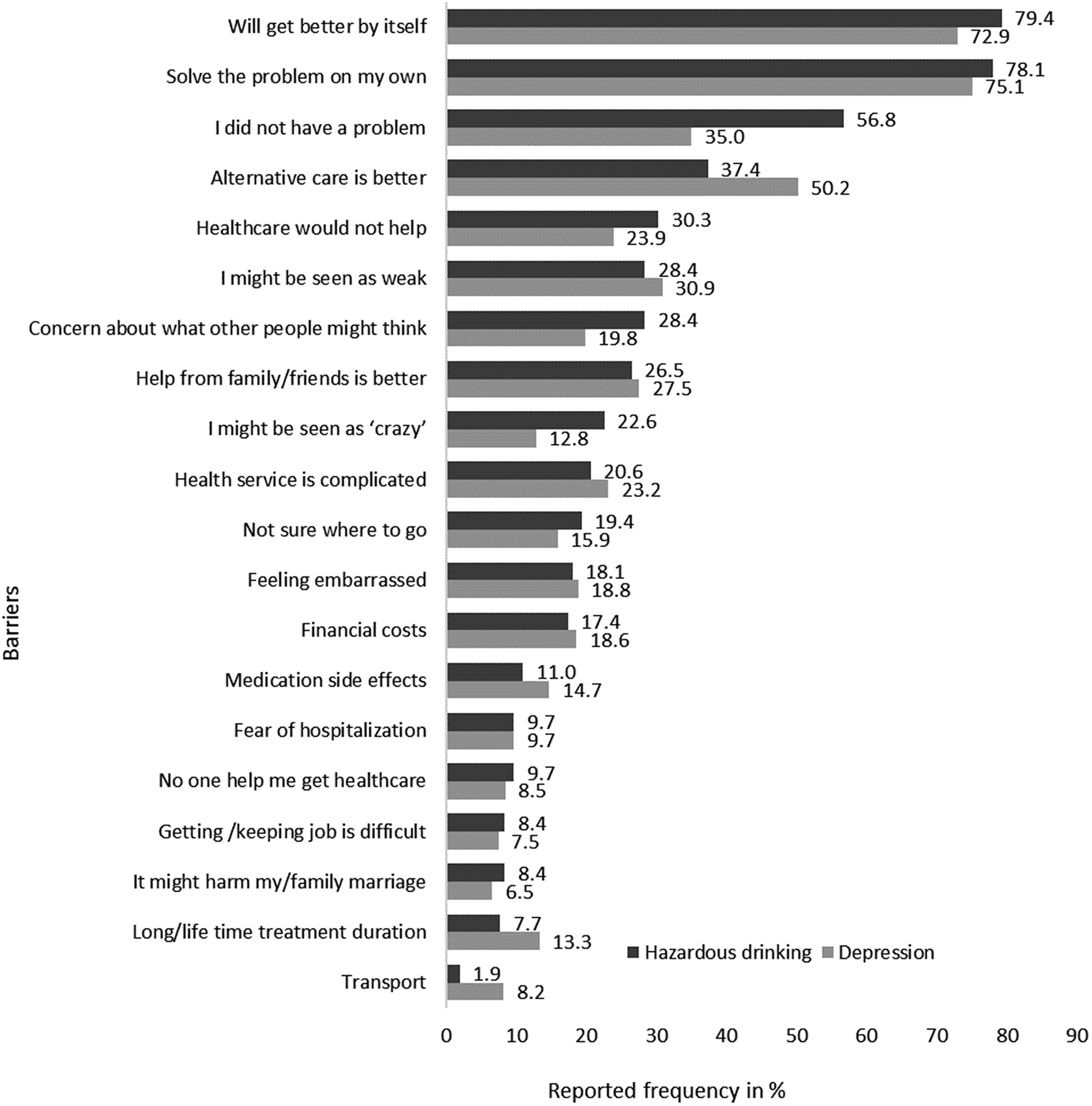
Figure 2. Barriers to seek treatment from healthcare settings for depression (n = 414) and hazardous drinking (n = 155).
Discussion
We conducted a cross-sectional survey at Merawi town in Northwest Ethiopia to assess treatment-seeking behavior and identify barriers to seeking treatment for depressive symptoms and hazardous drinking. This study provided important implications in the mental health services of a resource-limited setting, highlighting the barriers in treatment-seeking and participants’ preferences in the treatment sources.
Our finding showed that 19.6% of participants with depressive symptoms sought treatment either from healthcare or non-healthcare settings. Only 14% of participants sought treatment for depression from healthcare settings. Younger participants have reported relatively lower treatment rates for depression, while those in middle age have reported higher rates across all treatment sources. Although this difference is not significant in our regression model, previous studies have reported that middle-aged individuals are more likely to seek mental health treatment (Magaard et al., Reference Magaard, Seeralan, Schulz and Brütt2017; Roberts et al., Reference Roberts, Miguel Esponda, Krupchanka, Shidhaye, Patel and Rathod2018). Perceived stigma and preference for self-reliance may prevent young people from seeking help (Gulliver et al., Reference Gulliver, Griffiths and Christensen2010). No participant with hazardous drinking sought treatment from healthcare settings. Only two participants (1.3%) reported seeking help from their families/friends for their drinking problem, which is lower than the previous study (13% treatment-seeking) in the Southern part of Ethiopia (Zewdu et al., Reference Zewdu, Hanlon, Fekadu, Medhin and Teferra2019). The relatively higher treatment-seeking in the previous Ethiopian study may indicate a better mental health awareness in the community due to the mental health programs implemented in that area (Lund et al., Reference Lund, Tomlinson, De Silva, Fekadu, Shidhaye, Jordans, Petersen, Bhana, Kigozi, Prince, Thornicroft, Hanlon, Kakuma, McDaid, Saxena, Chisholm, Raja, Kippen-Wood, Honikman, Fairall and Patel2012). Our result is consistent with the previous meta-analyses that reported a range of 11–23% depression treatment rate (Mekonen et al. Reference Mekonen, Chan, Connor, Hides and Leung2021b) and mostly 0% alcohol use disorder treatment rate (Mekonen et al., Reference Mekonen, Chan, Connor, Hall, Hides and Leung2021a) in low-income countries.
Health workers could administer brief behavioral interventions (Pfeiffer et al., Reference Pfeiffer, Heisler, Piette, Rogers and Valenstein2011), psychological interventions (Cuijpers et al., Reference Cuijpers, Quero, Dowrick and Arroll2019), pharmacological treatments (Arroll et al., Reference Arroll, Chin, Martis, Goodyear-Smith, Mount, Kingsford, Humm, Blashki and MacGillivray2016; Connor et al., Reference Connor, Haber and Hall2016), or a combination of them (Pampallona et al., Reference Pampallona, Bollini, Tibaldi, Kupelnick and Munizza2004) to effectively treat depression and alcohol use disorder. However, 80% of participants with depressive symptoms and almost 100% of people with hazardous drinking in the current study had never sought help. These low rates of treatment-seeking created a large treatment gap, particularly for people with moderate to severe depressive symptoms who may benefit from pharmacological or behavioral interventions (NICE, 2022). Regardless of the treatment sources, 79% of treatment-seeking participants in the current study reported that their treatment-seeking helped to improve their depressive symptoms. Those groups of people who did not seek treatment could have benefited from the available helpful interventions.
Healthcare and non-healthcare settings were equally important sources of treatment for depressive symptoms. For instance, the prevalence of treatment-seeking was 12.1% from general medical care and 11.8% from religious and traditional healers. Interestingly, religious places were reported to be the most helpful source of treatment (39.5%) for depressive symptoms. A preference for religious and traditional healers over healthcare facilities was also reported in our previous qualitative study where seeking treatment from healthcare facilities was the last resort in the treatment-seeking pathway (Mekonen et al., Reference Mekonen, Chan, Belete, Menberu, Davidson, Hides and Leung2022). Previous studies in Ethiopia reported that patients were comfortable taking treatments from healthcare facilities alongside religious/traditional healers (Baheretibeb et al., Reference Baheretibeb, Wondimagegn and Law2021). As such, mental health services coverage could be increased by utilizing the existing help-seeking pathway of religious/traditional healers. Basic mental health training for religious leaders and traditional healers could also help increase referrals to health facilities (Mekonen et al., Reference Mekonen, Chan, Belete, Menberu, Davidson, Hides and Leung2022).
Consistent with the previous studies from Ethiopia and other LMIC (Andersson et al., Reference Andersson, Schierenbeck, Strumpher, Krantz, Topper, Backman, Ricks and Van Rooyen2013; Zewdu et al., Reference Zewdu, Hanlon, Fekadu, Medhin and Teferra2019), several barriers that hindered, delayed, or discouraged treatment-seeking from healthcare settings were reported by people with depressive symptoms and hazardous drinking. More than 97% of participants with depressive symptoms and hazardous drinking reported at least one barrier to seeking treatment from healthcare settings. According to the WHO Mental Health Atlas 2020 (WHO, 2021), the financial and human resources for mental health are meager in low-income countries with less than two mental health workers and mental hospital beds per 100,000 population. In Ethiopia, there were only 0.68 mental health workers per 100,000 population (WHO, 2021). With this paucity of mental health resources, one might expect structural barriers to be the most common barrier to seeking treatment from health facilities. However, consistent with the previous studies (Sareen et al., Reference Sareen, Jagdeo, Cox, Clara, ten Have, Belik, de Graaf and Stein2007; Andrade et al., Reference Andrade, Alonso, Mneimneh, Wells, Al-Hamzawi, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Florescu, Gureje, Hinkov, Hu, Huang, Hwang, Jin, Karam, Kovess-Masfety, Levinson, Matschinger, O’Neill, Posada-Villa, Sagar, Sampson, Sasu, Stein, Takeshima, Viana, Xavier and Kessler2014; Zewdu et al., Reference Zewdu, Hanlon, Fekadu, Medhin and Teferra2019), our study showed that the top reported barriers to treatment seeking from healthcare settings were attitudinal and stigma-related barriers.
It is worth noting that attitudinal and stigma-related barriers are not separate from structural barriers. Rather, structural barriers could contribute to the increased occurrence of attitudinal barriers. The assumptions related to the low perceived need for treatment (e.g., “the problem will get better by itself”, “I do not have a problem”, and “wanting to solve the problem by myself”) can indicate the low level of mental health literacy. This low level of mental health literacy can be improved by addressing the structural barriers embedded at the health facility and policy levels (WHO, 2021). Without treatment, nearly 90% of people with depression will continue to have symptoms beyond 3 months (Mekonen et al., Reference Mekonen, Ford, Chan, Hides, Connor and Leung2022).
In addition to the low mental health literacy, people may opt not to seek mental health services due to the stigma and discrimination attached to receiving mental illness diagnoses (Corrigan, Reference Corrigan2004; Mekonen et al., Reference Mekonen, Chan, Belete, Menberu, Davidson, Hides and Leung2022). This is also indicated in our study that seeking treatment for depressive symptoms was three-fold more likely in participants who had positive attitudes about mental illness (adj OR = 2.84) and participants who reported low internalized stigma of depression (adj OR = 3.00). Unless mental health literacy is improved, the public acceptance and perceived need for mental health services might be diminished (Jorm, Reference Jorm2000), and people with mental illness may avoid seeking mental health services (Mekonen et al., Reference Mekonen, Chan, Belete, Menberu, Davidson, Hides and Leung2022). Population-based campaigns aiming in increasing mental health awareness and decreasing stigma could help in increasing mental health services coverage and utilization (Donovan et al., Reference Donovan, Jalleh, Robinson and Lin2016; WHO, 2022b).
Consistent with the previous systematic review (Roberts et al., Reference Roberts, Miguel Esponda, Krupchanka, Shidhaye, Patel and Rathod2018), our study showed no difference in the sociodemographic characteristics of people who had sought treatment for depressive symptoms, compared to those who had not. This can be also another implication of attitudinal and stigma-related barriers being more critical at the individual level. Increasing mental health awareness, especially in the group of people who have a low perceived need to seek help could minimize the missed opportunity of accessing the available treatments.
Interpretation of the findings should consider the following limitations: first, the sample is from a semi-urban area in Northwest Ethiopia. The results may not be generalizable to the wider Ethiopian population. Descriptive statistics showed similar rates of depressive symptoms by gender, while in many contexts females generally have a higher rate. However, similar patterns of barriers to care were observed as indicated by the study conducted in the Ethiopian Southern part, especially for hazardous drinking (Zewdu et al., Reference Zewdu, Hanlon, Fekadu, Medhin and Teferra2019). Second, the sample (cases with depressive symptoms and hazardous drinking) is relatively small which could be less powered in detecting cases and associated factors of treatment-seeking. Third, as we used screening tools to measure depression (PHQ-9) and hazardous drinking (AUDIT-C), the cases did not imply clinical diagnoses. While these tools are not diagnostic tools, they are widely used and have good psychometric properties including in the African contexts (Bush et al., Reference Bush, Kivlahan, McDonell, Fihn and Bradley1998; Gelaye et al., Reference Gelaye, Williams, Lemma, Deyessa, Bahretibeb, Shibre, Wondimagegn, Lemenhe, Fann, Vander Stoep and Andrew Zhou2013; Seth et al., Reference Seth, Glenshaw, Sabatier, Adams, Du Preez, DeLuca and Bock2015). Most of the measurement tools employed in this study (except PHQ-9 and ISMI) were not validated in the Ethiopian general population context, potentially introducing a bias. However, it is worth noting that these measurement tools have been widely used in previous Ethiopian studies and have demonstrated acceptable to high internal consistency in our study. Additional limitation to consider is that the assessment of internalized stigma assumes that participants identified themselves as having depressive symptoms or hazardous drinking. However, this may not always be the case, introducing potential bias as some participants may not recognize these symptoms. Nonetheless, we took measures to mitigate this potential bias during the administration of internalized stigma assessment items by prompting participants to connect the ISMI questions with the symptoms they had previously reported.
Conclusion
Only one in five people with depressive symptoms living in Merawi town had sought treatment from any source. Treatment-seeking for hazardous drinking was extremely rare where only 1.3% reported seeking help from family/friends. Both healthcare and non-healthcare settings were reported as valuable sources of treatment. A positive attitude about mental illness and low-level internalized stigma of depression was positively associated with seeking any treatment for depressive symptoms. The top reported barriers to treatment seeking from healthcare settings for both depressive symptoms and hazardous drinking were attitudinal and stigma-related barriers. The structural barriers including the financial cost of treatment-seeking and the complicated process of health services were also substantial.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2023.88.
Data availability statement
The data is available from the corresponding author on reasonable request.
Acknowledgements
We would like to acknowledge the study participants for their involvement in this research.
Author contribution
T.M.Y.: Conceptualization, design, protocol development, data analysis, synthesis, write-up, manuscript review and edits. G.C.K.C.: Conceptualization, synthesis, manuscript review and edits, supervision. H.B.: Data collection, manuscript review and edits. L.H.: synthesis, supervision, manuscript review and edits. J.L.: Conceptualization, protocol development, synthesis, supervision, manuscript review and edits. All authors read and approved the final manuscript.
Financial support
This research did not receive any specific grant from funding agencies. T.M.Y. is supported by The University of Queensland Research and Training Program (RTP) scholarship. G.C.K.C. and J.L. are supported by NHMRC Investigator grants. The data collection was financially supported by the College of Medicine and Health Sciences, Bahir Dar University.
Competing interest
The authors declare none.
Ethics statement
This study followed the ethical principles in accordance with the declaration of Helsinki. The University of Queensland (approval number: 2020/HE000945) and the College of Medicine and Health Sciences, Bahir Dar University (approval number: 009/2021) approved this study. A formal permission letter was obtained from the local administration to collect the data. Participants were informed about the confidentiality of their responses, and their right to refuse or to withdraw from the interview. Data collectors obtained informed consent from each participant. Participants with severe depressive symptoms, anxiety symptoms, and hazardous drinking were referred to the nearest health facility for the necessary treatment.






Comments
Dear Editor,
We are pleased to submit our manuscript entitled “Treatment-seeking behavior and barriers to mental health service utilization for depressive symptoms and hazardous drinking: The role of religious and traditional healers in mental healthcare of Northwest Ethiopia”, for consideration of publication at the Global Mental Health.
This study aimed to assess treatment-seeking and barriers to seek treatment for depressive symptoms and hazardous drinking among community sample in Northwest Ethiopia. This study provided important implications in the mental health services of a resource limited setting, highlighting the barriers in treatment-seeking and participants’ preference in treatment sources. We believe the findings from this study can help to inform policymakers for planning mental health service coverage and reaching untreated cases. Identifying the barriers that can hinder, delay, or discourage people from seeking mental health treatment is an important step towards improving mental health services and reducing the treatment gap.
Only one in five people with depressive symptoms had sought treatment either from healthcare or non-healthcare settings. Treatment-seeking for hazardous drinking was extremely rare with only 1.3% had sought help from family/friends. Religious and traditional healers were equally important as healthcare settings in providing mental healthcare. Attitudinal and stigma-related barriers were the most frequently reported barriers.
This manuscript has not been previously published and is not under consideration in the same or substantially similar form in any other scientific journals. All authors listed have contributed sufficiently to the project to be included as authors, and all those who are qualified to be authors are listed in the author byline. All authors declare that they have no competing interests, and they also approved the manuscript as well as the submission of this paper.
We appreciate your time, and we look forward to the response of the Editorial team to this manuscript.
Sincerely,
Corresponding author
Tesfa Mekonen