Impact statement
Perinatal depression (PND) can occur during pregnancy or up to one year post-delivery. It is one of the most common health-related issues experienced by mothers and is linked to ill health for the mother and child. In low- and middle-income countries (LMICs), one in four women experience PND, compared to one in ten in high-income countries. Nevertheless, in LMICs, over 90% cannot access treatment. Psychological interventions for PND have shown to be effective, but there is limited research on details behind their success. Investigating how and why psychological therapies for PND are successful in diverse contexts is critical to understanding how we can intervene at a public health level to improve outcomes. Currently, a rapidly growing body of researchers is developing sustainable mental health interventions for LMICs, and some of these studies explore factors which may explain the effectiveness of therapies for PND. We systematically reviewed this evidence to provide an overview of the factors which may be associated with the success of psychological therapies for women with PND in LMICs. We found seven publications on trials conducted in Asia and sub-Saharan Africa. Gaps in quantity and quality of analyses limited interpretability and generalisability of findings and also calls for further research and reporting guidelines. However, current reliable evidence suggests that patient engagement with care and social support may be key elements of successful therapies, increasingly depressed women who begin therapy may be more responsive to treatment, and women entering therapy who have had depression for less time may have increased success rates compared to those who have been depressed for longer.
Introduction
Perinatal depression (PND), which can occur antenatally or up to one year postnatally, is one of the most common health-related issues experienced by mothers, yet it often goes untreated (Rahman et al., Reference Rahman, Waqas, Nisar, Nazir, Sikander and Atif2021). PND is associated with several negative health outcomes, such as decreased maternal social support, increased risk of continued and worsened depressive symptoms and negative outcomes in the physical and cognitive development of the child (Bright et al., Reference Bright, Charrois, Mughal, Wajid, McNeil, Stuart, Hayden and Kingston2020; Rahman et al., Reference Rahman, Waqas, Nisar, Nazir, Sikander and Atif2021). Unfortunately, these concerns are exacerbated in low- and middle-income countries (LMICs), where about one in four women experience PND (Roddy Mitchell et al., Reference Roddy Mitchell, Gordon, Lindquist, Walker, Homer, Middleton, Cluver, Tong and Hastie2023) compared to about one in ten women in high-income countries (Gavin et al., Reference Gavin, Gaynes, Lohr, Meltzer-Brody, Gartlehner and Swinson2005). This may be due to decreased mental health resources and increased socioeconomic adversities in low-resource settings, which increase the risk for PND (Fisher et al., Reference Fisher, Cabral de Mello, Patel, Rahman, Tran, Holton and Holmes2012; Honikman et al., Reference Honikman, Sigwebela, Schneider and Field2020).
Research has demonstrated the effectiveness of psychological therapies for the treatment and prevention of PND, including interpersonal psychotherapy, cognitive behavioural therapy (CBT) and behavioural activation (BA) (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Honikman et al., Reference Honikman, Sigwebela, Schneider and Field2020; Rahman et al., Reference Rahman, Waqas, Nisar, Nazir, Sikander and Atif2021). In recent years, studies carried out in various LMICs have shown that employing strategies such as ‘task-sharing’, where non-specialists are trained to deliver mental health treatments, and delivery of care through digital technologies are successful and feasible approaches to implementing psychosocial interventions in contexts with limited human resources for mental healthcare (Munodawafa et al., Reference Munodawafa, Mall, Lund and Schneider2018; Rahman et al., Reference Rahman, Waqas, Nisar, Nazir, Sikander and Atif2021). Despite this evidence base, over 90% of women with PND in LMICs still do not have access to treatment (Rahman et al., Reference Rahman, Waqas, Nisar, Nazir, Sikander and Atif2021). Understanding how effective interventions can be optimised for scale-up is therefore essential to relieving this burgeoning mental health crisis.
While psychological interventions have been shown to be effective in reducing PND symptom severity, what is less understood are the mechanisms behind their success, particularly in low-income contexts (Munodawafa et al., Reference Munodawafa, Mall, Lund and Schneider2018). While this evidence gap is present in psychotherapy research in general (Kazdin, Reference Kazdin2007), the specific complex challenges that accompany adapting an intervention to suit a new population, culture and set of resources (Eaton et al., Reference Eaton, McCay, Semrau, Chatterjee, Baingana, Araya, Ntulo, Thornicroft and Saxena2011), combined with the high prevalence of PND and significant treatment gap in LMICs in particular, make understanding key mechanisms in diverse contexts especially important when planning for scale-up in such settings. Specifically, having an understanding of the mechanisms through which an intervention improves outcomes for PND provides insight on different features to target to improve effectiveness at a population level.
For effective scale-up, more research is needed to understand how, under what conditions and for whom such treatments are effective. A lack of evidence in this area means that future efforts to implement and adapt successful therapies for this population may fail to bring these active ingredients to life. The predictors, moderators and mediators of psychological therapies for women with PND in LMICs require further investigation.
Predictors, moderators and mediators are three factors that influence the impact of the intervention on the outcome; however, they are by no means synonymous. Where predictors are pre-randomisation, baseline factors that demonstrate an association with the outcome of interest (e.g., individual traits or contextual factors that are non-specific to treatment condition) (see Figure 1a), moderators describe subgroups of people for whom the intervention works (e.g., men vs. women) (Kraemer et al., Reference Kraemer, Wilson, Fairburn and Agras2002). Moderators are typically considered baseline factors; however, unlike predictors, which act independently of treatment, moderators interact with treatment type to amplify or reduce its effect on the outcome (see Figure 1b). For instance, if patients living closer to their treatment provider experienced improved treatment outcomes regardless of treatment type when compared to individuals living farther from their treatment provider, treatment proximity may be considered a predictor of treatment effectiveness. On the other hand, treatment proximity would be a moderator of treatment effectiveness if only those receiving one kind of treatment benefitted (e.g., improved outcomes for those receiving talk therapy but not for those receiving drug therapy). Moderators may also be considered post-randomisation variables that modify the effect of the intervention on treatment outcome (e.g., an increased effect of the intervention when more sessions are attended) (see Figure 1c) (Dunn et al., Reference Dunn, Emsley, Liu, Landau, Green, White and Pickles2015). Lastly, mediators represent potential mechanisms that are triggered by the intervention and have an effect on the outcome (e.g., self-efficacy, improved levels of social support, increased BA). Unlike predictors and moderators, mediators sit on the causal pathway, creating a direct link between the intervention and the outcome (see Figure 1d) (Kraemer et al., Reference Kraemer, Wilson, Fairburn and Agras2002).

Figure 1. (a) Predictor variable. (b) Baseline moderator variable. (c) Post-randomisation moderator variable. (d) Mediator variable.
Identifying predictors, moderators and mediators of an intervention are important for scale-up because they provide insight into ways that an intervention can be optimised. In randomised controlled trials (RCTs), a moderator of treatment effect sheds light on for whom the intervention may be successful (Baron and Kenny, Reference Baron and Kenny1986). Furthermore, moderators provide insight onto how treatment effectiveness may be maximised by matching particular interventions to individual circumstances. In a similar light, awareness of predictors reveals for whom interventions may be successful in general and also when improved outcomes may not be entirely due to the treatment itself. Lastly, a mediator of the outcome suggests the mechanism through which the treatment works (or not). Identification of a potential mediator provides insight on features of an intervention to target to improve outcomes in the future (Baron and Kenny, Reference Baron and Kenny1986; Kraemer et al., Reference Kraemer, Wilson, Fairburn and Agras2002).
To date, there is no systematic review which identifies predictors, moderators and mediators of effects of psychological treatments for PND; however, some systematic reviews explore predictors of PND itself (Gelaye et al., Reference Gelaye, Rondon, Araya and Williams2016), mediators of treatments for depression (Domhardt et al., Reference Domhardt, Steubl, Boettcher, Buntrock, Karyotaki, Ebert, Cuijpers and Baumeister2021), or predictors, mediators and moderators of treatments for depression in other populations (Courtney et al., Reference Courtney, Watson, Krause, Chan, Bennett, Gunlicks-Stoessel, Rodak, Neprily, Zentner and Szatmari2022).
Relevant factors that have been identified in the current literature (e.g., social support and patient activation as mediators) (Singla et al., Reference Singla, MacKinnon, Fuhr, Sikander, Rahman and Patel2021) must be carefully evaluated and considered in conjunction with one another in order to establish a well-rounded, accurate and quality-assessed picture of how (mediators), why (predictors) and for whom (moderators) psychological therapies for PND are effective. Increased understanding behind these details of psychological therapies for PND in LMICs is crucial to maximising treatment outcomes and increasing treatment coverage in this population and setting.
This systematic review aims to synthesise the current knowledge about the predictors, moderators and mediators of psychological therapies associated with reduced symptoms of PND in LMICs.
Methods
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Supplementary Appendix A) (Page et al., Reference Page, McKenzie, Bossuyt, Boutron, Hoffmann, Mulrow, Shamseer, Tetzlaff, Akl, Brennan, Chou, Glanville, Grimshaw, Hróbjartsson, Lalu, Li, Loder, Mayo-Wilson, McDonald, McGuinness, Stewart, Thomas, Tricco, Welch, Whiting and Moher2021) and has been registered on PROSPERO, registration CRD42022342026.
Eligibility criteria
Articles included in the review explore data from studies that were experimental, had any quantitative or mixed methods design, and that used quantitative approaches to evaluate predictors, moderators and mediators. Articles evaluating data from non-experimental studies, qualitative studies, discussion papers, studies not available in English, or studies that were either not peer-reviewed or that did not obtain ethical approval were excluded.
Articles evaluating data from studies that enrolled women (adolescent or adult) with PND were included. PND was defined as depression at anywhere from conception to 12 months postnatal, as determined by diagnostic interview or by use of a validated screening tool for depression. If an article evaluated data from a study in which the primary diagnosis was not depression, it was excluded from the review.
Articles that evaluated data from RCTs assessing psychological therapies for PND were included. Psychological therapies were broadly defined as talk therapies or any mental health intervention utilising forms of psychosocial components (e.g., individual or group therapeutic activities, techniques or strategies). Articles evaluating data from pharmaceutical treatments only were excluded.
Articles evaluating data from a study using any kind of active or inactive control comparison group, besides pharmaceutical treatment only, were included (e.g., perinatal treatment as usual, enhanced usual care (EUC), waitlist control, placebo).
Articles were eligible for inclusion if they evaluated data from a study assessing the effect of a psychological therapy on PND symptom reduction and additionally tested for at least one predictor, moderator or mediator of treatment effect. Articles were excluded if they did not clearly indicate the effect of a predictor, moderator or mediator with a quantitative measure.
Articles were eligible for inclusion if they assessed data from studies that took place in LMICs (as defined by the World Bank at the time of the study) (“World Bank Country and Lending Groups – World Bank Data Help Desk”, n.d.).
Search strategy
On the 4 April 2022, a scoping search was carried out using the following databases on Ovid: Embase, MEDLINE and APAPsycINFO. On 6 June 2022, a systematic literature search using a finalised search strategy was conducted on the following five databases: Embase (Ovid), MEDLINE (Ovid), APAPsycINFO (Ovid), Cochrane Library (Wiley Online Library) and CINAHL (EBSCOhost). All results were exported to Endnote, where duplicates were deleted automatically and by hand on 9 July 2022.
Search terms included any combination of the following (including synonyms and alternate spellings): perinatal AND depression AND psychological therapy AND (moderators OR mediators OR predictors) AND LMICs. Please refer to Supplementary Appendix B for the full search strategy. To ensure no relevant articles were omitted, backward citation searching of the included studies was conducted and experts of the review topic were contacted.
Study selection
Once all duplicates were deleted on Endnote, remaining articles were exported to the online software Rayyan (Ouzzani et al., Reference Ouzzani, Hammady, Fedorowicz and Elmagarmid2016) and screened using an electronic screening tool (found in Supplementary Appendix C). From 13 to 14 July 2022, the screening tool underwent two rounds of piloting and subsequent discussions with both the main author and a second reviewer (A.M.). Inter-rater reliability of both reviewers was 100%. On 16 to 17 July 2022, a single reviewer carried out screening phase 1. Using titles and abstracts, articles were either excluded or set aside in Rayyan for later full-text screening (Phase 2). From 20 to 23 July 2022, the reviewer located all full-text articles of potentially eligible studies to carry out the full-text screening (Phase 2). From 28 to 30 July 2022, articles identified from backward citation searching and from correspondence with experts were screened (Phase 3). All screening decisions were individually cross-checked.
Data collection
Between 31 July to 8 August 2022, a data extraction form was developed, piloted and then used to extract data from the included articles in extraction phase 1. The extraction form may be found in Supplementary Appendix D.
From 8 to 12 August 2022 and again on 28 August 2022, extraction phase 2 took place, during which key information from the extraction form was formatted onto extraction tables and individually cross-checked. A.M. cross-checked the data tables of a random selection of 50% of the articles.
Quality assessment
Between 12 to 16 August 2022 and again on 26 August 2022, all original trials included in the review were assessed for methodological quality using the Cochrane Risk of Bias 2 (RoB 2) tool (Sterne et al., Reference Sterne, Savović, Page, Elbers, Blencowe, Boutron, Cates, Cheng, Corbett, Eldridge, Emberson, Hernán, Hopewell, Hróbjartsson, Junqueira, Jüni, Kirkham, Lasserson, Li, McAleenan, Reeves, Shepperd, Shrier, Stewart, Tilling, White, Whiting and Higgins2019). A second round of quality assessment took place for all included articles to evaluate the quality of analysis of potential predictors, moderators or mediators. This involved assessment of five criteria based on guidance from the Cochrane handbook and a consensus study of international experts (Pincus et al., Reference Pincus, Miles, Froud, Underwood, Carnes and Taylor2011). A.M. cross-checked a random selection of 50% of the quality assessment results. Quality assessment results were also individually cross-checked. A Guideline for Reporting Mediation Analyses (AGReMA), an international, consensus-based set of guidelines developed using the Enhancing Quality and Transparency of Health Research (EQUATOR) methodological framework (Lee et al., Reference Lee, Cashin, Lamb, Hopewell, Vansteelandt, VanderWeele, MacKinnon, Mansell, Collins, Golub, McAuley, Localio, van Amelsvoort, Guallar, Rijnhart, Goldsmith, Fairchild, Lewis, Kamper, Williams and Henschke2021), although not a quality assessment tool, was considered when evaluating mediation analyses included in the review.
Data analysis
Findings of the different articles were reported qualitatively using narrative synthesis in accordance with the PRISMA statement (Page et al., Reference Page, McKenzie, Bossuyt, Boutron, Hoffmann, Mulrow, Shamseer, Tetzlaff, Akl, Brennan, Chou, Glanville, Grimshaw, Hróbjartsson, Lalu, Li, Loder, Mayo-Wilson, McDonald, McGuinness, Stewart, Thomas, Tricco, Welch, Whiting and Moher2021). This approach was chosen due to a limited number of studies included in the review. Importantly, there was a high degree of heterogeneity between studies as a result of the diverse range of settings represented and the various ways in which predictors, moderators and mediators were captured. All articles identified were included in the narrative synthesis, in which identification and description of patterns and relationships found in the data was carried out by using data extracted from each article on predictors, moderators and mediators of psychological therapies for PND in LMICs.
Results
Study selection
The search strategy yielded a total of 413 articles. After duplicates were removed, 294 articles were deleted through title and abstract screening (Phase 1). Twenty-four articles underwent full-text screening (Phase 2), and 16 additional articles were identified through backhand citation searching and correspondence with experts of the review topic (Phase 3). Final results from all three phases of screening yielded a total of seven articles eligible for inclusion in the review (see Figure 2). The term ‘article’ is used in this review to refer to both original trials and secondary data analyses. The terms ‘trial’ and ‘study’ are used to refer to original trials only.
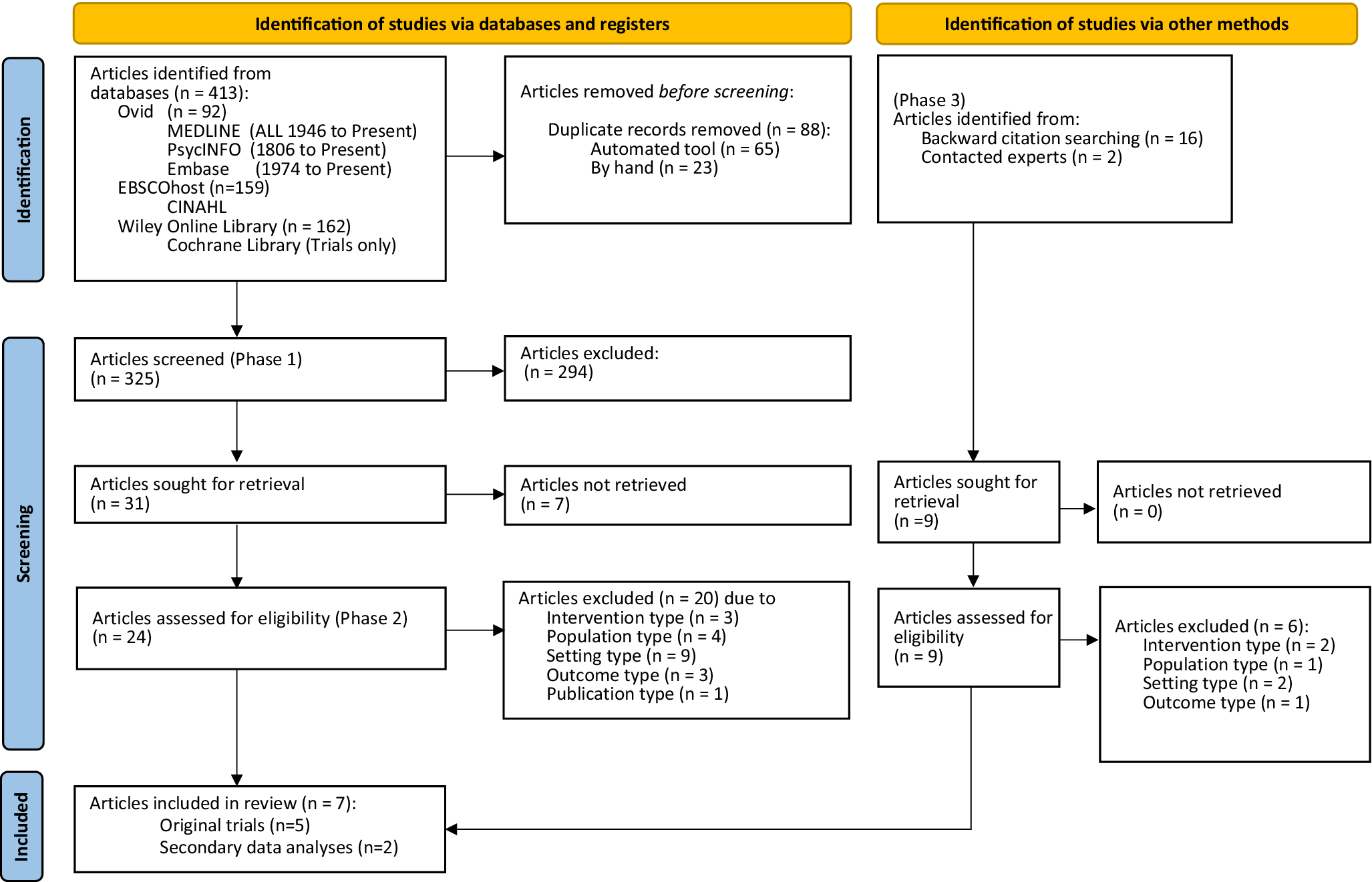
Figure 2. PRISMA flowchart.
Study characteristics
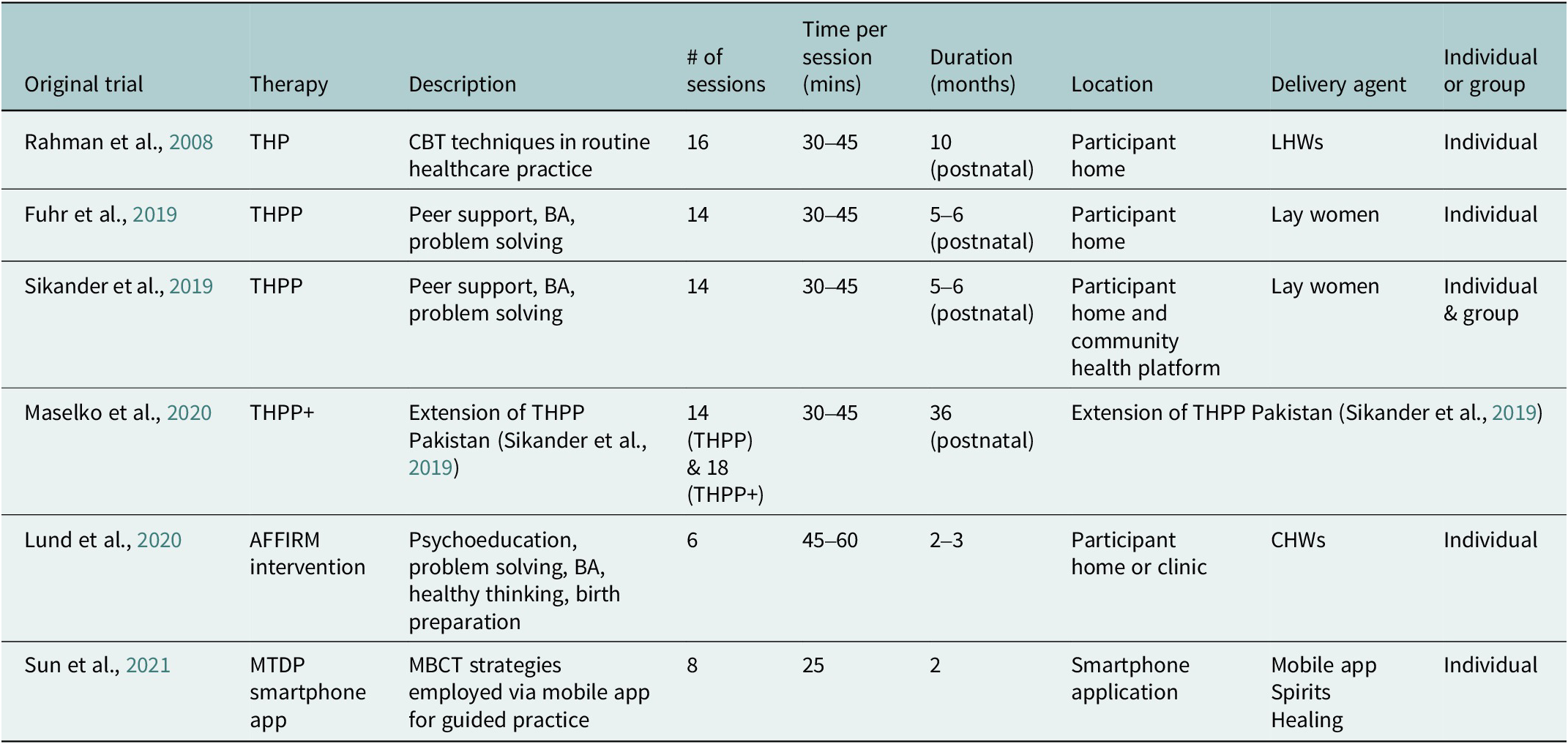
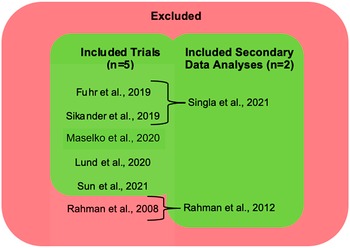
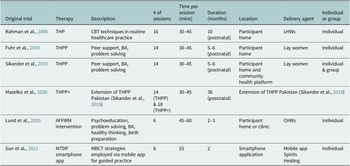
Table 1 describes a summary of characteristics of the included articles. A visual representation of the included original trials and secondary data analyses is presented in Figure 3. There were seven articles in total; five were original trials (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020; Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021), and two were secondary data analyses (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012; Singla et al., Reference Singla, MacKinnon, Fuhr, Sikander, Rahman and Patel2021). One of the original trials (Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020) is an extension of another trial (Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019) and is included in this review as a separate study as it evaluates an additional component of the original intervention. One of the secondary data analyses (Singla et al., Reference Singla, MacKinnon, Fuhr, Sikander, Rahman and Patel2021) reported on original trials which were included in the review (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019). The other secondary data analysis (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012) reported on an original trial (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008) (referred to in this review for study details) which was not eligible for inclusion since it did not include any quantitative analysis of predictors, moderators or mediators (see Figure 3). The included articles were published in the past ten years (2012–2021), and sample sizes ranged from 168 to 903 participants. The five original trials included in the review were mainly conducted in Asia (India (n = 1) (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019), Pakistan (n = 2) (Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020) and China (n = 1) (Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021)), and one was conducted in South Africa (Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020). The secondary data analysis of an original trial which was not included in the review (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012) was based on an original trial that took place in Pakistan (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008). All included articles were based on randomised trials (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008; Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020; Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021). All included articles were based on studies that recruited prenatal women either from an antenatal clinic (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020; Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021) or registers of community health workers (CHWs) (Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020). To assess depression severity at baseline and follow-up, most trials (n = 3) used a culturally validated version of the Patient Health Questionnaire 9 (PHQ-9) (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020). The other two included trials, in addition to the original trial of an included secondary analysis, employed the Hamilton Depression Rating Scale (HDRS) (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008; Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020) and the Edinburgh Postnatal Depression Scale (EPDS) (Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020; Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021).
Table 1. Characteristics of the included articles on psychological therapies for PND in LMICs

Note: *p < 0.05; **p < 0.01; ***p ≤ 0.001.
Abbreviations: AFFIRM, Africa Focus on Intervention Research for Mental Health; CHC, community health centre; CI, confidence interval; CRT, cluster randomised trial; EPDS, Edinburgh Postnatal Depression Scale; EUC, enhanced usual care; HDRS Hamilton Depression Rating Scale; LHWs, Lady Health Workers, MTDP, mindfulness training during pregnancy, NI, no information; PHCs, primary health centres; PHQ-9, Patient Health Questionnaire 9; PND, perinatal depression; RCT, randomised controlled trial; SD, standard deviation; TAU, treatment as usual; THP, Thinking Healthy Program; THPP, Thinking Healthy Program Peer-Delivered; THPP+, Extended Thinking Healthy Program Peer-Delivered.
a Study dropout was calculated as follows: 1 – (participants completing posttreatment assessment/randomised participants across groups). These calculations are not necessarily in accordance with the study dropout rates as reported in primary studies.
b This extension study includes participants from a third study arm without depression (n = 584), separate from the n = 570 allocated to either the intervention or control arm.
c Pooled sample size: N = 850.

Figure 3. Original trials and secondary data analyses included in the review.
Therapy types and methods of delivery
Characteristics of therapies evaluated in the included articles can be found in Table 2. Three of the included original trials and one secondary analysis from an original trial (four mediation analyses in total) were based on evaluated variations of the Thinking Healthy Program (THP) (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008; Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020). Three trials assessed the adapted, peer-delivered version of THP, called the Thinking Healthy Program Peer-Delivered (THPP) (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020). One of these THPP trials evaluated an extended version of the intervention (THPP+) (Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020). A separate trial, on which one included secondary data analysis was based (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012), assessed the original THP intervention delivered by trained CHWs called Lady Health Workers (LHW) (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008).
Table 2. Characteristics of therapies evaluated by included articles
Abbreviation: AFFIRM, Africa Focus on Intervention Research for Mental Health; BA, behavioural activation; CBT, cognitive behavioural therapy; CHWs, community health workers; LHWs, Lady Health Workers, MBCT, mindfulness behavioural cognitive therapy; MTDP, mindfulness training during pregnancy; THP, Thinking Healthy Program; THPP, Thinking Healthy Program Peer-Delivered; THPP+ Extended Thinking Healthy Program Peer-Delivered.
One trial assessed a smartphone-based intervention delivered via mobile app (Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021). The trial by Lund and colleagues, part of the Africa Focus on Intervention Research for Mental Health (AFFIRM), assessed a task-sharing psychological intervention delivered by CHWs (Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020).
Comparison conditions
Most trials assigned EUC to the control group (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008; Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020; Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021). In the THPP and THPP+ trials (n = 3), participants in the control group were assigned to EUC, comprised of antenatal treatment as usual and receiving information on healthcare resources. EUC was also assigned to the intervention group in addition to THPP or THPP+ (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020). The control group in the THP trial also received EUC, which meant participants received the same number of visits as those in the THP group but by routinely trained LHWs (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008). In the AFFIRM intervention, EUC in the control group included routine clinic antenatal care and three monthly check-ins by CHWs via phone call (Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020). In the study by Sun and colleagues, participants in the attention control condition received regular health consultations by a trained nursing assistant via a mobile application (Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021). Control conditions of each trial included in the review may be found in Table 1.
Study results
Results of analyses for potential predictors, moderators and mediators
A summary of predictors, moderators and mediators evaluated in the included studies (including analysis methods used and power of effects) is detailed in Table 3. Table 3 excludes analysis methods used by Sun and colleagues (Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021) due to unclear reporting. In terms of predictors, the THP trial found evidence that the following baseline variables predicted higher depression scores at follow-up: high depression score (p ≤ 0.001), low body mass index (BMI) (p < 0.01), older age (p < 0.01), not being financially empowered (p ≤ 0.001), the presence of household debt (p < 0.01) and low family support (p < 0.05) (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012). Sun and colleagues reported that being primiparous at baseline was a predictor of depression at two months post treatment allocation (p < 0.01) (Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021).
Table 3. Summary of analyses of potential predictors, moderators and mediators of psychological therapies for PND in LMICs

Note: *p < 0.05; **p < 0.01; ***p ≤ 0.001.
Abbreviations: ANCOVAR, analysis of covariance; AUDIT, Alcohol Use Disorder Identification Test; BMI, body mass index; EPDS, Edinburgh Postnatal Depression Scale; FAI, Functional Assessment Instrument; GEE, generalised estimating equations; HDRS, Hamilton Depression Rating Scale; IPV, intimate partner violence; ITT, intention-to-treat; LHWs, Lady Health Workers; MINI, Mini-International Neuropsychiatric Interview; MSPSS, Multidimensional Scale of Perceived Social Support; PAAS, Premium Abbreviated Activation Scale; PHQ-9, Patient Health Questionnaire 9; THPP, Thinking Healthy Program Peer-Delivered; WHODAS, WHO Disability Assessment Schedule.
a Exact p value and quantitative results are not specified because of high correlation with financial empowerment.
b Effect found at 8 weeks after group allocation only.
c Effect modification was only found for remission at 6 months (PHQ-9 < 5), not symptom severity at 6 months.
d Exact p value is unknown; however, the 95% CI of coefficient estimate does not cross zero, indicating significance.
e Empowerment was re-assessed after 6 months and debt was reassessed after 1 year.
In terms of moderators, Fuhr and colleagues found that women with a shorter duration of depression at baseline were more likely to respond to THPP than women with a longer duration of depression at baseline (p < 0.05), but only regarding its impact on depression remission at six months (PHQ-9 < 5), not on PHQ-9 score (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019). The study by Lund and colleagues found high baseline HDRS score to be a moderator of treatment response at eight months gestation (p ≤ 0.001), three months postpartum (p ≤ 0.001) and 12 months postpartum (p ≤ 0.001) follow-up periods, although the same result was not found with other measures of depression at baseline (e.g., EPDS, Mini-International Neuropsychiatric Interview diagnosis). The secondary analysis by Rahman and colleagues on THP demonstrated that at baseline, women who reported being in debt (p < 0.05) or not financially empowered (p < 0.05) showed more improvement in depression scores (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012). The publication by Sun and colleagues reports that time since treatment allocation moderated effects of the digital intervention (p < 0.01), although details related to directionality of effect are not clear in this particular study. They also reported on multiple three-way interactions between treatment group, time since treatment allocation and multiple other variables; however, it must be noted that no interaction term was described in the included article (Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021). Findings from the THPP+ trial and the THPP Pakistan trial found no evidence of moderation (Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020).
In terms of mediators, Singla and colleagues (Singla et al., Reference Singla, MacKinnon, Fuhr, Sikander, Rahman and Patel2021) identified patient activation and social support as mediators of THPP in the trials that took place in India and Pakistan (p values not reported). The same result was found for patient activation (p < 0.05) and social support (p < 0.05) when data between the two parallel trials were pooled. On the other hand, mother–child attachment was not found to be a mediator of treatment effect for THPP (Singla et al., Reference Singla, MacKinnon, Fuhr, Sikander, Rahman and Patel2021). In the THP trial, no evidence of mediation was found for changes in household debt or for level of financial empowerment (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012).
Study quality
RoB 2; methodological quality assessment
Results of the risk of bias assessment using the RoB 2 tool for individual RCTs and CRTs are presented in Figures 4a and b, respectively. Five of the six studies presented some concern of bias overall (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008; Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020). The study conducted by Sun and colleagues demonstrated a high risk of bias overall; missing data were imputed with median values which may have resulted in a biased estimate of the assignment to the intervention (Domain 2), and the assessment of a large number of outcomes at many different time points may have resulted in a biased selection of the reported result (Domain 5) (Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021). Due to the nature of most of the included interventions, which made blinding of participants and delivery agents impossible, all trials evaluating THP (including THPP and THPP+), in addition to the AFFIRM intervention, presented some concern of bias in the associated domain (Domain 2) (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008; Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020). All CRTs had some concern of bias regarding randomisation (Domain 1), as there was no confirmation that the allocation sequence had been concealed until clusters were enrolled and assigned to treatment (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008; Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020). Additionally, the original study of the included secondary data analysis by Rahman and colleagues (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008) did not indicate if participants or recruiting staff were blind to allocation status before participants were enrolled into the trial (Domain 1b). The THPP+ trial by Maselko and colleagues presented some concern of bias in Domain 4 due to assessors being blinded to treatment allocation only until the end of THPP at six months but not throughout the remaining 30 months of extended (THPP+) sessions (Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020). Finally, the trials by Rahman and colleagues and Sun and colleagues did not have prespecified protocols (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008; Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021). This may have introduced bias into the selection of the reported result for these three trials (Domain 5) (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008; Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021).

Figure 4. (a) Assessment of risk of bias for individual RCTs included in the review (using RoB 2) (McGuinness and Higgins, Reference McGuinness and Higgins2021). (b) Assessment of risk of bias for CRTs included in the review (using RoB 2 for CRTs) (McGuinness and Higgins, Reference McGuinness and Higgins2021).
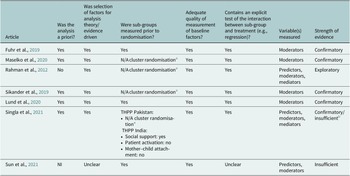
Quality assessment of analysis of predictors, moderators and mediators
Results from the assessment of predictor, moderator and/or mediator analyses may be found in Table 4. Most included reports (n = 5) had a high strength of evidence (‘confirmatory’) in their assessment of predictors, moderators and/or mediators (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019; Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019; Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020; Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020; Singla et al., Reference Singla, MacKinnon, Fuhr, Sikander, Rahman and Patel2021). It is important to note that the secondary mediation analysis of THPP by Singla and colleagues (Singla et al., Reference Singla, MacKinnon, Fuhr, Sikander, Rahman and Patel2021) had a high strength of evidence for mediation analyses, but only in its analysis of data concerning THPP Pakistan, not THPP India, which was deemed as insufficient due to patient activation and mother–child attachment not being measured at baseline. Findings of analyses conducted by Rahman and colleagues are ‘exploratory’ analyses, as analyses of predictors, moderators and mediators were not a priori (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012). Analyses of mediators and predictors of the mindfulness intervention were deemed insufficient. This was mainly due to a lack of explicit information on whether analyses of potential moderators and predictors were a priori, how interactions, particularly between treatment arm and time point, were assessed, and why time since allocation was chosen as a potential moderator (Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021).
Table 4. Quality assessment of moderator, mediator and predictor analyses
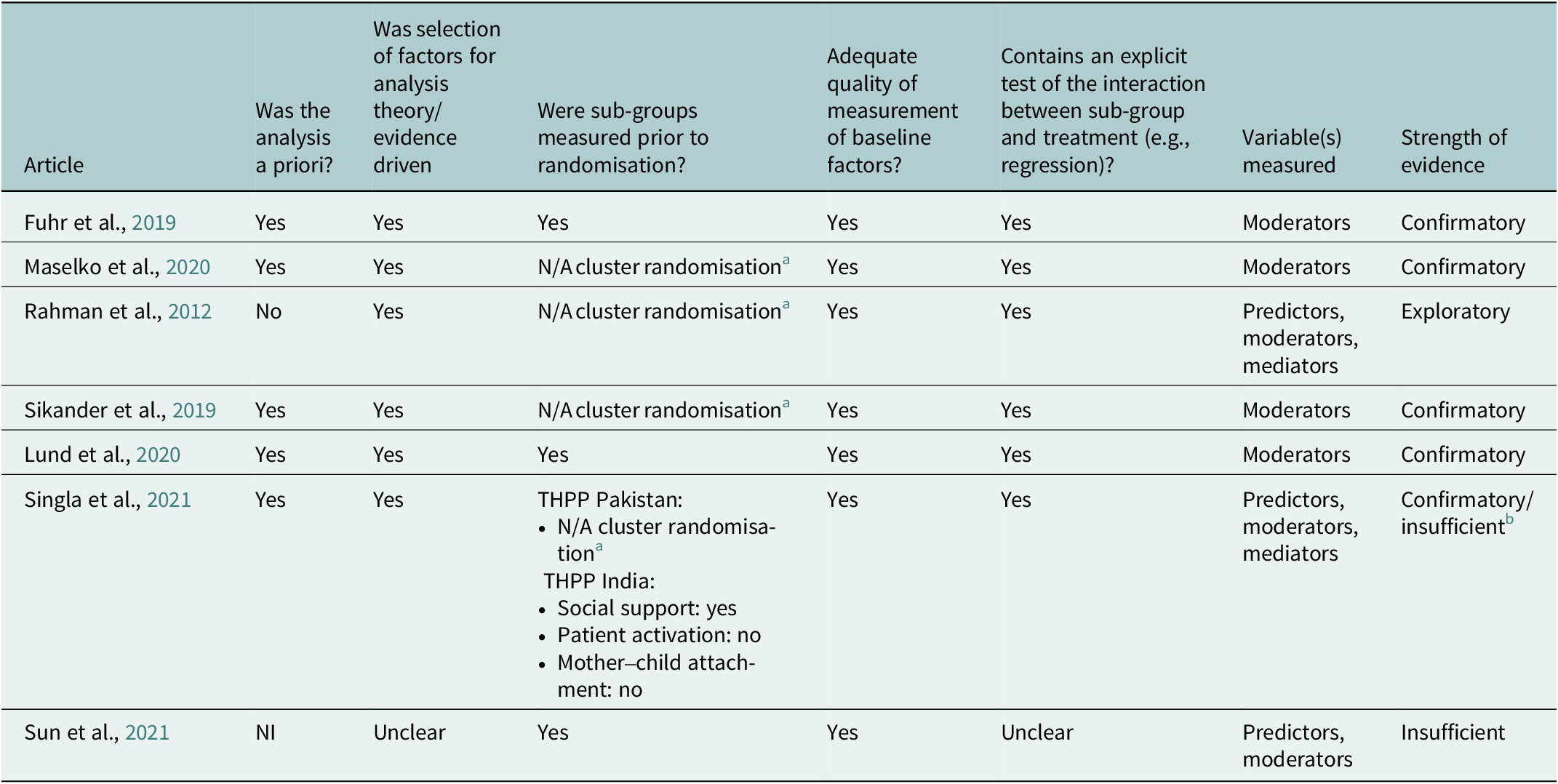
Confirmatory evidence: The study fulfils all of the quality assessment criteria for moderator studies (a priori analysis, factors evidence driven, moderators measured prior to randomisation, adequate measurement of baseline factors and explicit test of the interaction between moderator and treatment).
Exploratory evidence: Fulfilling the last three quality assessment criteria. Insufficient evidence: The studies failed to provide adequate statistical analysis of the moderators.
The study did not carry out an explicit test of interaction or measurement of the sub-groups was reported to take place post randomisation.
Abbreviations: N/A, not applicable; NI, no information; THPP, Thinking Healthy Program Peer-Delivered.
a Due to the nature of CRTs, recruitment, screening and baseline assessments took place after randomisation.
b Analysis is confirmatory for those regarding THPP Pakistan; however, analyses concerning THPP India are insufficient as potential mediators (apart from social support) were not measured at baseline.
The mediation analysis conducted by Singla and colleagues (Singla et al., Reference Singla, MacKinnon, Fuhr, Sikander, Rahman and Patel2021) satisfied 20 of the 25 AGReMA criteria. The missing criteria were due to the article’s omission of the following information: study dates, sensitivity analyses to test causal assumptions, a conflict of interest statement and codes for sharing data. Singla and colleagues measured mediators at distinct time points before the outcome (Singla et al., Reference Singla, MacKinnon, Fuhr, Sikander, Rahman and Patel2021); however, temporality for mediation analyses was not mentioned in the study by Rahman and colleagues (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012). The use of AGReMA for secondary data analyses requires that mediation is the primary focus of the study. As such, it could not be applied to the secondary analysis by Rahman and colleagues as the article’s primary focus was moderation analysis (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012). Although it is explicitly stated in the AGReMA guidelines that they are not meant to be a quality assessment tool, it is worth shedding light on this important set of guidelines in the context of this review as it facilitates transparency behind the mediation analyses presented.
Discussion
In this systematic review, the existing evidence base on predictors, moderators and mediators associated with outcomes of psychological therapies for PND in LMICs was synthesised using a comprehensive search strategy and data extraction process. Investigating predictors, moderators and mediating pathways through which psychological therapies may alleviate depressive symptoms in women with PND has the potential to illuminate which kinds of treatments are best suited for specific needs and contexts.
The combined findings of five original trials and two secondary data analyses included in the review presented evidence on predictors, moderators and mediators. Predictors of a higher depression score at follow-up included high depression score at baseline, low BMI, older age, not being financially empowered, the presence of household debt, having only one child and low-level family support. Moderators of psychotherapy effectiveness included a higher depression score at baseline, a shorter duration of depression at baseline, being in debt and not being financially empowered. Time since treatment allocation was also found to be a moderator of treatment effectiveness, although directionality of effect was not clearly indicated. Finally, mediators of treatment effect included patient activation and social support.
Comparison with existing evidence
Much of the data reported in this review are consistent with the existing evidence base. A body of research has identified links between low socioeconomic status and increased risk of PND (Patel et al., Reference Patel, Rodrigues and DeSouza2002; Abujilban et al., Reference Abujilban, Abuidhail, Al-Modallal, Hamaideh and Mosemli2014), and financial empowerment of women and mental health in general (Kermode et al., Reference Kermode, Herrman, Arole, White, Premkumar and Patel2007). Baranov and colleagues found that women who received the original THP intervention in Pakistan had improved economic outcomes seven years later (Baranov et al., Reference Baranov, Bhalotra, Biroli and Maselko2020). Additionally, a variety of studies have found that low levels of social support may increase one’s risk for PND onset in LMICs (Sawyer et al., Reference Sawyer, Ayers and Smith2010; Dibaba et al., Reference Dibaba, Fantahun and Hindin2013). Data on nutritional status, specifically on low BMI as a predictor of higher depression score, are in line with past research done in LMICs, indicating that depressed mothers are more likely to be underweight than non-depressed mothers (Adhikari et al., Reference Adhikari, Williamson, Sparling, Ferguson and Cunningham2020). Data found on mediators of psychological therapy correspond to evidence from the Health Activation Program trial, in which activation was similarly reported as a mediator of psychotherapy for depression in LMICs (Weobong et al., Reference Weobong, Weiss, McDaid, Singla, Hollon, Nadkarni, Park, Bhat, Katti, Anand, Dimidjian, Araya, King, Vijayakumar, Wilson, Velleman, Kirkwood, Fairburn and Patel2017; Seward et al., Reference Seward, Vansteelandt, Moreno-Agostino, Patel and Araya2023). Finally, social support has been recognised as a mediator of psychotherapy for women in low-resource communities, for instance, amongst economically disadvantaged mothers (Toth et al., Reference Toth, Rogosch, Oshri, Gravener-Davis, Sturm and Morgan-López2013) and mothers in rural Uganda (Singla et al., Reference Singla, Kumbakumba and Aboud2015).
On the other hand, some findings outlined in this review do not support the larger evidence base. Dissimilarly to findings from the AFFIRM Intervention in South Africa (Lund et al., Reference Lund, Schneider, Garman, Davies, Munodawafa, Honikman, Bhana, Bass, Bolton, Dewey, Joska, Kagee, Myer, Petersen, Prince, Stein, Tabana, Thornicroft, Tomlinson, Hanlon, Alem and Susser2020), a recent meta-analysis evaluating findings from RCTs comparing psychotherapy with pharmacotherapy effectiveness found no evidence that baseline depression severity moderated psychotherapy effectiveness (Tröger et al., Reference Tröger, Miguel, Ciharova, de Ponti, Durman, Cuijpers and Karyotaki2024). Interestingly, evidence from pharmaceutical trials have found it may be a predictor of treatment response (Kilts et al., Reference Kilts, Wade, Andersen and Schlaepfer2009). Contrary to former evidence, the secondary analysis by Rahman and colleagues (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012) found that high depression severity at baseline was associated with high depression severity at follow-up. Furthermore, a review on CBT for mood disorders reported that those undergoing psychotherapy with a longer duration of depression at baseline were less likely to relapse compared to those with a shorter duration at baseline (Driessen and Hollon, Reference Driessen and Hollon2010); however, in the THPP India trial, participants with a shorter duration of depression were more likely to respond to the intervention (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019). Additionally, intimate partner violence and low educational attainment were not identified as predictors, even though research on psychotherapies for PND in LMICs indicate the contrary (Gomez-Beloz et al., Reference Gomez-Beloz, Williams, Sanchez and Lam2009; Lara et al., Reference Lara, Natera-Rey, Berenzon, Juárez-García, Villatoro-Velázquez, Nieto and Medina-Mora2014). Furthermore, the data report older age as a predictor of higher depression score, while many other sources of evidence point to younger age as a predictor for PND (Fisher et al., Reference Fisher, Cabral de Mello, Patel, Rahman, Tran, Holton and Holmes2012). In addition, the data contradict past findings that shed light on greater parity as a risk factor for PND (Magalhães et al., Reference Magalhães, de Souza, dos Santos Barros, Eufrásio, do Nascimento Júnior and de Souza Ramalho Viana2021). As mother–child attachment has previously been found to mediate the effect of psychotherapy for PND (Stein et al., Reference Stein, Gath, Bucher, Bond, Day and Cooper1991) and treatment expectations to moderate treatment effect (Kirsch, Reference Kirsch1999), it was surprising that similar findings were not presented here.
Strengths and limitations
Quality of evidence
There were several limitations identified in the included articles. The methodological quality of original trials all presented at least some concern of bias. Participants and delivery agents in all included original trials (and an original trial of one included secondary data analysis) were unblinded to the treatment arm. Additionally, even though randomisation of participants before enrolment is part of the nature of the CRT study design, it results in a sample that is not equally representative of all included clusters. Some of the included articles did not have an openly accessible protocol (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008; Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021), which makes it possible that only favourable results and their corresponding analyses were reported. The trial by Sun and colleagues was of particularly low methodological quality; the imputation of missing values and the large number of analyses conducted mean that findings on the effectiveness of the mobile intervention may have been inflated (Sun et al., Reference Sun, Li, Wang, Chen, Bazzano and Cao2021). Gaps in methodological rigour may have led to biased results of intervention effectiveness on which analyses of corresponding predictors, moderators and mediators were based.
Most analyses of predictors, moderators and mediators were of high quality and explicitly reported by study authors; nonetheless, some analysis results must be regarded with a high level of caution, or even as potentially erroneous, due to unclear methods of analysis and analyses not being a priori. Sun and colleagues, for instance, assessed time for moderation and for triple interaction effects with other variables; methods of assessment were unclear for this particular study. It is also of concern that many of the mediation analyses did not account for the complexity of these trials, including the fact that there were likely multiple mediators with different interactions and non-linearities. Failing to account for this complexity can seriously bias estimates (VanderWeele, Reference VanderWeele2016).
Heterogeneity
Even though all included trials used a randomised design, the data still presented a notable amount of heterogeneity between study methods and characteristics of evaluated interventions. For instance, the number of sessions spanned between six and 32, and intervention duration spanned from two to 36 months. Delivery agents included a mix of lay workers, CHWs and a mobile application. Most therapies utilised BA strategies, but some employed strategies from CBT and MBCT. Even though most trials assigned EUC to the control group, only some of them also assigned EUC to the intervention arm. Furthermore, most trials measured depression using the PHQ-9, EPDS or HDRS; however, cutoff scores varied and so did the number and time points of follow-up assessments. The kinds of mediators captured and the measures used to evaluate them also varied; studies evaluating THPP captured patient activation, social support and mother–child attachment, and measured them through the use of standardised questionnaires (Multidimensional Scale of Perceived Social Support, Premium Abbreviated Activation Scale, Maternal Postnatal Attachment Scale) (Singla et al., Reference Singla, MacKinnon, Fuhr, Sikander, Rahman and Patel2021), whereas the THP trial evaluated changes in household debt and financial empowerment by administering interviews at baseline and follow-up (Rahman et al., Reference Rahman, Sikander, Malik, Ahmed, Tomenson and Creed2012). Finally, unlike in the THPP India trial (Fuhr et al., Reference Fuhr, Weobong, Lazarus, Vanobberghen, Weiss, Singla, Tabana, Afonso, De Sa, D’Souza, Joshi, Korgaonkar, Krishna, Price, Rahman and Patel2019), chronicity of depression was not found to be a moderator of depression remission in the parallel THPP Pakistan trial (Sikander et al., Reference Sikander, Ahmad, Atif, Zaidi, Vanobberghen, Weiss, Nisar, Tabana, Ain, Bibi, Bilal, Bibi, Liaqat, Sharif, Zulfiqar, Fuhr, Price, Patel and Rahman2019) or in the THPP+ Pakistan trial (Maselko et al., Reference Maselko, Sikander, Turner, Bates, Ahmad, Atif, Baranov, Bhalotra, Bibi, Bibi, Bilal, Biroli, Chung, Gallis, Hagaman, Jamil, LeMasters, O’Donnell, Scherer, Sharif, Waqas, Zaidi, Zulfiqar and Rahman2020). Considering that similar findings on treatment effectiveness across both studies demonstrate relatively good validity between the studies, this inconsistent finding is important, as it may shed light on how contextual and cultural factors may influence pathways of recovery and lead to moderating pathways which are specific to the intervention setting.
The review process
One main limitation of the review process was the small number of articles included in the review, which limited the generalisability and interpretability of findings. Nevertheless, the lack of available evidence was not surprising; not only are predictors, moderators and mediators of intervention effect often excluded from psychotherapy research (Kazdin, Reference Kazdin2007), but mental health research capacity in LMICs is still fairly limited despite its continued growth (Patel et al., Reference Patel, Saxena, Lund, Thornicroft, Baingana, Bolton, Chisholm, Collins, Cooper, Eaton, Herrman, Herzallah, Huang, Jordans, Kleinman, Medina-Mora, Morgan, Niaz, Omigbodun, Prince, Rahman, Saraceno, Sarkar, De Silva, Singh, Stein, Sunkel and UnÜtzer2018). Limitations of the review process include the exclusion of papers that did not have full texts in English or that were not published in a peer-reviewed journal. Due to time constraints, it was not possible to search grey literature or translate articles to English. This may have introduced selection bias and publication bias into the review. A full dual-screening was also not possible; however, a perfect inter-rater reliability score verified that the partial dual-screening was still robust. Additionally, two included articles were secondary analyses. Secondary analyses are an important means of exploring predictors, moderators and mediators, particularly as publications of original trial findings often have tight word limits. It was therefore decided that secondary analyses would be included and listed separately from original trials, as not all original trials of respective included secondary analyses were eligible for inclusion in the review.
Despite these limitations, the registration of a prespecified protocol on PROSPERO in addition to the use of the PRISMA statement (Page et al., Reference Page, McKenzie, Bossuyt, Boutron, Hoffmann, Mulrow, Shamseer, Tetzlaff, Akl, Brennan, Chou, Glanville, Grimshaw, Hróbjartsson, Lalu, Li, Loder, Mayo-Wilson, McDonald, McGuinness, Stewart, Thomas, Tricco, Welch, Whiting and Moher2021) and the review guidebook by Boland and colleagues (Boland et al., Reference Boland, Cherry and Dickson2017) to advise the procedures undertaken to conduct this review supported the rigour of this review. Robustness of the review is also evidenced by the use of synonyms and advanced search techniques in the search strategy, the range of databases to which the search (and a preliminary scoping search) was applied, and the complimentary search techniques used (e.g., contacting experts, backward citation searching). Furthermore, detailed inclusion and exclusion criteria developed in line with PICOS and applied using an organised and dually piloted screening tool ensured accuracy during the screening process.
Quality assessment was conducted using two quality assessment tools, including a top-rated tool for randomised trials (RoB 2), to guarantee that assessment was thorough and that it accounted for all details relevant to the review topic. Furthermore, the addition of a second reviewer to pilot the screening tool, dual screen a random selection of articles, and conduct cross-checks on a random selection of extracted data and quality assessments reduced the risk of bias and error introduced into the review. To further reduce the risk of error, experts of the review topic were consulted as needed to cross-check extracted data. The steps taken to ensure robustness in the review bring confidence to the prospect that all relevant data were included and synthesised and that emerging conclusions are based on all available evidence.
Generalisability of findings
While this review sheds light on a number of reported predictors, moderators and mediators of psychotherapies for PND in LMICs, gaps in the amount of available research and in the quality of study methods and analyses limit our interpretability of the data. Nevertheless, data from studies of acceptable methodological and analytical quality highlight the following: patient activation and social support are mediators of psychotherapy effectiveness, high baseline depression severity is a moderator of psychotherapy effectiveness and a shorter duration of depression at baseline is a moderator of the effectiveness of psychotherapy on depression remission.
Despite acceptable quality behind these specific data, a lack in quantity of acceptable data limits the generalisability of these findings. Findings were not collectively supported across all included studies. Rather, each finding was supported by only one included study. This means that the data presented in this review may only be generalised to the particular population, setting and circumstances in which the original trial took place. Therefore, in terms of social support as a mediator of treatment effect for women receiving therapy for PND, it is only reasonable to generalise this finding to those enrolled in THPP who reside in Goa, India or rural Pakistan. Patient activation may also mediate treatment effect, but this may only be for communities in rural Pakistan. Similarly, a shorter duration of depression at baseline may only improve the impact of psychotherapy on PND depression remission for women who are receiving individual sessions of THPP and reside in Goa, India. Furthermore, depression severity at baseline may only moderate psychotherapy effectiveness on PND in women from the peri-urban settlement of Khayelitsha in Cape Town, South Africa, who are receiving a two-month long, problem-solving psychological intervention delivered individually by CHWs.
Recommendations
Findings from the current review highlight the need for future trials exploring the effectiveness of psychotherapies for PND in LMICs to appropriately measure predictors, moderators and mediators of treatment effect. For instance, multiple regression analysis, structural equation modeling, path analysis and bootstrap methods are statistical techniques recommended for evaluating mediators (Kazdin, Reference Kazdin2007). Moderated regression analyses, subgroup analyses and analyses of variance are recommended for the evaluation of predictors and moderators and should be chosen based on the kind of variable being assessed and study characteristics (e.g., dichotomous, continuous, categorical) (Aguinis, Reference Aguinis1995; Helm and Mark, Reference Helm and Mark2012). For instance, researchers carrying out a moderated multiple regression analysis should ensure that sample sizes across subgroups are equal and that the overall sample size exceeds 120 participants to reach a substantial power of effect (Stone-Romero et al., Reference Stone-Romero, Alliger and Aguinis1994; Aguinis, Reference Aguinis1995). Additionally, the use of these analysis methods should be explicitly and clearly reported, along with each variable being assessed as a potential predictor, moderator or mediator to allow for transparency of methodological quality. To facilitate appropriate use and transparency of these procedures, methods of analyses for predictors, moderators and mediators should be standardised using recognised, consensus-based guidelines such as AGReMA, a checklist for mediation analyses (Lee et al., Reference Lee, Cashin, Lamb, Hopewell, Vansteelandt, VanderWeele, MacKinnon, Mansell, Collins, Golub, McAuley, Localio, van Amelsvoort, Guallar, Rijnhart, Goldsmith, Fairchild, Lewis, Kamper, Williams and Henschke2021). Similar tools should be developed to also assess analyses of predictors and moderators. Furthermore, the use of these tools should be recognised and encouraged by peer-reviewed journals and stakeholders involved in the development, evaluation and implementation of mental health interventions in LMICs. Doing so would aid in the development and scale-up of effective treatments for PND in LMICs and potentially alleviate the gap in access to appropriate mental healthcare in this population and setting.
Conclusions
The scarce availability of well-founded evidence presented in this review means that no general conclusions can be confidently made regarding predictors, moderators and mediators of psychological therapies for PND in LMICs. This includes conclusions surrounding specific characteristics of women and their contextual environment that may improve treatment outcomes (predictors), variables associated with pathways of recovery (moderators) or mechanisms that explain why or how psychological therapies for PND may lead to pathways of recovery (mediators).
Nevertheless, the inclusion of only seven articles in this review clearly illustrates the existing evidence gap and the need for further research in this area.
Increased understanding behind these details of psychological therapies for PND in LMICs is crucial to maximising treatment outcomes and increasing treatment coverage in this population and setting. If mental health is indeed a fundamental human right (Patel et al., Reference Patel, Saxena, Lund, Thornicroft, Baingana, Bolton, Chisholm, Collins, Cooper, Eaton, Herrman, Herzallah, Huang, Jordans, Kleinman, Medina-Mora, Morgan, Niaz, Omigbodun, Prince, Rahman, Saraceno, Sarkar, De Silva, Singh, Stein, Sunkel and UnÜtzer2018), steps must be made to reframe mental healthcare in LMICs as a whole. Careful consideration of the evidence and recommendations presented in this review may provide insight on how to do so in the context of psychological therapies for PND.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2024.3.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1017/gmh.2024.3.
Data availability statement
All data relevant to this review are available within the published manuscript and its online supplements.
Acknowledgements
This research was supported by The King’s College Institute of Psychiatry, Psychology & Neuroscience and The London School of Hygiene & Tropical Medicine who provided academic support and access to technological resources required to conduct this review. We are also grateful for the support of Aitor Martinez (A.M.), who acted as a second reviewer.
Author contribution
N.S. led the conceptualisation of the review. A.E. was responsible for the data curation, analysis, investigation, methodology, project administration, visualisation and writing an original draft of the review. This consisted of the development of inclusion and exclusion criteria reflected in a detailed search strategy, conducting a literature search followed by data extraction and writing up a full draft of the methods and findings. N.S. and C.L. equally supervised the whole process, providing guidance and validation of methods, content and visualisation at key stages as needed, including editing and reviewing the original draft by A.E and providing final approval for submission.
Financial support
This work was completed in part fulfilment of the requirements for a Master’s in Science and received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interest
The authors declare no competing interests exist.








Comments
September 13, 2023
Gary Belkin, MD, MPH, PhD
Editor in Chief, Cambridge Prisms: Global Mental Health
Dear Professor Gary Belkin,
Please find enclosed our submission to Cambridge Prisms: Global Mental Health entitled “Predictors, moderators, and mediators of psychological therapies for perinatal depression in low- and middle-income countries: A systematic review.” This manuscript is 35 pages long and includes 4 tables and 4 figures.
This manuscript examines and synthesises the current evidence base for interventions to treat perinatal depression in low-resource settings. Importantly, understanding the predictors, moderators, and mediators of psychological interventions can provide insight on how, under what conditions and for whom effective treatments work. This information can help us understand how these interventions can be optimised for scale up, particularly within settings where a lack of available mental health specialists and a high burden of common mental disorders call for novel approaches to treatment delivery. Optimising interventions for perinatal depression in low resource settings would allow for improved health outcomes for both the mother and the child and ultimately, reduce global inequities in health.
Given the importance of understanding such mechanisms, in addition to the lack of quality of evidence in this area and the rapidly growing body of work to develop and implement scalable mental health programmes in low- and middle-income countries, we felt it was important to synthesise and evaluate the existing evidence base on predictors, moderators and mediators of psychological interventions for perinatal depression, and provide recommendations for future research. As Cambridge Prisms: Global Mental Health publishes papers that aim to play a role in alleviating disparities in access to mental healthcare in a diverse range of settings and contexts, we thought this journal would be the ideal place for this manuscript.
This manuscript is original and has not been published elsewhere. My co-authors and I have no conflicts of interest to disclose with regard to the submitted work. All authors have agreed to the order of authors and to submission of the manuscript in its present form.
I will be the corresponding author for this manuscript. We look forward to hearing from you.
Sincerely,
Alexa Elias, MSc
Flat 72
Tower House
81 Fieldgate St
London
E1 1GU
England
+44 7929715766
[email protected]