Introduction
HIV and depression in sub-Saharan Africa
People living with HIV (PLWHIV) experience mental disorders and psychological distress at a two- to three-fold increased rate compared with the general population (Olatunji et al. Reference Olatunji, Mimiaga, O'Cleirigh and Safren2006; Chibanda et al. Reference Chibanda, Benjamin, Weiss and Abas2014). Of these, major depressive disorder (MDD) is the most common (Dubé et al. Reference Dubé, Benton, Cruess and Evans2005), with a reported prevalence ranging from 11% to 38% in sub-Saharan Africa (SSA) (Gaynes et al. Reference Gaynes, Pence, Atashili, O'Donnell, Njamnshi, Tabenyang, Arrey, Whetten, Whetten and Ndumbe2015). PLWHIV who are also living with comorbid MDD can experience impaired psychosocial functioning and quality of life (Preau et al. Reference Preau, Bonnet, Bouhnik, Fernandez, Obadia and Spire2008; Carrico et al. Reference Carrico, Bangsberg, Weiser, Chartier, Dilworth and Riley2011; Chen et al. Reference Chen, Shiu, Yang and Simoni2013). Furthermore, comorbid MDD has been associated with reduced motivation to seek health care, impaired initiation and adherence to treatment, and increased mortality in PLWHIV (Safren et al. Reference Safren, Otto, Worth, Salomon, Johnson, Mayer and Boswell2001; Cook et al. Reference Cook, Grey, Burke, Cohen, Gurtman, Richardson, Wilson, Young and Hessol2004; Pence, Reference Pence2009; Mayston et al. Reference Mayston, Kinyanda, Chishinga, Prince and Patel2012; Rane et al. Reference Rane, Hong, Govere, Thulare, Moosa, Celum and Drain2018). Despite the abundance of evidence, MDD remains underdiagnosed and undertreated in PLWHIV (Freeman et al. Reference Freeman, Patel, Collins and Bertolote2005; Seedat et al. Reference Seedat, Stein, Herman, Kessler, Sonnega, Heeringa, Williams and Williams2008; Kagee & Martin, Reference Kagee and Martin2010; Pence et al. Reference Pence, O'Donnell and Gaynes2012; Marinho et al. Reference Marinho, Mota-Oliveira, Peixoto, Marques and Braganca2016; World Health Organisation, 2017). The expansion of HIV treatment initiatives into low- and middle-income countries (LMICs) of SSA, a region with an estimated 25.5 million people infected with HIV who represent 69% of global prevalence (UNAIDS, 2016), provides an opportunity to integrate mental health services into existing programmes (Freeman et al. Reference Freeman, Patel, Collins and Bertolote2005; Collins et al. Reference Collins, Holman, Freeman and Patel2006).
Integration of care
Integrated care for coexisting illnesses, especially physical and mental disorders, has proven to be practical and more cost-effective than separate disease care (Katon et al. Reference Katon, Lin, Von Korff, Ciechanowski, Ludman, Young, Peterson, Rutter, McGregor and McCulloch2010; Jenkins et al. Reference Jenkins, Baingana, Ahmad, Mcdaid and Atun2011). Leveraging already existing HIV treatment facilities and programmes to integrate mental health care would expand the resource base, awareness and management of mental disorders (Freeman et al. Reference Freeman, Patel, Collins and Bertolote2005). In fact, integrating mental health into HIV services was recommended by the very first global HIV treatment initiative, ‘Treat 3 Million by 2005’ (‘3 by 5’). The ‘3 by 5’ initiative acknowledged that a successful HIV intervention programme must include the assessment of mental disorders as part of the normative service (WHO, Reference Who2003; Freeman et al. Reference Freeman, Patel, Collins and Bertolote2005). Screening for comorbid MDD in routine care is essential to mental and physical health outcomes for PLWHIV. Treatment of MDD is one of the best interventions for reducing adherence attrition that often accompanies clinical depression in PLWHIV (Krumme et al. Reference Krumme, Kaigamba, Binagwaho, Murray, Rich and Franke2015). However, many HIV services have taken on a vertical nature, with clinics solely focused on HIV and separated from all other treatments (Mahomed et al. Reference Mahomed, Asmall and Freeman2014). This has resulted in inefficiencies in the health care delivery system as well as a missed opportunity to strengthen not only HIV services but also to promote mental health in all primary care services (Freeman et al. Reference Freeman, Patel, Collins and Bertolote2005; Mahomed et al. Reference Mahomed, Asmall and Freeman2014).
eMental Health
The shortage of providers trained to deliver mental health screening and treatment in primary care, particularly in LMICs (Saxena et al. Reference Saxena, Thornicroft, Knapp and Whiteford2007; Naslund et al. Reference Naslund, Aschbrenner, Araya, Marsch, Unützer, Patel and Bartels2017), calls for creative solutions to be implemented. Task shifting – training non-physician healthcare workers to perform tasks traditionally undertaken by physicians – when also accompanied by appropriate health system re-structuring, is a potentially effective and affordable strategy for improving access to health care (Hongoro & McPake, Reference Hongoro and Mcpake2004; Callaghan et al. Reference Callaghan, Ford and Schneider2010; Joshi et al. Reference Joshi, Alim, Kengne, Jan, Maulik, Peiris and Patel2014). However, in LMICs with substantial staff shortages and failing health systems (Callaghan et al. Reference Callaghan, Ford and Schneider2010), non-physician healthcare workers are overburdened and may not be able to take on more responsibility (Calpin-Davies & Akehurst, Reference Calpin-Davies and Akehurst1999; Ojikutu, Reference Ojikutu2007; Van Rensburg et al. Reference Van Rensburg, Steyn, Schneider and Loffstadt2008). Therefore, traditional task shifting alone will not solve human resources problems in HIV services (Callaghan et al. Reference Callaghan, Ford and Schneider2010). In areas with an absolute shortage of all levels of staff, shifting mental health screening to technology, assisted by lay health care workers (non-medical staff) (Naslund et al. Reference Naslund, Aschbrenner, Araya, Marsch, Unützer, Patel and Bartels2017), may make screening and early detection of mental health conditions more feasible. The use of information technology to improve access to and the delivery of mental health care is known as eMental Health (Wise, Reference Wise2017; Wozney et al. Reference Wozney, Newton, Gehring, Bennett, Huguet, Hartling, Dyson and McGrath2017).
Computerised neuropsychological assessment devices (CNAD) are being increasingly used for large-scale eMental Health screenings both in high- and low-income settings (Bauer et al. Reference Bauer, Iverson, Cernich, Binder, Ruff and Naugle2012; Tomita et al. Reference Tomita, Kandolo, Susser and Burns2016). A CNAD is an instrument that utilises a digital interface instead of a human examiner to administer, score or interpret tests of brain function or neurologic health and illness (Bauer et al. Reference Bauer, Iverson, Cernich, Binder, Ruff and Naugle2012). For example, a study conducted in South Africa used a text-messaging application to successfully screen for depression in refugees (Tomita et al. Reference Tomita, Kandolo, Susser and Burns2016). CNADs have several advantages over traditional screen practices, including increased portability, decreased administration time and minimised examiner influence on participant performance (Bauer et al. Reference Bauer, Iverson, Cernich, Binder, Ruff and Naugle2012). However, CNADs should be viewed as a ‘resource’ for health workers, rather than as a ‘substitute’ (Bauer et al. Reference Bauer, Iverson, Cernich, Binder, Ruff and Naugle2012) and should not undermine the need for human resource development in mental health.
To the authors’ knowledge, considerations around implementing a digital screening tool to effectively screen and reliably diagnose depression in PLWHIV in a LMIC context have not been examined. A Theory of Change (ToC) approach was utilised as an evidence-based tool to assess the viability and acceptability of integrating an eMental Health screening intervention into an HIV primary health care settings in South Africa.
Method
Study design
This formative study, using the ToC framework, was conducted through individual interviews and a group session. ToC is a qualitative method of research used to describe the causal pathways through which a programme is hypothesised to have an effect (Breuer et al. Reference Breuer, De Silva, Fekadu, Luitel, Murhar, Nakku, Petersen and Lund2014). The workshop and interviews had three aims: (1) to conceptualise a contextually relevant and informed digital screening tool as an intervention; (2) to initiate buy-in from key stakeholders; and (3) to construct a ‘ToC map’ as a visual depiction of the pathways to change (Breuer et al. Reference Breuer, De Silva, Fekadu, Luitel, Murhar, Nakku, Petersen and Lund2014). In this study, digital depression screening for HIV-positive patients was referred to as Mood in Retroviral Positive Individuals Application Monitoring (MIR + IAM).
Ethical approval was obtained from the Human Research & Ethics Committee of the University of Witwatersrand, South Africa (Ref: M16067). Written informed consent was obtained from all study participants. Experts for individual interviews were drawn from the London School of Hygiene & Tropical Medicine and the Institute of Psychiatry, Psychology and Neuroscience, King's College London. Ethical approval to conduct ToC interviews and collect professional opinions from academic staff was not required by their ethics committees. Permission was obtained through email contact with the head of department at the respective institutes.
Study setting and population
A ToC is developed in consult with key stakeholders and experts in workshops or interviews (Mason & Barnes, Reference Mason and Barnes2007). Stakeholders are individuals who might be involved in the implementation of the intervention or who might be affected by the intervention (Breuer et al. Reference Breuer, De Silva, Fekadu, Luitel, Murhar, Nakku, Petersen and Lund2014). The selection criteria for stakeholders included HIV health care service providers and working professionals or academic researchers in the fields of mental health, HIV, health systems or digital technology. The group ToC session was facilitated by RVP and NB in a staff room at the HIV clinic in Charlotte Maxeke Johannesburg Academic Hospital, South Africa. Permission was granted by the clinical head of department and all clinic staff were invited to attend the session. The individual interviews were conducted telephonically or face-to-face by RVP in a private meeting space. Individual participants were selected on the basis of global expertise in the respective fields of global mental health, health systems, digital technology and mental health in HIV.
Data collection
The group ToC session was conducted for an hour and each individual interview was conducted for 30 min. Facilitators used the basic concept of a digital depression screening tool to initiate the ToC discussion. The discussion started with the presumed impact of the intervention and worked backwards to cover all the domains of the ToC including long- and short-term outcomes, treatment, identification, resources and capacity. As the discussion moved through the ToC pathway, participants were asked to identify rationales, assumptions, interventions and possible methods of evaluation (indicators) for MIR + IAM. The individual interviews addressed the same domains. However, because individual interviews were only conducted for 30 min, questions were directed towards the interviewees’ expertise. Online Supplementary Appendix 1 describes specific questions used during each interview. Data saturation was achieved when no new themes emerged from the individual or group interviews and ToC (Fusch & Ness, Reference Fusch and Ness2015). Data were collected through process documentation, including participant lists, minutes and physical notes used to plot participant ideas.
Analysis
Field notes were transcribed, imported into Atlas.ti version 7.5.18 (Friese, Reference Friese2013) and analysed using a thematic approach. A list of a priori codes, derived from the conceptual framework of the ToC, were used to initially categorise the data. Later, these codes were refined into sub-themes or expanded into larger themes (Gibbs, Reference Gibbs2008). A chart was constructed with the final themes from the participant views. The ToC map was constructed using the chart to justify the pathway to effect. The initial coding was developed by IDE and RVP independently; differences were resolved through discussion and finalised by co-authors.
Results
Characteristics of study participants
Individual interviews were conducted with study participants in the UK from September to October 2016. These participants included one academic in the field of health systems, one mental health and HIV researcher, one psychiatrist working in the field of depression in LMICs with a focus on PLWHIV and, one expert in digital technology. The group ToC workshop took place in March 2017. Six clinic staff attended the session including two HIV care nurses, two infectious disease resident physicians and two infectious disease consultant physicians.
ToC pathway to change: rationale, outcomes and impact
The ToC map summarises our findings and plots the pathway to change (Fig. 1). The study participants unanimously agreed that, if adopted and implemented to scale, MIR + IAM has the potential to improve the diagnosis and treatment of depression in PLWHIV in South Africa. The long-term outcome would integrate screening, diagnosis and treatment of depression into HIV clinics. Early detection of depression can have a significant impact on successfully treating depression, HIV and other chronic comorbidities by streamlining the process of entering mental health systems and enhancing geographical and clinical integration of treatment. The participants identified a strong rationale for the intervention because MIR + IAM targets a vulnerable population with a known elevated risk for and prevalence of depression. Health care practitioners in the group ToC acknowledged that medical practice should keep up with the digital trends of other professional fields. Furthermore, mobile and digital device use in Africa is high, indicating potential acceptance of a digital intervention in SSA. Little stigma exists within the HIV clinic between patients, thereby making the clinic a practical setting for a screening intervention. The six themes that emerged from the ToC framework are presented in Table 1 and discussed below.
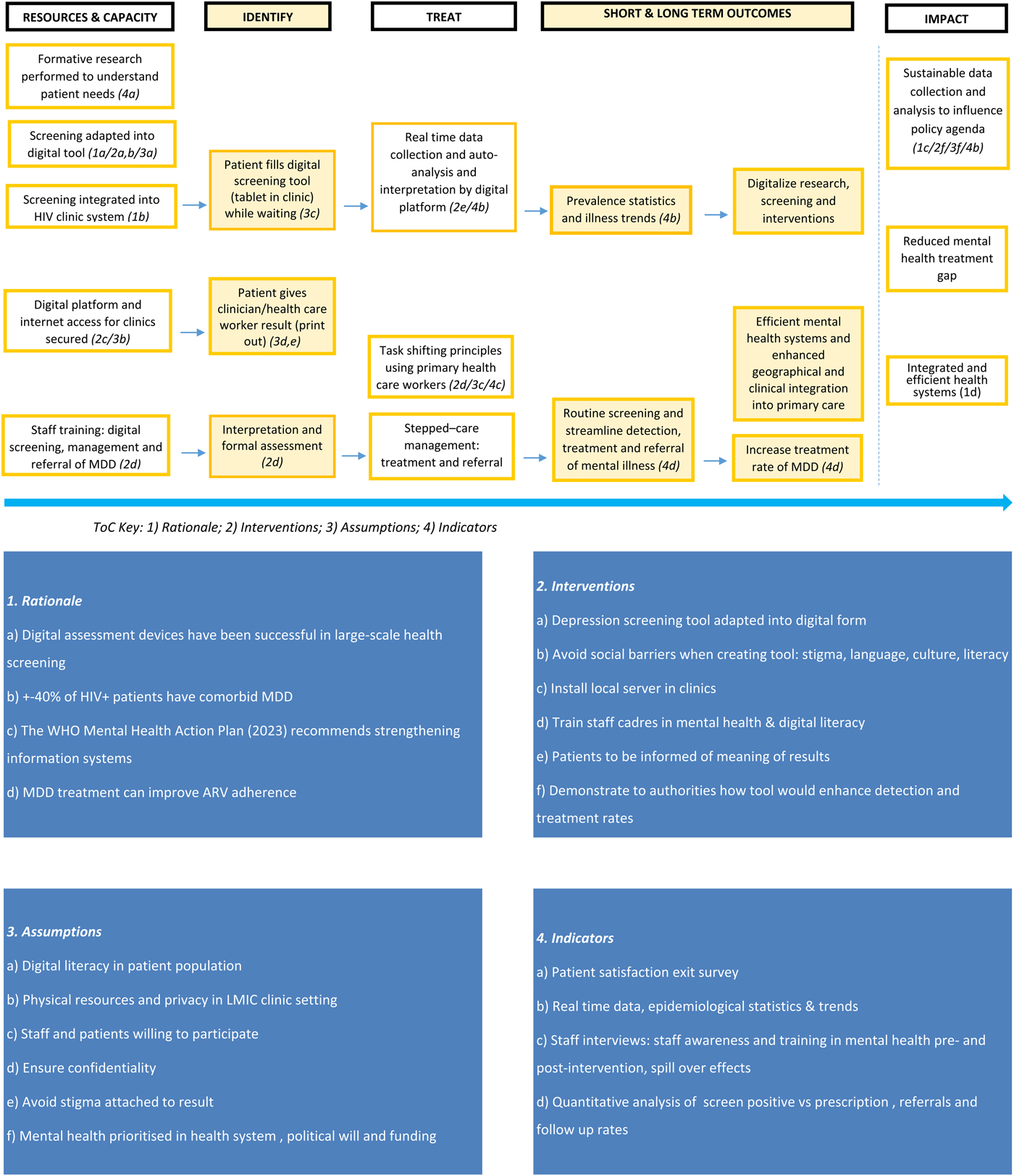
Fig. 1. Theory of Change.
Table 1: ToC Framework & Themes
(1) Centring user experience: target population, acceptability and privacy
The participants in the group ToC suggested that the intervention could be targeted at both adults and adolescents, and that the intervention should consider high-risk groups such as newly diagnosed patients. Extensive formative research with service users is required to inform the intervention. This research could be conducted through patient focus groups to discuss user expectations of the intervention, preferred information delivered by the intervention, and user perspectives on entering mental health data into a digital tool.
The introduction of digital depression screening to the patients and their acceptance of the intervention is a rate-limiting step to this intervention. Firstly, it is essential that HIV patients with comorbid depression accept their HIV status and demonstrate willingness to access care. Secondly, according to the health system expert, patients would require basic digital literacy skills and must be willing to input their data into a digital survey. The interviews surfaced the assumption that, in order for MIR + IAM to have uptake, the tool is confidential and data-secure. This assumption rests heavily on the health care workers and the security protocols of the digital tool; this assumption could limit patients’ acceptance of intervention use. The digital technology expert recommended that data should be unidentifiable, requiring no name or patient number to be entered by the service user into the screening device. Lastly, family or caregiver support was recognised as pivotal to patients’ acceptance of the intervention. Thus, the starting point of the intervention should centre the patients’ needs, and technology ought to be adapted to fit those needs.
The screening tool should have the capacity to screen a patient successfully based on self-imputed data. Therefore, the MDD screening tool used must be validated in the culture and language of the region, and the technology built should be informed by service users. In regard to the presentation of a patient's results, two schools of thought arose. Firstly, some experts agreed that it might be beneficial to give results as a symbol (e.g. red fruit to symbolise high risk) or number, to avoid stigmatisation. Secondly, other experts acknowledged that often patients talk openly among themselves at the clinic, and deserved to receive immediate and explicit information about their screening result. Ultimately, rather than relying on patients to memorise their result, the participants in the group ToC agreed that results from the screening need to be physically recorded and added to patient's health records.
Lastly, adverse local cultural perceptions of MDD and digital screening (i.e. stigma) could be another barrier to implementation. The cultural and social differences between the patients and the other actors (e.g. nurses, clinicians, technical engineers) may impede acceptance of MIR + IAM. This includes social barriers such as poverty, language and digital literacy. In addition to the human and cultural barriers, barriers emanating from the illness experience (depression) might predispose the patients to higher levels of stress that may dampen motivation to accept the intervention.
(2) Optimizing the digital tool: data collection and health promotion
The digital technology expert suggested that the ‘backend’ of the tool [the technology that powers the components which enable the user-facing side of the website to exist (Wales, Reference Wales2014)] should provide real-time data collection, auto-analysis and interpretation by a digital platform. This would provide current statistics to be used as key epidemiological indicators. Again, different views were expressed regarding patient data collection. Some participants thought the data should be anonymised and used as epidemiological statistics (e.g. prevalence trends), while others suggested that data on each patient be specific and followed up. Linking the digital tool with patient electronic health records would create a monitoring system for patient retention, treatment and outcomes, thus expanding the intervention beyond screening which could lead to improved continuity of care. Furthermore, participants described additional screening mechanisms for the digital tool, such as identifying those at risk for hypertension and diabetes.
Participants in the group ToC suggested that the incorporation of MDD screening into the HIV clinic could enhance health promotion, e.g. by introducing routine educational talks on MDD while patients wait (often for long periods) to be seen by a physician in the clinic. Furthermore, the digital platform opens an opportunity to provide primary illness prevention via virtual education incorporated into the screening tool. Creating an innovative digital tool that is patient-centred ultimately increases opportunities for health and mental health promotion among patients.
The health system expert recommended that the success of the screening tool can be assessed by quantitative analysis of the number of screen-positive results v. the number of prescriptions written and treatment dispensed. Additional indicators of successful implementation include symptom relief, admissions, treatment adherence, follow-up rates, satisfaction and patient perspectives of screening evaluated through patient exit surveys. Intermediate indicators may take up to 6 months to generate. Overall, an increase in detection of depression would be the most pivotal indicator of success as no previous method for detection was in place.
(3) Promoting access to treatment: principles of justice
The assumption that health care workers would be willing to educate, treat or refer a patient who screens positive for depression is integral to the uptake and success of the intervention. After screening positive, patients must have access to immediate MDD formal assessment and treatment by a trained member of staff (of any cadre). The provision of formalised detection and care of MDD is critical to the ethical principle of justice, where a screening tool should not be provided without adequate treatment available. The mental health and HIV researcher, as well as participants of the group ToC, recommended a stepped care method of treatment, with patients receiving a level of care matched to their individual needs (e.g. counselling, psychology, medication and/or referral). To facilitate this, a protocol with the correct pathways to treatment needs to be provided.
(4) Building capacity: physical, human and social resources
The need for physical resources surfaced through the interviews, including the digital tool itself, a method of recording results of the screening and space to conduct the screening. A private area, e.g. in the room where each patient has their vital signs recorded, will be required to conduct screening. The digital tool could be provided by the clinic, or patients could access the screening programme using their personal mobile devices. The psychiatrist suggested that a paper-based screening tool should also be considered as an option. The digital technology expert considered a digital tool which used a web-based platform to be the most practical resource because of its ‘responsiveness’, allowing users to access the screening tool with any device that has Internet access and for technicians to update the screening tool remotely. However, within the clinic, the digital tool should function regardless of Internet connection, and be able to store data until it can be uploaded onto a data-secure central server or ‘cloud’ system. Installation of the local server and storage capacity for the offline devices should be considered in remote areas. However, the digital technology expert explained that the amount of physical resources required would vary depending on the scale of the programme. A printing machine would be required to print results. This takes the burden of remembering their result off the patient and creates a hard copy for medical practitioners to keep a record of the patient's depression screening results. Practical barriers to consider in the context of a LMIC clinic include poor Internet availability (i.e. lack of access to personal data or Wifi) and storage capacity at local facilities. Furthermore, the lack of data safety may be a barrier since privacy within a crowded clinic can be compromised and digital tools may be liable to theft.
Another fundamental barrier highlighted was the heavy workload for staff in primary care. MIR + IAM is dependent on the assumption that primary health workers are capable of screening for depression and administering medications. Therefore, human resources would be needed for training and supervising lay health care workers to allow for successful task shifting. Additionally, the creation of a digital tool or ‘application’ requires expert skill and human resources. However, according to the digital technology expert, with a team of developers, the basic client face of the programme could be created in a very short span of time (about 5 days). The basic backend of the programme which manages security settings, credentials, user information, etc., could also be designed in a relatively short time (about 10 days).
Organisational culture was considered to be a possible barrier to implementation for multiple reasons. Critically, mental health is not currently on the health systems agenda, and a patient's physical illness often takes priority in time and resource restricted settings. An additional concern mentioned by the health systems expert was the possible tension created by cultural differences among various sectors involved with the digital screening tool. Programmers, medical staff and policymakers all have different agendas, schedules and methods of working on the tool. However, trust-building and the intersectoral collaboration is achievable if space to promote open communication, both informal and formal, is created between sectors (e.g. weekly reviews of the intervention process with clinic staff). Furthermore, community engagement, family support and local non-governmental organisations represent important social resources.
(5) Training: task shifting
Because MIR + IAM would be integrated within an existing clinic, its success would depend on health care workers as the primary human resource. One of the main barriers highlighted was the heavy staff workload in primary care. Principles of task shifting could be used to allow multiple cadres of health workers from the clinic to serve as human resources for the implementation of the intervention. Nurses were identified as the most feasible actors to implement the intervention. Multiple cadres of staff could be trained to use the digital screening tool, in order to better diagnose and treat MDD, followed by ongoing clinical supervision. The psychiatrist noted that this would require task shifting principles, again informed by formative research, to ensure the intervention fits the needs of the service providers. Staff interviews would also generate useful indicators of staff interest, workload perceptions and attitude about work. The willingness of the health care workers serves as a key indicator of success. This would be demonstrated in the agreement between screening results and trends in depression treatment of identified patents. According to the psychiatrist, the tool could be used to generate statistics on staff performance by comparing screening, referral and treatment records. The impact of such analyses may improve implementation and intervention research in the field of HIV and MDD.
(6) Generating interest: demonstrating usefulness
Both the mental health and HIV researcher as well as the health systems expert noted the importance of generating conversation, creating awareness and planting the seed of interest in the health workers through appropriate communication channels. Securing interest from the ‘top’, i.e. government health agencies, would be just as vital as gaining commitment from intermediate-level managers. Ideally, a senior leader would ‘champion’ the cause, take accountability and regularly inquire about the implementation of the intervention. Practical outcomes surfaced in the interviews included political and funder buy-in for the initiation of a pilot study and future scale up.
Outcomes of the intervention – measurable by data generated on clinical improvement and prevalence statistics – could demonstrate usefulness and encourage interest in the intervention. Such data may include short-term outcomes, e.g. symptom relief, admission, treatment adherence and improved care/satisfaction, or long-term outcomes, e.g. suicide prevention and adherence HIV treatment. Data collected by MIR + IAM could lead to overall improvement on health indices as a result of information generated by the screening tool. The mental health and HIV academic expert suggested that the data gathered could be used in the future planning of health care for patients with both depression and HIV. These data could also provide insight on the patients’ perception of services and care for further formative research.
Discussion
This study aimed to conduct formative mental health systems research on the implementation of routine depression screening, using a digital platform, in HIV primary care in South Africa. The research covered expectations of impact, outcomes, interventions, resources, assumptions, indicators and rationale through a ToC framework. The research participants determined that using a digital screening tool to identify patients with MDD in HIV care services is relevant for the improvement of mental health in this population. The themes highlighted through the ToC process focused on several key areas: (1) user experience with the digital tool, MIR + IAM, including acceptability by patients; (2) utilisation of the tool for data and educational purposes while addressing the barriers of confidentially and privacy; (3) access to treatment; (4) resource capacity; (5) training through task shifting; and (6) generation of interest in the intervention.
User experience is fundamental to the success of the digital screening tool. Creating a well-designed, culturally and linguistically appropriate tool will help to ensure the engagement of patients who are inputting data on their own. Making the tool user-friendly for a variety of ages, languages and cultural perspectives may address the issue of acceptability across a diverse patient population. Expert participants emphasised the importance of patients receiving their results instantaneously and keeping the information in patients’ electronic records for future clinical reference. Storing patient data electronically can streamline information for more efficient coordination of care and treatment (Bates et al. Reference Bates, Saria, Ohno-Machado, Shah and Escobar2014). Furthermore, providing immediate results to patients will promote autonomy to make decisions around their diagnosis. When providing results to patients, MIR + IAM can be used as a digital platform for educational purposes to inform service users about clinical depression and its impact on functionality. The digital screening tool could achieve not only point-of-care monitoring, but also could incorporate health promotion. Increasing mental health literacy in PLWHIV may reduce stigma around mental illness in this population and promote early detection of MDD symptoms in other patients. Combining screening and health promotion would improve operational efficacy of primary health systems and address issues such as patient flow. However, these findings need to be confirmed in larger samples or future systematic reviews. Adopting a holistic approach to prevention, detection and treatment would ensure that patients are treated as individuals and not as disease entities (Mahomed et al. Reference Mahomed, Asmall and Freeman2014).
An additional use of the digital tool described during the study is data collection for several uses, including epidemiological research, records of mental health symptoms, and monitoring of treatment processes and outcomes for patients’ electronic records. The vertical nature of HIV services has resulted in a strong emphasis on the collection of data for HIV outcomes (Mahomed et al. Reference Mahomed, Asmall and Freeman2014). Integration of mental health into the existing data culture and structure presents an enormous opportunity to ensure information for service improvement. Epidemiological research is particularly valuable in primary care because of the lack of policy-relevant information in LMICs (Tomlinson et al. Reference Tomlinson, Rudan, Saxena, Swartz, Tsai and Patel2009). This information could thus be used to generate interest from policymakers and funders and to advocate for mental health provisions. The use of the digital tool to gather and analyse such data aligns with the World Health Organisation's goals to strengthen information systems, evidence and research for mental health (World Health Organisation, 2013). Furthermore, streamline translation into policy, programmes and practice should be prioritised to realise change (Passchier, Reference Passchier2017). However, when collecting sensitive information from patients, protecting private and confidential information is critical to building and maintaining trust. The use of mobile or digital tools in health and mental health requires additional measures to secure sensitive information.
Training lay health workers to use eMental Health may reduce the mental health screening burden on health providers and make diagnosis and treatment more feasible in low-resource settings (Mendenhall et al. Reference Mendenhall, De Silva, Hanlon, Petersen, Shidhaye, Jordans, Luitel, Ssebunnya, Fekadu and Patel2014; Naslund et al. Reference Naslund, Aschbrenner, Araya, Marsch, Unützer, Patel and Bartels2017). As South Africa moves towards a universal health care system, technological tools will help to create a public health care infrastructure that is efficient, equitable and able to accommodate the needs of health care users (Fusheini & Eyles, Reference Fusheini and Eyles2016). There is a growing global consensus that health systems should evolve to harness the potential of technology (Wozney et al. Reference Wozney, Newton, Gehring, Bennett, Huguet, Hartling, Dyson and McGrath2017). However, leveraging digital tools and task shifting to readily screen and diagnose depression in HIV patients may dramatically increase the number of patients that will require mental health care. Therefore, screening should be recognised as only the first step, and access to treatment for those identified with MDD is essential (Krumme et al. Reference Krumme, Kaigamba, Binagwaho, Murray, Rich and Franke2015). We note the critical importance of aligning the implementation of MIR + IAM with health care administrators and government leadership to ensure that there are adequate mental health services available to address the clinical needs of patients (Padmanathan & De Silva, Reference Padmanathan and De Silva2013). Therefore, social and physical resources are crucial considerations when assessing the feasibility of implementing digital tools in primary care settings. To successfully realise implementation, buy-in from mental health service providers, health care leadership and policymakers will be required. This buy-in could be won by generating interest through demonstration of the intervention's utility through pilot studies, data collection and evaluation.
Integration of mental health into primary health care services was outlined by the WHO Mental Health Action plan 2013–2020 (World Health Organisation, 2013; Marais & Petersen, Reference Marais and Petersen2015). The South African National Mental Health Policy Framework and Strategic Plan 2013–2020 (Department of Health Republic of South Africa, 2013) followed with a call for Integrated Chronic Disease Management (Asmal & Mahomed, Reference Asmal and Mahomed2014) and an emphasis on vulnerable populations, such as PLWHIV (Stein, Reference Stein2014). There is a need to develop models for the delivery of mental health care based on the principles of affordability, acceptability and availability, as detailed by the ‘3 in 5’ Mental Health task team (WHO, Reference Who2003; Freeman et al. Reference Freeman, Patel, Collins and Bertolote2005; Mahomed et al. Reference Mahomed, Asmall and Freeman2014). The use of technology in primary care settings is an opportunity to address the mental health gap in HIV primary care services. Using eMental Health may alleviate the burden of detecting and diagnosing depression in low-resource care settings that lack mental health practitioners. However, understanding and being responsive to the complexity of local realities, interests and contexts is essential for implementing a new strategy (Lehmann & Gilson, Reference Lehmann and Gilson2012).
Limitations
Because ethical clearance for patient participation was not obtained, we were unable to include service users in the ToC. The lack of service user involvement is the most significant limitation of this study. Health system research should ensure that the policies and programmes that are put in place are responsive to the needs of health care users (Marais & Petersen, Reference Marais and Petersen2015). This key consideration was reiterated by the participants who called for further insight from service users. As Bishai et al. acknowledge, ‘people who own the problem can anticipate the most likely social obstacles to its resolution, and their participation is essential,’ (Bishai et al. Reference Bishai, Ghaffar, Kelley and Kieny2015). A second group of key stakeholders that could have been included at this early stage was government officials from the Department of Health. These actors can exert valuable power over implementation of health policy, ranging from authoritative power – derived from hierarchy and budget control – to mid-level decisions to grant labour and training resources (Lehmann & Gilson, Reference Lehmann and Gilson2012). The value of engaging government stakeholders was noted as a key lesson in the PRIME ToC workshops, where the support of policymakers was necessary to add legitimacy to the workshops and increase the likelihood of implementation of the intervention (Breuer et al. Reference Breuer, De Silva, Fekadu, Luitel, Murhar, Nakku, Petersen and Lund2014). In South Africa, where mental illness is a low priority and managerial and planning capacity to develop and implement mental health care plans is weak (Marais & Petersen, Reference Marais and Petersen2015), involvement of government stakeholders might increase the likelihood of intervention uptake in primary care services.
Another limitation is the limited participation by lower level staff in the group ToC workshop, potentially due to the hierarchical nature of service providers in the local health system (Breuer et al. Reference Breuer, De Silva, Fekadu, Luitel, Murhar, Nakku, Petersen and Lund2014). Composition of workshops should strike a balance with staff members of different levels to promote open engagement among varied participants (Breuer et al. Reference Breuer, De Silva, Fekadu, Luitel, Murhar, Nakku, Petersen and Lund2014). Seeking participation from high-level professionals through focused interviews allowed us to stratify participants and gain international opinion. However, because the interviews and the workshop were conducted separately, the development of the ToC map was fragmented. The final ToC was culminated at the discretion of the same researchers who ran the workshops. This may have resulted in biased view of the ToC with an overestimation of the viability and usefulness of the intervention. The final ToC map is therefore not entirely ‘owned’ by all the participants, as recommended by the Aspen Institute (Roundtable, Reference Roundtable1997; Breuer et al. Reference Breuer, De Silva, Fekadu, Luitel, Murhar, Nakku, Petersen and Lund2014).
Furthermore, this study is limited by the sample size of 10 participants. Input from a larger group of participants would have possibly elicited greater insights, and increased participation should be encouraged in future studies through vigorous reminders to staff. However, while the study's sample size was low, the quality and power of the information proved by the participants was high, as all participants were directly involved in fields relevant to the study's narrow aim of conducting formative research through a ToC approach (Malterud et al. Reference Malterud, Siersma and Guassora2016). Lastly, the interviews and group ToC were not audio recorded; therefore, the use of quotations from participants was not included in the results. Though the researchers took careful written notes, actual quotes would have increased the data quality of this study.
Conclusion
Comorbid depression for PLWHIV has been the subject of extensive research; however, little action has been taken to address this unmet health care need. In SSA, where the burden of HIV and its associated morbidity is dangerously high, integrating mental health into HIV primary care services is, undoubtedly, a critical component of treatment for sustainable improved HIV outcomes. Formative research with key stakeholders and experts suggests that routine digital depression screening and mental health data collection through automated analysis is both a desirable intervention and a practical service that could improve the mental and physical health of PLWHIV. Careful consideration of the local health system's capacity, including facilities, health care workers and patients, is required. This evidence, though promising, is preliminary. Future research to refine the intervention should be informed by service users and should ensure buy-in from key decision-makers.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/gmh.2018.35
Acknowledgements
Thank you to the experts who contributed to this body of knowledge: Rosie Mayston; Melanie Abas; Helder Oliveira and Dina Balabanova. Thank you Dr Sarah Stacey and the medical team at Charlotte Maxeke Johannesburg Academic Hospital HIV clinic. Thank you Dr Alex Cohen for your teaching and inspiration in Global Mental Health. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Interest
None.




