Impact statement
Population aging has been taking place rapidly in Bangladesh. The country has one of the fastest-growing aging populations in Southeast Asia. Geriatric depression has become a leading mental health problem among older adults, particularly in rural areas. This study examined the relationship between depression and cognitive social capital among rural older adults in Bangladesh. Geriatric depression was significantly associated with marital status, education, occupation, family type, family size, and family income of older individuals. Both the interpersonal trust and reciprocity domains of cognitive social capital were found to be associated with depression. Older persons without interpersonal trust had more chance of experiencing depression. Independence, autonomy, reciprocity, and trust of older individuals with their families and communities could foster cognitive social capital. The study findings could contribute to designing future social capital policies and interventions for the well-being of rural older people in a developing country like Bangladesh. Community-based motivational interventions could encourage older citizens to be involved in volunteering diverse social activities to prevent geriatric depression.
Introduction
Aging is a process that begins at conception and continues throughout the lifespan. Considering the rapid increase in the number of older population, several instruments are adapted to assess the quality of life and physical resilience of older people. Different instruments are proposed to encompass their mental and physical capacities associated with functional ability, intrinsic capacity, and healthy aging. The most popular and validated instruments include the WHOQOL-BREF for quality of life (Lin et al., Reference Lin, Li, Lin and Chen2016), COSMIN for intrinsic capacity (Chen et al., Reference Chen, Kukreti, Yang, Liu, Yeh, Fung, Liu, Liu, Graffiths, Y-C and Lin2023), and PRIFOR, and EQ5D for resilience (Fan et al., Reference Fan, Li, Chang, F-W and Lin2023; Hu et al., Reference Hu, Lin, Yueh, Lo and Lin2022). An increasing body of evidence suggests that psychological and sociological factors cause mental disabilities in older adults (Singh and Misra, Reference Singh and Misra2009). Depression is an established mental disorder in older adults of both industrialized and developing nations. It is projected to become the leading cause of global illness burden by 2030 (Lépine and Briley, Reference Lépine and Briley2011). Due to its severe morbidity and mortality rates among older persons, depression is a leading public health concern. Depression is not a normal part of aging; it is a treatable medical illness, yet the risk of depression among older adults remains high. Geriatric depression is one of the most prevalent mental health issues worldwide. Depression was identified as the second leading cause of the global burden of mental illness in terms of DALYs estimated for all ages by 2020 (Reddy, Reference Reddy2010).
Geriatric depression results in additional difficulties for older persons and society, including a decrease in quality of life and functional capacity and an increase in using medical services and in the mortality rate (Vicerra, Reference Vicerra2022; Chen et al., Reference Chen, Huang, Wu, Kuo and Lin2019a, Reference Chen, Wang, Wu, Lin, Wu, Chuang, Ho, Kuo, Leu and Lin2019b). It also increases the incidence of comorbid dementia. The double burden of depression and dementia poses a huge burden on their family caregivers, which in turn contributes to the poor quality of life of family caregivers (Su et al., Reference Su, Chang, Wang, Chen, Yang and Lin2019, Reference Su, Chang, Yang, Chen, Li and Lin2020; Hu et al., Reference Hu, Chang, C-h, Chen, Su, Lin and Griffiths2023). Populations are quickly aging; many countries face substantial challenges due to astounding rises in healthcare and long-term care expenses for older persons (Katon et al., Reference Katon, Lin, Russo and Unützer2003). Bangladesh is one of the twenty developing nations with the highest proportion of senior citizens. The country, along with four other Asian nations, will account for over half of the world’s old population by 2025 (Chaklader et al., Reference Chaklader, Haque and Kabir2003).
Today’s population is aging faster than ever before. From 2015 to 2050, the percentage of the world’s older population will nearly double from 12% to 22%. In 2050, eighty percent of older persons will reside in low- and middle-income countries. Approximately 15% of older adults suffer from mental diseases, while 10–20% of older individuals worldwide have depression (Cao et al., Reference Cao, Guo, Ping, Tan, Guo and Zheng2016; World Health Organization, 2001). In Asian countries, the prevalence of geriatric depression ranges from 12–34% (Wada et al., Reference Wada, Ishine, Sakagami, Okumiya, Fujisawa, Murakami and Matsubayashi2004). Over 7.5% of the country’s total population are senior citizens and will reach 20% by 2050 (Bangladesh Bureau of Statistics, 2015), and one out of every five Bangladeshi will be an older citizen. The prevalence of mental diseases ranged from 6.5% to 31.0% in Bangladesh and from 36.9% to 45% among the older population (Hossain et al., Reference Hossain, Ahmed, Chowdhury, Niessen and Alam2014). Rural residence, loneliness, illiteracy, and lack of religious practice and social support were associated with geriatric depression in Bangladesh (Disu et al., Reference Disu, Anne, M-D and Mamun2019).
Social capital has been addressed in diverse vantage points by experts. From the standpoint of social cohesion, social capital denotes “properties of social organization, such as trust, norms, and networks that can enhance the efficiency of society by promoting coordinated action” (Putnam et al., Reference Putnam, Leonardi and Nanetti1992). Social capital comprises two dimensions, including cognitive social capital, and structural social capital (Nyqvist et al., Reference Nyqvist, Forsman, Giuntoli and Cattan2013). Cognitive social capital consists of the rules, values, and beliefs that affect the engagement of individuals in society (Agampodi et al., Reference Agampodi, Agampodi, Glozier and Siribaddana2015) and is measured through neighborly trust and reciprocity (Nyqvist et al., Reference Nyqvist, Forsman, Giuntoli and Cattan2013). Structural social capital depicts interactions between individuals frequently organized in formal community groups and measured by membership in organizations and social activities (Agampodi et al., Reference Agampodi, Agampodi, Glozier and Siribaddana2015).
In Bangladesh, social support and mental health are intimately linked (Islam and Iqbal, Reference Islam and Iqbal2008). Studies demonstrate that those with more social support have fewer mental health issues. Diverse management concerns like altering socioeconomic and demographic transitions, widespread poverty, shifting social and religious values, and inadequate health care facilities for the senior population exist in Bangladesh. Consequently, older persons suffer from numerous issues, including debt, loss of authority, social instability, inadequate leisure facilities, and a lack of comprehensive physical and mental care. All these make the older individuals more susceptible to depression.
The indicators for subjective well-being and life satisfaction of the older population include interpersonal trust and reciprocity. Socio-demographic transition, losing spouses, friends, social networks, social involvement, and support tend to predispose depression among older citizens. For this, the cognitive part of social capital is essential for day-to-day assistance and support for the older segment of the community. This case-control study intended to assess the relationship between cognitive social capital and depression in the rural older population.
Methods
Study settings
This case-control study was conducted from January to December 2020. We selected the Gobra union from the Sadar upazila of the Gopalganj district as the geographical area of interest. The study population included all the rural older individuals residing in rural communities of the Gobra Union. The Gobra union comprises nine wards having defined geographical boundaries.
Sample size and sampling technique
We calculated the sample size using the appropriate formula for a case-control study. The calculated sample size was 564 (284 cases and 284 controls). Considering the resource constraints and selection criteria, the study enrolled 420 older individuals, including 210 cases and 210 controls. We used a cluster sampling technique to recruit the participants from the rural communities. We considered each ward of the Gobra union with a defined geographical boundary as a cluster, and four wards were selected randomly as four clusters. Our field team (comprising two field supervisors and four data enumerators) visited all the households within the clusters (wards) and identified 712 households with older members. One eligible participant was selected from each household randomly. Among 712 identified rural older individuals, 14 (1.97%) were severely ill, 16 (2.24%) were unwilling to participate, and 12 (1.68%) were unavailable during data collection. Finally, 670 older persons were eligible for the study. The expert team (comprising a psychiatrist and a public health expert) used the Geriatric Depression Scale-15 (GDS-15) and identified 210 older individuals with depression for recruiting as cases and another 210 older persons without depression for recruiting as controls (Figure 1). To ensure adequate power, effect size was calculated for the chi-square test between the type of participants and outcome variables (Interpersonal trust and Reciprocity). For interpersonal trust, the effect size was 0.59, and for reciprocity, it was 0.81. Finally, we used G*Power (version 3.1) software to conduct the post hoc power analysis, which was found to be >0.80 in both cases (Kang, Reference Kang2021).
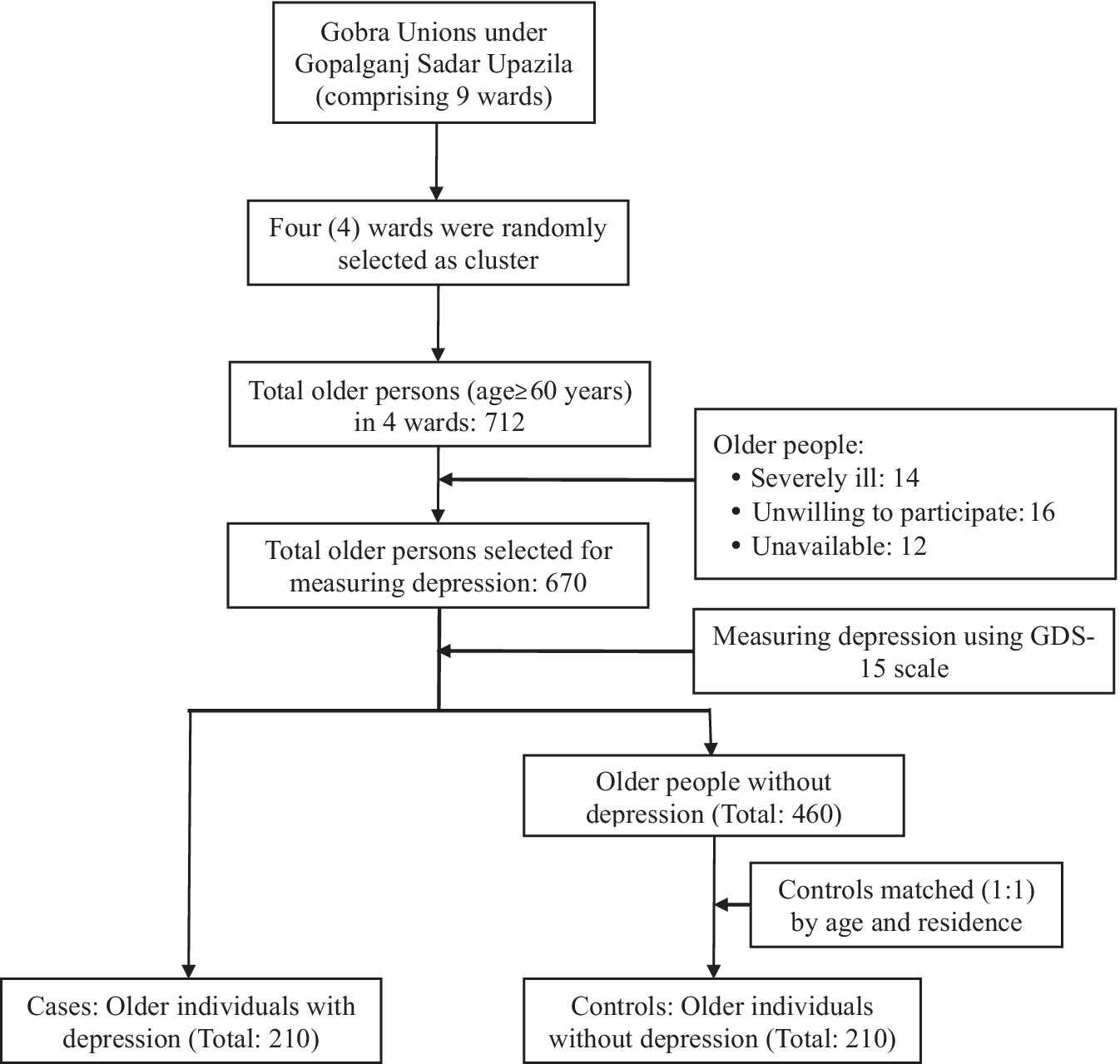
Figure 1. Flowchart of selecting study participants (Cases and Controls).
Study cases
Inclusion criteria:
-
1. Both male and female older persons aged 60 years and above.
-
2. Older persons suffering from depression are diagnosed by experts (comprising public health experts and psychiatrists) using the Geriatric Depression Scale-15 (GDS-15).
-
3. Older individuals who provided informed consent.
Exclusion criteria:
-
1. Older persons who were not willing to participate.
-
2. Older persons who were absent during data collection on two occasions.
-
3. Participants who were severely ill.
Study controls
Inclusion criteria:
-
1. Both male and female older persons aged 60 years and above.
-
2. Older persons not suffering from depression were identified by experts (comprising public health experts and psychiatrists) using the Geriatric Depression Scale-15 (GDS-15).
-
3. Older individuals who provided informed consent.
Exclusion criteria:
-
1. Older persons who were not willing to participate.
-
2. Older persons who were absent during data collection on two occasions.
Controls were enrolled (ratio of 1:1 to cases) and matched individually to each case by age (±2 years) and residence (rural). We described the study objectives and procedure to all the controls and obtained informed consent for their participation. Due to different reasons like social and religious norms of rural communities, unavailability and unwillingness of some participants, scattered geographical distribution of rural households, work engagement of participants, and discontinuation of interviews, we couldn’t match gender to enroll the controls.
Data collection methods and instrument
The study used a semi-structured questionnaire to collect data through face-to-face interviews. The questionnaire comprised variables related to background features (age, gender, marital status, educational qualification, occupation, family type, number of family members, monthly family income) and cognitive social capital (interpersonal trust, reciprocity). It also included the items of the GDS-15 checklist to determine geriatric depression. The present study used a Bangla version of the scale for collecting data related to depression, which was previously used by another study and was validated (Lahiri et al., Reference Lahiri and Chakraborty2020). The data enumerators made appointments with the participants to conduct the interviews at a convenient time and place. Each interview took approximately 25 minutes to complete.
Operational definitions
Geriatric depression
The GDS-15 scale is widely used and has achieved validation in clinical and community settings for assessing depression among older individuals (Yesavage et al., Reference Yesavage, Brink, Rose, Lum, Huang, Adey and Leirer1982). There are several versions of GDS scales: GDS-15, a 5-item version by Hoyl MT et al., (Reference Hoyl, Alessi, Harker, Josephson, Pietruszka, Koelfgen, Mervis, Fitten and Rubenstein1999) and Molly DW et al., (Reference Molly, Standish, Dubois and Cunje2006), and a 4-item version by Marwijk HWV et al., (Reference Marwijk, Wallace, Bock, Hermans, Kaptein and Mulder1995), and Li YP et al., (Reference Li, Lin, Hu and Shih2021). The current study used the GDS-15 scale to evaluate depression symptoms that had been present the week before. The scale consists of 15 items, which need answering with a “yes” or “no” answer. Out of 15 items, 10 indicate the presence of depression if positive answers are received. The remaining items (Items 1, 5, 7, 11, and 13) denote the presence of depression when answered negatively. The scale has a total score of 15 (ranging from 0 to 15). A cut-off score of ≥5 has been suggested to indicate depression and exhibits 92% sensitivity, and 89% specificity (Sheikh and Yesavage, Reference Sheikh and Yesavage1986). The current study also considered a cut-off score of≥5. The internal consistency of the scale was quite good (Cronbach’s alpha = 0∙796) in the present study.
Elderly
People aged 60 years or above were considered elderly individuals.
Cognitive social capital
The cognitive dimension of social capital included interpersonal trust and reciprocity using a single-item questionnaire. The study assessed interpersonal trust by asking the participants an item: “Generally, do you think that most people are trustworthy?” This variable was coded with a 3-point Likert scale where “1” meant “Maximum people are trustworthy”; 2 meant “Try to be careful”, and “3” meant “I don’t know.” In logistic regression analysis, we graded interpersonal trust 1 = Believe (“Maximum people are trustworthy” and “Try to be careful”) and 2 = Not believe (“I don’t know”).
The study measured “Reciprocity” by using an item asking the participants: “Are you willing to help your neighbor who urgently needs your help [e.g. blood donation]?” We coded the variable with a 5-point Likert scale where “1” meaning “Strongly agree” and “5” meaning “Strongly disagree.” For logistic regression, we graded “Reciprocity” as “1” = Disagree (strongly disagree, disagree, neither agree and nor disagree) and “2” = Agree (agree, strongly agree). Several studies used these single-item questionnaires previously to evaluate interpersonal trust and reciprocity (Kim et al., Reference Kim, Yoon, Kim and Kim2017; Han and Lee, Reference Han and Lee2015; Park, Reference Park2017).
Data management
Data were checked and verified after collection at the field and central level to ensure quality. Data were kept safely under the control of the principal investigator. We checked the data thoroughly to verify its relevancy and consistency. Data were coded, categorized, cleaned, and entered into software for analysis. We also performed a double entry of data for its quality control check.
Statistical methods
The study used IBM SPSS software (Version 26.0) for data analysis. In the case of descriptive statistics, we estimated frequency distribution, percentage, mean, and standard deviation. Continuous data were tested by Shapiro-Wilk for normality and presented as mean and standard deviation. Categorical data were represented as counts and percentages. To find any association between categorical variables, we used the chi-square test as a part of inferential statistics. We developed a logistic regression model with all significant variables identified by chi-square tests to find the strength of association. A p-value <0.05 was considered statistically significant. All statistical tests were two-sided and performed at a significance level of α = 0.05.
Results
A total of 420 older individuals (210 depressed as cases and 210 non-depressed as controls) participated in this case-control study. The study found no significant differences in age between cases and controls. Females were 55.2% among cases and 41.9% among controls, while males were 44.8% among cases and 58.1% among controls. Regarding marital status, most of the cases (64.8%) and controls (86.7%) were married, and this difference was statistically significant (p < 0.001). Concerning educational status, primary education was highest in the controls (49.5%), and illiterate was highest in the cases (65.7%), which was statistically significant (p < 0.001). Concerning occupation, housewife was significantly higher (p < 0.01) among cases (54.3%) than in the controls (41.0%). Joint family was found to be higher among the control (82.9%) than the cases (63.7%), which was statistically significant (p = 0.001).
Regarding the number of family members, there was a statistically significant (p < 0.001) difference between cases (53.3% had 5–8 members) and controls (65.7% had 5–8 members). In respect of monthly family income, the higher segment of the cases (56,2%) had 5000–10,000 taka, while the higher portion of the controls (56,2%) had 11,000–20,000 taka, and the difference was significant (p < 0.001) statistically (Table 1).
Table 1. Comparison of socio-demographic characteristics between cases and controls
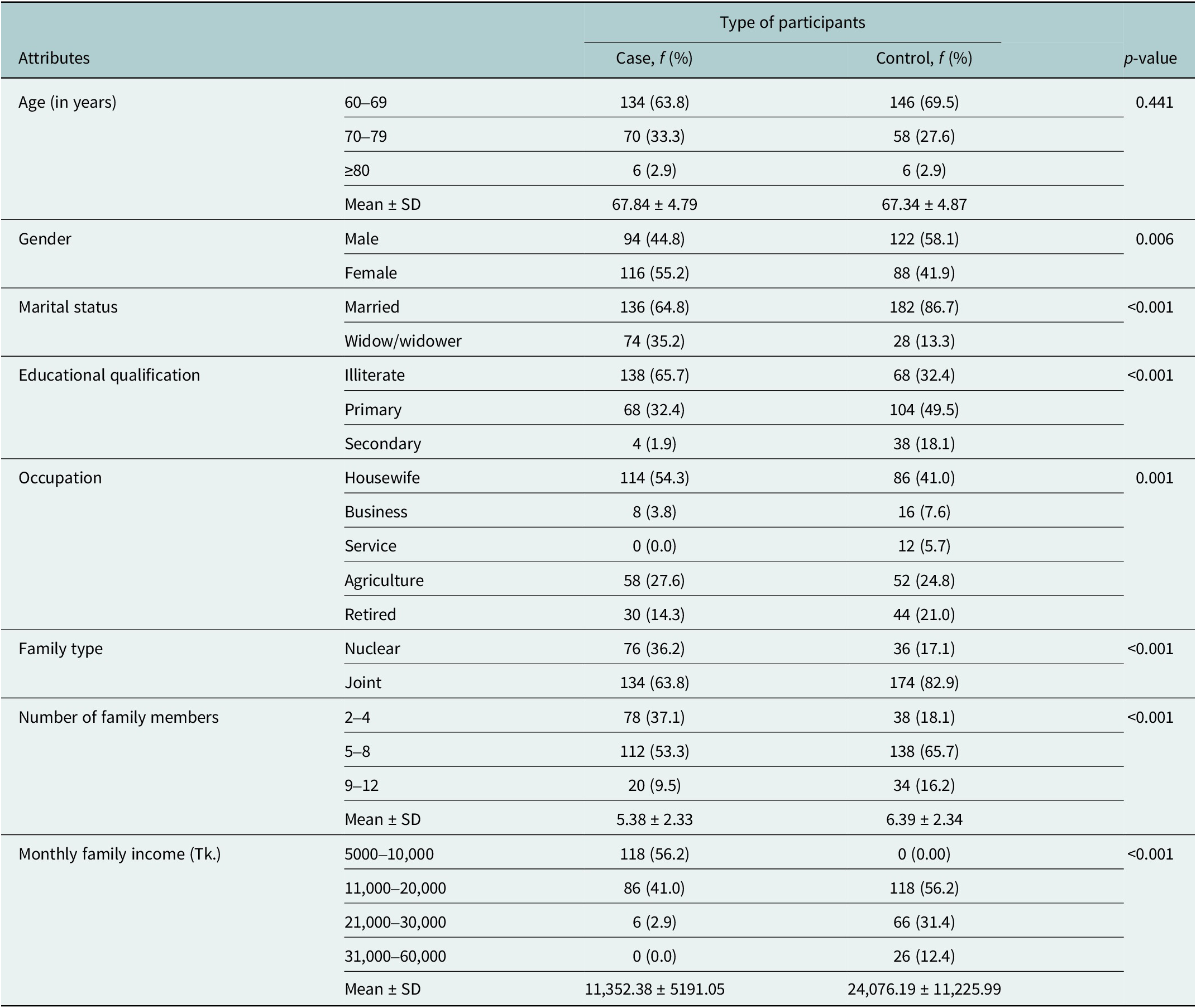
f: frequency; %: percentage; SD: standard deviation; significance: Chi-square test, p < 0.05 with 95% CI.
Both interpersonal trust and reciprocity were found to be significantly (p < 0.001) different between cases and controls. Regarding interpersonal trust, 55.2% of the cases answered, “I don’t believe,” while 71.4% of the controls answered, “Maximum people are trustworthy.” Concerning reciprocity, 45.7% of the cases answered “Disagree,” while 60.0% of the controls answered, “Strongly agree” (Table 2).
Table 2. Comparison of cognitive social capital (interpersonal trust and reciprocity) between cases and controls
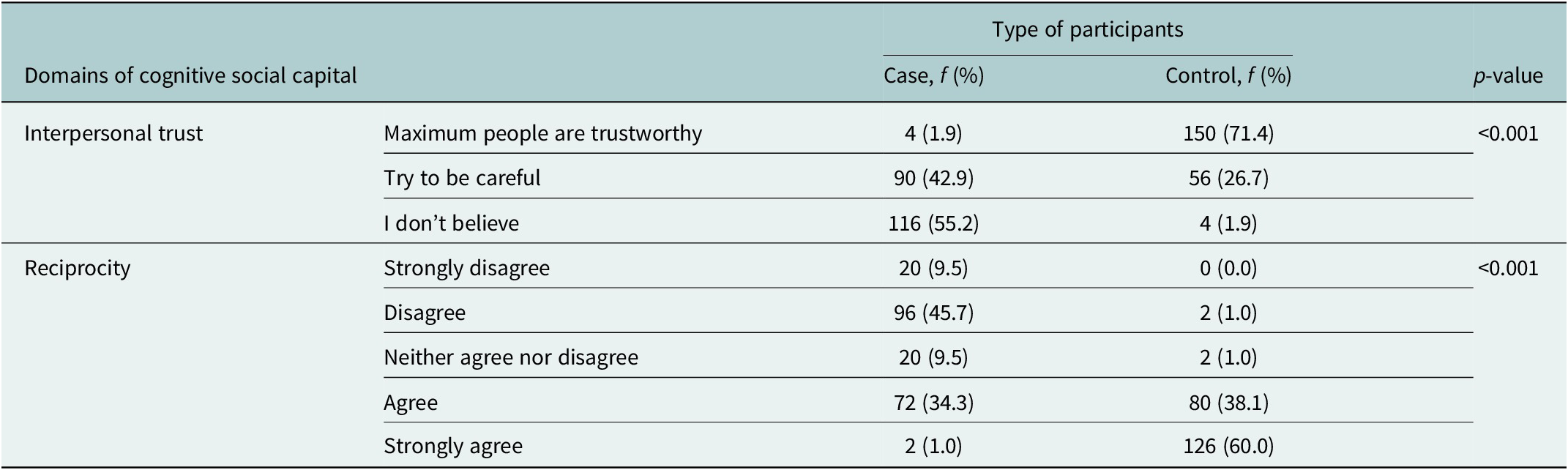
f: frequency; %: percentage; SD: standard deviation; p < 0.05: significant at 95% CI.
The logistic regression analysis showed that participants who didn’t have interpersonal trust were 6.771 times more at odds of experiencing depression than those who had interpersonal trust (AOR = 6.771; 95% CI: 1.985–23.094; p = 0.002). Concerning reciprocity, older individuals who didn’t agree to help neighbors who urgently needed help had more than 31 times higher risk of having depression (AOR = 31.133; 95% CI: 9.93–97.602; p < 0.001) (Table 3).
Table 3. Logistic regression analysis of the association between cognitive social capital (interpersonal trust and reciprocity) and depression
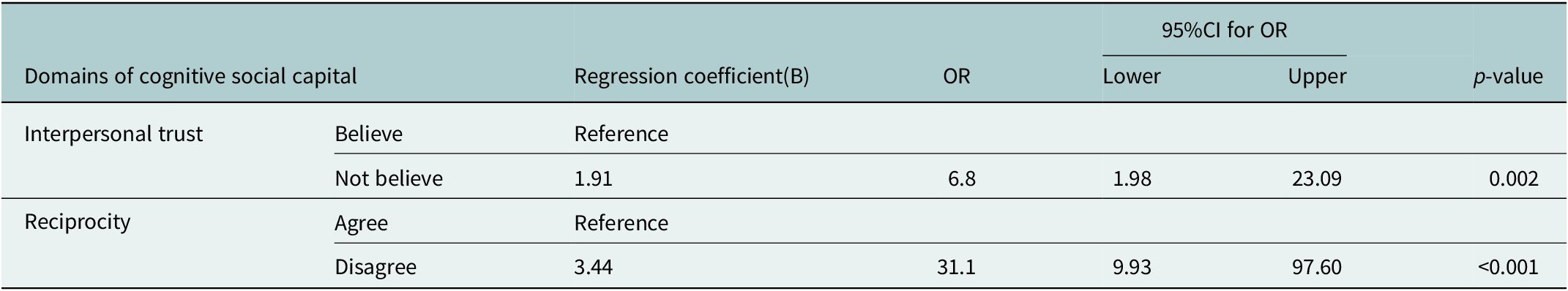
OR: odds ratio: CI: confidence interval; reference category for depression: absent.
Discussion
Social capital is a determinant of mental health and explains why mental health varies across societies. Lower social capital was connected to mental diseases such as depression and high suicide rates by previous research (Han and Lee, Reference Han and Lee2015; Bassett and Moore, Reference Bassett and Moore2013). Hence, it is a social element of importance for public health, notably for older persons and healthy aging (Aihara et al., Reference Aihara, Minai, Kikuchi, Aoyama and Shimanouchi2009). Literature also suggests that interpersonal trust and reciprocity are crucial determinants of older mental health characteristics, and they affect life satisfaction, self-rated health, depression, physical disability, and death rates in older adults (Lu et al., Reference Lu, Jiang, Lou, Zeng and Liu2018; Islam, Reference Islam2019). The current study examined the relationship between social capital and depression in rural older adults in Bangladesh.
Previous literature review revealed that relevant data on cognitive social capital and geriatric depression is not available in the context of rural Bangladesh. This case-control study was conducted between two groups of older population, cases having depression and controls having no depression. Using a community-based case-control study design, the current study sought to uncover the link between cognitive social capital and older adults` depression in a rural setting.
The present study found a statistically significant association between gender and depression among older individuals, which collaborates with previous studies that have also found the same findings (Zhou et al., Reference Zhou, Li, Ogihara and Wang2022; Konda et al., Reference Konda, Sharma, Gandhi and Ganguly2018). This may be because older women are often deprived of adequate care, more so than their counterparts in the sub-continent. The marital status of older people has a significant association with geriatric depression. Another study conducted in India also reports similar findings (Konda et al., Reference Konda, Sharma, Gandhi and Ganguly2018). This may be because older people are culturally dependent on their spouses for care and emotional support, a lack of which often leads to depression. A statistically significant association was also found between educational qualification, occupation, family type, number of family members, and monthly family income (in taka) with depression in older adults.
In this study, it was found that a higher level of cognitive social capital (in terms of interpersonal trust and reciprocity) was associated with a lower chance of having depressive symptoms, which corresponds to previous studies (Han et al., Reference Han, Han, Shin, Jee, An, Yoon and Kim2018; Li et al., Reference Li, Zhou, Ma, Jiang and Li2017; Cao et al., Reference Cao, Li, Zhou and Zhou2015). Previous studies also suggested that a lower level of cognitive and social capital (in terms of interpersonal trust and reciprocity) is associated with suffering from depression among older people, which conforms with our study. These findings indicate the importance of cognitive social capital while addressing the issues of depression among older people. Several studies have suggested some methods that can help to improve the level of cognitive social capital among older people which will consequently improve the mental health condition and quality of life of older adults. Using social networks is an adaptive method that can help older people to overcome their depression and increase the quality of life (Siah et al., Reference Siah, Ooi, Zaman and Low2023). Implementing physical activity programs and promotion of vaccination programs can also improve the quality of life of older individuals (Lee et al., Reference Lee, Hsieh, Laio, Tsent, Chen, Griffiths, Chuang and Lin2024; Lin et al., Reference Lin, Fan, Ahorsu, Lin, Weng and Griffiths2022).
Conclusion
The present study provided evidence on the relationship between cognitive social capital and geriatric depression and showed that cognitive social capital is associated with depression. Individuals who had lower reciprocity and trust were more prone to have depression. The literature review revealed that relevant data on cognitive social capital and geriatric depression is scarce in the context of rural Bangladesh. The findings could be helpful in developing policies and programs for public awareness to promote and maintain social capital activities to safeguard our older people from late-life depression.
Limitations of the study
The study enrolled only older people from the rural communities of Bangladesh. So, the study findings could not be generalized to the whole country. In addition, for some valid reasons, the study could not match gender in enrolling the control group.
Recommendations
Depression among older persons in rural areas needs to be an integral component of public health interventions in the community. To prevent depression, reciprocal relationships, and social interaction of Older with their family, friends, and neighbors should be increased. Interpersonal trust needs to be ensured within families and communities to prevent older depression. To provide need-based interventions for the prevention and control of depression among rural elderly individuals, community-based activities like night education, age-based vocational training, etc., should be required.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2024.72.
Data availability statement
The data that support the findings are available on request from the corresponding author, MZ Islam. The data are not publicly available due to containing information that could compromise the privacy of research participants.
Acknowledgements
The authors would like to offer special thanks to the Bangladesh Medical Research Council (BMRC) for providing financial support for the study.
Author contributions
M.Z.I. and E.P. provided substantial contributions to the conception or design of the work; acquired, analyzed, and interpreted the data. S.F., M.F.A.F., and S.S.E. drafted the data. M.Z.I., E.P., M.F.A.F., S.F., and S.S.E. revised the manuscript critically for important intellectual content and approved the final version of the article for submission and publication. M.Z.I., E.P., M.F.A.F., S.F., and S.S.E. are agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Financial support
This study was supported by the Bangladesh Medical Research Council (BMRC).
Competing interest
The authors have no relevant conflicts of interest to declare. The funders had no role in designing and conducting the study.
Ethics statements
The study obtained ethical clearance from the Institutional Review Board (IRB) of the National Institute of Preventive and Social Medicine (NIPSOM). All the study participants participated voluntarily and provided informed written consent. We strictly maintained the confidentiality of data and used it only for the present study. We also preserved the privacy of the participants during data collection with the highest priority.







