Article contents
White matter disconnection and decreased functional connectivity between orbitofrontal cortex and the contralateral temporo-occipital cortex in adults with obsessive compulsive disorder
Published online by Cambridge University Press: 13 August 2021
Abstract
Obsessive compulsive disorder (OCD) affects 2-3% of the general population. The neurobiology of OCD has been linked to dysfunction of cortico-striatal circuits connecting the orbitofrontal (OFC) to the striatum. Recently, this loop has become an approved target for non-invasive neuromodulatory treatment of OCD.
To explore structural and functional connectivity of the OFC in OCD subjects and healthy controls.
14 OCD patients and 12 age/sex-matched controls underwent magnetic resonance imaging (MRI) (3T-Philips scanner) for diffusion tensor imaging (DTI) and resting state functional connectivity (rsFC). DTI images were brain extracted and corrected for movement and eddy currents. A diffusion tensor model was fitted to each voxel and used to generate Fractional Anisotropy (FA) maps. Voxel-wise statistical analysis of FA was performed using Tract-Based Spatial Statistics. RsFC images were preprocessed and seed-based correlation (SBC) analysis was performed using Data Processing Assistant for Resting-State fMRI.
We found decreased values of FA in the body of the Corpus Callosum bilaterally (MNI_coordinates: x= 16, y= -16, z= 33 and x= -19, y= -16, z= 42) and left superior longitudinal fasciculus in OCD patients (fig 1, left), as well as decreased rsFC of the right superior orbitofrontal seed with the left inferior frontal gyrus and left middle occipital gyrus (fig 2, right).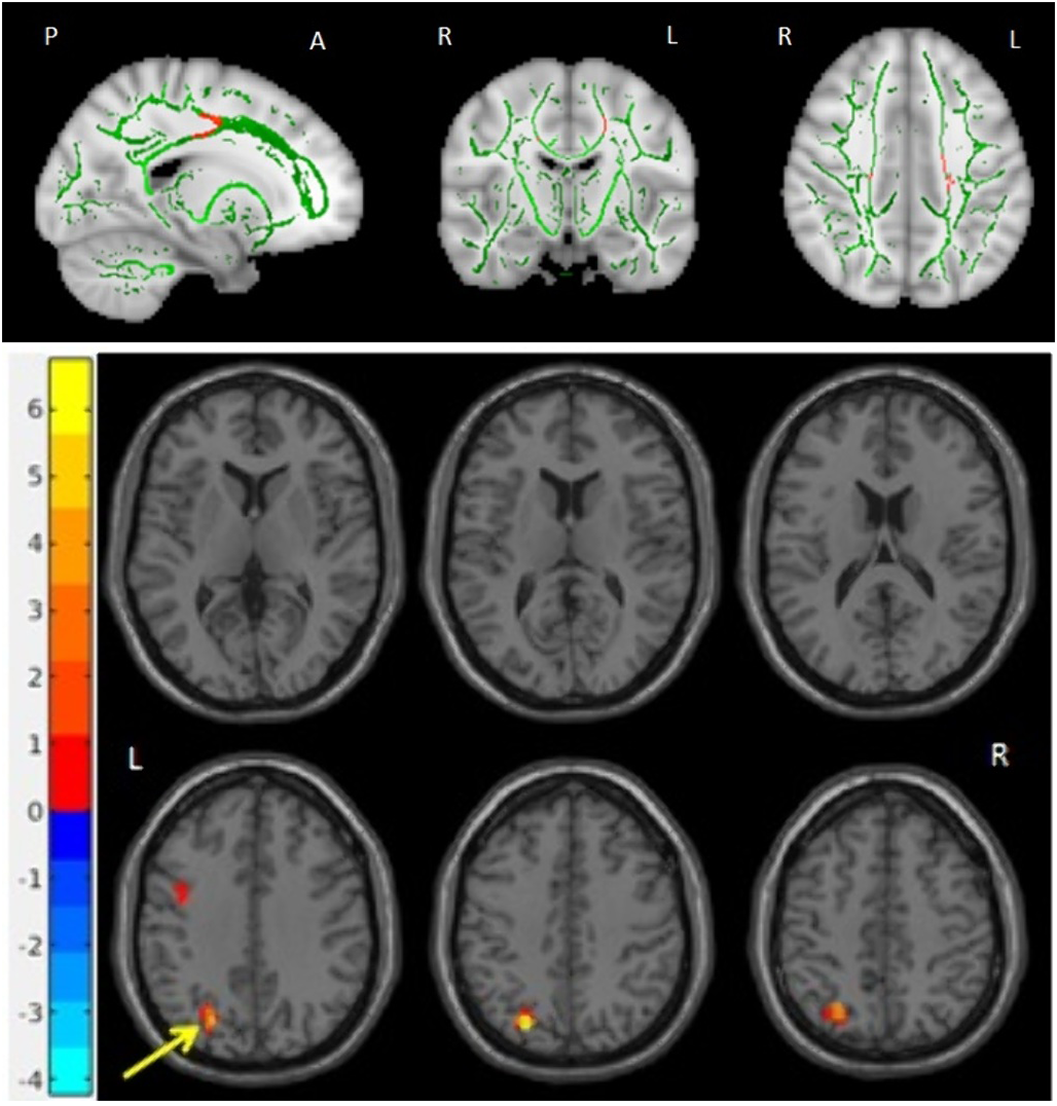
Using an exploratory multimodal approach we found evidence of abnormal structural and functional long-range connectivity of the OFC in OCD. If confirmed in a larger sample these connectivity abnormalities could be explored as potential predictors of response to OFC-targeted non-invasive neuromodulatory interventions.
No significant relationships.
Keywords
- Type
- Abstract
- Information
- European Psychiatry , Volume 64 , Special Issue S1: Abstracts of the 29th European Congress of Psychiatry , April 2021 , pp. S135 - S136
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2021. Published by Cambridge University Press on behalf of the European Psychiatric Association
- 1
- Cited by



Comments
No Comments have been published for this article.