Introduction
The association between poor physical health and severe mental illness (SMI), traditionally defined as schizophrenia-like disorders, bipolar disorder, and other nonorganic psychoses, is now well-established and has gained prominent research and policy attention over the years [Reference Phelan, Stradins and Morrison1].
People with SMI are at particular risk for increased physical health morbidity, given their higher risk of unhealthy lifestyle choices such as smoking [Reference Osborn, Nazareth and King2,Reference Diwan, Castine, Pomerleau, Meadow-Woodruff and Dalack3], treatment with antipsychotic drugs [Reference Mitchell, Vancampfort, De Herdt, Yu and De Hert4], social deprivation [Reference Harrison, Gunnell, Glazebrook, Page and Kwiecinski5], diminished awareness of their poor physical health [Reference Osborn, Nazareth and King2,Reference Buhagiar, Parsonage and Osborn6], and delayed treatment for their physical problems [Reference Mitchell, Malone and Doebbeling7] relative to the general population. The combination of these risk factors leads to excess disability, culminating in reduced life-expectancy [Reference Chang, Hayes, Perera, Broadbent, Fernandes and Lee8], and excess mortality [Reference Harris and Barraclough9] that have been increasing over the years relative to the general population [Reference Saha, Chant and McGrath10,Reference Hayes, Marston, Walters, King and Osborn11]. In light of these serious physical health risks, public health policies, and treatment interventions have therefore focused their attention on people with SMI [Reference Lewis and Hayes12], as opposed to other patient groups with more prevalent common mental disorders (CMDs) such as anxiety disorders and unipolar depression.
Despite being mostly treated in primary care, people with CMDs also have a very complex association with physical disorders acting in a multifaceted and bidirectional pathway that increases disability and health resources [Reference O’Neill, Williams, Stevenson, Oldenburg, Berk and Sanderson13,Reference Weich, Bebbington, Rai, Stranges, McBride and Spiers14]. Previous studies have consistently demonstrated elevated risks of physical comorbidity among people with CMDs compared with the general population [Reference Sareen, Cox, Clara and Asmundson15,Reference Sareen, Jaconif, Cox, Belik, Clara and Stein16], predisposing to even worse outcomes than having either illness alone [Reference O’Neill, Williams, Stevenson, Oldenburg, Berk and Sanderson13,Reference Gaulin, Simard, Candas, Lesage and Sirois17]. Additionally, the prevalence of unhealthy lifestyle behaviors among people with CMDs may be comparable to those observed in people with SMI in some instances [Reference Thapar, Collishaw, Pine and Thapar18]. SMI and CMDs as groups of disorders, however, differ markedly from one another from both psychological and sociodemographic perspectives [Reference Marneros, Deister and Rohde19], contributing to variations in their progression, which may subsequently also influence comparative physical health needs and outcomes [Reference Lawrence, Holman, Jablensky and Hobbs20,Reference Manderbacka, Arffman, Sund, Haukka, Kemkimaki and Wahlbeck21].
Despite the wealth of research evaluating physical comorbidities in people with SMI, studies at population-based level have not generally explored comparative associations relative to people with CMDs [Reference Gaulin, Simard, Candas, Lesage and Sirois17]. The physical health needs of people with CMDs compared with those of people with SMI have therefore not been fully quantified and appear to be less well understood [Reference Lewis and Hayes12]. In addition, there are no UK-specific data on the relationship of CMDs and physical conditions relative to general population, which may be affected by unique geographical factors and intricacies of healthcare systems. The prevalence of CMDs globally is about 10-fold higher than that of SMI [22], hence shows a much greater impact on overall morbidity at population-based level. However, to date, there exist no policies and treatment interventions aimed specifically at people with both CMDs and physical conditions, in contrast with the extensive attention given internationally to people with SMI with similar physical health problems [Reference Lewis and Hayes12].
We need to understand whether there are quantitative differences in the physical health outcomes between these two distinct patient groups. In turn, this would clarify whether there is a need to recalibrate public health policy to make equitable focus on people with all types of chronic mental disorders and not merely SMI.
The primary aim of the current study was to compare (a) the prevalence of recent physical conditions and (b) recent health service utilization for physical conditions among people with CMDs compared to those with SMI. Our secondary aim was to compare these associations for people with CMDs relative to those without mental illness. We hypothesized that people with CMDs have: (a) comparable physical health outcomes and utilization relative to people with SMI and (b) higher risk of physical conditions and health service utilization compared with people without mental illness.
Methods
Sampling and interviewing procedures
We conducted a secondary analysis of data from the Adult Psychiatric Morbidity Survey 2007 (APMS 2007) [Reference McManus, Meltzer, Brugha, Bebbington and Jenkins23], a sample survey of all adults living in private households in England, collecting nationally representative cross-sectional data for the population aged 16 and above. The dataset has been made publicly available via the U.K. Data Service [24], while the full sampling methodology is available in the main survey report published elsewhere [Reference McManus, Meltzer, Brugha, Bebbington and Jenkins23]. In summary, the survey adopted a multistage stratified probability sampling design, according to socio economic grouping and geographical region, yielding a total of 7,461 actual participants (response rate = 57%), with eventual usable data from 7,403 participants. Data were weighted to take account of nonresponse and reduce selection bias so that the results were representative of the entire population (see Supplementary Note 1). Ethical approval was obtained from the Royal Free Hospital and Medical School Research Ethics Committee (ref 06/Q0501/71).
Main measures
Psychiatric morbidity
Common mental disorders: The Clinical Interview Schedule Revised (CIS-R) [Reference Jordanova, Wickramesinghe and Gerada25] was used to identify 14 categories of nonpsychotic symptoms. The CIS-R has two initial filter questions for each of these categories of symptoms covering 1 month prior to the interview, with a positive answer leading to more detailed enquiry about symptoms in the previous week. Responses were then entered into a computer algorithm to subsequently generate six categories of CMDs in the previous week according to ICD-10 criteria: depression, generalized anxiety disorder, panic disorder, phobia, obsessive–compulsive disorder, and mixed anxiety and depressive disorder. For our analyses, we used a derived variable combining the prevalence estimates of all six diagnostic categories.
Severe mental illness: People with probable psychotic disorder were identified if they responded positively to one of several screening questions in the survey, as detailed in the APMS report [Reference McManus, Meltzer, Brugha, Bebbington and Jenkins23] (see Supplementary Note 2). If they did, participants were then eligible for a further clinical assessment for a diagnosis of definitive psychotic disorder using the Schedule for Clinical Assessment in Neuropsychiatry version 2.1 (SCAN) [Reference Wing, Babor, Brugha, Burke, Cooper and Giel26]. For our analysis, we assigned participants meeting criteria for either probable or definitive psychotic disorder in the past year to a single group as a proxy for SMI, consistent with previous research [Reference Meltzer, Bebbington, Dennis, Jenkins, McManus and Brugha27].
People without mental disorders: We identified a group of participants who did not meet the diagnostic criteria for any of the mental disorders assessed in the survey, including personality disorders, dependence on alcohol or drugs, history of self-harm, and problem gambling. Hazardous use of alcohol and nonproblematic drug use were not exclusion criteria.
Physical comorbidity
Physical health conditions were assessed by asking participants if they had suffered from a number of mostly long-term physical conditions presented to them on a list, first in the year preceding the interview and second, in their lifetime since the age of 16 years. We included diabetes, hypertension, angina/myocardial infarction, any cancer, ear disorders/hearing problems, cataracts/eyesight problems, emphysema/bronchitis, asthma, bladder problems/incontinence, bowel/colon problems, stomach ulcers/digestive problems, musculoskeletal problems, infectious diseases, and skin problems. We specifically excluded epilepsy, dementia, and migraine due to their potential symptomatic overlap with mental disorders. We then generated a categorical variable for past-year physical conditions: (a) having at least one physical condition or not and (b) the total number of physical conditions reported per participant, classifying participants into four groups around the median consistent with previous studies [Reference Woodhead, Rona, Iversen, MacManus, Hotopf and Dean28].
Health service utilization and treatment
Physical health service utilization: Participants were asked about their recent use of health services for physical health problems with respect to (a) consultations in person or by telephone with their general practitioner (GP) in the past year; (b) planned visit to an out-patient clinic in the previous 3 months; and (c) acute admission to a general hospital in the previous 3 months, defined as at least one overnight stay except for childbirth.
Mental health treatment: Data regarding named psychotropic medications and mental health service use received by participants were collected, the latter acting as a proxy for receipt of secondary psychiatric care.
Covariates
Socio demographic variables: age, gender, ethnicity, marital status, educational qualifications, occupation, and debt.
Clinical variables: We generated variables for body mass index (BMI; obesity, BMI ≥ 30 kg/m2) and current smoking status. The Alcohol Use Disorders Identification Test (AUDIT) [Reference Saunders, Aasland, Babor, Dela Fuente and Grant29] was used as a screening tool for patterns of harmful and hazardous drinking, followed by the Severity of Alcohol Dependence Questionnaire (SAD-Q) [Reference Stockwell, Sitharan, McGrath and Lang30] to determine dependence. We created a dichotomous variable for participants with a drinking problem (hazardous use or dependence) vs. those without a drinking problem during the past 6 months. Participants were also asked about their drug intake using a computer-assisted self-completion interview followed by a selection of questions from the Diagnostic Interview Schedule [Reference Malgady, Rogler and Tryon31] for each drug reported. We used a dichotomous variable, classifying participants into being dependent on any drug or not.
Data analysis
Data analysis was conducted using the survey commands in Stata 12.0 for Macintosh (Stata Corp LP, College Station, TX). These commands allow for the use of clustered data inherent in complex survey designs modified by probability weights and provide robust estimates of variance. The weighting procedure is necessary in order to account for potential biases that may be caused by nonresponse.
We described variables using actual counts, but proportions and ratios are derived from weighted measures. We first compared sociodemographic and clinical variables between the CMD and SMI groups, using Pearson chi-square tests with Rao and Scott second-order correction for survey data for categorical variables or Student’s t tests for continuous variables. First, we calculated the total number of past-year physical conditions in each participant group. We then used univariable and multivariable logistic regression analysis to compare associations across people with CMDs and SMI, the latter acting as a reference group. The multivariate models were conducted in accordance with previously published studies addressing similar research questions [Reference Remes, Wainwright, Surtees, LaFortune, Khaw and Brayne32] and included potentially confounding sociodemographic covariates associated with both mental disorders and physical health outcomes: age, gender, ethnicity, employment, education, as well as covariates for behavior risk factors: BMI, smoking status, alcohol intake, and drug dependence. Although the latter group of covariates may be regarded as potential mediators of associations between mental disorders and health outcomes, they themselves also represent directly or indirectly psychiatric comorbidities, hence also acting as potential confounders in these associations of interest [Reference Remes, Wainwright, Surtees, LaFortune, Khaw and Brayne32].
Second, we used univariable logistic regression in order to compare the odds of physical health service utilization (GP visits, outpatient visits, and acute somatic hospitalization) between the two main groups of interest, followed by a multivariable logistic regression analysis adjusting for the number of reported lifetime physical disorders in addition to the selected covariates above.
A second set of analyses was repeated for all of these physical health outcomes, comparing people with CMDs with participants without mental disorders.
Results
Sample characteristics
CMDs were identified in 1,248 participants, meeting the criteria for the following specific ICD-10 diagnoses: severe depression (n = 85, 6.3%), moderate depression (n = 63, 4.8%), mild depression (n = 88, 6.2%), panic disorder (n = 67, 6.0%), obsessive–compulsive disorder (n = 31, 2.8%), social phobia (n = 37, 2.7%), agoraphobia (n = 16, 1.3%), specific phobia (n = 19, 1.7%), mixed anxiety and depression disorder (n = 637, 52.4%), and generalized anxiety disorder (n = 207, 15.7%). There were 40 participants with SMI and no comorbid CMDs, while 5,695 participants did not meet the criteria for any mental disorder. Table 1 summarizes the sociodemographic and clinical characteristics of the two main participant groups. Participants with CMDs were significantly less likely than those with SMI to have been in contact with secondary care services for mental disorders (Table S1).
Table 1. Characteristics of participants with common mental disorders and severe mental illness
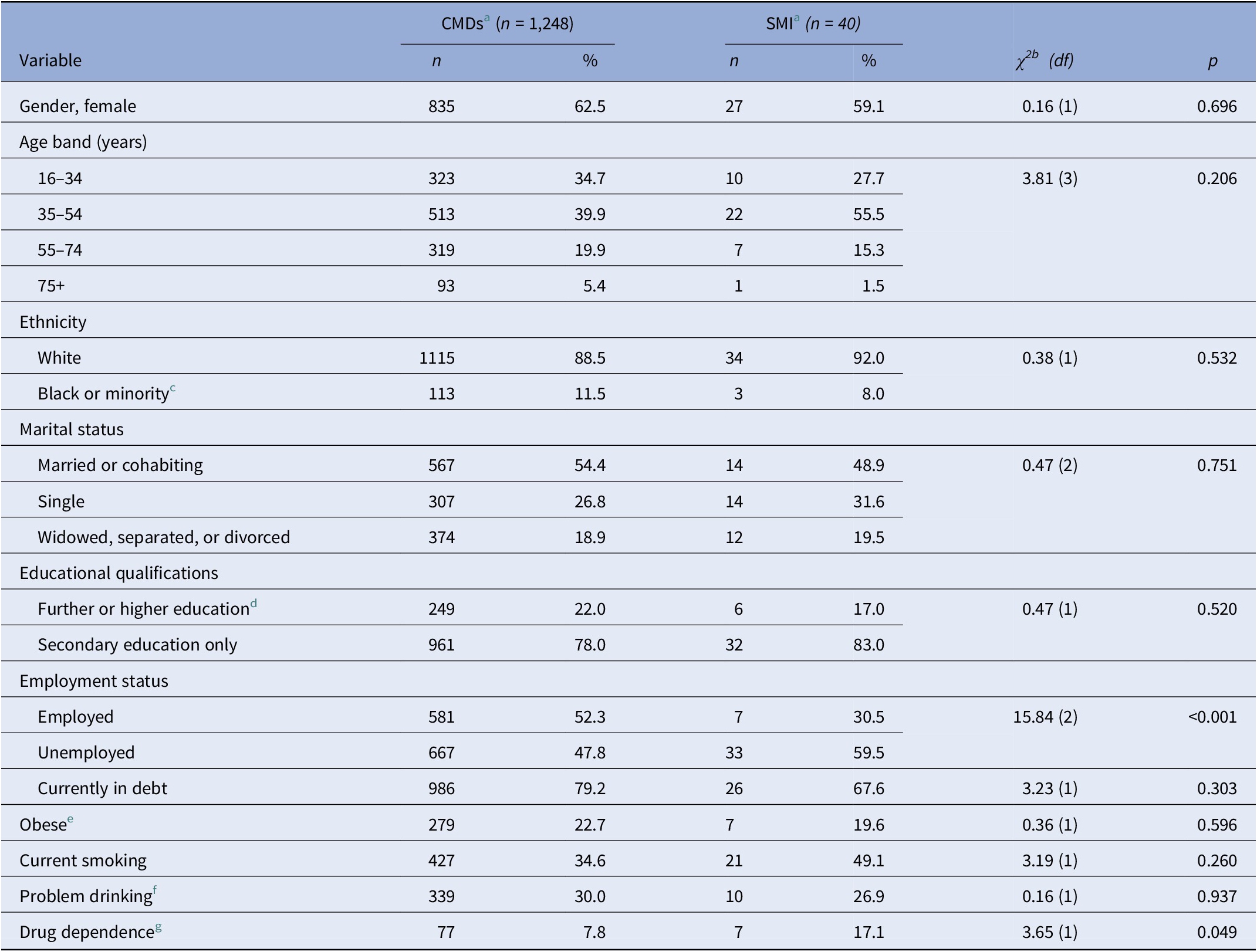
Abbreviations: CMD, common mental disorders; SMI, severe mental illness.
a Percentages are weighted to account for complex survey design. Counts may not add up to totals due to missing data.
b Pearson’s χ 2 with Rao and Scott second-order correction for survey data analysis.
c Includes South Asian and mixed race participants.
d Includes university degrees or professional qualifications only.
e BMI ≥ 30 kg/m2.
f In the past 6 months, assessed with the Severity of Alcohol Dependence Questionnaire.
g In the past year, assessed with the Diagnostic Interview Schedule.
Comparison between CMDs and SMI
Physical disorders
Nearly one-third of all participants reported having at least one past-year physical condition (CMDs, n = 815, 62.1%; SMI = 27, 63.1%), with no statistically significant difference between participant groups in both unadjusted (odds ratio [OR] = 0.93, 95% confidence intervals [CI] 0.47–1.79, p = 0.873) and adjusted models (OR = 0.96, 95% CI 0.42–1.98, p = 0.784). Repeating the analysis using categorical variables according to the total number of self-reported past-year physical conditions also failed to reveal variation between the two groups, even when confounders were taken into account (Table 2).
Table 2. Physical conditions in the past year among people with common mental disorders compared with people with (a) severe mental illness and (b) without mental disorders: weighted self-reported prevalence and results of logistic regressions for their association with participant groups
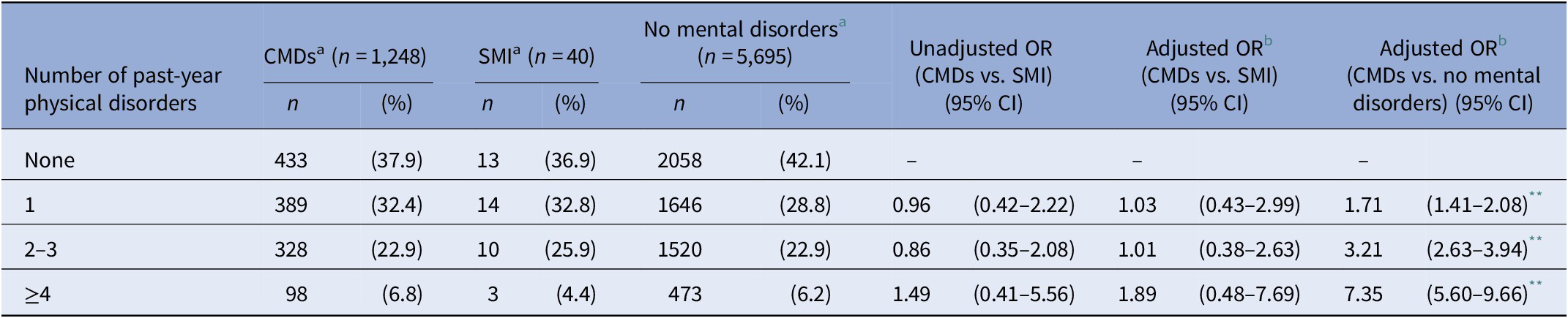
Abbreviations: CI, confidence interval; CMD, common mental disorders; OR, odds ratio; SMI, severe mental illness.
a Percentages are weighted to account for complex survey design.
b Adjusted for age, body mass index, gender, ethnicity, education, employment, smoking, alcohol consumption, and drug dependence.
** p value <0.001.
Health service utilization
As summarized in Table 3, people with CMDs had significantly elevated odds of acute hospital admissions for physical disorders in the past 3 months even after adjusting for participant characteristics and number of lifetime physical conditions (OR = 6.33, 95% CI 5.05–10.0, p = 0.045), despite similar rates of GP and out-patient visits.
Table 3. Physical health service utilization among people with common mental disorders relative to people with (a) severe mental illness and (b) people without mental disorders
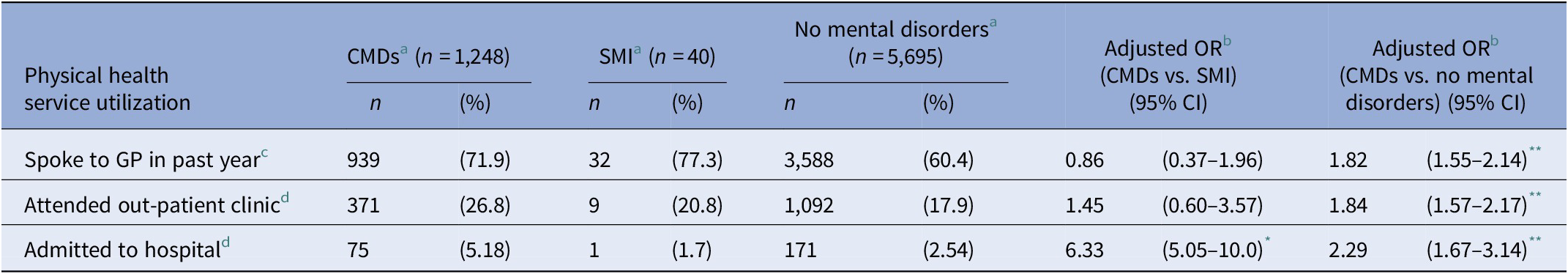
Abbreviations: CI, confidence interval; CMDs, common mental disorders; GP, general practitioner; OR, odds ratio; SMI, severe mental illness.
a Percentages are weighted to account for complex survey design.
b Adjusted for age, body mass index, gender, ethnicity, education, employment, number of physical disorders, smoking, alcohol consumption, and drug misuse.
c In person or by telephone regarding a physical health problem.
d For physical health problem only except for giving birth in previous 4 months.
* p value <0.05.
** p value <0.001.
Supplementary analyses
Comparing a subgroup of participants with CMDs who had consulted their GP in the past year for a mental health problem (n = 512, 41.3%) relative to the total SMI group, revealed findings consistent with those of the total CMD sample (past-year physical conditions, adjusted OR = 0.89, 95% CI 0.46–1.81, p = 0.797; somatic GP consultations, adjusted OR = 0.85, 95% CI 0.32–1.97, p = 0.598; somatic out-patient visits, adjusted OR = 1.38, 95% CI 0.56–3.76, p = 0.562; and somatic hospital admissions, adjusted OR = 5.21, 95% CI 4.13–8.7, p = 0.036). The smaller subgroup of CMD participants already taking psychotropic medications or undergoing psychotherapy at the time of the interview (n = 317, 24.2%) also reported similar rates of physical conditions in the past year relative to the SMI participants (adjusted OR = 0.91, 95% CI 0.32–1.86, p = 0.626).
To further test the robustness of our findings, we finally compared people with SMI with people without mental illness with respect to all outcomes of interest. Despite the elevated odds among people with SMI to report at least one past-year physical condition (OR = 3.46, 95% CI 1.23–8.04, p = 0.038), their odds for acute somatic hospitalization were nearly half as much (OR = 0.54, 95% CI 0.07–0.83, p = 0.032). Full results of these additional analyses are summarized in Table S2.
CMDs vs. people without mental illness
Physical disorders
People with CMDs had significantly higher odds of reporting physical conditions in the past year (OR = 1.21, 95% CI 0.98–2.26, p < 0.001; adjusted OR = 1.82, 95% CI 0.96–2.16, p < 0.001) compared with people without mental illness. As shown in Table 2, this trend continued when physical disorders were also analyzed as categorical variables, with the odds for greater multimorbidity among people with CMDs becoming increasingly elevated.
Health service utilization
People with CMDs were significantly more likely than the general population to seek medical help for their physical conditions in both primary and secondary care (Table 3).
Discussion
In this population-based study of a nationally representative study in England, we found that nearly two-thirds of participants with either CMDs or SMI reported having at least one physical condition in the past year. In addition, we found no statistically significant variation between people with CMDs and those with SMI in the odds of having past-year physical conditions, even after taking into account socio demographic variables and modifiable risk factors predisposing to poor physical health. Although people with CMDs and SMI visit their GP or outpatients for physical health problems just as often, people with CMDs are considerably more likely to be recently hospitalized for physical complaints even when physical multimorbidity was controlled for. Direct comparisons across distinct groups of people with mental illness, as opposed to comparisons with the general population, have seldom been explored before.
Through our secondary objectives, we confirmed the elevated odds of physical conditions and physical health service utilization in people with CMDs compared with the general population as seen in international literature [Reference Sareen, Cox, Clara and Asmundson15,Reference Sareen, Jaconif, Cox, Belik, Clara and Stein16]. The odds of severe past-year physical health multimorbidity (≥4 conditions) among people with CMDs were over seven times as elevated.
Interpretation of findings and comparison with other studies
Only a very small proportion of people with CMDs (c. 3%) in our sample had received specialist psychiatric care, implying less severe symptomatology overall, yet their physical health compared with that of the general population was poor and even comparable with that of people with SMI. The chronic nature and the multiple past-year physical conditions present in a large proportion of people with CMDs are also indicative of the high rates of active physical multimorbidity, in line with previous findings elsewhere [15–17].
Given the complex bidirectional relationship between CMDs and physical disorders, within the context of the study’s cross-sectional design, the temporal relationship between the two cannot be entirely elucidated. In other words, it is possible that a proportion of individuals meeting diagnostic criteria for CMDs at the time of participation might have developed neurotic symptoms as an aftermath to a recently diagnosed physical condition, rather than the CMD itself being a precursor. This may have inflated our findings with respect to the high rates of physical conditions in people with CMDs, consequently equaling those found in people with SMI. However, our sensitivity analyses exploring somatic outcomes among subgroups of CMD participants (i.e. those who made contact with their GP about mental health problems in the previous year or had already been taking treatment for a CMD at interview), revealed similar results with those of the main CMD vs. SMI analysis. Given the time-frames for inclusion in these subgroups, these participants are likely to have had at least emerging neurotic symptoms predating the onset of the physical conditions or the need for somatic hospitalization. These findings, may therefore underline the strong antecedent role of CMDs in predisposing to the later emergence of physical conditions. Recent findings from population-based longitudinal data in the United States in fact, do show a strong independent predictive effect of CMDs on a wide range of physical symptoms and diagnosable conditions, and that CMDs themselves may act as even stronger risk factors than obesity and smoking for physical conditions [Reference Niles and O’Donovan33].
The comparable rates of recent physical conditions among people with CMDs relative to those with SMI are surprising prima facie given the public health focus on the latter group [Reference Lewis and Hayes12]. However, our findings also showed the equally elevated rates of unhealthy lifestyle risk factors (e.g., obesity, alcohol consumption, and smoking) in people with CMDs, mirroring emerging findings [Reference Thapar, Collishaw, Pine and Thapar18]. The lack of physical health policies specific to people with CMDs may therefore not be a reflection of their lack of true physical health needs, but perhaps the result of an inadvertent oversight by policymakers to date.
To the best of our knowledge, only one previous smaller study (total n = 200) based in the United States has made direct comparisons of the rates of self-reported physical conditions between people with depression and those with schizophrenia receiving community care [Reference Sokal, Messias, Dickerson, Kreyenbuhl, Brown and Goldberg34], reporting findings in line with the current study. Data regarding physical conditions in both the latter and the current study were entirely obtained by self-report, calling reliability and validity into question, although studies elsewhere have evidenced the reliability of self-reports about physical conditions in people with mental illness [Reference Goldberg, Seybolt and Lehman35,Reference Reilly, Planner, Hann, Reeves, Nazareth and Lester36].
The excess physical health service utilization by people with CMDs compared with the general population is well recognized [Reference Katon37] and replicated by our findings. People with CMDs also had markedly higher odds than people with SMI for somatic hospitalization in the preceding 4 months despite no variation in the rates of recent GP consultations and somatic out-patient visits. These excess rates of hospitalization may reflect the systematically poorer healthcare for people with SMI in hospitals [Reference Lawrence, Holman, Jablensky and Hobbs20,Reference Manderbacka, Arffman, Sund, Haukka, Kemkimaki and Wahlbeck21,Reference Mitchell and Lawrence38], while paradoxically favoring people with CMDs [Reference Lawrence, Holman, Jablensky and Hobbs20,Reference Lawrence and Kisely39,Reference Shefer, Henderson, Howard, Murray and Thornicroft40]. It is well known that nonpsychiatric clinicians are less likely to make accurate somatic diagnoses and may provide suboptimal somatic health care to people with SMI relative to those with nonpsychotic mental disorders and the general population [Reference Shefer, Henderson, Howard, Murray and Thornicroft40]. People with SMI may also be less capable to describe their physical symptoms [Reference Shefer, Henderson, Howard, Murray and Thornicroft40], despite their motivation to access physical healthcare as frequently as those with CMDs as shown by our results. The combination of these factors may then lead to fewer hospitalizations being offered to them despite the clinical indication [Reference Shefer, Henderson, Howard, Murray and Thornicroft40]. On the other hand, people with CMDs may be prone to describe physical symptoms more emphatically by virtue of their neuroticism, leading to more frequent admissions even in the absence of clear need [Reference Buhagiar, Parsonage and Osborn6,Reference Lawrence, Holman, Jablensky and Hobbs20]. While the differential misclassification bias resulting from these opposing factors might have inflated the true estimate of the association between somatic hospitalization and CMDs, it is unlikely that it accounts entirely for the more than sixfold higher odds identified in our study. This finding thus underlines: (a) the significant synergy between physical health problems and CMDs, acting in a complex multifaceted manner; (b) the strain exerted on inpatient physical healthcare systems by people with CMDs; and therefore (c) the specific need to prevent and improve the care of physical health problems of people with CMDs. Our findings are closely in line with those of a robust large national study in Australia, showing lower rates of somatic hospitalization for people with SMI and higher rates for people with CMDs relative to the general population [Reference Lawrence, Holman, Jablensky and Hobbs20]. A more recent study using a large dataset from a county in the east of England, also confirmed the increased risk of somatic hospitalization for people with co-occurring anxiety and depression compared to those with no mental illness, at least in those over the age of 40 [Reference Remes, Wainwright, Surtees, LaFortune, Khaw and Brayne32].
Limitations
One limitation of the study is the small size of the SMI group, indicative of the relative rarity of psychotic symptoms across the population, yet potentially undermining the statistical power of our analyses. However, both the selection methods and the weighting procedures in the survey ensured that nonresponse bias was minimized on a range of sociodemographic and area characteristics, as demonstrated by the stable prevalence of psychosis compared with the earlier versions of the survey in 1993 and 2000 [24]. Furthermore, previous studies based on these participants with SMI have been robustly reported elsewhere [Reference Meltzer, Bebbington, Dennis, Jenkins, McManus and Brugha27,Reference Bebbington, Jonas, Kuipers, King, Cooper and Brugha41,Reference Jonas, Khalifeh, Bebbington, McManus, Brugha and Meltzer42]. In one such study [Reference Bebbington, Jonas, Kuipers, King, Cooper and Brugha41], multiple analyses were conducted to confirm the statistical power yielded by this group, as well as sensitivity analyses to confirm the validity of the results so obtained. Repeating similar power calculations and supplementary analyses for this sample was therefore beyond the scope of the current study.
Our participants with SMI do not necessarily meet the full criteria for a psychotic disorder such as schizophrenia. However, a previous analysis has demonstrated that participants reporting as little as one psychotic symptom on the PSQ share similar sociodemographic and clinical correlates to those with SMI proper [Reference Johns, Cannon, Singleton, Murray, Farrell and Brugha43]. Similarly, we also know that subtypes of CMDs carry heterogeneous patterns and strengths of associations with physical disorders [Reference Sareen, Cox, Clara and Asmundson15], yet we did not draw a distinction in our analysis between these different subtypes. However, there are strong overlaps in the psychological constitution of CMD participants [Reference Goodwin, Cox and Clara44].
Additionally, we make tentative inferences about the relative timing of onset of physical disorders from a cross-sectional survey. The issue of bidirectionality of the association between mental and physical health outcomes is an area of great complexity [Reference O’Neill, Williams, Stevenson, Oldenburg, Berk and Sanderson13,Reference Weich, Bebbington, Rai, Stranges, McBride and Spiers14], yet the design of our study precluded us from making temporal inferences with accuracy. A related issue is that of the discrepancy in the time-frame of the diagnosis (SMI, 1 year; CMD, at least 1 month). However, our sensitivity analyses that included only CMD participants with potential psychiatric symptoms in the previous year and/or already receiving psychiatric treatment, made little difference to the results.
Many of our physical conditions and physical health utilization variables were broad in their definition, although, this is an inherent limitation of using existing datasets.
The main advantage of the current study is the population-based approach. The sampling procedure ensured that a large probability sample representative of the entire population of England could be analyzed. The accompanying wealth of data provided the ability to control for important confounding covariates. Although the response rate of 57% was relatively modest, robust weighting procedures were incorporated in the analysis. The population-based approach also meant that sampling biases otherwise resulting from more circumscribed population groups employed in previous studies could be minimized. This was particularly the case in the CMD group, where only a small fraction of the participants had had contact with psychiatric secondary care. Well-validated instruments, including the CIS-R and the SCAN were used in order to ascertain the diagnosis. The use of a general population comparison group without psychiatric morbidity is a further strength.
Clinical implications
A main objective of the UK government’s mental health policy is to improve the physical health and reduced associated mortality in people with all mental disorders [45] and a drive to push forward the integration between physical and mental health care [46]. However, policy documents focusing on the physical health of people with mental disorders have generally only made fleeting reference to CMDs [Reference Goodwin, Cox and Clara44]. A number of strategies have also been implemented aimed at reducing the gap in physical health outcomes and mortality between people with SMI and the general population [47] but no comparable recommendations exist for people with CMDs [Reference Lewis and Hayes12]. Despite these efforts, the physical health and mortality gap between people with SMI and those without mental illness continues to prevail [Reference Hayes, Marston, Walters, King and Osborn11]. Given this context and the findings from our study, it is safe to postulate therefore, that in the absence of similar recommendations for people with CMDs, the physical health needs in this patient group continue to be unmet. Our findings affirm the continued burden of somatic comorbidity in people with mental disorders irrespective of the SMI/CMD dichotomy. Efforts to improve physical health outcomes therefore need to be directed to people with CMDs as well as SMI.
Conclusion
Our findings demonstrate the widespread physical health burden among people with CMDs relative to the general population, but more significantly also indicate that the physical health of people with CMDs may be just as poor as that of people with SMI. In clinical practice, a more proactive approach by policymakers and healthcare providers could ensure equity of healthcare provision and physical health outcomes across all vulnerable groups of people with mental illness.
Financial Support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors report no conflict of interest.
Data Availability Statement.
The data that support the findings of this study are openly available in the UK Data Service archive at http://doi.org/10.5255/UKDA-SN-6379-1 [24].
Supplementary Materials.
To view supplementary material for this article, please visit http://dx.doi.org/10.1192/j.eurpsy.2020.22.






Comments
No Comments have been published for this article.