No CrossRef data available.
Published online by Cambridge University Press: 16 April 2020
Rapid and robust antidepressant-like effect of ketamine in subanesthetic doses was already manifested in depressive patients. Maximum of mood improvement was shown within the period from 2 hours to 3 days. Previous studies proved predictive value of prefrontal QEEG theta cordance reduction after 1 week on a new antidepressant.
Congruently with previous findings we hypothesised in our compressed model decrease of QEEG cordance in 10 minutes of ketamine hydrochloride infusion as the prediction of antidepressant response.
14 MDD patients (6F/8M) diagnosed with a moderate to severe depressive episode without psychotic symptoms were included. All of the participants received the 30 minutes lasting only infusion with subanesthetic dose of ketamine hydrochloride solution (0.54 mg/kg). EEG measurements on the baseline, after 10 and 30 minutes of infusion were taken into account in computation of QEEG cordance.
9 (64.3%) of subjects responded to single ketamine infusion following day and 8 (88.9%) of them decreased QEEG cordance. T-test pair comparison found significant difference between baseline and after 10 minutes of ketamine infusion in responders (F = 4.12; p < 0.003).
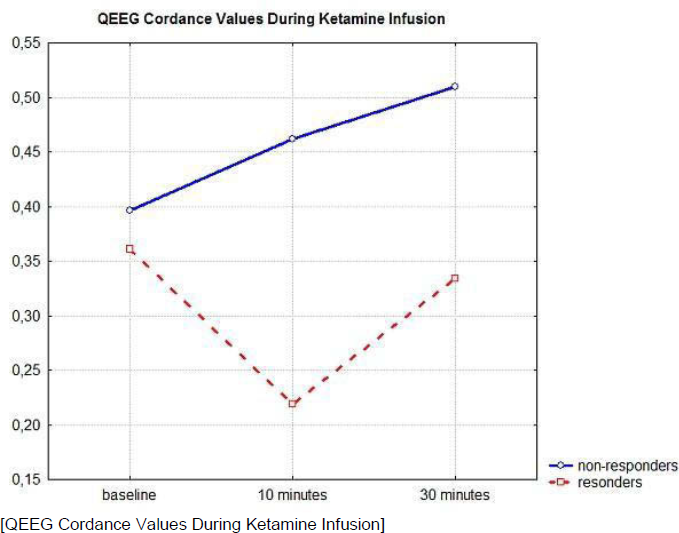
Preliminary results have shown the tendency of prefrontal QEEG cordance to decrease as a ketamine response prediction. Larger sample size is needed to increased precision in estimates of cordance sensitivity and specificity. Combination of latest QEEG method and fastest-acting antidepressant-like effect of ketamine in this trail is unexampled. Supported by IGA (MH CR) No.NS10379-3, 1M0517 (MEYS CR), MZ0PCP2005 (MH CR). Local Ethics Committee approval has been granted.
Comments
No Comments have been published for this article.