Background
As of December 14, 2020, 70.4 million confirmed cases of coronavirus disease 2019 (COVID-19) and 1.6 million deaths have been reported to the World Health Organization [1]. The outbreak of COVID-19 spread rapidly, caused enormous losses to individual health, national economy, and social wellbeing [Reference Steele, Orefuwa and Dickmann2,Reference Gardner and Moallef3]. Currently, control of the epidemic of COVID-19 is still the dominant task across the world, millions of people are scared and even panic of the possible loss of health, life, and wealth. Although it is too early to predict how many people worldwide will be infected with this emerging virus, it is believed that the numbers of case and death will continue to increase in the forthcoming months.
Some psychologists draw attention toward post-traumatic stress disorder (PTSD) as the second tsunami of the COVID-19 pandemic [Reference Dutheil, Mondillon and Navel4]. According to the Diagnostic and Statistics of Mental Disorders, the fifth edition (DSM-5), the clinical features of PTSD include persistent avoidance of stimuli, persistent intrusion symptoms, negative alterations in cognition or mood and marked alterations in arousal and reactivity, all of which are related to traumatic events [5]. PTSD could cause clinically significant distress or impairment in occupational, social, or other important functioning [Reference Greene, Neria and Gross6]. The outbreak of COVID-19 is the most severe pandemic since Spanish Influenza, the outbreak itself and the measures taken to bring it under control have likely been highly stressful for many individuals, which is very likely to promote PTSD [Reference Chang and Park7,Reference Lahav8]. Additionally, it is said that such new type of infectious diseases were very traumatizing for people across the world with a poor understanding of viruses and spreading mechanisms [Reference Dutheil, Mondillon and Navel4]. The evocation of COVID-19 is thus generating a great anxiety and biased responses to threat, which can also promote PTSD [Reference Bo, Li, Yang, Wang, Zhang and Cheung9].
When COVID-19 breaks out, people may experience many types of psychological trauma, such as directly suffering from the symptoms and traumatic treatment (respiratory failure, tracheotomy, etc.) [Reference Lahav8], witness of suffering, struggling, and dying of patients [Reference Fiorillo and Gorwood10]. Additionally, individuals may experience the fear of infection, social isolation, exclusion, and stigmatization, as patients, related caregivers, and workers, or even the general public [Reference Kisely, Warren, McMahon, Dalais, Henry and Siskind11,Reference Morganstein and Ursano12]. It is said that there is a dose–response relationship between the degree of trauma and the mental health burden of disasters [Reference Galea and Resnick13]. The prevalence of PTSD is higher among people who were directly exposed to the disaster, lower among related caregivers and rescue workers, and yet even lower in the general population. These different populations are likely to represent different levels of severity of trauma exposure, with direct victims having the highest exposure and associated PTSD prevalence while people in the general population having the lowest levels of exposure and associated PTSD prevalence [Reference Neria, Nandi and Galea14]. Currently, the relationship between the degree of trauma and the mental health burden of COVID-19 outbreak is unclear.
As one of the most widely researched consequence of traumatic events [Reference Neria, Nandi and Galea14], the prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak varies greatly across studies [Reference Salehi, Amanat, Mohammadi, Salmanian, Rezaei and Saghazadeh15–Reference Cenat, Blais-Rochette, Kokou-Kpolou, Noorishad, Mukunzi and McIntee18]. In addition, many factors have been reported to be associated with the prevalence of PTSD during COVID-19 outbreak, such as gender, age, and degree of trauma exposure [Reference Lahav8,Reference Cai, Hu, Ekumi, Wang, An and Li19,Reference Liu, Baumeister, Veilleux, Chen, Liu and Yue20], but the results are not consistent in different studies. The possible causes of the inconsistencies in the current estimates were unclear. For taking effective measures to reduce the psychological sequelae caused by COVID-19 across the world, it is necessary to determine a more accurate estimation of the prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak, and to explore the possible causes of the inconsistencies in the current estimates. This review aimed at examining the pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak, summarizing possible vulnerability factors of post-traumatic stress symptoms and examining potentially vulnerable populations, try to provide a reference for COVID-19 and possible outbreak of infectious diseases in the future.
Methods
This review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA guideline) and Meta-analyses of Observational Studies in Epidemiology guidelines [Reference Moher, Liberati, Tetzlaff and Altman21,Reference Stroup, Berlin, Morton, Olkin, Williamson and Rennie22]. The protocol of this review is registered in the International Prospective Register of Systematic Reviews (registration number: CRD42020180309). See Supplementary Material for the details.
Search strategy
PubMed, EMBASE, Web of Science, the Cochrane Library, MEDLINE, and Chinese National Knowledge Infrastructure were independently searched for published articles by two reviewers with no restrictions on date or language of publication up until 30 June 2020, and an update search was conducted on October 14, 2020. The following search terms were used: “COVID-19” (including “coronavirus disease 2019,” “SARS-CoV-2,” “severe acute respiratory syndrome coronavirus 2,” “COVID-19,” “Covid 19,” “SARS-CoV,” “novel coronavirus,” “coronavirus,” “CoV-2,” “2019-nCoV,” and “SARS COV2”); “Post-traumatic stress disorder” (including “post-traumatic stress disorder,” “post-traumatic syndrome,” “PTSD,” “stress disorder,” “post-traumatic,” and “post-traumatic syndrome”). See Supplementary Data for a full search strategy.
Study selection
Studies were included if they meet the following criteria: (a) the study was observational study; (b) the participants were adult aged ≥18; (c) information about prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was provided; (d) the full article was written in English or Chinese. Studies were excluded if (a) the report was a review, comments, meta-analysis, or protocol and (b) the participants with comorbid symptoms or chronic disease (such as mental illness, cancer, etc.).
Data extraction
Data extraction was conducted independently in pairs by trained researchers who used standardized data extraction forms. Two reviewers (D.Q. and Y.L.L.) checked the titles, abstracts, and full-texts of the initial search results independently. Data were extracted on first author, country or area, survey period, target population, study design, sample size, response rate, percentage of male participants, mean age of participants, instruments used to identify post-traumatic stress symptoms, prevalence of post-traumatic stress symptoms, and quality score of the included studies. Any discrepancies that emerged in these procedures were discussed and resolved by involving a third reviewer (S.Y.X.).
Quality assessment
Two independent reviewers (J.H. and F.Y.O.Y.) used the established guidelines, the Loney criteria, to evaluate the methodological quality of the included studies, which has been widely used to evaluate observational studies [Reference Loney, Chambers, Bennet, Roberts and Stratford23,Reference Sanderson, Tatt and Higgins24]. The included papers were scored according to eight criteria, such as study design, sample size, sampling method, response rate, definition of participants, appropriateness of measurement and analysis. The scores range from 0 to 8, with a score of 0–3 as low quality, 4–6 as moderate, and 7–8 as high [Reference Qiu, Yu, Li, Li and Xiao25]. See Table S3 for details on the quality assessment.
Statistical analyses
When data were available for three or more papers, prevalence was combined [Reference Becasen, Denard, Mullins, Higa and Sipe26]. When there were four or more papers, quantitative subgroup analysis was conducted [Reference Zachariae, Lyby, Ritterband and O’Toole27]. All the statistical analyses were performed using the “meta” (4.12-0) and “metafor” package (2.4-0) of R version 4.0.0. Between-study heterogeneity was evaluated by Cochran’s Q test and quantified by the I 2 statistic, with values >50% indicating moderate heterogeneity [Reference Ades, Lu and Higgins28,Reference Higgins, Thompson, Deeks and Altman29]. As we expected considerable heterogeneity, we calculated pooled prevalence with the random effects model. The pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was combined using Logit transformation method by a random effects model [Reference Higgins, Thompson, Deeks and Altman29,Reference Higgins30]. If more than one dataset was reported for the same group of participants, the outcomes that were assessed at the baseline were used. In order to compare the prevalence from different papers, we conducted subgroup meta-analysis. Because subgroup analyses should be interpreted with caution [Reference Jike, Itani, Watanabe, Buysse and Kaneita31], we planned a priori to limit our subgroup analyses to a small number of baseline characteristics including gender, age, area, population, survey time after the outbreak, sample size, assessment tool, and quality score. The difference between subgroups was examined using the Cochran’s Q chi-square tests [Reference Higgins30]. Mixed-model meta-regression analyses were performed by using Freeman–Tukey double arcsine method to explore potential moderators on the heterogeneity [Reference Dai, Liu, Kaminga, Deng, Lai and Yang32]. Publication bias was investigated by funnel plot and Egger’s test [Reference Higgins30,Reference Egger, Davey Smith, Schneider and Minder33]. To evaluate the consistency of the results, sensitivity analysis was performed. In this study, sensitivity analyses were planned a priori for the primary analyses set by: (a) excluding studies one by one and (b) excluding studies with extreme outcomes [Reference Higgins30,Reference Jike, Itani, Watanabe, Buysse and Kaneita31]. All the statistical tests were two-sided, with a significance threshold of p < 0.05.
Results
Literature search
As shown in Figure 1, a total of 7,032 references were identified. Among them, 3,897 duplicates were removed. By screening titles and abstracts, 2,964 irrelevant articles were excluded. A total of 171 potentially relevant full-text articles were independently assessed based on the selection criteria. Further, 95 studies were excluded because of the following reasons: duplicate articles or results (n = 6); review or conference abstract (n = 2); did not provide data on PTSD (n = 75); unable to locate full text (n = 10); not in English or Chinese (n = 1); and not for participants aged ≥18 (n = 1). Finally, 76 eligible studies were included in this review [Reference Chang and Park7–Reference Bo, Li, Yang, Wang, Zhang and Cheung9,Reference Cai, Hu, Ekumi, Wang, An and Li19,Reference Liu, Baumeister, Veilleux, Chen, Liu and Yue20,Reference Tee, Tee, Anlacan, Aligam, Reyes and Kuruchittham34–Reference Huang, Han, Luo, Ren and Zhou104]. The reliability for the full-text review between the two reviewers (D.Q. and Y.L.L.) was rated as good (Kappa = 0.78) [Reference Sands and Murphy105]. See Figure 1 for the details.
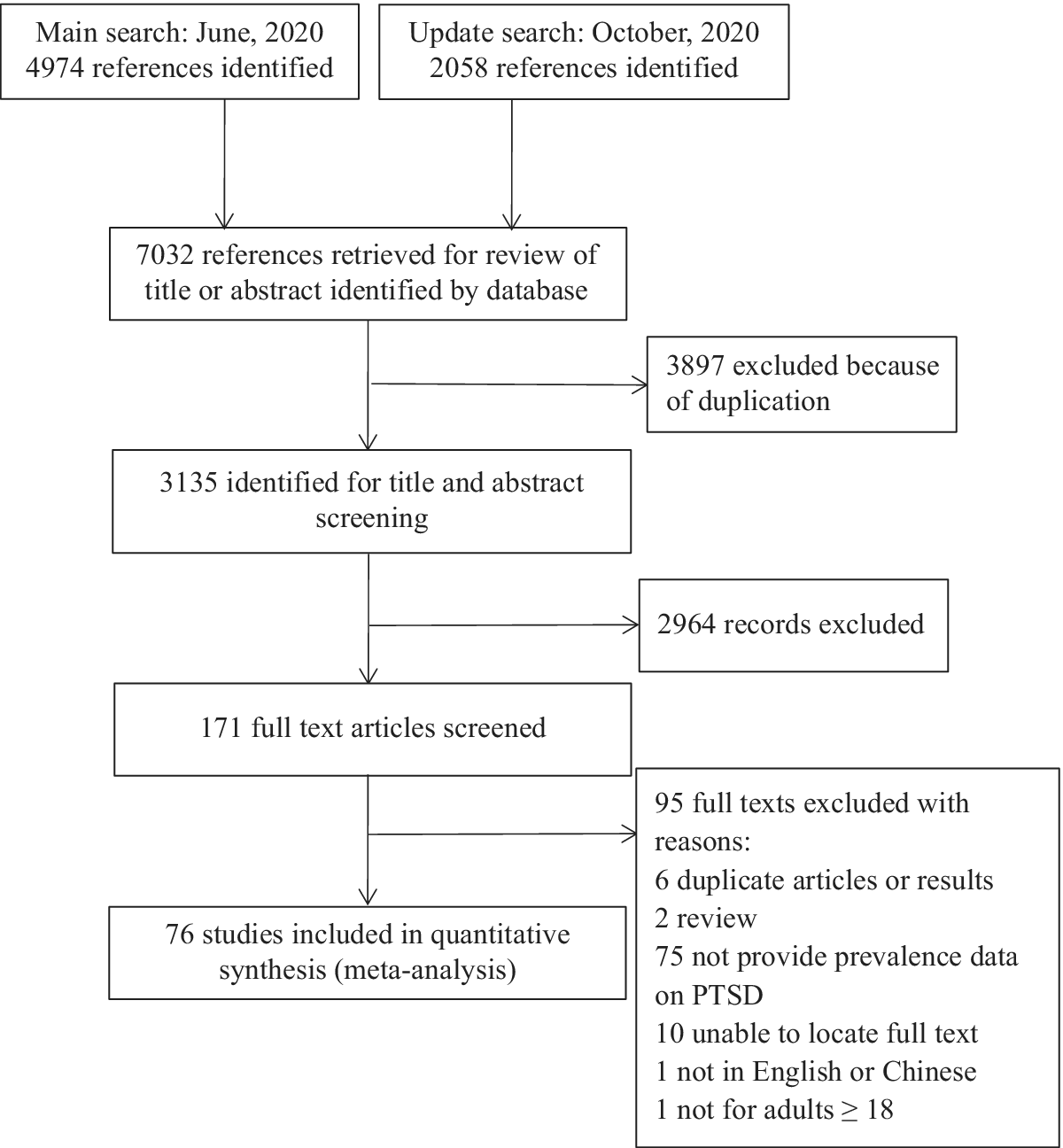
Figure 1. Flow of studies through review.
Study characteristics
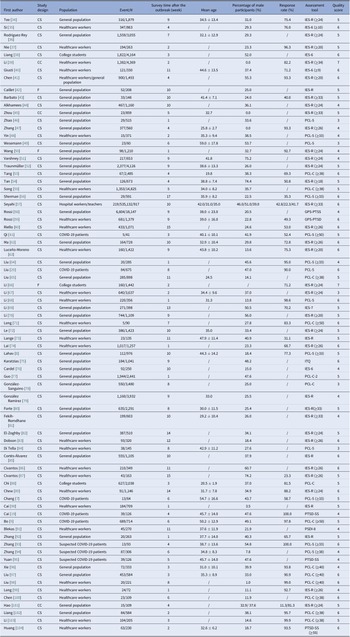
Table 1 presents the main characteristics of the 76 included studies. Among them, 66 were in English and 10 were in Chinese. Most of the included studies were from Asia, such as China, Indian, and Singapore. See Table 1 for the details. From the 76 papers, 1 (1.31%) study was rated as high quality, 70 (92.11%) were rated as moderate, and 5 (6.58%) were rated as low quality. The reliability for the quality assessment between the two reviewers (J.H. and F.Y.O.Y.) was rated as good (Kappa = 0.73) [Reference Sands and Murphy105]. For data extraction, all the criteria received a kappa value >0.85. Details of the methodological quality assessments of all 76 studies are showed in Tables S2 and S3.
Table 1. Study characteristics of the included studies.
Abbreviations: CC, case–control study; COVID-19: coronavirus disease 2019; CS, cross-sectional study; F, follow up study; IES-6, The Impact of Event Scale-6; IES-R, The Impact of Event Scale-Revised; ITQ, The International Trauma Questionnaire; PCL-5, the Post‐traumatic stress disorder checklist‐5; PCL-C, The amended self-reported Post-Traumatic Stress Disorder (PTSD) Checklist-Civilian Version; PSDI-8, Posttraumatic Stress Disorder-8 inventory; PTSD-SS, Post-traumatic stress disorder self-rating scale.
Pooled prevalence of post-traumatic stress symptoms among people influenced by the COVID-19 outbreak
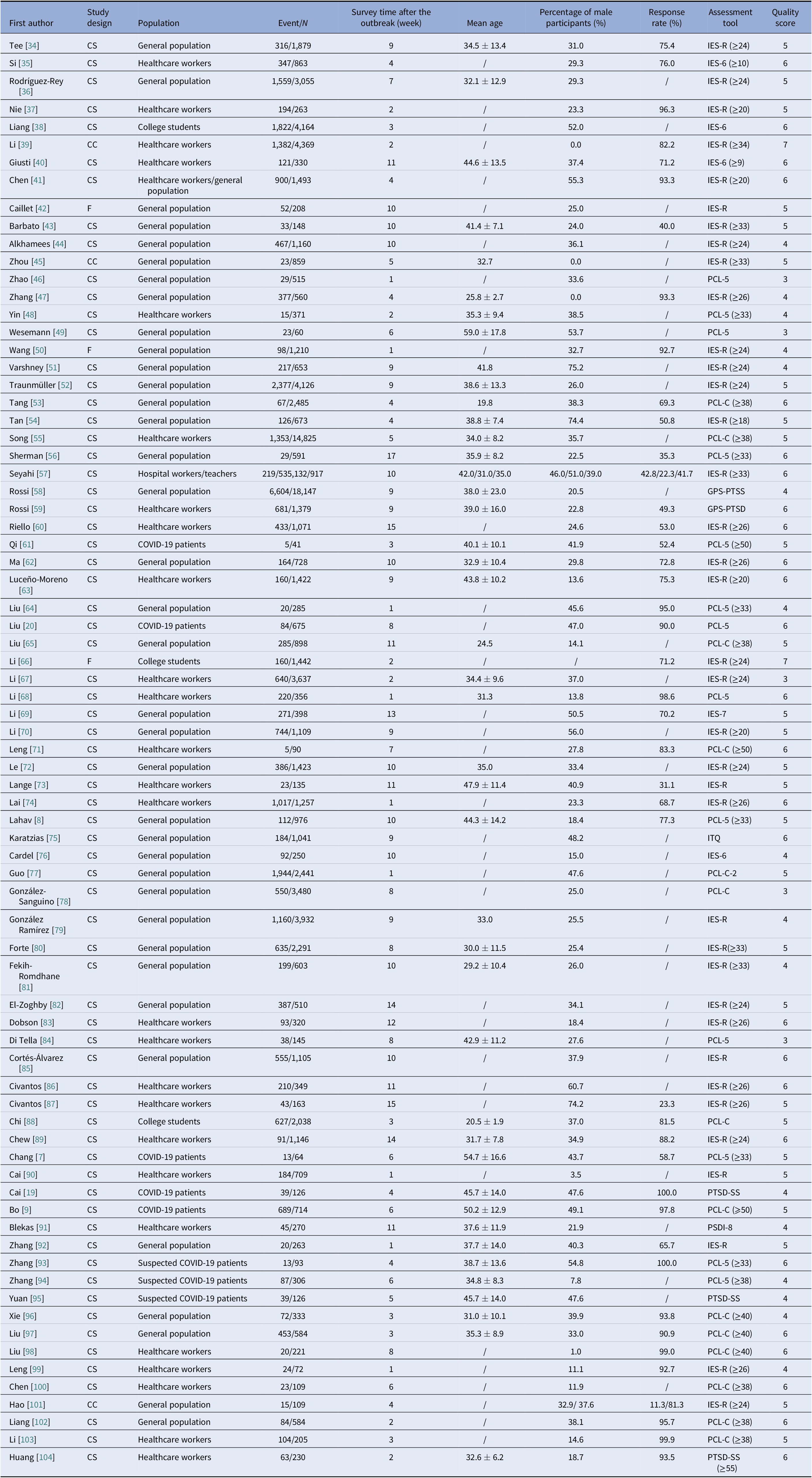
There were 76 studies reported prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from the COVID-19 outbreak. The forest plot in Figure 2 depicts the details. A total of 106,713 people exposed to the trauma resulting from the COVID-19 outbreak were identified in the 76 articles, of which 33,810 were reported with post-traumatic stress symptoms. The random effects model was used to determine the pooled prevalence (Q = 14,854.51, I 2 = 99.70%, p < 0.001), the pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was 28.34%, with a 95% confidence interval (CI) of 23.03–34.32%.
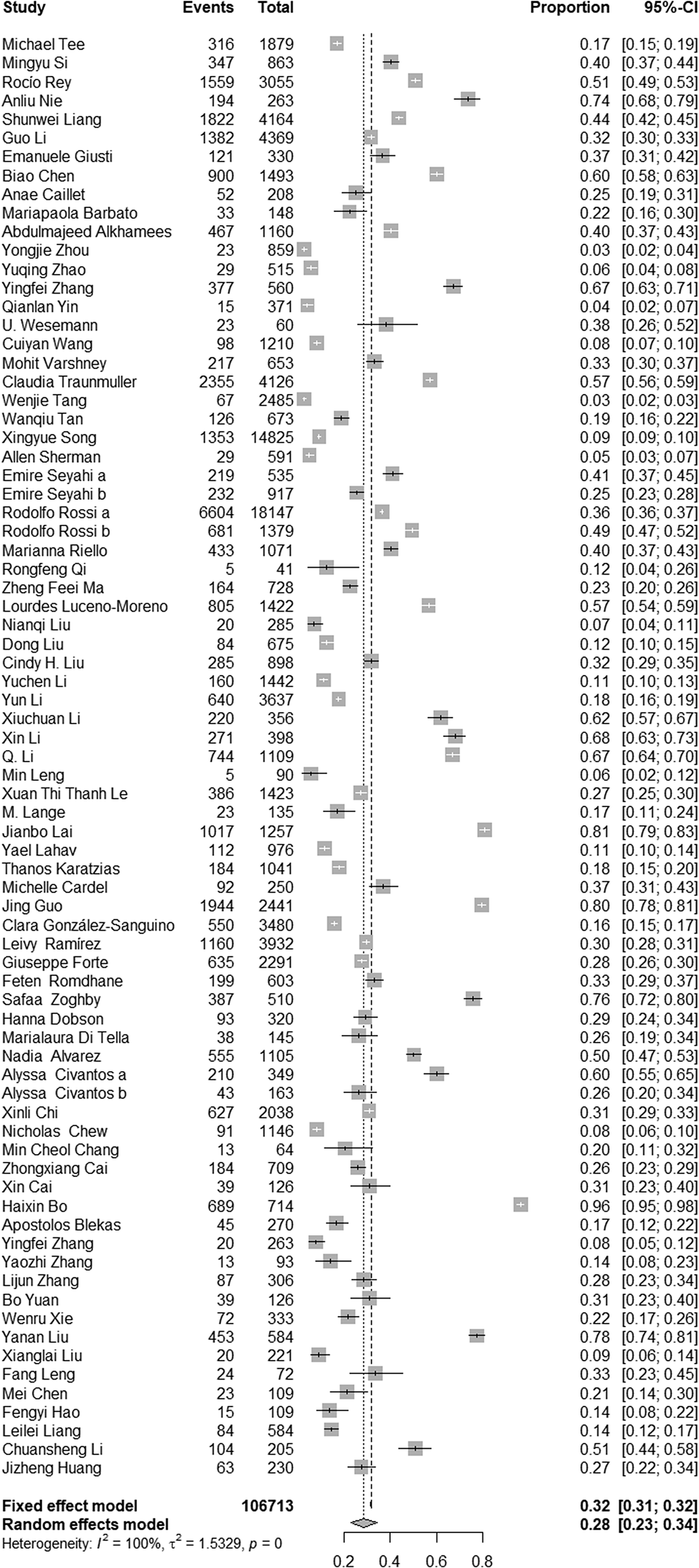
Figure 2. Forest plots.
Subgroup analysis for the included studies
The details of subgroup analyses are presented in Table 2. Significant differences in the prevalence of post-traumatic stress symptoms between different ages were found (Q = 221.97, p < 0.001). The results indicated that older participants (with a mean age ≥51) showed higher prevalence of post-traumatic stress symptoms (62.16%), younger participants (with a mean age between 18 and 20) showed lowest prevalence of post-traumatic stress symptoms (2.70%). Significant difference in the prevalence of post-traumatic stress symptoms between different gender was observed, the results indicated that studies with higher percentage of male participants (>50%) showed higher prevalence (26.70 vs. 41.79%; Q = 5.31, p = 0.021). The pooled prevalence of post-traumatic stress symptoms among people in the European region, the America region, the Eastern Mediterranean region, the Western Pacific region, and the South-East Asia region were 32.13%, 30.48%, 37.74%, 26.34%, and 17.16%, respectively. No significant differences in the prevalence of post-traumatic stress symptoms between different region were found (Q = 2.94, p = 0.580). Furthermore, the pooled prevalence of post-traumatic stress symptoms among people in the high-income region, the upper-middle-income region, and the lower-middle-income region were 30.03, 27.26, and 36.07%, respectively. No significant differences in the prevalence of post-traumatic stress symptoms between different income classification were found (Q = 0.81, p = 0.667). Also, the pooled prevalence of post-traumatic stress symptoms among COVID-19 patients, healthcare workers, suspected cases of COVID-19, the general population, and teachers/students were 36.30, 29.22, 24.47, 27.13, and 29.39%, respectively. No significant differences in the prevalence of post-traumatic stress symptoms between different population were found (Q = 0.87, p = 0.928). Although the prevalence of post-traumatic stress symptoms greater in earlier surveys (31.49%) than later surveys (25.79%), there were no significant differences in prevalence of post-traumatic stress symptoms between different survey time after the outbreak (Q = 1.05, p = 0.304). In addition, significant difference in the prevalence of post-traumatic stress symptoms between studies with different sample size was observed, articles with higher sample size showed lower prevalence (20.33 vs. 32.08%; Q = 6.61, p = 0.010). Studies used Impact of Event Scale (IES) as assessment tool showed higher prevalence (33.43%), studies used the amended self-reported PTSD Checklist—Civilian Version as assessment tool showed lowest prevalence (21.41%) and studies used Post-Traumatic Stress Disorder Self-Rating Scale, International Trauma Questionnaire, and Post-Traumatic Stress Disorder-8 Inventory showed moderate prevalence (28.96%). No significant differences in the prevalence of post-traumatic stress symptoms between studies used different assessment tools (Q = 3.47, p = 0.176). Lastly, no significant differences in the prevalence of post-traumatic stress symptoms between studies with different quality scores were observed (28.57 vs. 28.00%; Q = 0.01, p = 0.992).
Table 2. Subgroup analysis for the general population.
Abbreviations: COVID-19, coronavirus disease 2019; PCL-C, The amended self-reported Post-Traumatic Stress Disorder (PTSD) Checklist-Civilian Version; WHO, World Health Organization.
Meta-regression analyses for the included studies
Table 3 presents the results of meta-regression analyses. Due to too much missing data (only 57.89% of studies reported data) on the mean age of participants, we were unable to include this variable in the meta-regression model. Bivariate meta-regression suggested that higher prevalence estimates reported in studies which used IES as assessment tool (β = −0.11, p = 0.061). Specifically, assessment tool accounted for 3.16% of the heterogeneity across studies, but the difference between different groups was not significant. In addition, area (β = −0.03, p = 0.568), income (β = 0.01, p = 0.882), population (β = 0.06, p = 0.626), percentage of male participants (β = 0.01, p = 0.473), survey time after the outbreak (β = 0.01, p = 0.775), quality score (β = 0.03, p = 0.407), and sample size (β = −0.01, p = 0.891) were not significant moderators too. Of the multivariate model, no significant moderators for heterogeneity were found (p > 0.05, R 2 = 0.00%).
Table 3. Meta-regression analysis for the included studies.

Abbreviations: COVID-19: coronavirus disease 2019; IES, The Impact of Event Scale.
Publication bias and sensitivity analysis
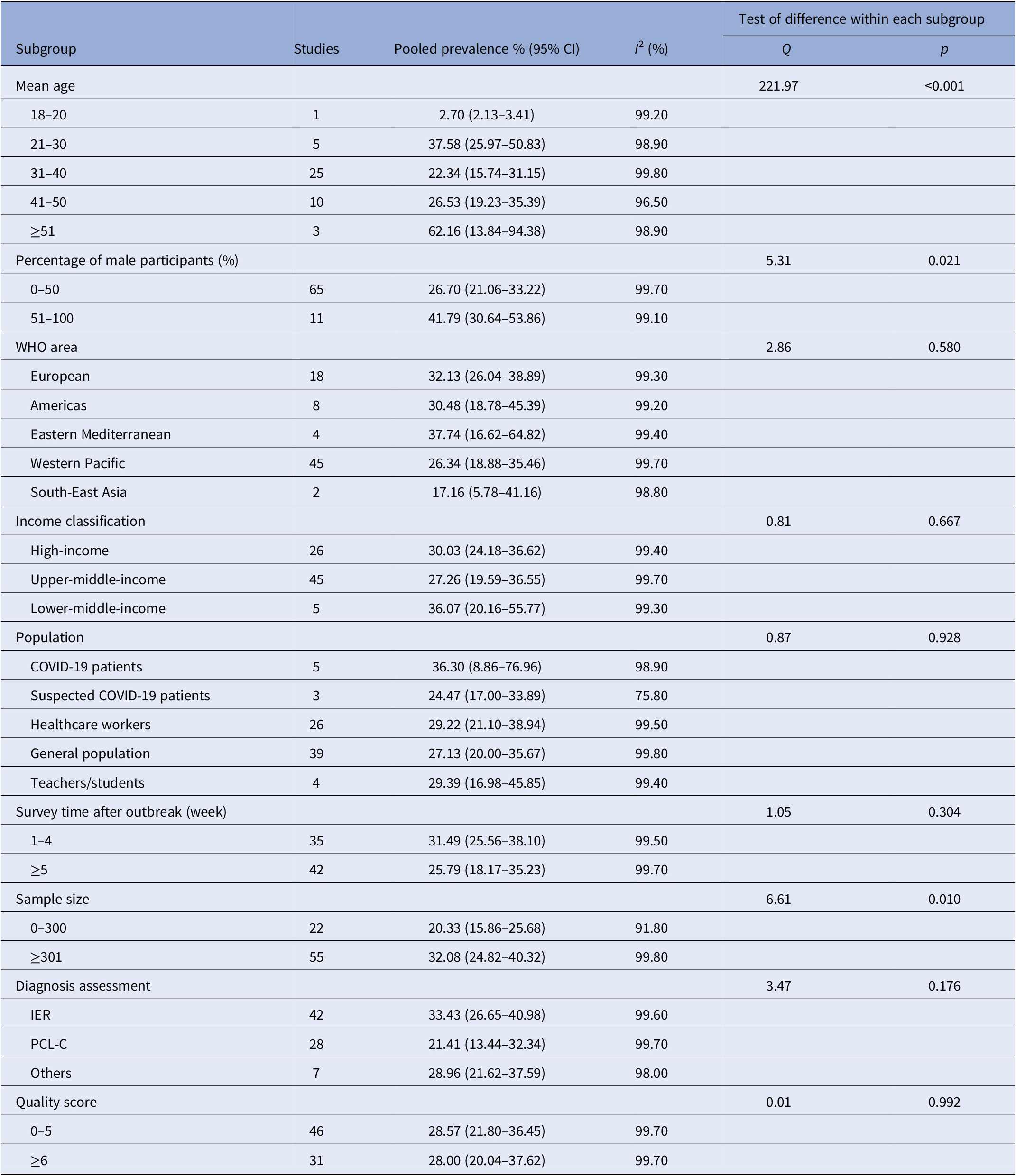
Funnel plot of publication bias is presented in Figure 3. The funnel plot of publication bias is basically symmetric, but publication bias cannot be ruled out, so Egger’s test was conducted. The results of the Egger’s test showed that publication bias was not found in this study (t = −0.971, p = 0.334).

Figure 3. Funnel plot of publication bias.
When each study was excluded one-by-one, the recalculated combined results did not change significantly. The pooled prevalence of post-traumatic stress symptoms ranged from 27.18% (95% CI: 22.40–32.55%) to 28.96% (95% CI: 23.72–34.81%), and the I 2 statistic has remained at 99.7%. The results in the current study indicate that no individual study significantly influenced the overall results. In order to examine the influence of extreme cases on the current results, we excluded all the extreme results to conduct a sensitivity analysis (with a prevalence <5% or >70%). After removing eight studies [Reference Bo, Li, Yang, Wang, Zhang and Cheung9,Reference Zhou, Shi, Liu, Peng, Wang and Qi45,Reference Tang, Hu, Hu, Jin, Wang and Xie53,Reference Sherman, Williams, Amick, Hudson and Messias56,Reference Lai, Ma, Wang, Cai, Hu and Wei74,Reference Guo, Feng, Wang and van IJzendoorn MH.77,Reference El-Zoghby, Soltan and Salama82,Reference Liu, Jiang, Cao, Zhou and Li97], the pooled prevalence of post-traumatic stress symptoms was 26.20% (95% CI: 22.17–30.67%), and the I 2 statistic was 99.5%. Compared with the initial results, no significant changes were found. See Figure S1 for the details of sensitivity analysis.
Discussion
Key findings
This review has highlighted the importance of considering the psychological impacts of people exposed to the trauma resulting from COVID-19 outbreak. A total of 106,713 people exposed to the trauma resulting from the COVID-19 outbreak were identified in the 76 articles, of which 33,810 were reported with post-traumatic stress symptoms. The pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was 28.34%, with a 95% CI of 23.03–34.32%.
Comparison with the literature
Based on the results of the World Health Organization World Mental Health Surveys in 2017, the global lifetime prevalence of PTSD-related symptoms among the general population was 3.90–5.60% [Reference Koenen, Ratanatharathorn, Ng, McLaughlin, Bromet and Stein106]. The pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak in this study was 28.34%, which was much higher than the general population. Between December 2019 and May 2020, a few reviews related to mental health and infectious disease outbreak reported limited data on pooled prevalence of PTSD-related symptoms during the COVID-19 outbreak. In Salehi et al.’s [Reference Salehi, Amanat, Mohammadi, Salmanian, Rezaei and Saghazadeh15] study, the pooled prevalence of PTSD-related symptoms during the coronavirus outbreaks (SARS, MERS, and COVID-19) was 18%, which was much lower than our results. In Krishnamoorthy et al.’s [Reference Krishnamoorthy, Nagarajan, Saya and Menon16] study, the pooled prevalence of PTSD-related symptoms during the COVID-19 outbreak ranged from 21.94 to 27.00% [Reference Cooke, Eirich, Racine and Madigan17,Reference Cenat, Blais-Rochette, Kokou-Kpolou, Noorishad, Mukunzi and McIntee18], were lower than our results. Those researches have explored a variety of mental health problems (such as depression, anxiety, and insomnia), PTSD is only one of the outcomes. Thus, we believe their search strategies on PTSD are inaccurate enough and the data they included were limited, which may affect the results. Despite the high heterogeneity in their studies, no subgroup analysis was conducted to explore the source of the heterogeneity on the pooled prevalence of PTSD in most of them [Reference Salehi, Amanat, Mohammadi, Salmanian, Rezaei and Saghazadeh15,Reference Krishnamoorthy, Nagarajan, Saya and Menon16,Reference Cenat, Blais-Rochette, Kokou-Kpolou, Noorishad, Mukunzi and McIntee18], which we think is another limitation. In Cooke et al.’s [Reference Cooke, Eirich, Racine and Madigan17] study, although the source of the heterogeneity was explored, they only included age and gender as moderators. Moreover, we found that the pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was higher than flood survivors (15.74%) and hurricane survivors (17.81%) [Reference Wang, Wu, Dai, Kaminga, Wu and Pan107,Reference Liu, Petukhova, Sampson, Aguilar-Gaxiola, Alonso and Andrade108], but equal to earthquake survivors (23.66%) [Reference Dai, Chen, Lai, Li, Wang and Liu109]. Compared with COVID-19 outbreak, some natural disasters such as flood and hurricane can be predicted, while earthquakes, infectious disease like COVID-19 were often happened suddenly and without a warning, pose a huge threat to people’s health and property in a short period of time [Reference Dai, Chen, Lai, Li, Wang and Liu109]. Therefore, earthquakes and infectious disease outbreak might have caused more damage to people’s mental health than flood and hurricane.
The prevalence of post-traumatic stress symptoms in older adults is significantly higher than the younger people in the subgroup analysis, which was consistent with other studies [Reference Dai, Liu, Kaminga, Deng, Lai and Yang32]. Due to too much amount of missing data (only 57.89% of studies reported data on mean age of participants), we were unable to include this variable in the meta-regression model. Thus, this observation requires further clarification. Based on the current results, healthcare providers should pay more attention to the assessment of early trauma responses among older COVID-19 patients in the clinical practice and implement early psychological interventions accordingly. It is said that females were more likely to develop PTSD [Reference Dai, Chen, Lai, Li, Wang and Liu109]. In the current study, however, males were associated with higher prevalence of post-traumatic stress symptoms. The possible reason is that males are more likely to be affected by COVID-19 and reported a higher fatality rate [Reference Del Sole, Farcomeni, Loffredo, Carnevale, Menichelli and Vicario110], they may experience higher level of severity of trauma exposure. In addition, although the epidemic situation is more serious in Europe and the Americas, no significant difference was found between different regions. It might be related to issues with numbers of studies, we think more prevalence studies in low-income countries are needed to understand the panorama of PTSD among people influenced by COVID-19. Besides, Previous research has shown that patients of infectious disease often directly suffering from the symptoms and traumatic treatment. After being cured, they were more vulnerable to social discrimination than other groups [Reference Neria, Nandi and Galea14]. These experiences may result in higher prevalence of PTSD among them when compared with other populations. Although the prevalence of PTSD among COVID-19 patients is higher than that of other populations in this study, the difference is not significant, which need further exploration. Also, post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak were higher in the immediate aftermath of the outbreak (0–4 weeks), but the difference was not significant, which was inconsistent with other studies [Reference Dai, Chen, Lai, Li, Wang and Liu109,Reference Righy, Rosa, da Silva, Kochhann, Migliavaca and Robinson111,Reference Heron-Delaney, Kenardy, Charlton and Matsuoka112]. The possible reason is that the epidemic has not abated over time and has been spreading, people have been exposed to the trauma resulting from COVID-19 outbreak. Thus, we think ongoing surveillance is essential. Furthermore, we found that the pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak identified by different assessment tools was not significant. Studies have indicated that prevalence identified by screening tools were higher than prevalence identified by diagnostic tools [Reference Edmondson, Richardson, Fausett, Falzon, Howard and Kronish113]. However, all the included studies in this study were used screening tools, we were unable to explore the difference. It is note of worthy that some instruments derived from different conceptualization of the disorder and they may encompass different symptoms (e.g., Impact of Event Scale-Revised derived from the Diagnostic and Statistical Manual-Fourth Edition, Text Revision (DSM-IV-TR) while Post-Traumatic Stress Disorder Checklist-5 from DSM-5, including more symptoms than the former) [Reference Murphy, Ross, Ashwick, Armour and Busuttil114]. Given that the included articles use many different screening tools, we think further research is needed to explore the influence of different screening tools on the prevalence of PTSD among people influenced by COVID-19 outbreak. It is reported that studies with poor methodological quality generally yielded more extreme prevalence estimates [Reference Mata, Ramos, Bansal, Khan, Guille and Di Angelantonio115], the current study showed similar results. After controlling for other factors, however, the results of meta-regression showed that the influence of methodological quality on prevalence is no longer significant. Hence, this observation requires further clarification.
Implications for the future
Epidemiological studies have demonstrated a rather high prevalence of mental health problems among different population after an epidemic of infectious disease [Reference Tucci, Moukaddam, Meadows, Shah, Galwankar and Kapur116–Reference Hong, Currier, Zhao, Jiang, Zhou and Wei118]. While most of these mental health problems will fade out after the epidemic, symptoms of PTSD may last for a prolonged time and result in severe distress and disability [Reference Vyas, Delaney, Webb-Murphy and Johnston119]. In terms of applicability to COVID-19, we think ongoing surveillance is essential and healthcare policies need to take into account both short-term and long-term preventive strategy of PTSD. In addition, all the included studies identified PTSD by self-reporting questionnaires rather than clinical interviews by professional psychiatrists, as a consequence of which, the pooled prevalence of PTSD may have been overestimated. Only 6.39% reported data on COVID-19 patients. Thus, we think a large multicenter prospective study using a single validated measure of PTSD and measuring possible confounding factors in randomly selected COVID-19 patients is needed in the future, which would provide a more accurate estimate of PTSD among people influenced by COVID-19 outbreak, especially for COVID-19 patients. Although, there is little doubt that there is a dose–response relationship between the degree of trauma and the mental health burden of disasters [Reference Neria, Nandi and Galea14], this relation may not necessarily mean that the principal mental health burden of people exposed to the trauma resulting from COVID-19 outbreak is among those who were most directly affected by the disease [Reference Galea and Resnick13]. It will be important to establish whether indirect exposure to a trauma during a COVID-19 pandemic was correlated with higher risk of PTSD. Also, it is necessary to assess the relation between exposure to multiple traumas and risk of PTSD in the future. Additionally, subgroup analyses and the meta-regression analysis did not identify major sources of the heterogeneity although a high degree of heterogeneity between studies was observed. Therefore, there might be a considerable amount of uncertainty regarding the pooled prevalence of PTSD among people influenced by COVID-19 outbreak. Future research should, therefore, explore more potential risk factors for PTSD among people influenced by COVID-19 outbreak, especially genetic background as well as social support, previous traumatic events or concomitant psychiatric disorder [Reference Dai, Chen, Lai, Li, Wang and Liu109,Reference Koenen, Nugent and Amstadter120].
Limitations
Firstly, we excluded studies were not written in English or Chinese. Besides, although subgroup analyses and meta-regression analyses were conducted to control many moderating factors for the pooled prevalence of post-traumatic stress symptoms, heterogeneity was still remained in this review. It is reported that heterogeneity is difficult to avoid in meta-analysis of epidemiological surveys, [Reference Winsper, Ganapathy, Marwaha, Large, Birchwood and Singh121] which suggesting the need for caution when drawing inferences about estimates of PTSD in post-disaster research. Additionally, although our study included relevant studies across 30 countries, more than half of the eligible studies were from upper-high income countries. Prevalence studies were scarce for many countries, especially for low-income countries. Considering the inconsistency of the healthcare environment and socioeconomic status across the world, more prevalence studies in low-income countries are needed to understand the panorama of PTSD among people influenced by COVID-19 outbreak. Also, we noticed that all the included studies were used screening tools to assess post-traumatic stress symptoms, no studies included were used diagnostic tools. It is possible that the pooled prevalence of post-traumatic stress symptoms caused by COVID-19 outbreak was overestimated in this review. Thus, we think ongoing surveillance is essential. Lastly, some included studies were investigated the prevalence before the time threshold from the first event (usually 30 days), we were unable to check this possible bias between studies. Although we explored the influence of survey time on the pooled prevalence, no significant result was found, which need further clarification.
Conclusion
This review has highlighted the importance of considering the psychological impacts of people exposed to the trauma resulting from COVID-19 outbreak. A total of 106,713 people exposed to the trauma resulting from the COVID-19 outbreak were identified in the 76 articles, of which 33,810 were reported with post-traumatic stress symptoms. The pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was 28.34%, with a 95% CI of 23.03–34.32%. Further research is needed to explore more possible risk factors for post-traumatic stress symptoms and identify effective strategies for preventing and treating PTSD-related symptoms among people exposed to the trauma resulting from COVID-19 outbreak.
Abbreviations
- 95% CI
95% confidence interval;
- COVID-19
coronavirus disease 2019;
- DSM-5
diagnostic and statistics of mental disorders, the fifth edition;
- IES-6
The Impact of Event Scale-6;
- IES-R
The Impact of Event Scale-Revised;
- ITQ
The International Trauma Questionnaire;
- PCL-5
The Post-Traumatic Stress Disorder Checklist-5;
- PCL-C
The amended self-reported Post-Traumatic Stress Disorder (PTSD) Checklist-Civilian Version;
- PSDI-8
Post-Traumatic Stress Disorder-8 Inventory;
- PTSD
post-traumatic stress disorder;
- PTSD-SS
Post-Traumatic Stress Disorder Self-Rating Scale.
Financial Support
This research was supported by the Ministry of Science and Technology of China (Grant no.: 2016YFC0900802). The funding agency did not take part in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Conflict of Interest
The authors declare no conflicts of interest.
Authorship Contributions
D.Q., S.Y.X., and Y.L.L. contributed to the design of the study. D.Q. and Y.L.L. screened the text. D.Q. and L.L. extracted and analyzed the data. J.H. and F.Y.O.Y. conducted the quality assessment. D.Q. wrote the first draft of the manuscript with input from S.Y.X. All the authors approved the final manuscript.
Data Availability Statement
The data that support the findings of this study are available in Table 1 and the Supplementary Material.
Supplementary Materials
To view supplementary material for this article, please visit http://dx.doi.org/10.1192/j.eurpsy.2021.24.








Comments
No Comments have been published for this article.