Introduction
In their latest editions, both the diagnostical and statistical manual of diseases (DSM) and the international classification of diseases (ICD) have introduced a dimensional concept of personality disorders, measured in part by personality functioning [1, 2]. Historically, the concept of personality functioning was first introduced in the operationalized psychodynamic diagnosis (OPD) almost 30 years ago [Reference Cierpka3]. Based on psychoanalytic theory, especially ego psychology, it was used to describe psychological abilities of a person to cope with inner conflicts and interpersonal problems [Reference Cierpka3]. According to the, personality functioning can be described by four dimensions each subdivided with regard to the self and others: perception, regulation, communication and attachment capacity (Supplement A) [Reference Cierpka3]. A patient can be categorized into one of 4 levels depending on the severity and rigidity of their impairment in one subdimension [Reference Cierpka3, 4]: High, moderate, low level of integration or disintegration. Finally, an overall impression was made on the basis of these assessments and the focus of treatment was set on the basis of this assessment.
In 2013, the DSM took up a long-standing criticism of the existing model of personality disorders, as it was shown that only 50% of all personality disorders are represented by the existing categories [Reference Blüml and Doering5, Reference Mitmansgruber6]. Furthermore research accumulated that personality disorders seemed to be based on intrapsychic and interpersonal impairment [Reference Bender, Morey and Skodol7]. In developing a model for personality functioning, the DSM-5 task force was inspired by existing models from psychoanalytic research [Reference Bender, Morey and Skodol7]. One influential model was Kernberg’s model of personality organization, which encompassed identity, reality testing, defense, and object relations [Reference Blüml and Doering5, Reference Bender, Morey and Skodol7, 8]. In this synthesis of the existing research situation, the DSM-5 task force decided to divide personality functioning into two basic dimensions, each with two subdimensions: the self with identity and self-direction and interpersonal relationships with empathy and closeness [1].
In 2021, the 11th revision of the ICD also introduced a dimensional model of personality disorders [2]. As in the AMPD of the DSM-5, the ICD-11 distinguishes between the self and interpersonal skills, but does not further divide them into two subdimensions. The ICD-11 also retains a distinction of impairment in 4 levels: severe, moderate and mild personality disorder and personality difficulty [Reference Blüml and Doering5, Reference Mitmansgruber6, 9]. The ICD-11 added a new assessment of the chronicity and rigidity of impairments [9].
To summarize in both the DSM-5 and the ICD-11 personality functioning is considered to be an underlying construct of personality disorders. In the OPD, personality functioning is seen as a person’s psychological abilities that they develop over the course of their life to cope with inner conflicts and interpersonal problems. Thus, the conceptualization in the OPD includes most of the concepts from both the DSM-5 and ICD-11 (Supplement A) [Reference Cierpka3, 4, Reference Zimmermann, Müller, Bach, Hutsebaut, Hummelen and Fischer10]. In fact, Zimmermann et al. could show that the global measurements of the OPD, the DSM-5 and the ICD-11 measure the same latent construct [Reference Zimmermann, Müller, Bach, Hutsebaut, Hummelen and Fischer10]. Recent studies have shown that personality functioning also varies in depressive disorders and anxiety disorders and can be used to predict how quickly a patient will improve in psychotherapy[Reference Doubkova, Heissler, Preiss and Sanders11-Reference Kindermann, Rollmann, Orth, Friederich and Nikendei13]. This suggests that personality functioning should not only be seen as a construct to capture personality disorders, but as a more general construct. Therefore, for this study, we use the OPD definition of personality functioning.
Along with this, research in recent years has shifted to view personality functioning as a dimension to be improved through psychotherapy: Several authors found that personality functioning can be improved by inpatient and outpatient psychotherapy [Reference Huber, Zimmermann and Klug14-Reference Lindfors, Knekt, Lehtonen, Virtala, Maljanen and Härkänen20]. However, only few studies have investigated the predictors of improvement in personality functioning: Flemming et al. found high attachment avoidance to be predictive of less improvement [Reference Flemming, Lübke, Masuhr, Jaeger, Brenk-Franz and Mestel21]. Kvarstein et al. found that borderline personality disorder was associated with greater improvements and older age with lower improvements in personality functioning [Reference Kvarstein, Frøyhaug, Pettersen, Carlsen, Ekberg and Fjermestad-Noll22].
Explorative, data-driven procedures, commonly described as machine learning, represent one possible approach to determine influencing factors of improvement in personality functioning [Reference Bi, Goodman, Kaminsky and Lessler23-Reference Hastie, Tibshirani and Friedman25]. In supervised machine learning, the mathematical algorithm attempts to develop a model that predicts the dependent variable with as little error as possible [Reference Hastie, Tibshirani and Friedman25]. Depending on the structure of the data and the researcher’s objective, various mathematical algorithms can be used [Reference Hastie, Tibshirani and Friedman25, Reference Barber26]. However, this explorative, data-driven approach is rarely used in psychotherapy research, especially psychodynamic psychotherapy research [Reference Aafjes-van Doorn, Kamsteeg, Bate and Aafjes27, Reference Rollmann, Gebhardt, Stahl-Toyota, Simon, Sutcliffe and Friederich28].
Considering the aspects mentioned above, the present study was designed to utilise machine learning to identify relevant variables that predict the improvement of personality functioning. For this purpose, we considered all variables that were routinely recorded at the beginning of psychotherapy at the Heidelberg Institute for Psychotherapy (HIP) as potential predictors [Reference Schauenburg, Dinger, Kriebel, Huber, Friederich and Herzog29]. Then, we used supervised learning algorithms to filter for variables that are relevant for predicting the improvement of personality functioning. Finally, we verified our results on a separate data set to assess generalizability.
Methods
Study design
This study involves an exploratory and retrospective analysis of routinely assessed longitudinal psychotherapy treatment data from the Heidelberg Institute for Psychotherapy (HIP), University of Heidelberg in Germany. The HIP is a training institute for psychodynamic therapists [Reference Schauenburg, Dinger, Kriebel, Huber, Friederich and Herzog29].
Participants
Patients
This study is based on a sample of NPatients = 648 completed outpatient psychodynamic psychotherapies. Age ranged from 18 to 76 years (M = 35.6, SD = 13.1). On average, patients received 53.7 sessions of psychotherapy (SD = 28.4, range: 1 to 120). The number of SKID-Diagnoses ranged from 0 to 10 (M = 2.4, SD = 1.6). Overall improvement in personality functioning ranged from -1.4 to 1.7. These psychotherapies took place between January 2013 and July 2021. Patients were included after providing written informed consent. To be included in the study, patients had to (1) be 18 years old, (2) speak German or English and (3) have had at least one diagnostic session with a therapist.
Therapists
All therapists were in training to become psychodynamic orientated therapists. NTherapists = 172 therapists participated in this study. Therapists had to (1) either have a degree in psychology (M.Sc. or Ph.D.) or be a medical resident (MD) and (2) have at least 1.5 years of clinical experience. On average, each therapist treated approximately M = 9.4 patients (SD = 5.4). The treatment was supervised every fourth session by an experienced psychodynamic orientated therapist with at least five years of experience.
Ethics
The study protocol was developed according to the Helsinki II declaration [Reference Williams30]. Prior to recruitment of patients and therapists, the study was approved by the independent ethics committee of the Medical Faculty of the Heidelberg University (S-195/2014). Written informed consent was obtained from all study participants.
Procedure
Diagnostic assessment
Each patient took part in a clinical interview in an outpatient department to assess the indication for a psychodynamic psychotherapy [Reference Schauenburg, Dinger, Kriebel, Huber, Friederich and Herzog31]. In this interview, the patients were informed about the study and invited to participate. Written informed consent was then given. After the intake interview, patients answered sociodemographic and psychometric questionnaires and were invited to a standardised diagnostic interview [SCID-I and SCID-II; [Reference First and Gibbon32], German version: [Reference Wittchen, Zaudig and Fydrich33]] with a trained psychologist. Finally, the patient was referred to one of the study therapists.
Psychotherapy
The treatment took place once a week for 50 minutes and consisted of individual depth psychologically founded psychotherapy [Reference Ermann34]. Treatment focuses on current psychosocial problem, which are worked through as re-actualized conflicts and results of structural deficiencies [Reference Ermann34]. Mean number of session was 53.7 (SD = 28.4). German public health insurance covers the full cost of treatment if patients apply for a distinct number of sessions in advance (12, 24, 60 or 100 sessions). Before applying for a distinct number of psychotherapeutic sessions, patients attend up to seven diagnostic and preparatory sessions for diagnostic reasons. The number of sessions is agreed upon with the therapist. After the first therapy session, the therapists and patients were asked to complete psychometric questionnaires. At the end of the last psychotherapy session, both the patient and the therapist were asked to complete psychometric questionnaires once again.
Instruments
Patients and therapists were asked to complete a total of 14 different psychometric questionnaires after the initial intake interview and the first requested session. Please see Supplement B for a description of all 14 questionnaires.
Data analysis
The complete analysis was done using R version 4.3.1. [35]. The individual steps of the data analysis can be seen in Figure 1. We operationalized our target variable ‘improvement in personality functioning’ by subtracting the mean value of the OPD-SQ post-questionnaire from the mean value of the OPD-SQ pre-questionnaire. A positive difference value therefore indicates an improvement in personality functioning.
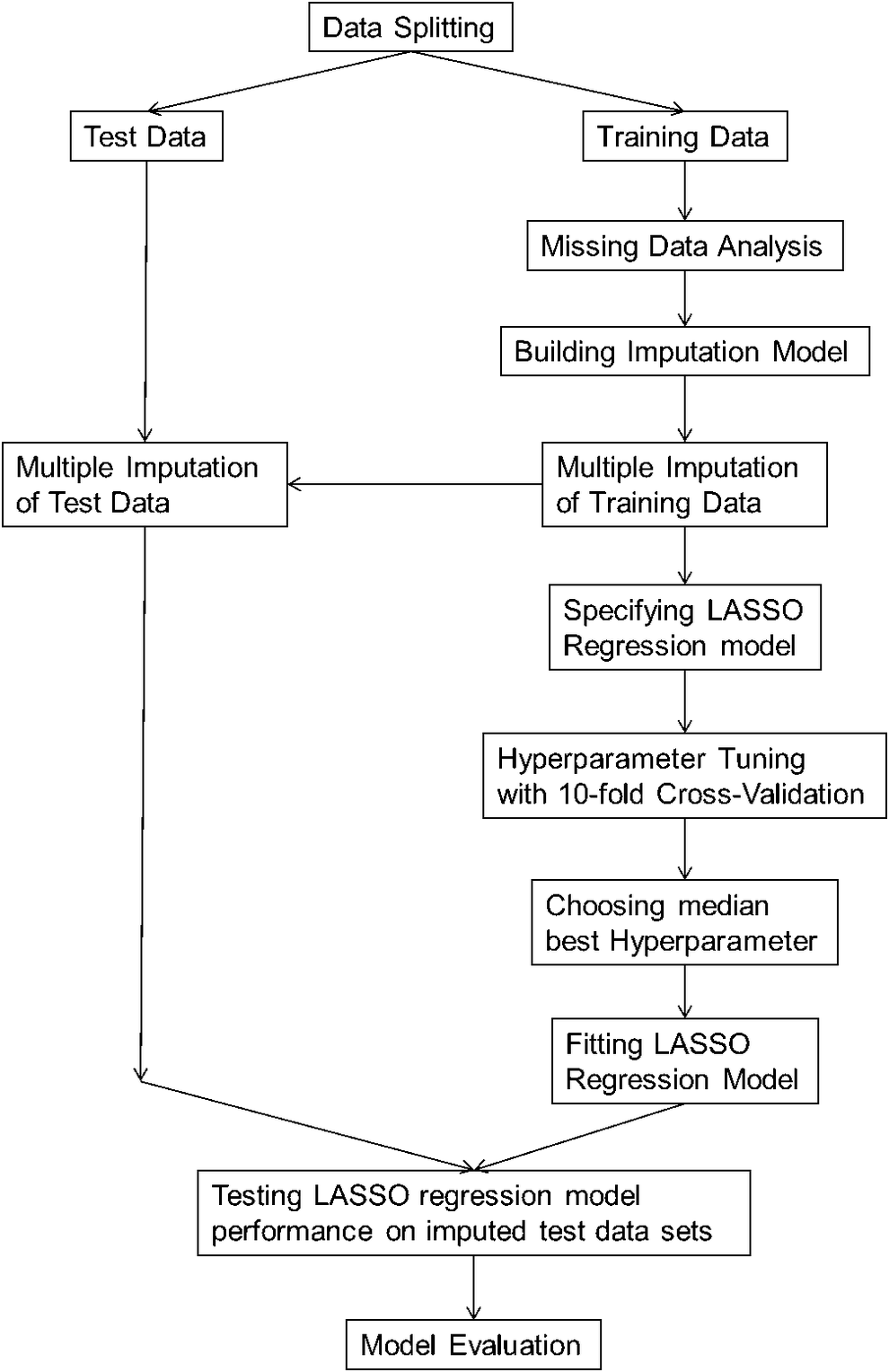
Figure 1. Data analysis‘ process.
Data splitting
To allow an unbiased assessment of model performance, to check for overfitting and to only utilize training data for model development we first randomly divided the dataset into training and test data [Reference Hastie, Tibshirani and Friedman25, Reference Van Buuren36]. Using the “Rsample” package [Reference Kuhn and Wickham37], we split the data into 80% training (Ntraining = 518) and 20% test data (Ntest = 130).
Missing data analysis (of training data)
We removed variables with more than 30 % missing values and an influx above 0.5 [Reference Van Buuren36]. Our target variable ‘improvement of personality functioning’ had 42% missing values and in total the training data had 14.4% missing values. All missing values correlated significantly with each other. We concluded that it was a patient variable that generated the missing values. The missing values in our target variable ’improvement of personality functioning’ correlated with previous inpatient psychiatric treatment, with substance abuse disorder, with the way therapy ended (regular, terminated, prematurely ended), and negatively with school education. Since we recorded all these variables and were able to incorporate them into our imputation model, we assumed a ’missing at random’ process to be reasonable.
Building imputation model
We performed the multiple imputation using the ‘mice’ package [Reference Van Buuren36, Reference van Buuren and G-O38]. All variables with a correlation of at least 0.2 were used as predictors, resulting in a median of 28 predictors per variable. Sums and means of several scales were imputed using passive imputation, other variables were imputed with predictive mean matching [Reference Van Buuren36]. Based on our considerations above, the end of therapy (completed, terminated, prematurely ended) was also added as a predictor for all variables. We first generated 10 imputed training data sets with 120 iterations of the algorithm. Plotting the means against the iteration number the streams intermingled freely with no definite trends [Reference Van Buuren36]. Furthermore, density plots and scatter plots showed that the data could have come from real patients. We judged the imputation model as being good and used it to create 30 imputed training data sets each using 150 iterations of the algorithm. Using the same imputation model, we created 30 imputed test data sets.
Lasso regression model
Predictors. All sociodemographic variables and scales of the psychometric questionnaires that were available at the beginning of therapy were used as predictors.
Hyperparameter Tuning and Selection. We used the ‘glmnet’ package [Reference Friedman, Tibshirani and Hastie39] and the ‘tidymodels’ [Reference Kuhn and Wickham37] framework for hyperparameter tuning and all other following calculations. We opted for a lasso regression, as it uses soft thresholding to remove all variables with low regression coefficients from the model by setting the regression weight to zero [Reference Hastie, Tibshirani and Friedman25]. The strength of the thresholding depends on a hyperparameter λpenalty that we determined for all 30 imputed training data sets with 10-fold cross validation, using 2001 evenly distributed possible values for λpenalty between 0 and 0.5 [Reference Hastie, Tibshirani and Friedman25]. For each of the 30 imputed training data sets, we then selected the λpenalty with the lowest cross validation mean absolute error (MAEcv).
Model Performance. Then, a final lasso regression model for each of the 30 training datasets was calculated using the median of the 30 selected λpenalty. To check for overfitting, we tested all 30 models on all 30 imputed test data sets. For each test data set, we predicted the improvement in personality functioning and calculated the MAEtest. Then, we pooled the MAEtest using Rubin’s rule [Reference Van Buuren36]. Overfitting was defined as MAEtest being two standard deviations above MAEcv.
Model Evaluation. For each variable, we calculated 2 parameters: the pooled regression weight according to Rubin’s rule [Reference Van Buuren36] and the number of models in which the regression weight of the variable was set to zero. If the regression weight of a variable was set to zero in five or less models, the variable could be described as a robust predictor.
Transparency
Our complete analysis and the analysis code can be found under the following DOI: doi.org/10.11588/data/50WFVL. To ensure the transparency of our evaluation, we adhere to the TRIPOD guidelines [Reference Collins, Reitsma, Altman and Moons40]. The datasets used and analysed during the present study cannot be shared due to restrictions by the Ethics Committee of the University of Heidelberg.
Results
Training and test sample description
The description of our training and test sample as well as the grand means of imputed training and test data sets can be seen in Table 1. On average, the test sample included a larger proportion of women and a higher number of previously utilised psychotherapeutic and psychiatric services. The training sample contained a higher proportion of depressive disorders, somatoform disorders, and eating disorders. In contrast, the test sample showed a higher proportion of personality disorders and substance abuse disorders. Both samples had a similar average level of personality functioning at the start of therapy. However, the improvement in personality functioning in the training sample was greater. Patients in the test sample terminated their treatments less frequently and brought them to a regular end more often. Furthermore, the overall mean value of the imputed data hardly differs from the values of the non-imputed data. Due to these differences between training and test data, it can be assumed that the model only receives little information about the test data from the training data set. Checking the performance on the test data set therefore represents a good test for overfitting.
Table 1. Sample description of training and test sample
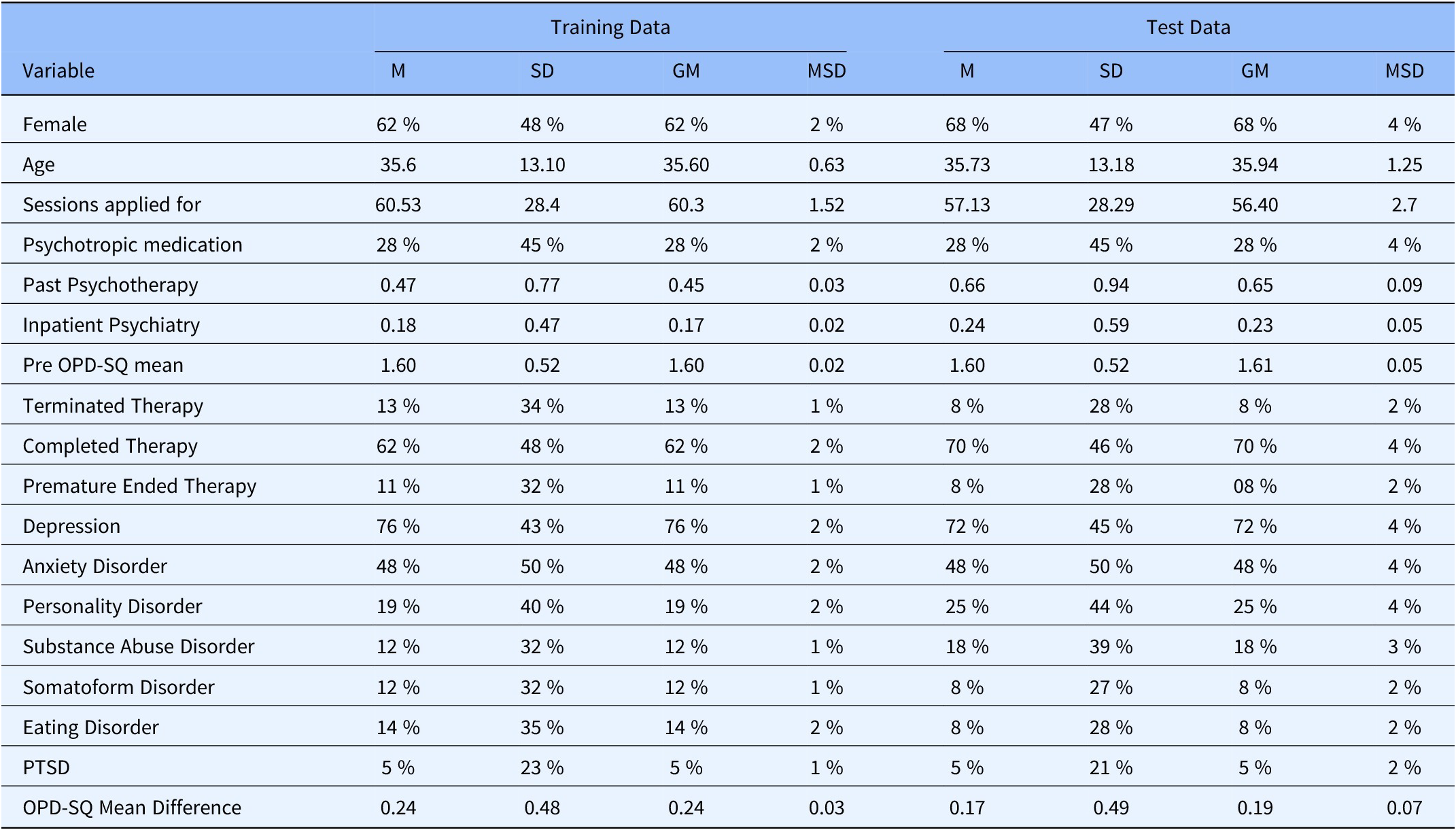
Note: M = Mean of Data without imputed data sets, SD = Standard Deviation of Data without imputated data sets, GM = Grand Mean of all imputed data sets, MSD = Standard Deviation of Means of imputed data sets. For Past Psychotherapy and Stationary Psychiatry values represent the mean number of previous treatments, respectively. Terminated, completed and prematurely ended therapies each indicate the proportion of patients who terminated therapy without the therapist’s consent, who completed therapy or who had to terminate therapy prematurely with the therapist’s consent.
Evaluation of overfitting
Figure 2 shows the cross-validation and test MAE plotted against imputation. Across all imputations, the deviation of the test MAE is smaller than two standard errors of the test mean absolute error. Therefore, we assume that we have not overfitted our model. The mean cross-validation MAE is 0.37 (SE = 0.01) and the mean test MAE is 0.42 (SE = 0.04). This means that the prediction of the improvement in personality functioning by our model deviates from the actual improvement by a median of 0.37 in the training data set and by a median of 0.42 in the test data set.

Figure 2. Comparison of cross-validation and test mean absolute error.
Note: Black line represents Cross-validation errors and white line represents test errors. Grey area represents two standard errors, respectively.
Evaluation of model error
Figure 3 shows an example of the performance of the final model on the test data. The model overestimates the improvement in personality functioning in patients who have not improved or even deteriorated. On the other hand, it underestimates the improvement of patients who improved significantly. Overall, however, there is a linear relationship between the prediction of the model and the actual improvement in the patient’s personality functioning (rmedian = 0.391, rmean = 0.386, rmin = 0.147, rmax = 0.568). Thus, the trend of the prediction corresponds to the actual improvement of the patient.

Figure 3. Example plot of model test errors.
Final model
Removed variables
The number of models a variable was removed from can be seen in Table 2. Eight variables were used in all models: The Intercept, pre OPD-SQ mean, the scale ‘limitation in social activities’ of the SF, the scales ‘Too caring’ of the IIP, the scale ‘Depression’ of the PHQ, the scale ‘Task’ of the WAI rated by the therapist, gender, and former outpatient psychiatric treatment. Furthermore, 6 variables were used in 29 of 30 models: the scales ‘Hard to be involved’ and ‘Hard to be supportive’ of the IIP, the subscale ‘Stress’ of the PHQ, former inpatient psychiatric treatment, the scale ‘Smoothness’ of the SE rated by the therapist, and retirement of the patient. In total we found 25 robust predictors of improvement in personality functioning, which can be seen in Table 2.
Table 2. Average penalized regression weights and number of times variable was removed
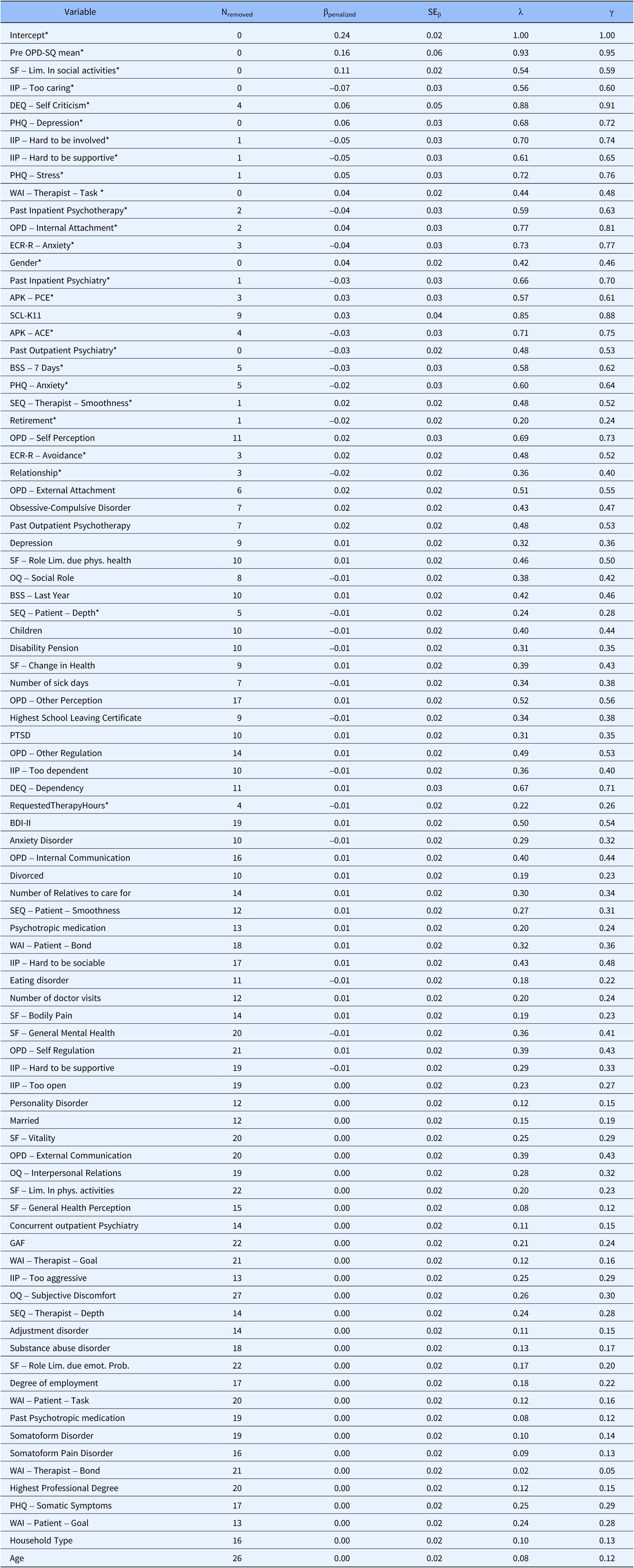
Note: Nremoved = Number of models this variable was removed from. βpenalized = Grand mean of the penalized regression coefficient. SEβ = Rubin’s rule pooled standard error of the penalized regression coefficient. λ = Proportion of Variation of βpenalized attributable to missing data. γ = Fraction of information missing about βPenalized due to missing data. Caution: As βpenalized is not t-distributed significance calculation cannot be done. Gender: men = 1, women = 2. All variables were standardised. This means that the βpenalized indicates by how much the improvement in personality functioning changes if the respective variable is increased by 1 standard deviation. Variables which were set to zero in five or less models, and defined as robust, are marked by a*.
Influence of variables
The pooled penalized lasso regression coefficients of a variable on the improvement in personality functioning can also be seen in Table 2. The absolute size of the pooled penalized lasso regression coefficients correlates with the number of models in which a variable was removed (r = -0.588).
Influence of missing values on results
Table 2 also shows how much variance was generated by the missing values or how much information was lost. A lot of variance was generated by the missing values, especially for the variables with a large pooled penalized lasso regression coefficient.
Discussion
We used machine learning to filter for variables that predicted the improvement of personality functioning. Then, we checked the model for overfitting on a separate test data set. There was no overfitting as the final model showed a comparable performance to the training data set. Personality functioning improved on average by 0.24 (SD = 0.48) points on the OPD-SQ scale from an initial average value of 1.60 [Reference Ehrenthal, Dinger, Horsch, Komo-Lang, Klinkerfuss and Grande41]. This corresponds to a medium effect size [Reference Döring and Bortz42]. Compared to the development study of the OPD-SQ, this improvement in our sample corresponds to two thirds of what would be required to reach the level of personality functioning of a healthy control sample [Reference Ehrenthal, Dinger, Horsch, Komo-Lang, Klinkerfuss and Grande41]. In total, we found 25 robust predictors of improvement of personality functioning with mostly small effect sizes. This means that the improvement in personality functioning is primarily explained on a multi-causal basis. In the following, a sample of these 25 predictors are discussed.
The variable with the greatest predictive power is the initial impairment of personality functioning. Patients with greater impairment at the beginning of outpatient psychotherapy experience greater improvement in personality functioning during psychotherapy. This result is in line with the findings of Kvarstein et al., who also found that personality functioning can improve especially for severely impaired patients, such as borderline personality disorder patients [Reference Kvarstein, Frøyhaug, Pettersen, Carlsen, Ekberg and Fjermestad-Noll22]. Although we did not find a connection between treatment discontinuation and personality functioning in our study, this has been shown in other works [Reference Kiel, Hopwood and Lind15, Reference Bach and Simonsen43]. If it is possible to motivate these patients to complete psychotherapy, greater than average improvement in personality functioning can be expected.
The SF measures health-related quality of life in a total of nine different dimensions [Reference Bullinger44]. Of these, the scale “limitation in social activities because of physical or emotional problems” has the second greatest predictive power for improvement in personality functioning [Reference Bullinger44, Reference Bullinger and Kirchberger45]. Our results showed that patients who initially feel less restricted in social activities experience a greater improvement in personality functioning. One explanation could be that these patients experience more new relationships as a result of fewer limitations in social activities, which ‘improves’ their personality functioning [4, Reference Rudolf46]. Together with the previous result, this finding suggests that impairments in personality functioning and limitations in social activity due to emotional and physical problems do not necessarily coincide. If patients have similar impairments in personality functioning, the patient who experiences less impairment in social activities will experience greater improvements in personality functioning.
The IIP measures interpersonal problems on a total of eight scales, which can be understood as extreme expressions of two bipolar dimensions: “Dominance” and “Affiliation”. The “too caring” scale corresponds to one pole of the “affiliation” dimension, while the “hard to be involved” and “hard to be supportive” scales correspond to the other [Reference Barkham, Hardy and Startup47, Reference Thomas, Brähler and Strauß48]. In our study, we found that patients who are too self-sacrificing or too cold towards others experience less improvement in personality functioning. Our results are therefore not entirely consistent with previous research: Ruiz et al. found that all eight scales were related to less symptomatic improvement, whereas in our study only the Affiliation dimension proved to be relevant [Reference Ruiz, Pincus, Borkovec, Echemendia, Castonguay and Ragusea49]. In another study, contrary to our results, it was found that those patients who reported the most severe interpersonal problems at the start of inpatient psychotherapy experienced most symptom improvement [Reference Davies-Osterkamp, Strauss and Schmitz50]. The direction of the influence therefore remains unclear. Further, is also possible that the influence of interpersonal problems differ on symptoms and personality functioning, which could indicate that these two constructs are different. Nevertheless, the initial interpersonal problems appear to be an important predictor of improvement in personality functioning.
Previous authors looked at the influence of personality functioning on depression in the context of a diathesis-stress model [Reference Huber, Zimmermann and Klug14, Reference Kerber, Gewehr, Zimmermann, Sachser, J and Knaevelsrud51]: personality functioning is seen as a resource that protects against depressive symptoms [Reference Kerber, Gewehr, Zimmermann, Sachser, J and Knaevelsrud51]. On the other hand, an improvement in personality functioning was accompanied by more stable symptomatic improvement in follow-up measurements [Reference Huber, Zimmermann and Klug14, Reference Knekt, Virtala, Härkänen, Vaarama, Lehtonen and Lindfors18-Reference Lindfors, Knekt, Lehtonen, Virtala, Maljanen and Härkänen20, Reference Leichsenring, Jaeger, Masuhr, Dally, Dümpelmann and Fricke-Neef52]. Our study complements these results. We found that high levels of depression and stress in the PHQ predicted greater improvement in personality functioning [Reference Gräfe, Zipfel, Herzog and Löwe53, Reference Löwe, Spitzer, Zipfel and Herzog54]. This implies, that patients who are depressed or under greater stress also experience more improvement in their personality functioning. In consequence, these patients gain a resource that protects them from future depressive symptoms.
In contrast to Kvarstein et al., who found a negative effect of age but no effect of gender on the improvement of personality functioning, we found a greater improvement for women but no age effect [Reference Kvarstein, Frøyhaug, Pettersen, Carlsen, Ekberg and Fjermestad-Noll22]. Instead, we found that retired patients experience a smaller improvement in personality functioning. Thus, this is probably not an age effect, but an effect that occurs with retirement. In the study by Kvarstein et al., retirement was not included as a variable in the model [Reference Kvarstein, Frøyhaug, Pettersen, Carlsen, Ekberg and Fjermestad-Noll22]. Therefore, it is possible that the effect found by the colleagues is due to retirement and that there is no influence of age.
Limitations
Our study was a retrospective observational study that used only the variables collected at the start of treatment to predict improvement in personality functioning. Further statements, such as the improvement in personality functioning depending on the length of therapy, also remain unanswerable using this approach. Many of the variables are based on self-assessment questionnaires, for some of which stronger effects were also found. This could be due to a methodological similarity in the measurement method. Furthermore, our results are limited by the fact that we had many missing values in our data set. To address this, we conducted a detailed analysis of missing values and were able to assume a ’missing at random’ process by adding some variables to our multiple imputation model. We can therefore assume that our results are unbiased, but future studies should replicate our findings [Reference Van Buuren36]. Another limitation of this work is the lack of information about the therapists. Thus, we were unable to include possible relevant influencing variables, such as patient-therapist gender interactions, in our model. Whilst this is not a limitation of our study, it would be desirable to validate our model using patients outside the HIP [Reference Hastie, Tibshirani and Friedman25, Reference Collins, Reitsma, Altman and Moons40].
Conclusion
We found 25 variables which can be assessed at the beginning of psychotherapy that robustly predict improvement in personality functioning during psychotherapy. These results suggest a primarily multicausal influence of other variables on improvement of personality functioning. Three noteworthy findings emerged from these results. First, patients with initially highly impaired personality functioning particularly benefit from psychotherapy. Second, limitations in social activities because of physical or emotional problems predict lower improvement in personality functioning. Third, patients who are too cold or too self-sacrificing in relationships experience less improvement in personality functioning through psychotherapy. Taken together, these findings emphasize the interpersonal and social domains as significant in the treatment of personality functioning. Clinical colleagues can collect these variables at the beginning of psychotherapy in order to develop a prognosis for treatment.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1192/j.eurpsy.2024.1780.
Data availability statement
The analysis code and all results are available at doi.org/10.11588/data/50WFVL. The datasets used and analyzed during the present study cannot be shared due to restrictions by the ethical review board.
Acknowledgements
Sources of funding: none. We thank Molly Sutcliffe for English language editing.
Author contributions
IR was responsible for all the calculations and was responsible for conducting the study. SST was responsible for proofreading all calculations. DK, JN were responsible for checking the results. HCF and CN were the supervisors of the project. MO was responsible for collecting the data.
Funding
We received no external funding for this study.
Competing interest
No conflicts of interest are declared.
Ethics approval statement
Ethical approval was granted by the Ethics Committee of the University of Heidelberg: No. S-195/2014.
Patient consent statement
Written informed consent was obtained from all study participants.








Comments
No Comments have been published for this article.