1. Introduction
Most studies in eating disorders (ED) have mainly focused on anorexia nervosa (AN), bulimia nervosa (BN), and recently on binge eating disorder (BED), neglecting other residual or subthreshold ED such as eating disorder not otherwise specified (EDNOS). Based on the Diagnostic and Statistical Manual of Mental Disorders fourth edition (DSM-IV-TR) [Reference APA1], EDNOS category was defined as a broad hodgepodge that includes many heterogeneous and not well-defined ED cases (i.e. those who do not fulfill the diagnostic criteria for AN or BN). The update of the DSM-5 [Reference APA2] reconfigured and renamed EDNOS as other specified feeding or eating disorder (OSFED). OSFED is a formal diagnostic category including heterogeneous nosological entities, such as: atypical anorexia nervosa (atypical-AN), purging disorder (PD), subthreshold bulimia nervosa (Sub-BN), subthreshold binge eating disorder (Sub-BED), and night eating syndrome (NES). These changes into the diagnostic framework of ED aimed to reduce the overrepresentation of cases in this residual category of EDNOS [Reference Gualandi, Simoni, Manzato and Scanelli3–Reference Flament, Buchholz, Henderson, Obeid, Maras and Schubert6], as well as it attempts to enhance the study of more homogeneous phenotypes [Reference Murray and Anderson7].
However, because this nosology is relatively recent, most of the research in this field refers to EDNOS, while OSFED subtypes have barely been studied in the literature so far. Due to the vast majority of diagnoses in clinical practice fall within the atypical/subthreshold ED umbrella [Reference Thomas, Vartanian and Brownell8], this diagnosis has been reported as the most prevalent ED [Reference Larrañaga, Docet and García-Mayor9–Reference Micali, Horton, Crosby, Swanson, Sonneville and Solmi13], but often not less severe and enduring than full syndromes [Reference Thomas, Vartanian and Brownell8, Reference Fairburn, Cooper, Bohn, O’Connor, Doll and Palmer14, Reference Smink, van Hoeken, Oldehinkel and Hoek15]. Epidemiological studies show that the prevalence of OSFED is about 1.5%, less than half of the prevalence of DSM-IV EDNOS [Reference Mustelin, Lehtokari and Keski-Rahkonen16]. Regarding the specific OSFED subtypes, some few studies revealed prevalence rates range between 1.1–5.3% for lifetime PD, 2.8–3.6% for atypical-AN, 4.4% for Sub-BN, and 1.5–5.7 % for NES [Reference Murray and Anderson7, Reference Stice, Marti and Rohde17, Reference Hammerle, Huss, Ernst and Bürger18]. Nevertheless, these prevalence data are regarding specific community samples (mainly adolescent populations), and they are not generalizable to other populations such as clinical or adult samples.
Despite the relevance, chronicity and considerable clinical severity of OSFED [Reference Mustelin, Lehtokari and Keski-Rahkonen16] there is a lack of research analyzing therapy outcomes. The few studies comparing response to treatment between atypical/subthreshold ED and full syndromes found similar patterns of remission and relapse [Reference Keel and Brown19–Reference Krug, Casasnovas, Granero, Martinez, Jiménez-Murcia and Bulik21], but also high dropout rates among the formers [Reference Swan-Kremeier, Mitchell, Twardowski, Lancaster and Crosby22]. Heterogeneous results among diagnostic subtypes have been described in the literature, with PD patients showing the best prognosis [Reference Smith, Crowther and Lavender23], whereas atypical-AN and sub-BN patients not showing differences with the full-threshold EDs [Reference Ekeroth, Clinton, Norring and Birgegård24]. Moreover, although data on diagnostic crossover in EDNOS/OSFED are sparse, available findings suggest that approximately 40% of these patients develop AN or BN later in life [Reference Milos, Spindler, Schnyder and Fairburn25].
Taking into account all the aforementioned gaps in the literature, mainly contradictory findings and studies where atypical/subthreshold ED represented a negligible portion of the sample, it is not possible to generalize results or define a clear hypothesis about treatment outcome in these clinical populations. Therefore, in the present study we were focusing in the most prevalent OSFED subtypes (namely, atypical-AN, PD, and sub-BN), with the following goals: (a) to examine clinical, motivational, psychopathological, and personality differences among the groups; (b) to explore short-term treatment outcome, therapeutic adherence, and dropout rates; and (c) to identify clinical predictors of therapy outcomes. To our knowledge, this is the first study assessing treatment outcome and dropout rates between well-differentiated OSFED subtypes following outpatient cognitive-behavioral therapy (CBT), which may contribute to advancements in the debate about whether these diagnostic subtypes would benefit equally from a joint CBT treatment. Also, the findings derived from the study might improve our ability to identify and better understand OSFED subtypes and thereby aid in tailoring the best treatment alternatives.
2. Methods
2.1 Ethics approval
The present study was approved by the Ethics Committee of the University Hospital of Bellvitge and all the participants provided signed informed consent.
2.2 Participants
The initial sample consisted of 201 patients with OSFED, consecutively admitted for treatment at the Eating Disorders Unit of the Bellvitge University Hospital. Of those, were excluded: 8 men (3.9%), 9 females with subthreshold BED (4.5%), and 8 females with unspecified feeding and eating disorders (UFED) (3.9%) because the number was too small for meaningful comparisons. Therefore, the final sample comprised 176 female patients diagnosed with OSFED (82 atypical-AN, 57 PD, and 37 sub-BN). All patients admitted before May of 2013 were originally diagnosed using the DSM-IV-TR [Reference APA1]. Diagnoses were made by means of a face-to-face semi-structured clinical interview, based on the SCID-I [Reference First, Spitzer, Gibbon and Williams26], and conducted by experienced clinical psychologists and psychiatrists. Diagnoses were reanalyzed post hoc using DSM-5 criteria [Reference APA2].
Exclusion criteria were: (a) patients aged <18 years old; (b) patients presented with severe comorbid psychopathological symptoms (e.g. risk of suicidal attempt or psychotic/bipolar disorders) requiring individual therapy and/or inpatient therapy.
2.3 Assessment
- Eating disorders inventory-2 questionnaire (EDI-2) [Reference Garner27] (Spanish validation [Reference Garner28]) to assess behavioral and psychological dimensions of the ED. The internal consistency for the current sample was excellent (α =.94).
- Symptom Checklist-90-Revised (SCL-90-R) [Reference Derogatis29] (Spanish validation [Reference Derogatis30]). This questionnaire was designed to assess psychopathological distress. The internal consistency of our sample was excellent (α =.97).
- Temperament and Character Inventory-Revised (TCI-R) [Reference Cloninger31] (Spanish validation [Reference Gutiérrez-Zotes, Bayón, Montserrat, Valero, Labad and Cloninger32]). This questionnaire consists of 240 items that measure temperament and character dimensions. Cronbach’s alpha for the current sample was good for “novelty seeking” (α =.78) to excellent (α =.90) for “harm avoidance”.
- Motivational stage. The motivational stage of change was assessed through five visual analogue scales named: subjective desire for treatment, need of treatment; impairment, Worry [Self], and Worry [Family]. The scales ranged from 0 to 8, with 8 being the maximum score indicating worry and motivation for change. The scale has been previously described and applied in ED patients [Reference Casanovas, Fernández-Aranda, Granero, Krug, Jimenez-Murcia and Bulik33].
Additional information such as sociodemographic variables, impulsive behaviours, and other relevant clinical variables were assessed by means of a face-to-face semi-structured clinical interview [Reference Fernández-Aranda and Turón34].
2.4 Treatment
The National Institute for Health and Care Excellence (NICE guideline Published: 23 May 2017 nice.org.uk/guidance/ng69) recommends implementing the first-line treatment for the most closely resembling ED, being the cognitive behavioural therapy-Enhanced (CBT-E) the recommended treatment for adult patients with EDs.
Treatment for OSFED consisted of 16 weekly outpatient group therapy conducted by experienced psychologist. All patients were treated in the same set of therapy group. Despite the distinct OSFED subtypes present heterogeneous clinical and symptomatological features, the treatment addresses the core characteristics that are common in the full spectrum of ED, such as training in problem solving strategies, cognitive restructuring, emotion regulation, improving self-esteem and body image, and relapse prevention strategies. In addition, therapy aimed to address eating-related symptomatology, introducing eating monitoring, regular nutritional patterns and increasing knowledge about negative consequences of the disorder. The treatment protocol was manualized and published in Spanish [Reference Fernández-Aranda and Turón34].
Patients were re-evaluated at discharge and categorized into the following three categories: full remission, partial remission, and non-remission. According to DSM-5 criteria [Reference APA2], the working definition of full remission was a total absence of symptoms meeting diagnostic criteria for at least 4 consecutive weeks, partial remission was defined as substantial symptomatic improvement but with residual symptoms, and the patients who presented poor outcomes were defined as non-remission. These categories were previously used to assess treatment outcome in threshold ED in other published studies [Reference Sauchelli, Jiménez-Murcia, Sánchez, Riesco, Custal and Fernández-García35–Reference Agüera, Sánchez, Granero, Riesco, Steward and Martín-Romera37]. Voluntary treatment discontinuation was categorized as dropout (i.e. not attending treatment for at least three consecutive sessions).
2.5 Statistical analysis
Analyses were carried out with Stata15 for Windows. First, the comparison between the diagnostic subtypes was based on chi-square tests (2) for categorical variables and in analysis of variance (ANOVA) for quantitative measures. Effect size was estimated through the Cohen’s-d coefficient, considering moderate effect size for |d|>0.50 and high effect size for |d|>0.80 [Reference Kelley and Preacher38]. To avoid increase in Type-I error due to multiple statistical comparison, Finner’s procedure was employed [Reference Finner39], a method included into the Familywise error rate stepwise procedures, and offers more powerful test than the classical Bonferroni correction.
Kaplan-Meier functions estimated the cumulative survival for the time to dropout. This method, also known as the product-limit-estimator, is a non-parametric procedure to estimate the survival function from “lifetime data”, and in the area of the Health Sciences it is often used to measure the proportion of patient “living” (surviving) for an amount of time after one event. In this study, the Kaplan-Meier estimator measured the length of time that patients remain participant (without dropout). Overall comparison of cumulate survival functions between the three diagnostic groups was done with the Log-Rank, Breslow and Tarone-Ware tests.
Finally, logistic regressions generated predictive models of the main therapy outcomes of the study: the risk of dropout and the risk of good therapy outcome (partial or full remission). Stepwise procedure was used to automatically select the variables with most predictive capacity, and the models were generated separately/stratified for each diagnostic condition. The goodness-of-fit for the final models were valued with the Hosmer-Lemeshow test (adequate fitting was considered for p > 0.05), the overall predictive capacity with the Nagelkerke’s pseudo-R2 coefficient and the discriminative capacity to differentiate between the groups with the area under the ROC curve.
3. Results
3.1. Characteristics of the sample
Table 1 contains the descriptive for the sociodemographics in the sample of the study, and the comparison between the diagnostic subtypes. Many participants were single (77.3%), with primary (33.5%) or secondary (46.0%) studies, and employed or studying (71.0%). No statistical differences between groups were found.
Table 1 Descriptive for the sample.

Note. AN: anorexia nervosa. PD: purging disorder. Sub-BN: subthreshold bulimia nervosa.
3.2 Comparison of the clinical profile at baseline between the diagnostic groups
Table 2 contains the comparison between the groups for the categorical clinical variables of the study. For the whole sample, the prevalence of childhood obesity was 13.1%. The 12.5% of the participants reported lifetime overweight. Non-suicidal self-harm behaviors were present in 30.7% of the sample, suicidal ideation in 40.9%, and suicidal attempts in 11.9%. In relation to the use/abuse of substances: 36.4% indicated tobacco use, 6.8% alcohol use-abuse, and 16.5% recognize to consume other illegal drugs. No differences between the groups were obtained for this set of variables.
Table 2 Clinical comparison for categorical-binary variables.
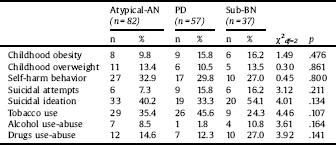
Note. AN: anorexia nervosa. PD: purging disorder. Sub-BN: subthreshold bulimia nervosa.
p-value includes Bonferroni-Finner’s correction for multiple comparison.
Table 3 contains the comparison between the groups for the quantitative clinical variables. Age of onset and duration of the disorder differed between the groups, being the PD subtype who has the latest age of onset, and the sub-BN the group with the longest duration of the disorder. Body mass index (BMI) measures also differed among the groups, being the atypical-AN phenotype the group with the lowest mean values, followed by the PD phenotype and lastly the sub-BN group. For the motivational scales, differences only emerged for the social impairment of daily tasks variable, which mean score was the highest for the sub-BN subtype. As expected, the frequency of vomits and laxatives achieved the highest mean in the PD group, followed by the sub-BN and the atypical-AN. Regarding EDI-2 scales, as a whole the highest means were obtained for the sub-BN, followed by the PD group and the atypical-AN. No statistical differences were found comparing the mean scores for the SCL-90R scales, and the only difference for the TCI-R scales was obtained for the persistence dimension (the highest mean was shown in the PD group, while no statistical difference emerged comparing atypical-AN and sub-BN).
Table 3 Clinical comparisons for quantitative clinical and psychometrical variables: ANOVA.

Note. AN: anorexia nervosa. PD: purging disorder. Sub-BN: subthreshold bulimia nervosa. SD: standard deviation. p-value includes Bonferroni-Finner’s correction.
* Bold: significant comparison (.05 level).
† Bold: effect size into the moderate (|d|>0.50) to good range (|d|>0.80).
3.3 Comparison of the therapy outcome between the diagnostic groups
The first part of Table 4 contains the comparison of the therapy outcome group (dropout, non-remission, partial-remission and full remission) between the three diagnostic conditions, and the second part of Table 4 the comparison for the number of attended sessions. Dropouts ranged between 36.8% and 50% among the groups. No statistical difference emerged comparing the three diagnostic subtypes. From those OSFED patients who completed treatment (n = 99; 56.6%), the 72.7% (n = 72) of the patients obtained good outcome (46.5% partial remission and 26.3% full remission) whereas the 27.3% of the completers presented non-remission.
Table 4 Comparison of therapy outcome.
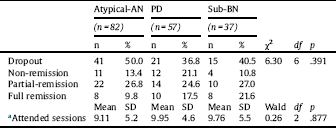
Note. AN: anorexia nervosa. PD: purging disorder. Sub-BN: subthreshold bulimia nervosa. SD: standard deviation.
a Results obtained in negative binomial model.
The Fig. 1 includes the cumulative survival functions (Kaplan-Meier estimation) for the time to the dropout of the study. As a whole, the highest risk of dropout and the highest rate was observed in the atypical-AN, nearly followed the other two diagnostic subtypes. Overall comparisons did not achieve statistical differences (p > 0.05 for the Log-Rank, Breslow and Tarone-Ware tests). The dropouts were constantly distributed along the whole therapy sessions.
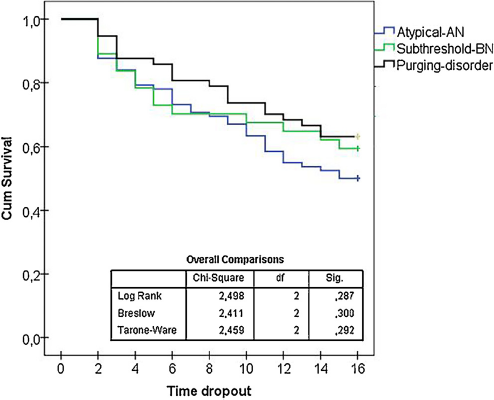
Fig. 1. Cumulative survival function for the time to dropout the therapy.
3.4 Predictive models of the therapy outcomes
Table 5 contains the final models with the variables with the best predictive capacity on the therapy outcomes dropout and partial-full remission. The list of potential predictors included EDI-2 total score, SCL-90R total score, personality profile measured through the TCI-R scales, chronological age, age at onset of the ED, duration of the disorder, BMI, motivational scales and frequency of binges-laxatives-vomits. The risk of dropout was increased differentially among the OSFED groups: (a) for atypical-AN by high frequency of binges-per-week, high scores in the novelty seeking trait, low levels in the self transcendence trait and low self-concern about the ED (Worry [Self]); (b) for PD by low scores in the personality traits of harm avoidance, reward dependence and self directedness; and (c) for sub-BN by high frequency of laxatives-per-week.
Table 5 Predictive models of the therapy outcomes dropout and remission: stepwise logistic regression.

Note. AN: anorexia nervosa; Sub-BN: sub threshold bulimia nervosa.
Note. List of predictors considered for the predictive models: EDI-2 total, SCL-90R GSI, personality profile measured with the TCI-R scales, chronological age, age of onset, duration of the disorder, BMI (maximum, minimum and current), motivational scales and frequencies of binges-laxatives-vomits.
HL: Hosmer-Lemeshow test (p-value). AUC: area under ROC curve.
Furthermore, the likelihood of partial-or-full remission was also increased differentially among the OSFED groups: (a) for atypical-AN by low scores in the novelty seeking personality trait and high perceived need of treatment; (b) for PD by high scores in the personality scales of harm avoidance, persistence and self directedness, and low Worry [Self]); and (c) for sub-BN by low frequency of laxatives-per-week, high levels in the self transcendence personality trait and low intensity perceived of the ED.
4. Discussion
The present study attempted to address an important gap in the literature, analyzing and comparing clinical and therapeutic features between different OSFED subtypes and, therefore, obtaining a better understanding of these ED. Moreover, since a good diagnostic categorization requires information regarding treatment outcome, the present study also aimed to analyze response to treatment, therapeutic adherence and predictors of therapy outcome among the different OSFED phenotypes.
The first main objective was to examine clinical differences between the most prevalent OSFED phenotypes. In agreement with other studies [Reference Ekeroth, Clinton, Norring and Birgegård24], our results showed that, overall, the three OSFED groups, besides of their symptomatological heterogeneity, share common eating and general psychopathological symptoms as well as personality traits [Reference Stice, Marti and Rohde17]. With regard to eating-related symptoms, the only meaningful difference was revealed in purging symptomatology, being the PD cases the ones who presented the highest frequency of vomiting and laxatives use. This result is not surprising since a recurrent purging behavior is the core symptom of this diagnostic subtype [Reference APA2]. Our results are also in line with previous studies which found that purging patients engaged in more frequent laxatives use as compensatory behavior [Reference Ekeroth, Clinton, Norring and Birgegård24, Reference Rockert, Kaplan and Olmsted40]. On the other hand, our results showed that the atypical-AN group showed the lowest scores in the EDI-2 bulimia subscale. These results were the expected ones because, unlike the other two diagnoses, atypical-AN patients do not required bulimic/purging behaviours for their diagnosis.
Patients with PD also presented a later age of onset, while sub-BN had significantly longer duration of the illness. These findings are similar to those reported in previous studies [Reference Smith, Crowther and Lavender23] indicating that PD is found to be rare before age 18 [Reference Stice, Marti, Shaw and Jaconis41], and most typically first onsets are at approximately 20 years of age [Reference Murray and Anderson7]. In this regards, previous studies have suggested that unhealthy weight control behaviors, such as purging behaviors, may appear as a mechanism to compensate the decline in physical activity and, therefore, energy balance dysregulation, which occurs in the late adolescence [Reference Stice, Marti and Rohde17]. On the other hand and not surprisingly, atypical-AN group presented lower BMI lifetime than the others. Although the diagnostic criteria for atypical-AN does not require meting the low weight of AN [Reference APA2], these patients present severe weight control strategies (restriction) which may justify these results.
Not surprisingly and consistent with prior literature [Reference Casanovas, Fernández-Aranda, Granero, Krug, Jimenez-Murcia and Bulik33], our results indicated that patients with OSFED report low motivation to change. When comparing the standardized scores of motivation for treatment between our OSFED patients and the full syndrome scores (based on the study of Casanovas et al. [Reference Casanovas, Fernández-Aranda, Granero, Krug, Jimenez-Murcia and Bulik33]), the former showed even lower scores (see supplemental files). In addition, no differences between the three groups were found, with the sole exception of a greater social impairment perceived by the sub-BN group. This result is consistent with previous research stating that binge eaters usually refer increased impairment in the social life and in the leisure activities because the binge-eating behaviors are associated with greater psychiatric comorbidity, distress and functional impairment [Reference Mond and Hay42–Reference Pawaskar, Witt, Supina, Herman and Wadden44].
Regarding treatment outcome, the rates of good remission in our sample ranged from 36.6% to 48.6% among the three phenotypes. These findings support other research which found an average percentage of remission of 40–45% [Reference Ekeroth, Clinton, Norring and Birgegård24]. However, they are not in accordance with others presenting recovery rates of 91% for sub-BN and 95% for PD [Reference Stice, Marti, Shaw and Jaconis41]. These discrepancies are probably due to the fact that the study of Stice et al. [Reference Stice, Marti, Shaw and Jaconis41] analyzed patients diagnosed with EDNOS according to DSM-IV and, therefore, more heterogeneous samples. Also, these authors analyzed adolescents from community samples and not adult ED patients who were seeking treatment, which may contribute to these contradictory results, since the latter probably present more chronic and severe eating pathology. In addition, no differences in remission rates were found between the three. In the same vein, a prior study found similar treatment outcome between the OSFED groups, but also between OSFED groups and ED full syndromes [Reference Ekeroth, Clinton, Norring and Birgegård24].
As regards dropout rates and therapeutic adherence, patients from the three OSFED diagnoses attended roughly the same number of therapy sessions and showed increased rates of dropout (36.8%–50%), which suggests that these patients are less motivated for treatment than full diagnoses of AN or BN, maybe because these patients generally exhibit less severe physical symptoms [Reference Thompson and Park45]. However, subthreshold diagnoses are not trivial and they should not be underestimated since they are disorders with severe comorbidity and similar chronicity to full syndromes [Reference Schmidt, Lee, Perkins, Eisler, Treasure and Beecham46]. Curiously, the survival analysis showed a constant and progressive evolution of the risk of dropout in all three groups. The lack of therapeutic adherence suggests that further research is needed to address the lack of motivation, beliefs about the disorder, perception about the control of the disease itself or awareness of disabilities derived from the disorder [Reference Baines and Wittkowski47]. In this sense, Lask and Framptom [Reference Lask and Frampton48] describe anosognosia associated with ED where the patient fluctuates from having insight into their disorder to moving to denial. This raises new premises about therapeutic targets. Future research should assess and compare key maintenance factors, such as denial of illness, lack of awareness, anosognosia or impaired insight [Reference Konstantakopoulos, Tchanturia, Surguladze and David49], as well as their association with therapy outcome. This will benefit clinicians to obtain a better conceptual understanding of the processes involved in the treatment of these patients. In this vein, it should be stated that motivational enhancement therapy interventions may be particularly important for those individuals diagnosed with OSFED [Reference Ackard, Cronemeyer, Richter and Egan50].
Finally, in terms of primary predictors of treatment outcome, our results were similar to those obtained in the literature on full ED syndromes, namely higher dropout and poorer therapy outcome associated to lower motivation and more dysfunctional personality traits. However, we found specific characteristics associated with the prognosis of each diagnostic subtype. First, for Atypical-AN, a higher novelty seeking and lower self-transcendence were associated with increased risk of dropout and less remission rates (although the three OSFED groups showed normative scores in novelty seeking [Reference Gutiérrez-Zotes, Bayón, Montserrat, Valero, Labad and Cloninger32]). Also for atypical-AN, a poor motivational stage with low concern for the disorder and lack of perceived need of treatment was related to worse prognosis. Second, for PD, lower scores on some personality traits such as harm avoidance, reward dependence, self-directedness and persistence were related to higher risk of dropout and poor outcome. Although the association between high harm avoidance and better prognosis in PD seems to be a striking and unexpected finding, it may suggest that patients with anticipatory worry, great sensitivity for criticism and fear of uncertainty [Reference Cloninger, Svrakic and Przybeck51] are more concerned about their disorder and, therefore, more motivated for treatment [Reference Fassino, Abbate Daga, Delsedime, Busso, Pierò and Rovera52]. Lastly, for the sub-BN group, high score on self-transcendence was the main predictor of therapy outcome. Unfortunately, we are not able to contrast our findings with previous studies, since no study has assessed the specific predictors of treatment outcome for the different diagnostic types of OSFED so far.
4.1 Limitations and strengths
The present study should be evaluated within the context of its several limitations. First, this study is limited by the lack of other diagnostic types of the wide spectrum of OSFED. It would have been useful to compare all OSFED but, unfortunately, we did not have enough sample size to make meaningful comparisons. Second, we included only adult female patients with ED. Hence, we cannot confirm whether our results are generalizable to adolescent or males with the same diagnosis. Third, not all the patients were naïve. That is, some patients were in a stage of the disorder with residual symptoms after a partial remission of the full-threshold disorders of AN or BN (diagnostic crossover). Hence, further studies assessing separately naïve and diagnostic crossover patients are needed for guaranteeing the homogeneity of the sample. Finally, our findings are mainly about symptomatological remission after the therapy, but not recovery (the term ‘recovery’ requires a long period of abstinence from ED symptomatology). Hence, further longitudinal studies collecting follow-up data are needed to replicate this study in order to assess whether there are differential rates of relapse or recovery.
Notwithstanding these limitations, the current study has also several strengths that should be noted. For the first time we have addressed treatment response across a large sample of adult females with different diagnostic types that fit into OSFED category. As far as we know, this is the first study assessing specific predictors of outcomes in these patients. A better description of the clinical features and treatment outcome of the distinct ED phenotypes, including subthreshold types, would most likely enhance its detection and diagnosis in clinical practice, mitigating diagnostic confusion [Reference Murray and Anderson7].
4.2 Conclusions
In sum, our findings revealed that the three OSFED subtypes were more similar than distinct in terms of clinical, psychopathological and personality features. Regarding treatment outcome, our findings suggest that OSFED patients, who complete the therapy, may benefit from the same treatment. However, the high dropout rates open the debate and highlight the need to add other therapeutic tools for improving the therapeutic adherence of these patients, for example, family, motivational or insight-based treatments.
Funding sources
This work was supported by the Instituto de Salud Carlos III (ISCIII) [grant numbers PI14/00290 and PI17/01167] and co-funded by European Regional Development Fund (ERDF) "a way to Build Europe", and by grants of the Ministerio de Economía y Competitividad [grant number PSI2015-68701-R] and the Generalitat de Catalunya [grant number PERIS SLT006/17/00077]. Centro de Investigación Biomédica en Red Fisiopatología de la Obesidad y Nutrición (CIBERobn) and Centro de Investigación Biomédica en Red Salud Mental (CIBERSAM) are both initiatives of ISCIII.
Declaration of interest
Authors have no conflict of interest to declare.
Acknowledgements
We thank Núria Mallorquí-Bagué for assistance with revising the English, and for her comments that greatly improved the manuscript.
Appendix A Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.eurpsy.2018.08.001.









Comments
No Comments have been published for this article.