1. Introduction
The recent Mental Health Action Plan 2013–2020, promoted by the 66th World Health Assembly [1], included among its main objectives the provision of comprehensive, integrated mental health and social care services in community-based settings, the implementation of strategies for promotion and prevention; and strengthened information systems, evidence and research. Mental health care comprises the main care domains provided to citizens with mental illness and/or substance use disorders (ambulatory, home, residential and semi-residential care) and accounts for 5% of total health care expenditure in Italy, remaining a neglected area of health policy compared to other countries [2]. The recognition of the complexity, multifactorial nature of mental illness has led to redefining the essential levels of care [3] for mental health and pathological substance dependence in Italy, with a focus on the assessment of health and social care needs, accessibility, continuity of care and personalized care pathways. To address this new challenge, in the last few years the ‘health budget’ has been introduced in some Italian regions as a new tool to manage the complex problems of patients with mental illness, in which the local and health care institutions, together with other resources (voluntary associations, cooperation, family) and the person himself, share pathways built on subject's needs. For each patient a personalized health budget is defined that brings together the economic, social, personal and context resources [4, Reference Starace5]. Still, the implementation of personalized care pathways tailored to patients’ needs would require a careful assessment of feasibility and sustainability of interventions over time. Moreover, no fine-grained data on activity-based budgeting of mental health services are available to support decision-making because estimates of mental health care costs are based on average costs obtained as the ratio between the overall costs of hospital and community care and the resident population [6].
Amaddeo et al. [Reference Amaddeo, Grigoletti and Montagni7] reviewed the few existing studies conducted on the analysis of the costs of the Italian mental health provision of care and described the current financing system for mental health care in Italy.
These costs are largely borne by the national health system through the Local Health Authorities (LHAs), by patients’ families and by a part of the municipality budget devoted to social care. LHA costs can broadly be divided into: costs sustained within the accounting year by the Mental Health and Pathological Dependence Department (MH-PDD) as part of the per-capita quota allocated to the Department and those generated by patients’ admissions to other departments and services (ambulatory consultations, drugs, emergency, hospitalization, day-hospital and long-term rehabilitation among public and private facilities, homecare).
The MH-PDD administers approximately 5% of the 1.940,61 € per-capita average regional expenditure in 2011–2012 [Reference Mapelli, De Stefano, Compagnoni, Gambino and Ceccarelli8] and its financing is granted to each LHA according to historical expenditure as a quota of the per-capita transfer made by the Region to the LHAs.
The current accounting schemes leave little room for measurement and provides no useful insight on individual care needs. MH-PDD costs are merely benchmarked yearly as the proportion of MH-PDD costs on the overall per-capita quota: an average € 82.4 for MH and an average of € 16.68 for PDD per-capita in 2011. Moreover, MH information systems and the LHA accounting systems are not yet integrated, hindering research on individual and organizational sources of variability [Reference Rampazzo9–Reference Fattore, Percudani, Pugnoli, Contini and Beecham11].
In the attempt to fill this knowledge gap, and given the lack of information on individual costs of mental illness, we set up a costing methodology to estimate the costs of 45 types of services provided by the MH-PDD. A simple bottom-up procedure was used, based on the principle of full absorption costs, that includes fixed and variable costs. The cost items included in the procedure were the workforce costs, the indirect costs associated with clinical activity and the general administration overheads allocated to MH-PDD at 2013 prices. After linking the mental health information system and the current accounting system of a Local Health Authority in Italy, we applied this methodology to estimate the overall annual MH costs borne by the LHA.
Converging evidence indicates that a small proportion of mental health care users account for a large share of health care costs [Reference de Oliveira, Cheng, Vigod, Rehm and Kurdyak12–Reference de Oliveira, Cheng, Rehm and Kurdyak14].
Our aims are therefore to compare the characteristics of patients in the top decile of costs with those of the remaining 90%, and to analyse the demographic and clinical determinants of costs.
2. Methods
2.1 Overview and data source
The study population consists of adult patients who had at least one contact with the mental health services of the Local Health Authority of Reggio Emilia (Italy, 535869 inhabitants at 01.01.2013) in 2013.
Data on patient characteristics and on the MH-PDD services they received in 2013 were extracted from mental health information system database (SISM) database. SISM includes information on socio-demographic characteristic, on ICD-9 CM diagnoses and on the number and type of services delivered. ICD-9 CM diagnoses are recorded at the first/second visit by the psychiatrists/psychologists when a specific treatment plan is defined, targeted to the patient’s needs and are updated over time if they change or when additional symptoms emerge. The algorithm for the classification into diagnostic groups is provided as Supplementary material.
Data are entered in the SISM on a regular basis by the mental health services operators and delivered to the Regional Health Authority for quality check twice a year. Inconsistencies are resolved and the Region, in turn, sends the data to the Ministry of Health for reporting. The SISM glossary (2013) defines 45 types of community services (Table 1), from the fulfillment of legal and organizational requirements (e.g. writing and exposing a report for the justice), not involving any contact with the patient, to group activities. The 45 services were classified into 7 clinical-therapeutic pathways that included initial (re)assessment, psychotherapy, psychiatric-clinical encounter, vocational training, socio-rehabilitation, day center (DC) and community day-hospital (CDH).
Table 1 Mental health unit services: skill-mix, venue and average length of service weights.

Specifically, socio-rehabilitation consists of individual or group daytime activities, tailored to the needs of care or rehabilitation of patients with a high degree of disability/chronicity. Socio-rehabilitation activities are aimed at providing patients social and/or economic support, or helping them (re) acquire daily activity skills and interpersonal functioning. They are carried out outside day centers or day hospital.
Day center activities are daytime group rehabilitative therapeutic activities for patients with severe mental illness.
Community day hospital interventions include drip, and parenteral or oral drug administration to patients in an acute illness phase, as an alternative to hospitalization. They are carried out in non-hospital facilities.
2.2 Cost calculation
The costing methodology used in the present study was based on a microcosting (bottom-up) approach to establish the costs of services at individual level.
The LHA accounting system was used to determine costs that are directly driven by service user care (clinical care staff time and the administered drugs) and those that are more loosely tied to service user activity (indirect costs and overheads).
Cost of labor estimates for each activity provided were possible because the MH-PDD database reports reliable information on the number and qualification of health professionals involved in each service and, to some extent, information regarding the duration and the location of the activity. The beginning and the end of each activity was estimated in a sub-sample of 19,634 records obtained by excluding services with zero or over 3 h duration. The average length in minutes for each MH-PDD activity was calculated and then validated by two experienced senior psychiatrists and a ‘displacement’ multiplication factor was assigned to services provided outside the typical setting (e.g. prison, patient home and acute service consultations by MH-PDD staff).
Gross hourly costs were attached to each service provided by the MH-PDD in 2013 up to a maximum of 4 health professionals involved in each activity, then multiplied by the duration of the service. The duration in minutes was set to the validated standard time (Table 1) when provided in the main location, otherwise a weight varying between 1.25–1.50 was applied if provided in other locations requiring personnel displacement. Group activities were assigned a 0.36 weight, assuming that on average 2.8 users took part in each group activity.
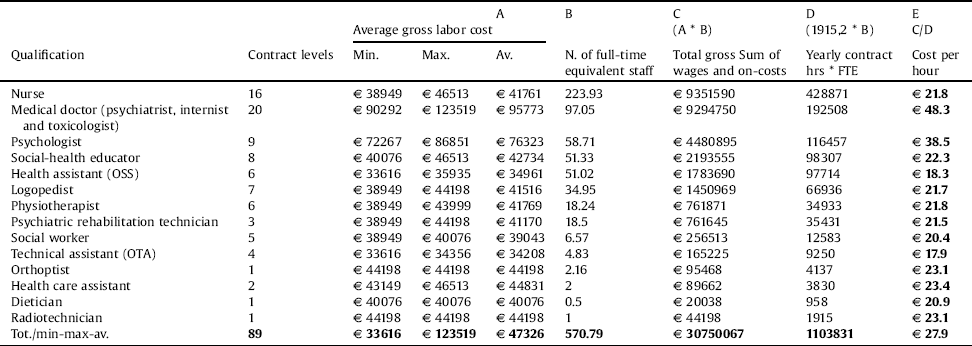
Because services are mainly relational and labor-intensive, only staff costs were considered as direct costs and were derived from actual labor costs in the LHA (Table 2).
Table 2 Gross hourly average labor cost by main qualification of health workers in the selected LHA, year 2013.
Indirect costs and overheads were taken from the LHA accounting system by selecting only those items referring to support clinical activities and MH-PDD general management. Among direct health care goods, pharmaceuticals and charges paid for buying health and rehabilitation services outside the MH-PDD were not included. Pathway costs were calculated as the sum of unit costs of services provided within each specific care pathway.
2.3 Statistical analysis
Patients’ characteristics were summarized and compared between 2 groups of patients: high-cost (HC), defined as those in the top decile of the cost distribution and non-high-cost (non-HC), including patients in 1st to 9th deciles of cost distribution.
Comparisons between groups were performed using Mann-Whitney test or t-test for continuous variables when appropriate (age, years in contact with MH services) and χ2-test for categorical variables.
Multiple linear regression models were used to identify the demographic and clinical predictors of community mental health care costs. The natural log of costs was taken as the dependent variable in the models to normalize the cost distribution, that was skewed to the right. Potential predictors were selected based on their known potential association with the outcome, consistent with Jones et al. [Reference Jones, Amaddeo, Barbui and Tansella15] and with a previous study of our group underscoring disparities in the use of mental health services between Italians and immigrants [Reference Rucci, Piazza, Perrone, Tarricone, Maisto and Donegani16]. They included gender, age, citizenship (Italian coded as 0 and non-Italian coded as 1), education, living arrangement and occupation and number of years since first contact with mental health services and diagnosis. Specifically, eight dummy variables were used to denote the presence or absence of eight primary or secondary diagnoses: psychosis, bipolar disorder, depression, anxiety, personality disorder, substance use disorder, dementia and other diseases. Three relevant socio-demographic variables (education, living arrangement and occupation) were not included in the models because the percentage of missing data was high (respectively 25.0%, 24.9% and 56.1%). All analyses were performed using IBM SPSS, version 23.
3. Results
3.1 Study population
Of the 8699 patients retrieved from the SISM database, 53 were excluded because their diagnosis had not been established yet, and 1045 were further excluded because their diagnosis was recorded using V-codes, that specify an encounter for administrative purposes or a general psychiatric examination. Therefore, the final analyzed population consisted of 7601 patients (Table 3), predominantly female, with a mean age of 51 years and a long-standing relationship with mental health services. The most frequent diagnoses were depression (30.7%), psychosis (22.3%) and personality disorders (15.8%).
Table 3 Patient characteristics (N = 7601).

3.2 Costs
The overall costs of the 274639 MH-PDD services provided in 2013 amounted to more than 17 million €. Estimated unit costs varied from a minimum of € 2.86 to a maximum of € 735.53, which respectively corresponded to a health-allied professional performing a 5 min task, and to an informal access to a day care facility which lasted more than 4 h and involved up to 4 health professionals (Table 4). Some unit costs had higher variance when infrequent and when performed by very different skill-mixes.
Table 4 MH services unit costs in 2013: key descriptive statistics.
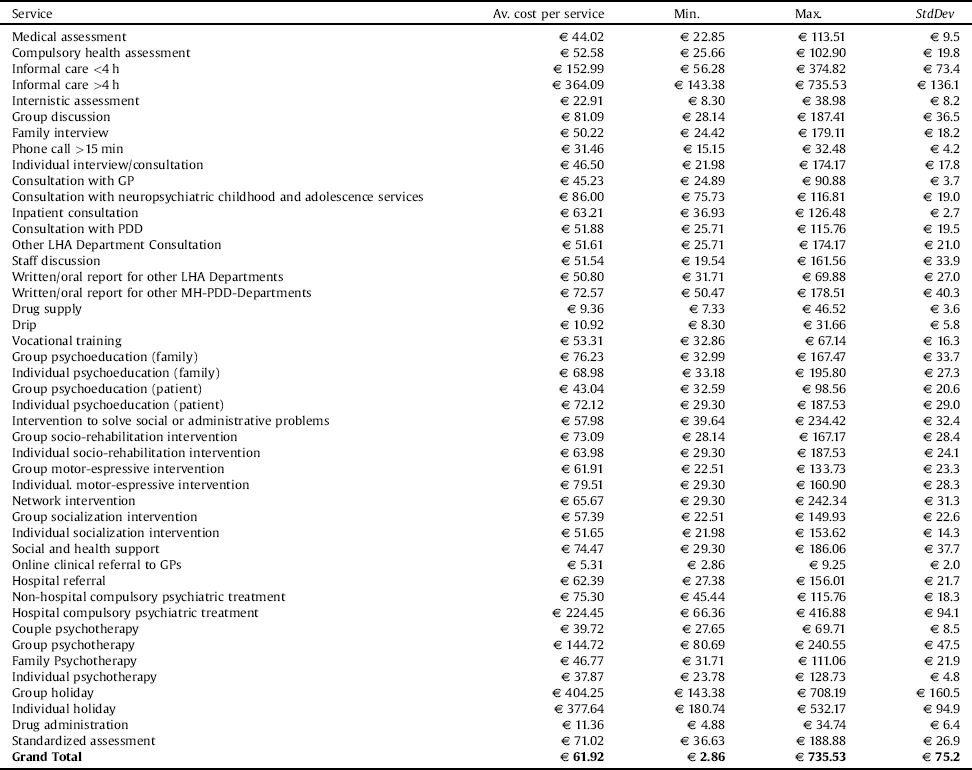
Pathway costs are displayed in Table 5. The cost methodologies defined for MH services imply that treatment costs increase with the duration and the number of operators involved. THCs socio-rehabilitation, day center and community day hospital care were by far the most expensive interventions, although they were provided to a minority of patients.
Table 5 Frequency of MH ‘pathways’ and costs per beneficiary in 2013.

For instance, day center activities accounted for more than 52% of total costs but involved less than 4% of patients. Psychotherapy costed annually a median of € 227 and was among the cheapest interventions together with vocational training (€ 187) and initial assessment (€ 98).
Fig. 1 shows that the HC (N = 764) accounted for 87% of costs and 73% of services, while the remaining 90% of patients accounted for only 13% of costs. The reason for such huge disparity is that the great bulk of costs incurred for HC included day-center, community day hospital and socio-rehabilitation services, that were extremely uncommon in non-HC (Fig. 2).
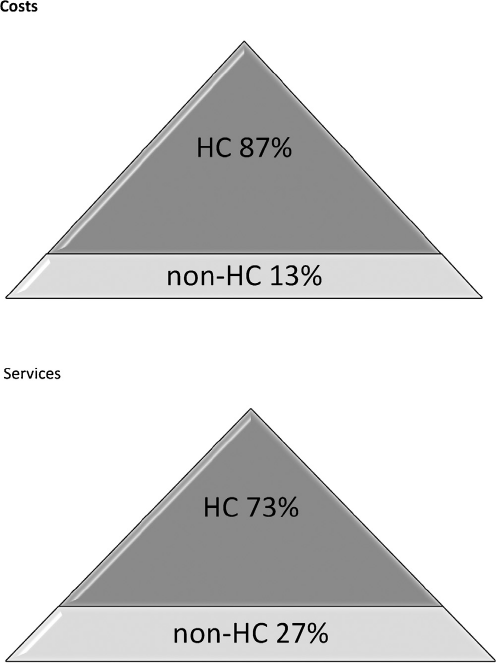
Fig. 1. Diagram showing the distribution of annual costs and services among patients treated at the MH-PDD in 2013.
High cost (HC): annual costs >€ 1520; non-high costs (non-HU): annual costs≤ € 1520. HC accounted for 87% of costs and 73% of services.

Fig. 2. Stacked bar chart showing the percentage distribution of cost by pathway in the top 10% (HC) and in the rest of the sample (non-HC).
High cost (HC): > € 1520; non-HC:≤ € 1520.
Comparison of HC patients with non-HC revealed that HC included a significantly higher proportion of males with psychosis, with a lower median age (46 years), a median of 12.5 years in contact with MHS and a median of 106 services in the index year (Table 4). Vice versa, non-HC (N = 6837) comprised predominantly women with a median age of 51 years, with common mental disorders (depression, anxiety or adjustment disorder), who had been in contact with MHS for 4.6 years and received a median of 7 services; 26.1% of them were incident cases.
The median cost of HC patients was about 22-fold higher compared to that of non-HC patients (€ 4238 vs. € 190).
Median annual costs were highest for psychosis (€ 562), although with a large variability (range € 8.3-391652), and were € 439 for bipolar disorder (range € 8.3 -137239), € 214 for personality disorder (range € 8.3-209607), € 182 for depression (range € 5-90162).
3.3 Predictors of costs
We regressed costs on age and gender and then entered, with a stepwise procedure citizenship, the 8 diagnoses and the duration of contact with MHS (in years). This model accounted for 20.7% of cost variance. The statistically significant predictors of costs, arranged in decreasing order of weight (standardized beta coefficient), were psychosis, a longer relationship with mental health services, younger age, personality disorder, bipolar disorder, depression, dementia and Italian citizenship (Table 6).
Table 6 Linear regression estimates of (log) costs by MH users characteristics (N = 7061). The adjusted R2 for the model is 0.207.

4. Discussion
In this study we developed a cost methodology that combines direct and indirect costs of community mental healthcare, and applied it to a cohort of patients treated in 2013 by the MH-PDD of an Italian local health authority to estimate the cost of services and care pathways. Day center was by far the more expensive pathway, accounting for 52.4% of the total annual costs, although it was used by a minority of patients.
Notably, our findings indicated that mental healthcare costs are concentrated among a small fraction of patients (10% of patients generating 87% of costs), suffering from severe mental illness, relatively younger than the rest of the patients and with an established relationship with mental health services. This suggests that most expensive interventions are targeted to complex and younger patients, in the attempt to counteract the burden of illness for patients and their families. In particular, high-cost patients were those who benefitted from care pathways including rehabilitation services delivered in day centers or community day hospitals.
Our results are consistent with evidence from a study conducted in the catchment area of Madrid [Reference Armesto, Medeiros and Wei17], in which 19.4% of patients generated 80% of costs and with the results of a US study of patients with depression [Reference Robinson, Grabner, Palli, Faries and Stephenson13], in which mean annual costs of high utilizers (top 10% of costs) were eightfold higher than those of non-high utilizers.
In addition, our finding that a minority of patients account for a disproportionately high share of health care cost is in line with a Canadian study showing that, among high-cost patients, those with a substantial use of mental health services incur in 30% higher costs [Reference de Oliveira, Cheng, Vigod, Rehm and Kurdyak12].
Results from multiple linear regression indicate that severe mental illness (encompassing the diagnoses of psychosis, bipolar disorder, and personality disorder), younger age, a longer relationship with mental health services, and dementia predicted higher annual costs. These findings are consistent with Jones et al. review [Reference Jones, Amaddeo, Barbui and Tansella15] and underscore the importance of previous psychiatric service utilization as a proxy of chronicity, that proved to be the most significant predictor of costs in Donisi et al. [Reference Donisi, Jones, Pertile, Salazzari, Grigoletti and Tansella18].
Our finding concerning the economic burden of patients with psychosis, compared with patients with other conditions, has been well documented in the literature and raises concerns worldwide. In a US study it has been estimated at $155.7 billion for the year 2013, including excess direct health care costs of $37.7 billion (24%), direct non–health care costs of $9.3 billion (6%), and indirect costs of $117.3 billion (76%) compared to individuals without schizophrenia. The largest components were excess costs associated with unemployment (38%), productivity loss due to caregiving (34%), and direct health care costs (24%) [Reference Baca-Garcia, Perez-Rodriguez, Basurte-Villamor, Quintero-Gutierrez, Sevilla-Vicente and Martinez-Vigo19]. De Oliveira et al. [Reference de Oliveira, Cheng, Rehm and Kurdyak14] underscored that expenditures for patients with chronic psychosis represent a sizeable portion of the Ontario health care budget (3%). A recent review of 19 studies on the societal cost of schizophrenia [Reference Cloutier, Aigbogun, Guerin, Nitulescu, Ramanakumar and Kamat20] reported that the annual healthcare costs vary from $US 1445 in Thailand to $US 60630 in Norway.
This study has a number of strengths. First, it is based on the large and heterogeneous real-world population attending the community mental health services of Local Health Authority and has no selection bias. Second, cost estimates are accurate because they rely on information recorded in the SISM database about the professional mix involved in the different activities and (when appropriate) the time spent on traveling to the service location. Another strength of our study lies in the novel bottom-up methodology focused on individual costs and based on the staff and MH-PDD resources actually involved in patients’ care. In this way, the annual cost per patient, per care pathway and per diagnostic cluster were obtained.
However, our findings should be interpreted in light of important limitations. First, the retrospective study design prevented from having complete data on diagnoses and on some demographic characteristics such as education, working status and living arrangement that may be important determinants of service use and costs. Second, because hospital, residential and drug costs were not included in the estimation, we underestimated overall mental health costs and the costs of patients mainly treated in sub-contracted facilities.
Despite these limitations, the methodology employed exploits routinely collected economic and activity data and offers a replicable cost breakdown procedure to be used in other regional local health authorities for a comprehensive estimate of resource utilization across community health services, provided that information systems collecting data at the same detail are available. To facilitate benchmarking, effective 2012, the Italian Ministry of Health has adopted a unique record layout for the mental health information system. All the regions have the obligation to send their data twice a year using a specific format, to allow the generation of reports and quality of care indicators. Moreover, because the magnitude of mental health cost estimates differs considerably across countries, due to different economic conditions, healthcare systems and widespread methodological heterogeneity among COI studies [Reference Jin and Mosweu21], our results can be useful for cross-national comparisons.
In conclusion, on a policy level, the large heterogeneity and the strong asymmetry in the distribution of individual costs of mental health care argues against the use of ‘average’ costs to summarize mental health care expenditure, in favor of an analytic breakdown based on individual care pathways. The adoption of a standardized microcosting methodology could also introduce MH-PDD healthcare professionals to clinical governance issues and support them in the definition of personalized health care plans that encompass all services and activities that jointly determine the success in meeting patient’s needs. This paves the way for measuring ‘value’ in term of patient outcomes for each euro spent [Reference Porter22, Reference Nuti, Vola, Bonini and Vainieri23]. From the clinical point of view, our results concerning the predictors of higher costs underscore the need of to undertake a systematic collection of symptomatic and functional outcomes of the multifaceted interventions provided by community mental health services to ensure that interventions meet patients’ needs and are cost-effective and sustainable.
Acknowledgment
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Appendix A Supplementary data
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.eurpsy.2018.02.001.











Comments
No Comments have been published for this article.