No CrossRef data available.
Published online by Cambridge University Press: 19 July 2023
The evaluation of healthcare pathways must be considered of fundamental importance. The quality of care provided to patients with severe mental disorders (SMD) does not correspond to the standards set by the recommendations. Therefore, measures such as the real coverage rate of psychiatric patients’ needs (contact coverage), by comparing epidemiological prevalence rates and the number of patients receiving adequate care, could be a valuable resource for implementing the transition to community mental health. However, simple assessment and reporting of rates of contact with mental healthcare potentially overestimate the full expected health benefits of services. Therefore, in addition to monitor the coverage rate achieved by the services, the evaluation of the effectiveness of the care provided (effective coverage) [De Silva et al. Int J Epidemiol 2014;43(2):341–53] is also of relevant importance.
To measure the gap between contact and effective coverage of mental healthcare, i.e., the effectiveness of interventions provided by services for the treatment of SMD in preventing an exacerbation of psychiatric symptoms.
Data were retrieved from Healthcare Utilization databases of four Italian Regions (Lombardy, Emilia-Romagna, Lazio, Sicily). 45,761 newly taken-in-care cases of depression, schizophrenia, bipolar, and personality disorder were included. A variant of the self-controlled case series method was used to estimate the incidence rate ratio (IRR) for the relationship between exposure (use of different types of mental healthcare such as pharmacotherapy, generic contacts with the outpatient service, psychosocial interventions, and psychotherapies) and relapse episodes (mental illness emergency hospital admissions).
11,500 relapses occurred. Relapse risk was reduced (Figure) during periods covered by (i) psychotherapy for patients with depression (IRR 0.67; 95% CI, 0.49 to 0.91) and bipolar disorder (0.64; 0.29 to 0.99); (ii) psychosocial interventions for those with depression (0.74; 0.56 to 0.98), schizophrenia (0.83; 0.68 to 0.99) and bipolar disorder (0.55; 0.36 to 0.84), (iii) pharmacotherapy for those with schizophrenia (0.58; 0.49 to 0.69), and bipolar disorder (0.59; 0.44 to 0.78). Coverage with generic mental healthcare, in the absence of psychosocial/psychotherapeutic interventions, did not affect the risk of relapse.
Image:
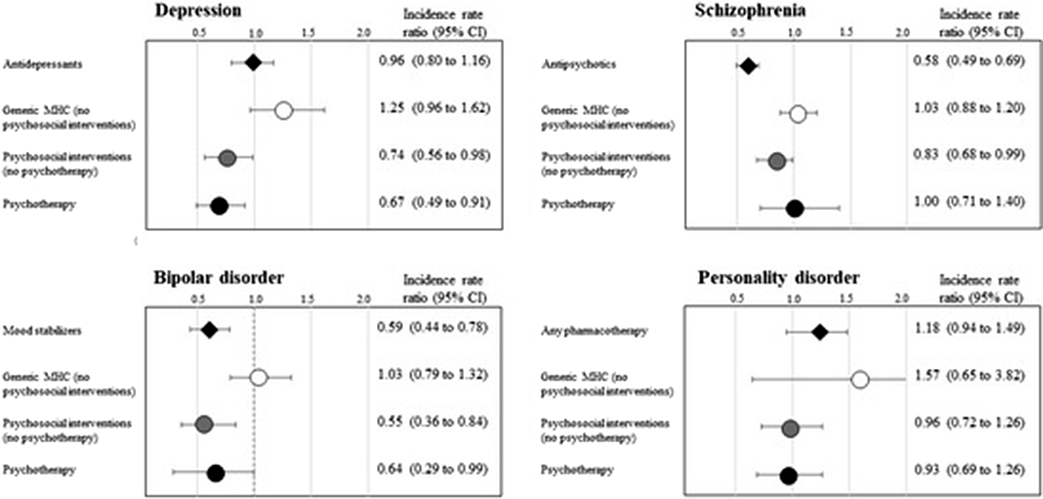
Psychosocial interventions, psychotherapies and specific pharmacotherapies can be considered particularly effective in treating patients with bipolar, depressive, and schizophrenic disorders. This study ascertained the gap between utilization of mental healthcare and effective coverage, showing that real-world data can represent a useful resource to monitor mental healthcare paths and to assess the effectiveness of a mental health system.
None Declared
Comments
No Comments have been published for this article.