Introduction
Schizophrenia is a serious psychiatric illness that affects approximately 1% of the population worldwide [Reference McGrath, Saha, Chant and Welham1,Reference Owen, Sawa and Mortensen2]. It involves emotional, cognitive, and behavioral symptoms [3] that are often difficult to treat [Reference Jääskeläinen, Juola, Hirvonen, McGrath, Saha and Isohanni4]. The annual economic burden of schizophrenia is estimated to vary between US$94 million and US$102 billion annually, with indirect costs responsible for between 50% and 85% of total expenses [Reference Chong, Teoh, Wu, Kotirum, Chiou and Chaiyakunapruk5].
Patients with severe mental illness, including schizophrenia, may be legally mandated to receive treatment. In the early 20th century most admissions to psychiatric institutions were involuntary, due to stigma, overcrowding and understaffing at the facilities. In industrialized societies, involuntary hospitalization legislation has since undergone various modifications [Reference Frankenburg6,Reference Saya, Brugnoli, Piazzi, Liberato, Di Ciaccia and Niolu7]. There has been an overall movement toward deinstitutionalization [Reference Perry8].
Despite attempts to standardize legally mandated treatment, rules, and regulations vary regionally and globally [Reference Saya, Brugnoli, Piazzi, Liberato, Di Ciaccia and Niolu7,Reference Zhang, Mellsop, Brink and Wang9]. For example, within Canada, there exists 12 Mental Health Acts, which equates to almost one separate act per province and territory [Reference Gray and O’Reilly10]. Overall, the criteria for involuntary detention in most countries requires that (a) a patient be suffering from a severe mental disorder and (b) compulsory treatment is required to protect the patient or others [Reference Zhang, Mellsop, Brink and Wang9].
Rates of legally mandated admissions for psychiatric patients are increasing [Reference Salize and Dressing11]. Among this population, patients with schizophrenia are more likely to be involuntarily admitted than patients with other disorders [Reference Curley, Agada, Emechebe, Anamdi, Ng and Duffy12–14]. Across the European Union, up to 50% of legally mandated admissions are for schizophrenia and related psychiatric disorders [Reference Salize and Dressing11,Reference Dressing and Salize15,Reference Preti, Rucci, Santone, Picardi, Miglio and Bracco16]. Rates of involuntary admission for mental disorders across the European Union vary from 6 per 100,000 people in France to 218 per 100,000 people in Finland [Reference Dressing and Salize15]. Heterogeneity in the rates of involuntary admission globally can be partially explained by different legal frameworks, individual-, system-, and area- related characteristics [Reference Curley, Agada, Emechebe, Anamdi, Ng and Duffy12].
Data regarding the effectiveness of legally mandated treatment is mixed. When compared to voluntary patients, involuntary patients tend to fare better with certain outcomes, and worse with others [Reference Kennedy17–19]. A systematic review compared outcomes for acute adult psychiatric patients who were admitted involuntarily and voluntarily. Length of stay, risk of readmission and involuntary readmission were at least equal or greater for involuntary individuals. Involuntary patients had higher suicide rates, lower levels of social functioning, and equal levels of general psychopathology and treatment compliance [Reference Kallert, Glöckner and Schützwohl20].
The literature regarding patients’ attitudes toward their legally mandated psychiatric treatment is limited. One review evaluated patients with psychiatric illness and their positive and negative experiences with involuntary treatment [Reference Katsakou and Priebe21]. Areas of importance included patients’ perceived autonomy and participation in decision-making, feelings of being cared for, and their sense of identity [Reference Katsakou and Priebe21]. Unlike the previous publication [Reference Katsakou and Priebe21], our review includes a larger number of studies and emphasizes the experiences of patients with schizophrenia. Through this systematic review of qualitative studies, we aim to primarily describe the experiences of patients with schizophrenia and related disorders who were legally mandated to undergo psychiatric treatment. By understanding perspectives, healthcare providers can identify methods to strengthen patient–provider relationships [Reference Drossman and Ruddy22] and improve compassionate care [Reference Post23], which may enhance treatment adherence, satisfaction and well-being [Reference Post23]. Thus, improving patient experience could lead to better clinical outcomes [Reference Priebe, Barnicot, McCabe, Kiejna, Nawka and Raboch24,Reference Doyle, Lennox and Bell25].
Methods
Search strategy
Four electronic bibliographic databases were searched: CINAHL Plus (1981 to May 9, 2019), EMBASE (1947 to May 9, 2019), MEDLINE (1946 to May 9, 2019), and PsycINFO (1806 to May 9, 2019). The databases were searched for key words, text words and medical subject headings (MeSH) related to schizophrenia, legally mandated treatment, and patient experience. Duplicate records were removed. All titles and abstracts identified by the literature search were independently reviewed for study inclusion by two authors (J.E.P., S.M.). Any disagreements were resolved through discussions with a third author (D.M.B.). If the inclusion criteria were unclear from the abstract, the full text was retrieved for further assessment. References within each of the included studies were also searched to identify additional relevant publications. The reference lists of relevant reviews identified using search terms “compulsory treatment,” “mandated treatment” and “involuntary treatment” in the Cochrane Database of Systematic Reviews were searched. Email correspondence with authors was completed to obtain additional study info.
Inclusion and exclusion criteria
Studies where at least 50% of patients had a diagnosis of schizophrenia or schizoaffective disorder were included. Qualitative studies that reported on the experiences of patients under any form of legally mandated treatment were included. Different forms of legally mandated treatment included involuntary treatment, community treatment orders, community care orders, and forensic patients. Mixed-methods studies were included if qualitative findings were presented separately. Searches were limited to publications in the English language. Case-studies, commentaries, reviews, first-person accounts, and abstracts were excluded.
Data synthesis and analysis
A thematic analysis [Reference Dixon-Woods, Bonas, Booth, Jones, Miller and Sutton26,Reference Lucas, Baird, Arai, Law and Roberts27] was completed to synthesize data from each of the included studies. Thematic analysis was selected because it is a flexible approach which can provide a detailed account of data. It is also recommended when researchers want to gain insight into patients’ experiences [Reference Nowell, Norris, White and Moules28].
We selected the two broad themes of positive and negative patient experiences a priori. These included any positive and negative aspects of treatment that patients may have experienced while under any form of legally mandated treatment. We chose to proceed with positive and negative patient experiences to be consistent with a previous review of qualitative studies [Reference Katsakou and Priebe21] that identified these overlying themes from the patients’ perspective in their data.
Two authors (J.E.P. and S.M.) independently read all the included studies and extracted themes from the results sections. Where applicable, each sentence from the results section was coded as referring to a positive or negative patient experience.
Next, we went through the lines of coded text to identify subthemes. After discussing within the research team, we came to an agreement on subthemes to be used. The four most commonly identified subthemes were included in this review.
The first reviewer (J.E.P.) has experience completing systematic reviews. Her interpretations are driven by academic interests, rather than clinical experience. The second reviewer (S.M.) has experience working and assessing symptoms in patients with severe mental illness. D.M.B. is a psychiatrist with extensive experience treating patients with schizophrenia and other forms of severe mental illness. People with a lived experience of schizophrenia spectrum illness were not involved in developing or validating the thematic analysis.
Study quality assessment
The critical appraisal skills program (CASP) was used to assess the quality of each of the publications that met the inclusion criteria [Reference Programme29]. The CASP tool contains 10 questions regarding the clarity, methods, and results of the studies. Studies were accordingly ranked as low (0–3 points), medium (4–7 points), and high quality (8–10 points). Study quality was independently assessed by two authors (J.E.P. and S.M.). Any disagreements were resolved through discussions with a third author (D.M.B.).
Results
Search results
The search completed on May 9, 2019 yielded a total of 4,008 abstracts through electronic searches of MEDLINE (n = 586), EMBASE (n = 957), CINAHL Plus (n = 2102), and PsycINFO (n = 363). Searching the reference lists of included studies yielded an additional five citations. A total of 648 duplicate references were removed, and an additional 3,288 references were excluded through the review of titles and abstracts. After assessing 72 full-text articles for study eligibility, an additional 59 references were excluded for failing to meet the inclusion criteria. A total of 18 articles are included in this systematic review of qualitative studies. For detailed search results, see study flow diagram (Figure 1).

Figure 1. Study flow diagram.
Characteristics of included studies
A total of 18 publications with 401 patients were included in this systematic review of qualitative studies [Reference Adams and Hafner30–47]. Each study had a clearly stated goal or objective and explored slightly different aspects of patients’ experiences with various forms of legally mandated treatment. Studies were completed in England (n = 5), New Zealand (n = 3), Australia (n = 2), Sweden (n = 2), Austria (n = 1), Canada (n = 1), Ireland (n = 1), Japan (n = 1), Norway (n = 1), and Scotland (n = 1). Some of the methodological approaches included thematic analysis, grounded theory, and interpretative phenomenological analysis. All of the included studies, with the exception of one [Reference Adams and Hafner30] were rated as high quality. Detailed study characteristics can be found in Table 1.
Table 1. Detailed study characteristics.

Thematic analysis of results
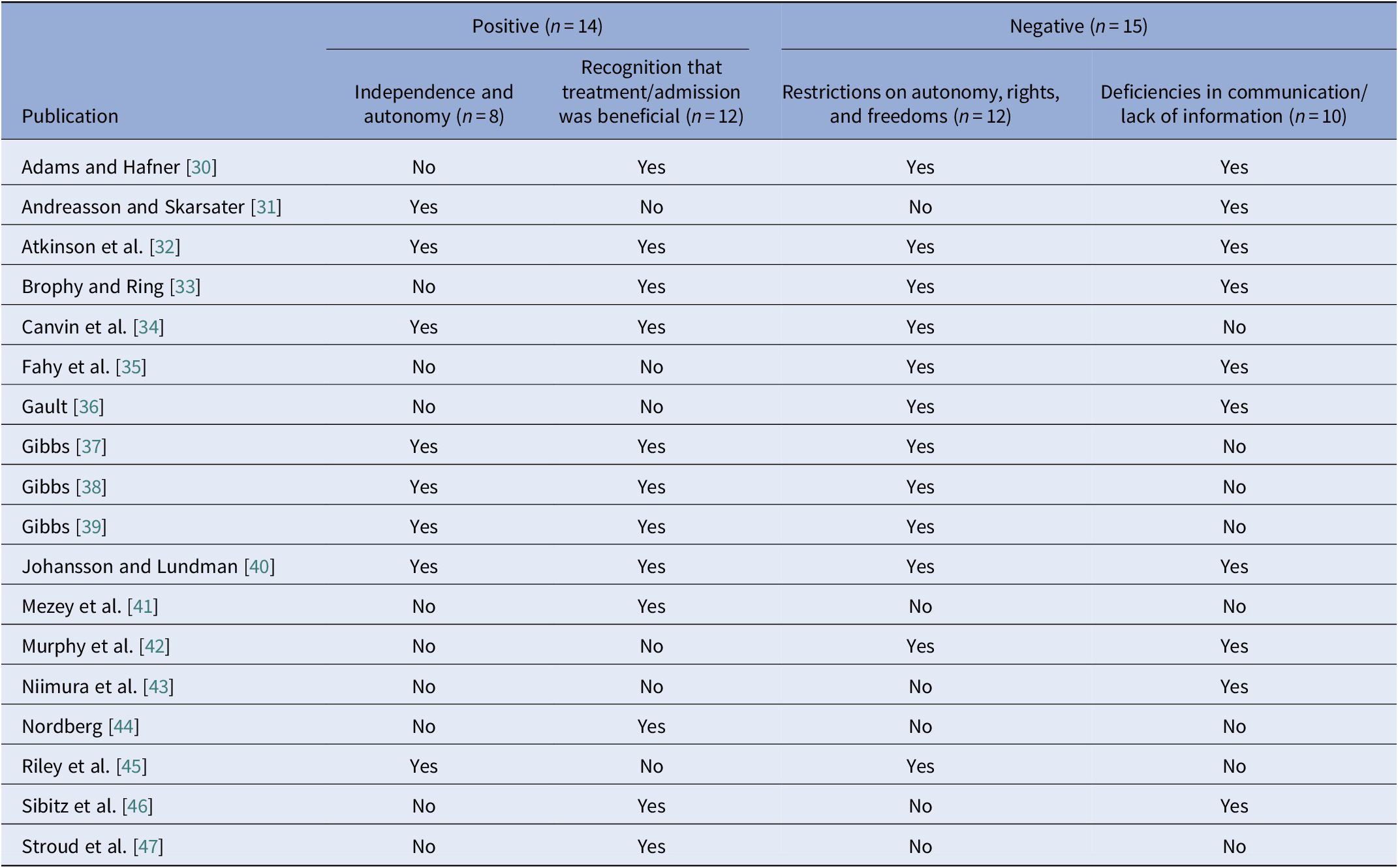
In this synthesis, published results from each of the included studies were coded as reporting either positive or negative experiences. Four additional subthemes were identified and classified under the two main themes of positive and negative patient experiences. Further study details can be found in Tables 1 and 2.
Table 2. Positive and negative patient experiences.
Positive patient experiences (n = 14)
Independence and autonomy (n = 8)
Despite being under compulsory treatment, patients valued independence [Reference Andreasson and Skarsater31]. One patient said; “He [the psychiatrist] tells me where I can live and where I cannot live, he is the one that is in charge of me [but] not in charge of my whole life. I still go to the pubs; he cannot stop me from going to the pubs to see my mates” [Reference Gibbs, Dawson and Mullen39]. Some patients reported that being on a community treatment order (CTO) allowed them to gradually gain more independence before being discharged [Reference Gibbs, Dawson, Ansley and Mullen38]. Patients enjoyed taking responsibility for their own care [Reference Johansson and Lundman40], and realized that they can obtain “freedom” if they follow the doctor’s orders [Reference Stroud, Banks and Doughty47]. Patients reported that community care orders [Reference Atkinson, Garner, Gilmour and Dyer32], guardianship or supervised discharged orders [Reference Canvin, Bartlett and Pinfold34], and community treatment orders [Reference Gibbs, Dawson, Forsyth and Mullen37–39] provided them with greater autonomy than other forms of legally mandated treatment. One patient reported enjoying “More freedom, responsibilities, choices, decision-making of my own rather than being told what to do all the time” [Reference Canvin, Bartlett and Pinfold34].
Recognition that treatment/admission was beneficial (n = 12)
Some patients reported that controls on their behavior, medications, and the electroconvulsive therapy that they received were beneficial. For example, “It placed controls on me that I needed when I first became ill”; “It made me take the tablets when I did not want to and needed to”; “It showed somebody cared”; and “They persuaded me to have the electric-shock treatments which have benefited me enormously” [Reference Adams and Hafner30]. Patients accepted their illness and the need for medications; “Does not bother me. I realize now that I’ve got to take the pills because I feel too much of a lack of adrenaline if I do not. They calm me down” [Reference Atkinson, Garner, Gilmour and Dyer32]. Patients believed that involuntary treatment was appropriate to manage those in crisis [Reference Brophy and Ring33]. Some patients requested to be placed under supervised orders because they found them to be beneficial [Reference Canvin, Bartlett and Pinfold34]. Patients expressed that community treatment orders helped them recover from illness, become independent, form close friendships, become aware of their illness, and prevented them from becoming severely ill [Reference Gibbs, Dawson, Forsyth and Mullen37]. A number of patients claimed that being on a CTO prevented suicide or self-harm, and that treatment was needed and ensured their safety [Reference Gibbs, Dawson, Ansley and Mullen38–40,Reference Sibitz, Scheutz, Lakeman, Schrank, Schaffer and Amering46,Reference Stroud, Banks and Doughty47]. One patient said; “And then, that you maybe for your own safety and the safety of others have to be locked in on the ward… it is done for my own good” [Reference Johansson and Lundman40]. Furthermore, patients believed that treatment was required for recovery [Reference Mezey, Kavuma, Turton, Demetriou and Wright41], and legally mandated treatment was described as a defining life experience [Reference Nordberg44].
Negative patient experiences (n = 15)
Restrictions on autonomy, rights, and freedoms (n = 12)
In reference to Guardianship Boards, patients said that it amounted to an infringement on their rights; “The fear of the police intruding on my privacy to take away my freedom was a real disadvantage when I was under a treatment order” [Reference Adams and Hafner30]. Patients reported that community care orders (CCOs) placed too many restrictions on their life. One individual did not like being told what to do by a “mere slip of the lass” [Reference Atkinson, Garner, Gilmour and Dyer32]. Several patients compared their involuntary treatment to being placed in jail [Reference Brophy and Ring33,Reference Gibbs, Dawson, Ansley and Mullen38]. Involuntary admission negatively affected patient freedom, lifestyle, and privacy; “I cannot do things I want to do. Travel, get a job, things like that” [Reference Canvin, Bartlett and Pinfold34]. They experienced a restriction on their autonomy and a fear that they would be detained if they did not obey; “The CTO restricts my liberty. The police can come to my flat whenever they want. They own my life. I’ve got no liberty” [Reference Fahy, Javaid and Best35]. In addition to loss of autonomy, patients reported feelings of coercion, and a recognition that as an involuntary patient, their views were no longer relevant [Reference Gault36]. Furthermore, they felt restricted in relation to their place of residence, physical movement, and social and work opportunities [Reference Gibbs, Dawson, Forsyth and Mullen37]. One patient was unable to visit his supportive father due to restrictions on the distance he could travel from his home [Reference Gibbs, Dawson and Mullen39]. Patients were overwhelmed by rules and inflexibility [Reference Johansson and Lundman40].
Deficiencies in communication/lack of information (n = 10)
Patients disliked an absence of appropriate communication and information; “I wasn’t told what was going on. It was like a court hearing. They should talk to you more”; and “I would have liked more discussion with the Board about my illness” [Reference Adams and Hafner30]. Patients would appreciate more communication with healthcare providers to divert their attention away from the negative aspects of their illness; “I think they could talk to me more often. I think it’s good, if you are lost in your own psychotic thoughts, then it’s good to be a little distracted… get something else to think about… It does not have to be about illness. It can be about the weather, sports, or whatever. I think they could do that more. Talk to the patients.” [Reference Andreasson and Skarsater31]. Patients were confused about the conditions and procedures surrounding their admission [Reference Atkinson, Garner, Gilmour and Dyer32,Reference Brophy and Ring33,Reference Murphy, McGuinness, Bainbridge, Brosnan, Felzmann and Keys42]. In one study, only 35% of patients reported satisfaction about the written information provided about their supervised community treatment; “I received info but did not understand it”; “written information was not clear for me to understand”; and “I cannot remember what it said” [Reference Fahy, Javaid and Best35]. Patients would have liked their views to be considered during their admission; “They talk about me behind my back, then they tell me what the team decided, the second time, they did not even have a ward round thing, the nurses just came up and said ‘right you are sectioned again’ I thought What?, it was a bit of a liberty” [Reference Gault36]. Furthermore, patients reported “being outside and not seen or heard”, receiving care without information, receiving a treatment they do not understand, being ignored, and wanting to be involved; “…I felt so extremely bad and I wanted someone to talk to, it was at night I recall. But he said ‘I cannot help you’ he said and he just went away, he could at least sit by my side. Or talk to me about anything then, I’m not, I do not expect him to work miracles but just being there would have been enough…” [Reference Johansson and Lundman40]. Patients would have appreciated more ordinary conversations and reported that healthcare staff often appeared aloof and unavailable [Reference Sibitz, Scheutz, Lakeman, Schrank, Schaffer and Amering46].
Discussion
This systematic review of qualitative studies explored the experiences of patients diagnosed with schizophrenia and related disorders while receiving variations of legally mandated treatment. Undergoing legally mandated or involuntary treatment is a complex and multi-faceted process that varies by jurisdiction [Reference Lepping and Raveesh48,Reference Gray, Hastings, Love and O’Reilly49]. This review is the largest review conducted to date including 18 qualitative studies with a total of 401 patients. Overall, patients reported satisfaction when their autonomy was respected and dissatisfaction when it was not. Patients retrospectively acknowledged that certain aspects of their treatment were beneficial and led to improved health outcomes. Importantly, patients were dissatisfied when there was limited communication of lack of information provided by healthcare staff.
Autonomy is a key tenet of healthcare ethics and outlines that patients should be permitted to make informed decisions about their healthcare, with freedom from controlling influences [Reference Beauchamp and Childress50]. Often patients who are admitted to hospital involuntarily lack capacity to consent to treatment, which limits their autonomy [Reference Sen, Gordon, Adshead and Irons51]. Patient autonomy is complicated by legally mandated treatment, since the patient’s diagnosis often interferes with their ability to consent to or decline treatment [Reference Zhang, Mellsop, Brink and Wang9,Reference Hess, Grudzen, Thomson, Raja and Carpenter52]. Patients who are more engaged in their treatment decisions exhibit improved treatment outcomes [Reference Loh, Leonhart, Wills, Simon and Härter53–56]. Patient participation includes being involved in decision making or expressing attitudes about different treatment options [Reference Thompson57]. An increased emphasis on collaborative care has the potential to increase the participation of patients in their own treatment and improve their autonomy [Reference Valentin-Hjorth, Patou, Syhler, MHD and Maier58].
Many patients described in this review retrospectively acknowledged that their treatment was beneficial. This is consistent with previous research, and is especially true for patients who achieved improvement of symptoms [Reference Katsakou and Priebe59,Reference Kane, Quitkin, Rifkin, Wegner, Rosenberg and Borenstein60]. In a previous systematic review, the majority of patients who were admitted involuntarily exhibited substantial improvement with treatment [Reference Katsakou and Priebe59]. Furthermore, between 33% and 81% of patients who were admitted involuntarily described their treatment as beneficial and/or justified [Reference Katsakou and Priebe59]. It has been argued through paternalistic grounds that involuntary treatment can be justified, namely that overruling of the patient’s autonomy is not always permanent. For example, involuntary treatment during a psychotic episode may restore a patient’s capacity, which would allow them to then make autonomous decisions [Reference Lepping, Palmstierna and Raveesh61].
Another theme that emerged from this review was that patients disliked deficiencies in communication and a lack of information regarding their treatment. Communication between patients with severe mental illness and their healthcare providers can be challenging [Reference Silverman, Kurtz and Draper62,Reference Poole and Higgo63]. However, improved patient communication leads to better health outcomes [Reference Stewart64,Reference Epstein and Street65]. Patient participation can be enhanced by working on the patient–physician relationship, recognizing the patient’s knowledge about their illness experiences, incorporating patient perspectives into shared decision making, and allocating sufficient time for patient participation [Reference Vahdat, Hamzehgardeshi, Hessam and Hamzehgardeshi66]. Furthermore, training of healthcare providers to improve communication skills with patients with severe mental illness has been shown to have a positive effect of patient experience in the therapeutic setting [Reference Papageorgiou, Loke and Fromage67,Reference McCabe, Heath, Burns and Priebe68].
We proceeded with a qualitative approach, which allowed us to gain insight into patients’ experiences [Reference Sandelowski69]. Qualitative research seeks to establish a holistic narrative and is flexible in its design [Reference Astalin70]. The qualitative research method that is most appropriate to use depends on the purpose of the study [Reference Teherani, Martimianakis, Stenfors-Hayes, Wadhwa and Varpio71]. Some of the qualitative approaches used in the reviewed studies include thematic analysis, grounded theory, phenomenology, inductive, and narrative. Each of these methods has its own advantages and disadvantages, which makes a direct comparison challenging. The narrative approach aims to explore the life of a person, phenomenology aims to understand the essence of the experience, and grounded theory develops a theory grounded in data from the field [Reference Johansson and Eklund72]. Thematic analysis develops themes based on the data [Reference Vaismoradi, Jones, Turunen and Snelgrove73]. Inductive analysis is similar to grounded theory and establishes potential themes a priori [Reference Thomas74].
The overall trend toward the deinstitutionalization of patients with psychiatric illness has led to an increased use of mandatory treatment in the community [Reference Brophy and McDermott75]. However, evidence regarding the efficacy of treatment in the community for patients with psychiatric illness is mixed [Reference Brophy and McDermott75–77]. There are various reasons why someone may be treated in the community rather than the inpatient setting [Reference O’Reilly, Hastings, Chaimowitz, Neilson, Brooks and Freeland78]. Mandatory treatment in the community was originally suggested to prevent frequent readmissions [Reference O’Reilly, Hastings, Chaimowitz, Neilson, Brooks and Freeland78]. It was also viewed as a method to increase access to care for patients with psychiatric illness [Reference Schneeberger, Huber, Lang, Muenzenmaier, Castille and Jaeger79–81]. This long-term approach supports the goal of recovery and re-integration into society, where patients are better prepared to pursue their personal education, social, and vocational goals [Reference O’Reilly, Hastings, Chaimowitz, Neilson, Brooks and Freeland78,Reference Anthony82].
This review provides some insight into patients’ experiences with legally mandated treatment beyond those reported in prior quantitative studies [Reference Kisely, Campbell and O’Reilly18]. Elaborating on the experiences of individuals with schizophrenia and related disorders was a recommended area of focus from previous reviews [Reference Katsakou and Priebe21,Reference Walker, Mackay, Barnett, Sheridan Rains, Leverton and Dalton-Locke83]. Despite the use of legally mandated treatment across the globe and accepted as a method to protect patients and society, ethical challenges continue to exist [Reference Zhang, Mellsop, Brink and Wang9,Reference Chin84]. Ethical issues related to the involuntary treatment of patients with psychiatric illness include conflicts between the principles of beneficence, autonomy and nonmaleficence. In medical ethics, beneficence (do good), nonmaleficence (do no harm), and autonomy should be valued equally [Reference Lepping, Palmstierna and Raveesh61,Reference Wettstein85]. Healthcare providers work toward achieving a balance between patients’ interests and those of society, and patient autonomy can be compromised when addressing this balance [Reference Wettstein85]. According to healthcare ethics, involuntary treatment is acceptable when it is in the patient’s best interest [Reference Salize, Dreßing and Peitz86].
There were several limitations of this systematic review. Three of the studies included in this review [Reference Gibbs, Dawson, Forsyth and Mullen37–39] were published by the same authors and used the same patient group. However, each study addressed slightly different aspects of patients’ experiences with community treatment orders. An additional limitation is the coding of qualitative data into positive and negative patient experiences. The analysis positioned findings as within a binary, whereas patient perspectives likely fall along a spectrum. Some aspects of care may be positive, others negative, and formerly positive experiences may at times be negative, and vice versa. Furthermore, there is the potential for selection bias in the included studies. For instance, results may have been coded as “positive” or “negative” because participants may have wanted to contribute socially desirable responses. Patients may have been inclined to provided positive responses, especially if members of their treatment team were running the study. In contrast, some participants may have seen the research as an opportunity to let their care team know how unhappy they were with their treatment, leading to predominantly negative descriptions. Furthermore, many of the included studies recruited patients from Oceania and Europe. There were limited studies published in North America, Asia, Africa, and South America. There are some potential explanations for this geographical imbalance. First, we excluded studies published in a language other than English. Second, rates of legally mandated treatment vary across the globe and are higher in some of the nations that were included in this review. For example, Australia tends to have higher rates of involuntary treatment than other English-speaking nations, such as the United States and Canada [Reference Light, Kerridge, Ryan and Robertson87]. Furthermore, most specialty mental health services in Australia are delivered in community settings and one-sixth of services comprise involuntary treatment [Reference Light, Kerridge, Ryan and Robertson87]. Third, while completing this review, it appeared that there was more research in general across Europe related to legally mandated treatment [Reference Salize, Schanda and Dressing88]. This may be partially explained by the finding that higher rates of involuntary hospitalization are associated with a lower rate of absolute poverty, with higher gross domestic product and healthcare spending per capita, an increased proportion of foreign-born people in a population, and greater amounts of inpatient beds [Reference Rains, Zenina, Dias, Jones, Jeffreys and Branthonne-Foster89]. Finally, criteria, procedures [Reference Saya, Brugnoli, Piazzi, Liberato, Di Ciaccia and Niolu7,Reference Hotzy, Kerner, Maatz, Jaeger and Schneeberger90], and rates [Reference Salize and Dressing11] of treatment in patients with psychiatric illness vary globally.
When patients with schizophrenia and related disorders are legally mandated to undergo treatment, they can have both positive and negative experiences. Retrospectively, many patients recognized that their treatment was beneficial, however, efforts should be made towards improving patient autonomy and ensuring clear communication with patients about their illness and treatment. Improving patient experiences is critical, as rates of involuntary admission are increasing and people with schizophrenia and related disorders are at higher likelihood of receiving legally mandated treatment [91–Reference Mulder, Uitenbroek, Broer, Lendemeijer, Van Veldhuizen and Van Tilburg94]. Training for healthcare providers that encourage patient-centered care may have positive effects on patient health behavior and health status [Reference Dwamena, Holmes‐Rovner, Gaulden, Jorgenson, Sadigh and Sikorskii95]. Findings from this study on patients’ experience could better inform healthcare providers when treating this vulnerable group of patients.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
J.E.P., S.B., and D.Z.B. have nothing to disclose. G.F. reports grants from the Canadian Institute of Health Research (CIHR) and the Center for Addiction and Mental Health (CAMH) Foundation, outside the submitted work. Z.J.D. reports grants from CIHR, the National Institute of Mental Health (NIMH), Brain Canada, and the Temerty Family and Grant Family, and through the CAMH Foundation and the Campbell Institute, outside the submitted work. D.M.B. reports grants from the National Institute of Health (NIH), CIHR, and Brain Canada. Z.J.D. and D.M.B. report other support from Brainsway and Megventure, outside the submitted work.






Comments
No Comments have been published for this article.