1. Introduction
Since Spring 2003, severe acute respiratory syndrome (SARS) prevailed in China and Hong Kong [4,28]. The whole world was under threat by this highly contagious, devastating viral pneumonia. The disease, which was later found to be due to a new coronavirus [21,22], took away 299 lives in Hong Kong, and 916 worldwide [25]. Princess Margaret Hospital has been designated to receive SARS patients in the early phase of the epidemic. Five hundred and ninety eight out of 1755 SARS patients were admitted into the hospital.
During the initial stage, much attention has been drawn to the definition, diagnosis and treatment of SARS. As time went on, many other complications of the disease and also of the treatment became apparent. Neuropsychiatric manifestations were among these complications. We saw patients attempted suicide during quarantine period, delirium was not uncommon Reference Cheng, Tsang, Ku, Wong and Ng[5], and many were anxious and worrying. Furthermore, many patients had neuropsychiatric symptoms persisted after discharge, and some patients developed new symptoms in the recovery phase. SARS had strong reasons to cause adverse neuropsychiatric impacts. It affected the whole family, either as being patients or patient contacts that required quarantine observations. High dose corticosteroids we used in the treatment, especially in the early epidemic when our knowledge on SARS was limited, had exposed patients to possible steroid related adverse effects. SARS was also a lethal disease and many patients required mechanical ventilation in intensive care units (ICU). Because of the contagious nature and unknown route of transmission, the disease carried a negative stigmatization. The purpose of our study is to evaluate the relative contributions of disease severity, use of corticosteroids and social factors on the symptoms in various neuropsychiatric domains in acute and convalescent phases.
2. Subjects and methods
2.1. Survey method
We conducted a questionnaire survey to 308 SARS victims who attended the Princess Margaret Hospital SARS follow up clinic from 15 April–15 May 2003. The questionnaires were administered by mail in early June 2003 with return envelopes. To encourage reply we gave phone call to all patients before sending them questionnaires. One of the questionnaires, the SARS Neuropsychiatric Symptoms Checklist (NPSC), was specifically designed to evaluate the neuropsychiatric complaints after SARS according to our initial experiences Reference Cheng, Tsang, Ku, Wong and Ng[5]. It consisted of 25 items covering six neuropsychiatric domains of interest (see Appendix for questionnaire), namely cognition (Q1–4), mania (Q5–8), depression (Q9–15), anxiety (Q16–18), psychosis (Q19–21) and behavioural symptoms (Q22–25). The items were scored on a four-point ordinal scale with ‘0’ representing ‘none’ and ‘3’ ‘always’. This questionnaire was duplicated into four. Two questionnaires were administered by patients and two were administered by their families. The first set was rated to the best of their recall during hospital stay (at acute phase), and the second set was rated according to their present state (at convalescent phase). The questionnaires administered by family members served to evaluate the reliability of the information provided by the patient. Severity of the SARS symptoms was recorded on a separate eight-item checklist using an ordinal scale from 0 to 3, which gave a maximum possible score of 24. We also included General Health Questionnaire 28 (GHQ28) as a screening tool for psychological well being at convalescent phase Reference Chan and Chan[3]. The study was approved by local ethics committee, and informed consent was obtained from every participant.
2.2. Reliability and consistency of NPSC
We performed the Pearson correlation between the patient rated questionnaire and family rated questionnaire on each neuropsychiatric domain. Using the strength assessment suggested by Munro Reference Munro[18], moderate strength correlations were assigned to cognition, depression, psychosis and mania while the correlation strength in anxiety was low. The items on behavioural symptoms were not well correlated. We believed families were difficult to observe the behavioural changes because they were not allowed to have direct patient contact during hospital stay. Cronbach α, which indicated the lower bound of inter-item correlation in a cluster of items Reference Cronbach[8], revealed a good internal consistency in the cognition (α = 0.70), anxiety (α = 0.78) and depression (α = 0.83). The questionnaire performance in convalescent phase was significantly correlated with GHQ28 (r = 0.64, P < 0.001).
2.3. Exploratory factor analysis on NPSC at acute and convalescent phases
For the acute phase, we extracted six components in the initial principle component analysis with eigen value more than one Reference Crocker and Algina[7]. According to the clustering of items at a factor loading cutoff of 0.4, we reconstructed the factor domains into anxiety-depression, psychosis, positive attitude, mania, cognition and behavioural symptoms, respectively. The common factors explained 65.3% of the total variances in the items. The factor structure at convalescent phase was slightly different from above. Instead of the six domains in acute phase, we constructed four common factors, namely anxiety-depression, positive psychological well-being, cognition and mania, which altogether explained 63% of the total variances in the items at convalescent phase.
2.4. Relationship between disease severity, use of corticosteroids, social factors and the neuropsychiatric symptoms of SARS patients in acute and convalescent phases
Factors scores calculated in each domain were used as the neuropsychiatric outcomes of interest for each patient. Effects of representative variables chosen for SARS severity, dosage and form of corticosteroids and social factors on the outcome variables were first examined in the univariate analysis, covariates were then tested in the multiple linear regression model. We used the SPSS software in statistical analysis [26]. All tests were two-end conducted at 0.05 level of significance.
3. Results
We received 102 valid replies, the response rate was 33%. The demography, social backgrounds and the clinical features of the replied were tabulated in tables 1 and 2, respectively. The mean duration from hospital discharge to questionnaire administration was 42 days (range 26–86). Sixty-six patients scored five or above in GHQ28, a cutoff level which indicated severe symptoms and possible benefit from psychiatric consultation.
table 1 Demography and social background of SARS survivors

table 2 Clinical variables of SARS survivors

3.1. Medications given for SARS
All but one patient received ribavirin and corticosteroids. Most patients received intravenous ribavirin at 1200 mg daily for 10–14 days. Different forms of corticosteroids, including hydrocortisone, prednisolone and methylprednisolone, were given in various dosages. About half of patients received pulse methylprednisolone at 500–1000 mg per dose. Apart from ribavirin and corticosteroids, all patients received potent antibiotics for empirical treatment. Antibiotics commonly used included extended spectrum penicillins, macrolides, fluoroquinolones and aminoglycosides.
3.2. Neuropsychiatric symptoms at acute and convalescent phases
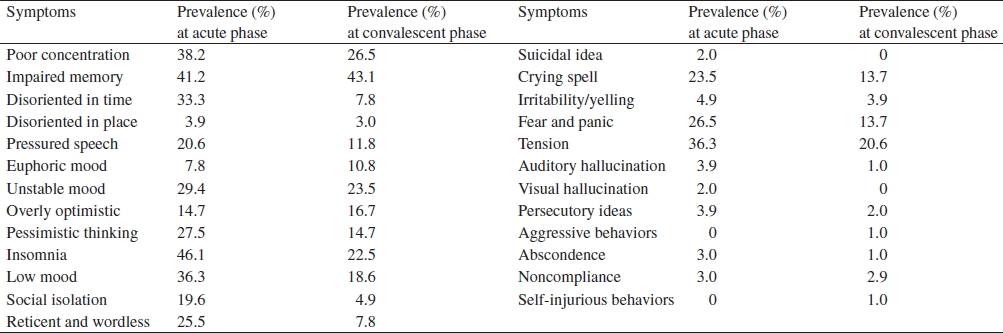
As presented in table 3, neuropsychiatric complaints were common at both acute and convalescent phases. In the analysis, only those answered 2 or 3 were regarded as ‘Yes’ for that item. Most of the common complaints, like poor concentration, memory, insomnia and tension, were consistent with anxiety and depression. A high proportion of time disorientation could suggest delirium, and psychotic symptoms were reported by a few. A decrease in prevalence at convalescent phase was noticed in most of the checklist items except poor memory, which persisted at high level of 43%. There was a higher degree of optimism among patients at convalescent phase.
table 3 Prevalence of symptoms on NPSC items. A score of 2 or 3 was regarded ‘Yes’ for the item
SARS sym, SARS symptoms; DOS-acute, duration of stay in acute hospital; SaO2, oxygen saturation; TPS, total dose of pulse steroid; PS, use of pulse steroid, N/F DSARS, neighbour/friend died of SARS; HCW, health care worker; Fam. DSARS, family member died of SARS, Fam. Supp., family support; Mental illness, history of mental illness.
3.3. Factors associated with neuropsychiatric complaints in acute phase
Severity of SARS and the corticosteroids were significantly associated with anxiety depression, psychosis and behavioural problems in acute phase (table 4). Health care workers had more anxiety-depression in univariate analysis, but the effect was not significant after controlling for covariates. Nevertheless, health care worker still had more cognitive problems at shown in our regression model, but they seemed to be protected from psychosis. All together, our model predicted 52% of the observed variance in anxiety-depression and 33% in psychosis. Individually, effects of disease, corticosteroids and social factors accounted for 29.9%, 2.9% and 18%, respectively of the observed variances in anxiety-depression, and 11%, 3.1% and 15.7% of the observed variances in psychosis at acute phase.
table 4 Factors contributing to neuropsychiatric symptoms at acute phase, multiple linear regression analysis using factors scores in each construct as dependent variables

3.4. Factors associated with neuropsychiatric complaints in convalescent phase
In the convalescent phase, the factors were less influential as the best model only predicted 33% of the observed variances in anxiety-depression (table 5). Noteworthy, effect of corticosteroids persisted in the convalescent period and was identified as a risk factor against psychological well-being. Being health care workers, which was not an independent risk factor for anxiety-depression at acute phase, became a risk factor at convalescence. Corticosteroids and being health care workers accounted for 5.1% and 2.8%, respectively of the observed variances in anxiety depression.
table 5 Factors contributing to neuropsychiatric symptoms at convalescent phase, multiple linear regression analysis using factors scores in each construct as dependent variables
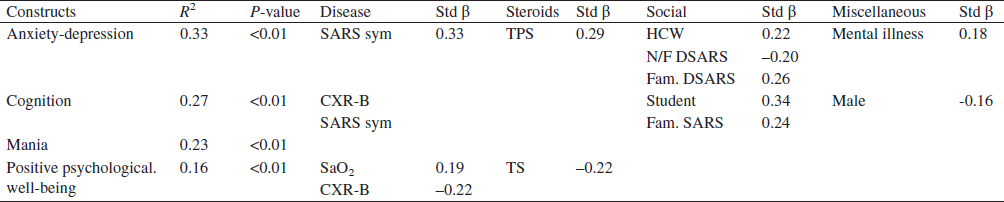
SARS sym, SARS symptoms; CXR-B, bilateral involvement on CXR; SaO2, oxygen saturation; TPS, total dose of pulse steroid; TS, total(accumulated) dose of steroid; HCW, health care worker; N/F DSARS,neighbour/friend died of SARS; Fam. DSARS, family member died of SARS; Fam. SARS, family member had SARS; Mental illness, history of mental illness.
4. Discussion
4.1. Limitations of the study
This study was a retrospective data collection relied on recalls from patients. The valid response rate at 33% was not high in a mail questionnaire survey. We learnt that at least four other studies were carried at the same time, and some patients did not want to join too many different studies. The age distribution and proportion of health care workers in our replied sample were similar to the Hong Kong cohort [25], but the male gender was underrepresented in our sample (34.3% in the sample vs. 44.3% in Hong Kong cohort). We did not have a good reason to explain this difference. In a post hoc survey on the utilization of clinical psychology service by SARS patients, we found our study sample was comparable to non-responders as well as the Hong Kong cohort, suggesting a similar psychological outcome. We believed our sample was representative of the Hong Kong SARS. We admitted difficulty in assessing the accuracy of information collected, although the worry was partially offset by the good item correlation in the family valued answers. The pattern of correlation, in which easily observed symptoms were better correlated than the difficult ones, suggested an independent rating in the questionnaires.
4.2. Disease severity, corticosteroids, social factors and neuropsychiatric outcomes
We focused on the modifying effects of disease, corticosteroids and social factors on neuropsychiatric complaints in SARS patients. Many of the anxiety-depression symptoms were adjustment reactions during acute stage of illness, and some of the symptoms like insomnia and poor concentration could also represent posttraumatic stress disorder (PTSD) which was expected to be common in this epidemic. Although we did not have information on psychological well being in the community during the epidemic as a control, our findings did show an impact from the factors we studied on the neuropsychiatric symptoms, both at acute and convalescent phases. Our patients were treated in isolation settings and had lots of uncertainties on their health. These were similar to patients treated in ICU where many have developed PTSD as a result [10,11]. We believed these constituted the main unmeasured variances and might also explain the inability of our questionnaire to show up the ICU impact.
Non-human coronaviruses like the mouse hepatitis virus in rats and haemagglutinating encephalomyelitis virus in pigs could cause demyelination and central nervous system (CNS) infections Reference Monto and Evans[17]. Since the new SARS associated coronavirus (SARS-CoV) was postulated to be originated from animals Reference Guan, Zheng, He, Liu, Zhuang and Cheung[9], direct involvement of nervous system in SARS was not impossible. Although clinical encephalitis was not seen in our patients, the virus had been identified in the cerebrospinal fluid Reference Lau, Yu, Chu, Lau, Sheng and Yuen[12]. We could not exclude a possible direct role of SARS-CoV in the neuropsychiatric symptoms we described.
Neuropsychiatric symptoms after a non-CNS viral infection were uncommon. The most frequently described neuropsychiatric problem after a viral infection was chronic fatigue syndrome (CFS), which also shared symptoms of anxiety and depression [6,23]. Our survey method could not distinguish CFS from other psychiatric diagnosis. We believed some of our patients might suffer CFS, especially if their symptoms persisted.
Previous reports suggested a high prevalence of dose related steroid effect on mental problems [2,14,15,20]. Since most of our patients had been given high dose corticosteroids, and there was no control group for comparison, its relative importance would be underestimated. Despite this restriction we still demonstrated a significant effect of corticosteroids especially on anxiety-depression in both phases, which was consistent with previous work that 80% of the steroid induced psychiatric disturbances were affective symptoms [2].
Our affected health care workers had more anxiety-depression after recovering from SARS. Health care professionals were well known to be among the group of high occupational stress Reference Laposa, Alden and Fullerton[13]. They were prone to develop overt psychological reactions under great stress like massive casualties [1,24]. In fact many unaffected staffs were carried away with unhappy memories during the epidemic. Many recovering health care workers still had problem of confidence and role adjustments. Some felt guilty on transmitting the disease to their families, and some staffs found themselves being isolated from other colleagues. They also worried about potential occupational hazards in the future, compensation issues, insurances, new hospital policies, etc. To address the importance of psychological health, the hospital has incorporated psychology sessions in the newly implemented infection control trainings. We encouraged psychology modules in medical and nursing schools, and consultation services should be easily assessable by all frontline medical staffs.
Our preliminary finding on a high prevalence of memory impairments at convalescence would need further confirmation. It could be steroid related. Through its effect on hippocampal metabolism, a big dose of exogenous steroid could induce reversible memory impairments as shown both in healthy subjects Reference Lupien, Gillin and Hauger[16] and in treatment of multiple sclerosis patients Reference Oliveri, Sibilia, Valentino, Russo, Romeo and Quattrone[19]. Chronic stimulation in the case of Cushing's disease could cause atrophy of the hippocampus Reference Starkman, Giordani, Berent, Schork and Schteingart[27]. Poor memory could also be a symptom of CFS which frequently accompanied with viral infections Reference Christodoulou, De Luca, Lange, Johnson, Sisto and Korn[6]. Adrenal insufficiency after steroid withdrawal is another possibility, especially when both the dosage was high and the duration was long. Further study is definitely required.
5. Conclusion
Our study suggested severity of SARS, high dose corticosteroids and being health care workers were independent predictors of neuropsychiatric complaints in both acute and convalescent phases.
Acknowledgments
The authors were indebted to Dr. Chee Wing Wong and Dr. Yin Kwok Ng from Kwai Chung Hospital who gave us invaluable comments in conducting this study. This study could not be possible without the strong support from Dr. Eugene Yuk Keung Tso, Dr. Owen Tak Yin Tsang, Dr. Kin Wing Choi and Dr. Wing Lok Tong from Princess Margaret Hospital and also Dr. Kuen Lam from Caritas Medical Centre. We would express our highest respect to all staffs from Department of Medicine and Geriatrics as well as the Department of Intensive Care of Princess Margaret Hospital, and also to many doctors from government and private sector who volunteered to fight against SARS during the epidemic in 2003.
Appendix
SARS neuropsychiatric symptoms checklist
Filled in by recovered SARS patients. During the period of hospitalization, you may have the following symptoms. Please indicate the frequency of each symptom with following scale:
0 = Not present
1 = Sometimes
2 = Often
3 = Always
1. Poor concentration
2. Impaired memory
3. Disoriented in time
4. Disoriented in place
5. Pressured speech
6. Euphoric mood
7. Unstable mood
8. Overly optimistic
9.Pessimistic thinking
10. Insomnia
11. Low mood
12. Social isolation
13. Reticent and wordless
14. Suicidal idea
15. Crying spell
16. Irritability/ yelling
17. Fear and panic
18. Tension
19. Auditory hallucination
20. Visual hallucination
21. Persecutory ideas
22. Aggressive behaviors
23. Abscondance
24. Noncompliance
25. Self-injurious behaviors
SARS Neuropsychiatric Symptoms Checklist
Filled in by recovered SARS patients. After discharge from hospital and cessation of steroid, you may have the following symptoms. Please indicate the frequency of each symptom with following scale:
0 = Not present
1 = Sometimes
2 = Often
3 = Always
1. Poor concentration
2. Impaired memory
3. Disoriented in time
4. Disoriented in place
5. Pressured speech
6. Euphoric mood
7. Unstable mood
8. Overly optimistic
9. Pessimistic thinking
10. Insomnia
11. Low mood
12. Social isolation
13. Reticent and wordless
14. Suicidal idea
15. Crying spell
16. Irritability/ yelling
17. Fear and panic
18. Tension
19. Auditory hallucination
20. Visual hallucination
21. Persecutory ideas
22. Aggressive behaviors
23. Abscondance
24. Noncompliance
25. Self-injurious behaviors








Comments
No Comments have been published for this article.