Introduction
At the wake of the COVID-19 pandemic, leading global and local health authorities [Reference Douglas, Douglas, Harrigan and Douglas1–3] as well as the public [Reference Cowan4] expressed worries about what the pandemic and the restrictions imposed to curb its spread may do to public mental health – based on experiences of previous pandemics [Reference Maunder5–Reference Cheng and Cheung7]. COVID-19 restriction measures were implemented by governments to reduce spread of the virus and typically included restrictions on movement, gatherings, business operations, and school closures, as well as the promotion of social distancing and hygiene measures. “Social distancing” has been one of the more common restrictions [Reference Mahase8] and has included mandates for individuals to self-isolate at home if experiencing COVID-19 symptoms. Other common COVID-19 restrictions have included bans on large gatherings; school closures; closures of “non-essential” places; and limiting contact with those who are at higher risk of developing severe COVID-19 [9]. Policies have varied in their breadth and duration across countries, from partial restrictions to complete stay-at-home-orders. They have been linked to negative impacts on society such as loneliness, worry, social isolation [Reference O’Connor, Wilding, Ferguson, Cleare, Wetherall and McClelland10], as well as increased stresses imposed on children and adolescents due to school closures [Reference Viner, Russell, Saulle, Croker, Stansfield and Packer11]. It has also been suggested that COVID-19 restrictions could trigger anxiety and depression through increased feelings of loneliness, heightened grief after bereavement as a result of not being able to visit the dying or attend memorial services, and the deprivation of personal liberties [Reference Santomauro, Mantilla Herrera, Shadid, Zheng, Ashbaugh and Pigott12]. Indeed, a previous study of 15 countries, 10 of which were European, found a significant albeit small association between policy stringency and psychological distress [Reference Aknin, Andretti, Goldszmidt, Helliwell, Petherick and De Neve13].
Findings regarding the effects of the pandemic on mental health have been mixed. A global meta-analysis of 48 studies covering the first year of the COVID-19 pandemic found that population mobility and daily COVID-19 infection rates were associated with an approximately 25% increase in the prevalence of probable major depressive disorder and generalized anxiety disorder in 2020 compared to 2019 [Reference Santomauro, Mantilla Herrera, Shadid, Zheng, Ashbaugh and Pigott12]. The study concluded that the consequences of the pandemic and restriction measures included short- and long-term impacts on rates of common mental disorders (CMDs) [Reference Santomauro, Mantilla Herrera, Shadid, Zheng, Ashbaugh and Pigott12]. On the other hand, other reviews and meta-analyses assessing studies with pre-pandemic to during pandemic data found no changes in the prevalence of a broader range of mental disorders and symptoms when assessed after mid-2020, though there was an initial increase in the prevalence at the beginning of the pandemic [Reference Robinson, Sutin, Daly and Jones14, Reference Sun, Wu, Fan, Dal Santo, Li and Jiang15].
Observing changes in CMDs during the COVID-19 pandemic is insufficient to prove that the pandemic gave rise to such changes. It is crucial to examine the association between CMDs and COVID-19 restriction measures, particularly in European countries, which is a relatively unexplored area [Reference Ren, Huang, Pan, Huang, Wang and Ma16], and has to our knowledge not been assessed in European countries in particular. The varying types, intensities, and timing of restrictions, along with similar healthcare systems and demographics in Europe, offer a unique chance to investigate the relationship between restriction measures and mental health. A better understanding of these associations may strengthen evidence-based policymaking and safeguard European population mental health during any future public health emergencies.
This aims of this study were to [Reference Douglas, Douglas, Harrigan and Douglas1] determine how the COVID-19 pandemic affected rates of self-reported emotional distress (from now on referred to as “mild CMD” or “mild anxiety/depression”) and anxiety and depression (from now on “severe CMD” or “severe anxiety/depression”) across Europe and [Reference Holmes, O’Connor, Perry, Tracey, Wessely and Arseneault2] explore whether public health restriction policies were related to changes in the rates of mild and severe CMDs. The research questions to be specifically addressed were:
-
1. How did rates of self-reported mild and severe CMDs change in Europe from pre- and early pandemic to later on during the COVID-19?
-
2. Were changes different for mild and severe CMDs?
-
3. Were changes in the prevalence of self-reported mild and severe CMDs different between the sexes and different age groups?
-
4. Were social distancing and school restriction measures associated with changes in self-reported mild and severe CMDs in Europe?
Methods
The screening of the articles and reporting of this meta-analysis were guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [Reference Page, McKenzie, Bossuyt, Boutron, Hoffmann and Mulrow17] and the Meta-analysis of Observational Studies in Epidemiology recommendations [Reference Stroup, Berlin, Morton, Olkin, Williamson and Rennie18].
Eligibility criteria
This meta-analysis included population-based prospective and cohort studies that addressed COVID-19 and CMD outcomes. Studies reporting the following data were included: (1) self-reported depression or/and anxiety; (2) depression or/and anxiety from pre-/early pandemic and during the COVID-19 pandemic; (3) data from any European country; (4) longitudinal or repeated cross-sectional studies; (5) study samples representative of the general population; and (6) the outcomes(s) measured by one if the validated instruments used in the previously published meta-analysis (e.g., GAD-7, HADS, PHQ-9, World Health Organization [WHO]-5 – for a comprehensive list, see Supplementary Table S2) [Reference Santomauro, Mantilla Herrera, Shadid, Zheng, Ashbaugh and Pigott12]. Studies were excluded if they were editorial papers or cross-sectional studies that evaluated depression or anxiety at only one time point. No language limitations were set for the search, and both published studies and unpublished studies were included if data were available. No manual searches were conducted.
Timing of the COVID-19 pandemic
According to the WHO, COVID-19 could be characterized as a pandemic on March 11, 2020, and the countries included in this meta-analysis started implementing government restrictions spanning from March 10 (Czech Republic) to March 23 (UK). This study considered pre-, early, and during pandemic time waves, to allow for the study of changes in CMDs, as well as the impact of restriction measures, which in many cases had not been implemented in the early pandemic period of the present study: The pre-pandemic time wave of the present study refers to the first data collection time point before March 11, 2020, and the early pandemic wave refers to the first data collection point between March 11, 2020 ,and March 31, 2020 (apart from in Austria, where data were collected in April 2020). The pandemic time wave refers to the latest data collection point of each individual study during the pandemic – April 21, 2022 at latest. The latest time point was included to allow for the assessment of more enduring effects.
Information sources and search strategy
This study builds upon previous findings from a meta-analysis on the effects of the COVID-19 pandemic on mental disorders [Reference Santomauro, Mantilla Herrera, Shadid, Zheng, Ashbaugh and Pigott12]. The present study builds upon the search strategy and search results of the published study, including all the studies found through that review, as well as an additional literature search – therefore, the present meta-analysis includes studies from January 1, 2020 until April 21, 2022. The added value of the present study in relation to the previous meta-analysis [Reference Santomauro, Mantilla Herrera, Shadid, Zheng, Ashbaugh and Pigott12] is the updated literature search, the narrower focus on European countries as detailed in the introduction, the assessment of the effects of restriction measures in particular, and assessment of effects on both mild and severe CMDs.
The searches for the present review were conducted in PubMed database (National Library of Medicine) (published studies) and in the COVID-MINDS database (gray literature). We included studies/protocols published between January 30, 2021 (which was the end point date of the previous meta-analysis search [Reference Santomauro, Mantilla Herrera, Shadid, Zheng, Ashbaugh and Pigott12]), and April 21, 2022. The keywords used in the search included different COVID-19 terms, CMDs, European countries’ names, and CMD outcome measurements; the search strings are shown in Supplementary File S1. The self-report outcome measures and the cut-off thresholds that were used can be found in Supplementary File S2.
Study selection
Two investigators (M.N. and V.L.) screened and identified potentially relevant titles, abstracts, and full texts independently. If there was any disagreement between the assessors, they consulted with a third investigator (P.F.) to reach an agreement. The Newcastle–Ottawa scale (NOS) was used to assess the quality of studies [Reference Wells, Shea, O’Connell, Peterson, Welch and Losos19].
Data extraction
A standardized data extraction template specifying requested data in detail was sent to all corresponding authors with access to microdata or aggregated data, depending on availability. The requested data included the following: the time period for the data collection, region, age group, sex, outcome measure, mean, 95% confidence interval (CI), standard deviation, number of respondents, number of respondents above mild threshold of self-reported anxiety and/or depression, and number of respondents above severe threshold of depression and/or anxiety. An invitation e-mail and three extra reminders in case of non-response were sent to all identified corresponding authors of the included studies.
The “female ratio” and “mean age” at baseline were collected from the original publications and datasets, and age ranges of 0–18, 19–64, and 65+ were used. The containment severity index was provided by Kubinec et al. [Reference Kubinec, Barcelo, Goldszmidt, Grujic, Model and Schenk20] and measures the intensity of government responses to COVID-19 across six distinct policy areas (for more details, see Supplementary File S3). We only used the “social distancing” and “school closures” measures as independent variables. The choice was motivated by the direct cost of these particular policies on the social isolation of the people under a government’s jurisdiction, which may therefore incur impacts on CMDs.
For the independent variables data, we chose the point prevalence of CMD for each study based on their primary outcome pre-/early and during pandemic time frames. For both pre-/early and during pandemic time frames, the recall period of the outcome measure used in each study was added to the time frame. The recall period for each outcome measure is listed in Supplementary File S2. The mean value restriction measure of each pre- and during pandemic time frame was calculated to assess associations with the changes in the prevalence of CMDs. The difference in values was calculated as the data from the during pandemic time point minus the data from the pre-pandemic time point.
Statistical analysis
The analyses generated pooled estimates of changes in the CMD prevalence in European countries both for (1) pre-during pandemic periods and for (2) early–during pandemic periods separately. Thus, the pooled results are reported as the average pre-/early-to-during difference in the prevalence (ΔPrev) and its 95% CI. Following the methodological recommendations [Reference Spineli and Pandis21], we also estimated and reported prediction intervals that reflect the uncertainty expected in the pooled results if a new study is included in the meta-analysis. We acknowledge that in case of high heterogeneity, the prediction interval will be wider than the 95% CI of the pooled results and that prediction intervals are imprecise if less than five studies are pooled [Reference Spineli and Pandis21] – thus, we do not report prediction intervals for subgroup analyses with <5 studies. First, we conducted a meta-analysis of changes in the prevalence of mild and/or severe anxiety and/or depression using random-effects analysis. Then, we studied those changes in mild and severe depression and anxiety in relation to demographic factors and changes in the COVID-19 restriction measures (in univariate meta-regression models, which were followed by additional adjustment for study quality). We ran models for the joint data of depressive disorder and anxiety disorders (mild and severe analyzed separately) first and then ran them separately for depressive disorders and anxiety disorders (mild and severe analyzed separately).
Statistical heterogeneity among studies was assessed using Q-test and I 2 statistics. For the Q statistic, a two-sided P < 0.10 was considered as representative of statistically significant heterogeneity, and I 2 values of 25, 50, and 75% were regarded as low, moderate, and high heterogeneity, respectively. Then, we conducted a univariate meta-regression relating changes in the prevalence of CMDs to changes in the restriction measures. Potential publication bias for each outcome in the main analyses was visualized by funnel plots and assessed using Egger regression asymmetry test [Reference Egger, Davey Smith, Schneider and Minder22]. If publication bias was revealed, the contour-enhanced funnel plot and Duval and Tweedie nonparametric trim and fill method were used to further test the data [Reference Duval and Tweedie23]. Sensitivity analyses were also conducted, where data from studies including children only [Reference Widnall, Winstone, Mars, Haworth and Kidger24] were excluded. Finally, influence analyses (also called “leave-one-out” analyses) were performed for each outcome by iteratively removing one study at a time to explore if the findings were influenced by any single study. All the analysis was performed in Stata MP 17.1 (StataCorp LLC, College Station, TX), and a two-sided P-value of < 0.05 was considered statistically significant. The codes for statistical analysis can be found in Supplementary Appendix 2.
Results
Study characteristics
The flowchart of the study selection process is shown in Figure 1. First, we included 13 studies from the previous meta-analysis (“Reference study” in Figure 1), which had screened altogether 5683 titles [Reference Santomauro, Mantilla Herrera, Shadid, Zheng, Ashbaugh and Pigott12]. Thereafter, our PubMed search yielded a total of 589 additional titles of published articles that were screened for eligibility. After the screening of titles and abstracts, 576 articles were excluded, which resulted in 14 full texts being screened. Five of these were excluded, which resulted in nine published articles being included in the meta-analysis. The gray literature search yielded a total of 170 studies from title screening, and the further screening steps of contacting authors to gain information about the study data resulted in 13 studies being included from the gray literature screening. However, due to time and financial restrictions, we were only able to include the studies in the present meta-analysis for which authors were able to provide data by September 31, 2022, which resulted in the exclusion of 8 of the 13 studies from the gray literature screening. In total, our study selection process resulted in 15 datasets from 27 studies that were eligible for inclusion in this meta-analysis.
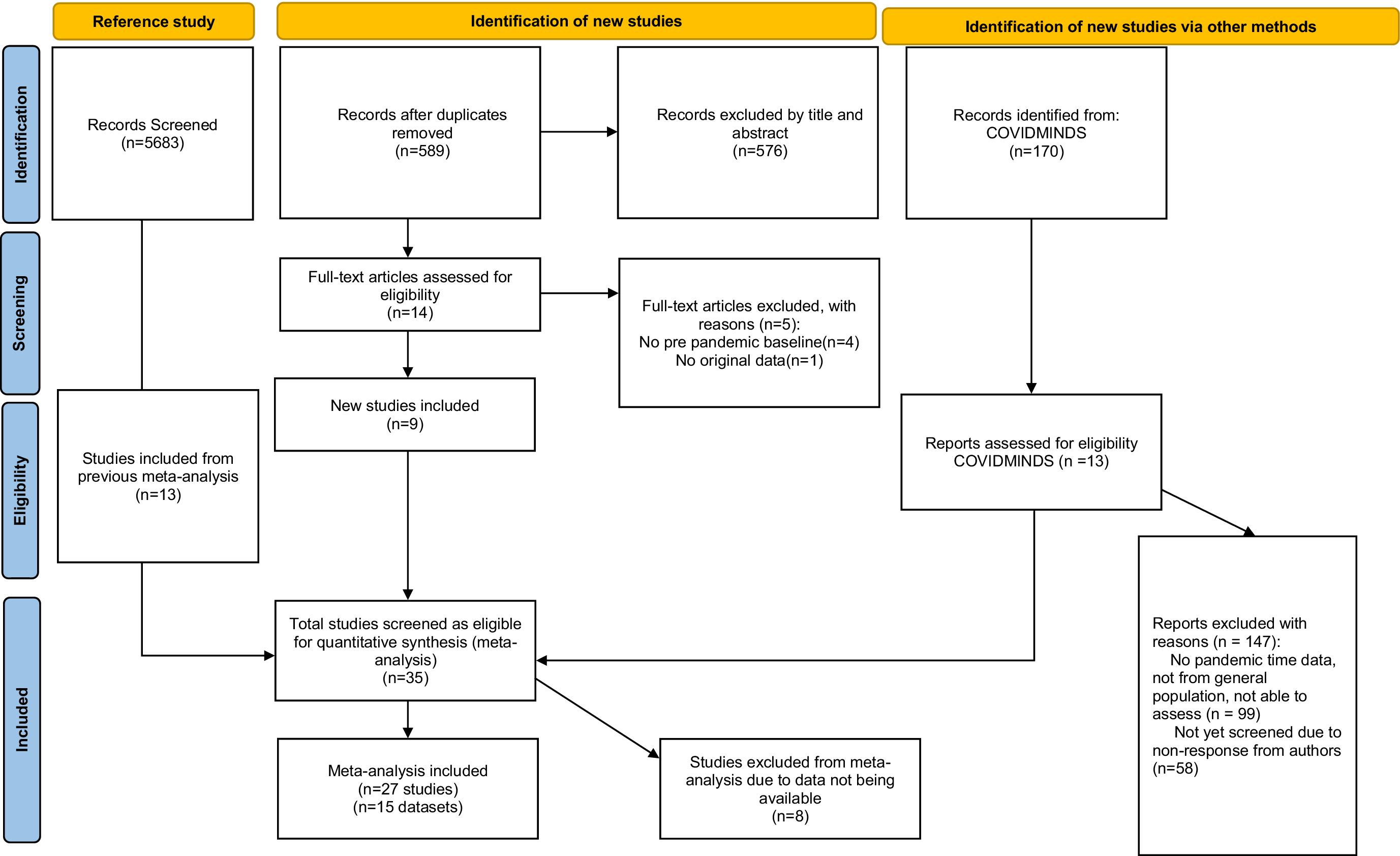
Figure 1. PRISMA flow diagram illustrating the study selection process.
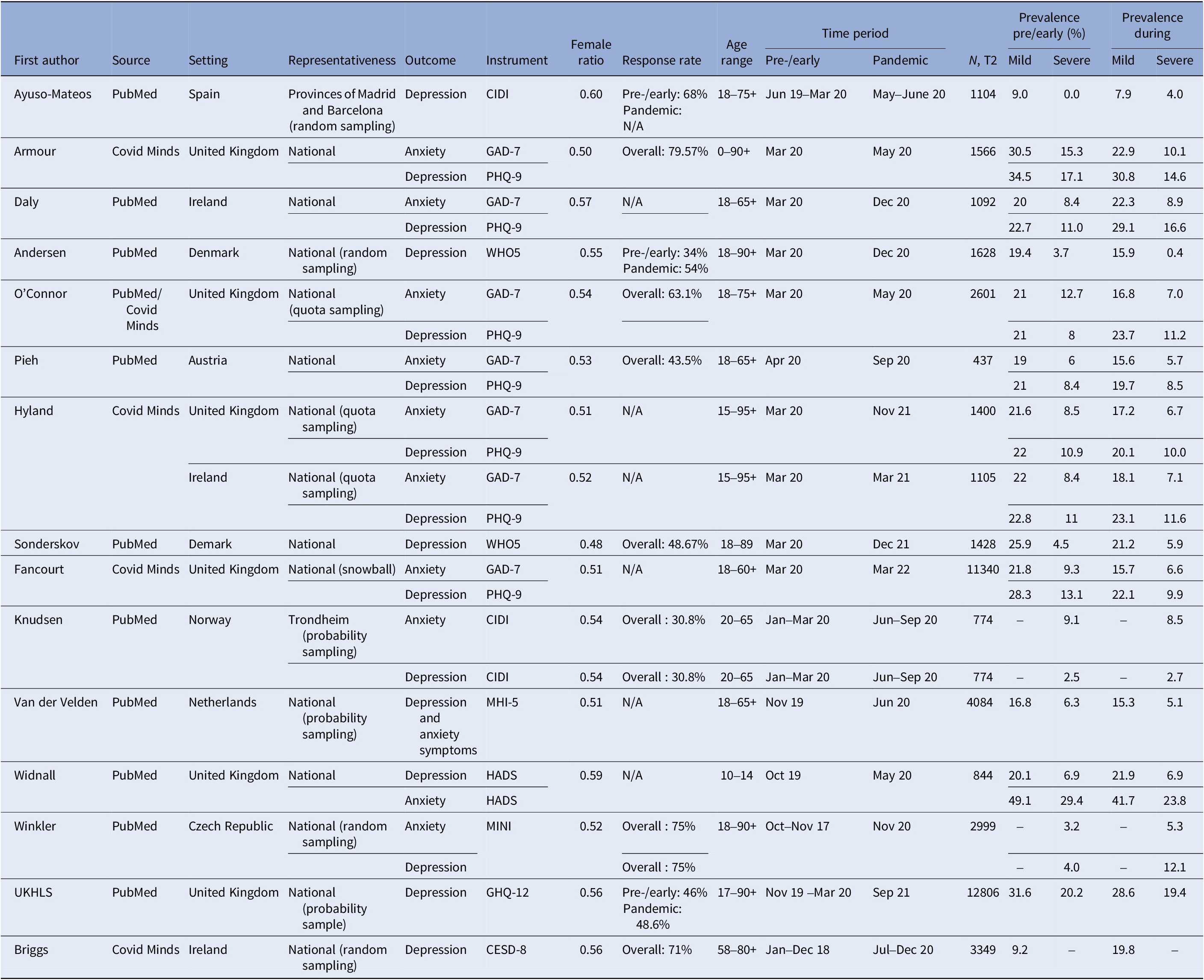
Table 1 overviews the included datasets and studies, and the total number of respondents at baseline from all studies was 88,620. The age range was from 12 to 99 years, the proportion of females was 54.7%, and the data of the included studies were gathered between October 2017 and March 2022. Studies with early pandemic data were from Spain [Reference Ayuso-Mateos, Morillo, Haro, Olaya, Lara and Miret25], the United Kingdom [Reference O’Connor, Wilding, Ferguson, Cleare, Wetherall and McClelland10, Reference Armour, McGlinchey, Butter, McAloney-Kocaman and McPherson26–Reference Fancourt, Steptoe and Bu30], Ireland [Reference Shevlin, McBride, Murphy, Miller, Hartman and Levita28, Reference Hyland, Shevlin, McBride, Murphy, Karatzias and Bentall29, Reference Daly, MacLachlan, Maguire, Power, Nolan and Shevlin31], Denmark [Reference Andersen, Fallesen and Bruckner32–Reference Sønderskov, Dinesen, Santini and Østergaard34], and Austria [Reference Pieh, Budimir, Humer and Probst35, Reference Pieh, Budimir and Probst36], and those with pre-pandemic data were from the Netherlands [Reference van der Velden, Hyland, Contino, von Gaudecker, Muffels and Das37], the United Kingdom [Reference Widnall, Winstone, Mars, Haworth and Kidger24, Reference Davillas and Jones38–Reference Proto and Zhang41], Ireland [Reference Briggs, McDowell, De Looze, Kenny and Ward42], Norway [Reference Knudsen, Stene-Larsen, Gustavson, Hotopf, Kessler and Krokstad43], and the Czech Republic [Reference Winkler, Formanek, Mlada, Kagstrom, Mohrova and Mohr44, Reference Winkler, Mohrova, Mlada, Kuklova, Kagstrom and Mohr45]. For a table including all results from all meta-analyses, please see Supplementary Tables S5 and S6, and for data visualizations in time plot graphs see Supplementary Figures S1 and S2. Of the 15 included studies, 11 obtained an overall quality score or 6 stars, while 4 obtained an overall quality score of 7 stars according to the NOS [Reference Wells, Shea, O’Connell, Peterson, Welch and Losos19]. The quality scoring for each included study can be found in the Supplementary Table S4.
Table 1. Summary of studies (n = 27) and datasets (n = 15) included in the meta-analysis
Changes in the prevalence of mild and severe levels of anxiety and depression
The meta-analysis of all included five datasets with data from pre-pandemic periods did not show any significant change in self-reported severe anxiety and/or depression from before the pandemic to during the pandemic in any of the demographic groups studied (see Supplementary Table S5) – the results did not significantly change in the sensitivity analyses where the dataset including children only [Reference Widnall, Winstone, Mars, Haworth and Kidger24] was removed (data not shown). Due to small number of studies, the analysis of publication bias and influence analysis were conducted only for anxiety and depression combined (mild and severe separately). No publication bias was detected (see Supplementary Figure S3B,C,E,F for corresponding funnel plots), and no influence of individual study on a pooled results was observed (see Supplementary Note S5). However, among the datasets with data from early pandemic, significant, but very minor decreases were found in levels of mild anxiety and depression combined (ΔPrev = −0.050 [95% CI: −0.085, −0.014], P = 0.006; I 2 for heterogeneity 98.3%; and 95% prediction interval [−0.13, 0.03]) (Figure 2), mild anxiety alone (ΔPrev = −0.055 [95% CI: −0.094, −0.017], P = 0.005; I 2 = 95.3%; and 95% prediction interval [−0.137, 0.026]), severe anxiety and depression combined (ΔPrev = −0.024 [95% CI: −0.042, −0.006], P = 0.008, I 2 = 96.9%, and 95% prediction interval [−0.066, 0.017]) (Figure 2B), and severe anxiety alone (ΔPrev = −0.025 [95% CI: −0.047, −0.003], P = 0.025, I 2 = 93.3%, and 95% prediction interval [−0.071, 0.021]) (see Supplementary Table S6). As reported in Supplementary Figure S3D,F, in the analyses of data from early pandemic, potential publication bias was detected for severe anxiety and depression combined and severe depression alone (Egger’s test P-value = 0.001 and 0.011, respectively; and trim-and-fill analysis results also suggested that the asymmetry in the corresponding funnel plots was likely related to publication bias). No potential publication bias was seen for other outcomes. Influence analyses revealed no indication that individual study, if omitted, would significantly influence the observed pooled estimates (see Supplementary Note S5).
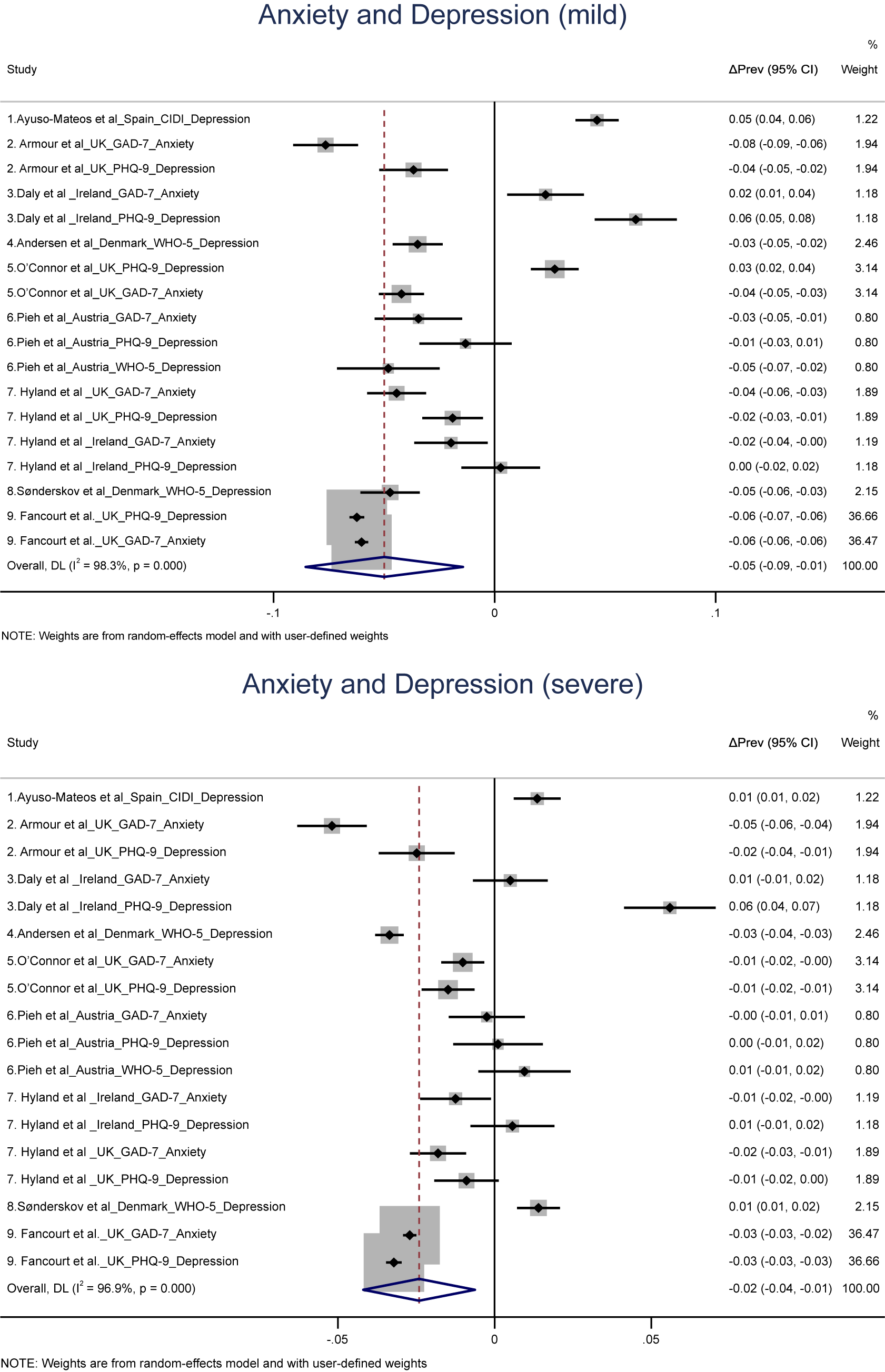
Figure 2. (A) Forest plot of random-effects meta-analysis results on early to during-pandemic changes in the prevalence of mild anxiety and depression. (B) Forest plot of random-effects meta-analysis results on early to during-pandemic changes in the prevalence of severe anxiety and depression. The results of individual studies and the pooled results are reported as the average early-to-during difference in the prevalence (ΔPrev) and its 95% confidence intervals (95% CI).
Changes in the prevalence of mild and severe anxiety and depression stratified by age and sex
None of the analyzed age and sex groups displayed significant pre–during pandemic changes in the prevalence of mild or severe depression or anxiety (combined or alone) (see Supplementary Table S6), and the results remained the same in the analysis when the dataset with children only [Reference Widnall, Winstone, Mars, Haworth and Kidger24] was removed (data not shown). Among studies with data from early pandemic, there were minor, but significant changes in the prevalence from early to during pandemic among the following age and sex groups: Among 19–64-year-olds, there was a significant decrease in mild depression and anxiety combined (ΔPrev = −0.059 (95% CI: −0.106, −0.013), P = 0.012; I 2 = 98.6%; and 95% prediction interval [−0.171, 0.052]). The significant decreases in mild depression and anxiety combined were found among males (ΔPrev = −0.039 [95% CI: −0.074, −0.004], P = 0.029; I 2 = 96.7%; and 95% prediction interval [−0.119, 0.041]) as well as females (ΔPrev = −0.059 (95% CI: −0.099, −0.019), P = 0.004; I 2 = 97.33%; and 95% prediction interval [−0.154, 0.035]), as was the decrease in mild anxiety among males (ΔPrev = −0.039 [95% CI: −0.073, −0.004], P = 0.029; I 2 = 89.9%; and 95% prediction interval [−0.111, 0.034]) and among females (ΔPrev = −0.070 (95% CI: −0.112, −0.028), P = 0.001; I 2 = 92.4%; and 95% prediction interval [−0.160, 0.020]). In addition, females in age group 65+ also reported a significant decrease in mild anxiety and depression combined (ΔPrev = −0.037[95% CI: −0.069, −0.005], P = 0.023; I 2 = 89.6%; and 95% prediction interval [−0.111, 0.036]) (see Supplementary Table S9). Moreover, with regard to severe depression and anxiety combined, there were significant decreases from early to during pandemic among 19–64-year-olds (ΔPrev = −0.031 [95% CI: −0.057, −0.005], P = 0.020; I 2 = 97.8%; and 95% prediction interval [−0.094, 0.032]) and among females (ΔPrev = −0.031 [95% CI: −0.051, −0.012], P = 0.002; I 2 = 94.6%; and 95% prediction interval [−0.078, 0.015]). Also, there were significant decreases in severe depression among females aged 0–18 (ΔPrev = 0.173 [95% CI: −0.325, −0.021], P = 0.026; I 2 = 88.4%; no prediction interval measures due to small number of studies). For detailed results, see Supplementary Tables S7–S10.
Changes in the prevalence of mild and severe anxiety and depression from pre to during pandemic stratified by country
Among the studies with pre-pandemic data, country-specific analyses revealed no overall changes in the prevalence of mild or severe depression and anxiety combined. Among studies with early pandemic data, country-specific analyses revealed an overall decrease in mild depression and anxiety combined in the UK (ΔPrev = −0.056 [95% CI: −0.082, −0.029], P = 0.000; I 2 = 97.7%; and 95% prediction interval [−0.120, 0.008]) and Austria (ΔPrev = −0.056 [95% CI: −0.082, −0.029], P = 0.000; I 2 = 97.7%; and 95% prediction interval [−0.120, 0.008]) and an overall decrease in severe depression in the UK (ΔPrev = −0.028 [95% CI: −0.038, −0.018], P = 0.000; I 2 = 91.6%; and 95% prediction interval [−0.120, 0.008]) (see Figure 3A,B).

Figure 3. (A) Forest plot of random-effects meta-analysis results on early to during-pandemic changes in the prevalence of mild depression and anxiety, stratified by country. (B) Forest plot of random-effects meta-analysis results on early to during-pandemic changes in the prevalence of severe depression and anxiety, stratified by country. The results of individual studies and the pooled results are reported as the average early-to-during difference in the prevalence (ΔPrev) and its 95% confidence intervals (95% CI).
Relationship between changes in the prevalence of mild and severe anxiety and depression with social distancing and school restrictions
The results in the following are reported as meta-regression coefficients for the change in the prevalence of anxiety and depression (coeff.), where the beta estimate denotes the effect 1-unit change in index has on the proportion of change in the outcome. Analyses are conducted for datasets with pre- and early pandemic data together. Through the meta-regression, we found that changes in school restrictions were significantly and positively associated with changes in the prevalence of mild anxiety and depression combined (coeff. = 9.41 × 10−5; P = 0.038). School restrictions and social distancing measures were not significantly associated with severe levels of anxiety and depression combined, or alone (Table 2). Additional adjustment for study quality did not alter the results (see Supplementary Table S11).
Table 2. Meta-regression coefficients for the change in the prevalence of anxiety and depression in relation to changes in social distancing and school restrictions for the COVID-19 pandemic

Note: For the analysis, data from both pre-to-during and early-to-during pandemic were used together.
Discussion
This meta-analysis examined changes in mild and severe CMD prevalence rates in eight European countries from before/early pandemic to during the COVID-19 pandemic. The findings indicate no significant changes in the prevalence of mild/severe depression and/or anxiety when assessed from pre-pandemic to during the pandemic. However, among studies with data from early pandemic, significant decreases in the prevalence were found for mild anxiety and depression combined, mild anxiety alone, severe anxiety and depression combined, and severe anxiety alone. Similar results were also observed for specific age, sex, and national subgroups. Another finding was the positive association between school restrictions and mild depression and anxiety combined and between social distancing and mild depression, though with small effects.
Our findings diverge from previous studies of changes in CMD during the initial stages of the pandemic, which mainly suggested that there was an increase in the prevalence of major depressive disorder and generalized anxiety disorder [3, Reference Santomauro, Mantilla Herrera, Shadid, Zheng, Ashbaugh and Pigott12, Reference Jacob, Tully, Barnett, Lopez-Sanchez, Butler and Schuch46, Reference Cardona, Andersen, Fallesen and Bruckner47]. However, unlike previous studies that typically relied on single threshold values for depression and anxiety prevalence [Reference Widnall, Winstone, Mars, Haworth and Kidger24, Reference Pieh, Budimir, Humer and Probst35, Reference Pieh, Budimir and Probst36], the present study utilized two separate thresholds (i.e., mild and severe). Moreover, the longer follow-up periods of the included studies have allowed us to study additional nuances in these changes and associations.
Indeed, in our study mild anxiety and depression decreased across various demographic groups and most countries from early to during the pandemic. This aligns with findings from the UK, where clinically diagnosed anxiety and depression decreased over time as pandemic restrictions eased [Reference Fancourt, Steptoe and Bu30]. Several explanations could account for this. It is possible that many were not significantly impacted by the pandemic in the longer term [Reference Butter, Murphy, Hyland, McBride, Shevlin and Hartman48] and the initial rise in anxiety and depression seen in the early pandemic literature reflects short-term changes. Another explanation may be that individuals developed resilience as the pandemic progressed and it became the “new normal” [Reference Prati and Mancini49]. Additionally, our findings are paralleled by two other meta-analyses of studies with pre-pandemic to during pandemic data that found no changes in the prevalence of a broader range of mental disorders and symptoms after mid-2020, although there was an initial increase in the prevalence at the start of the pandemic [Reference Robinson, Sutin, Daly and Jones14, Reference Sun, Wu, Fan, Dal Santo, Li and Jiang15].
Our study indicated that increased school restrictions were associated with small increases in mild depression and anxiety combined, and increased social distancing was associated with small increases in mild depression. This is in line with a meta-analysis of 25 studies that associated lockdown measures with increases in depression and anxiety [Reference Prati and Mancini49]. Also, studies have found increased distress levels in parents and children due to school closures [Reference Spinelli, Lionetti, Pastore and Fasolo50, Reference Ludwig-Walz, Dannheim, Pfadenhauer, Fegert and Bujard51], possibly resulting from the challenges of balancing personal life, work, and children at home, which can hinder their ability to provide adequate support and contribute to psychological symptoms among children [Reference Spinelli, Lionetti, Pastore and Fasolo50]. However, our findings contrast with a study across 33 countries, which found that the prevalence of depression was significantly lower in countries with promptly implemented stringent restrictions [Reference Lee, Lui, Chen-Li, Liao, Mansur and Brietzke52], but our study assessed prevalence at later time points, when restriction measures had already been implemented for an extended time.
Strengths and limitations
This meta-analysis has allowed us to assess the effect of the COVID-19 pandemic on CMDs in the European population. Relatively homogenous healthcare systems with universal access across European countries enables valuable multinational comparisons, considering their varied containment strategies for COVID-19. Another strength of our study was that we collected raw or aggregated data from the study authors, which allowed for fewer restrictions to the data analysis in comparison to if we had only relied on data that were reported in the published studies.
There are several limitations to this study. Our objective to assess CMD at two levels required the use of raw/aggregated data. This took us long time to obtain, which in turn constrained our capacity to conduct a systematic literature search in several databases within a reasonable time frame. However, the limiting of our search allowed us to access and work with raw/aggregated data from the included studies, which is a strength that may in part outweigh the limitation of the search being non-systematic. The data are unweighted, so the results may not accurately represent the population being studied, and pre-/early and during demographics are thus not necessarily comparable. Moreover, we chose to define the pre-pandemic period as any time point up until March 2020. This definition of our pre-pandemic time point may impact comparability of our results with other studies using different time points. The choice of date for pre-pandemic periods in our study however will not affect the results regarding associations between lockdown measures and outcomes. Finally, it is noteworthy that all results presented large heterogeneity, which may be due to several possible confounding factors that vary between studies and settings, such as disparities of populations, heterogeneity of the outcomes measures used, and differences of the healthcare systems and policies implemented in the different countries. Therefore, the generalizability of the present findings is limited, and additional studies are needed to better understand how pandemic restrictions affect CMD.
Conclusion
This study suggests that as the COVID-19 pandemic progressed in Europe, there was a decline in mild forms of emotional distress when compared to the initial increase in early pandemic, while rates of depression and anxiety remained stable. When comparing to pre-pandemic prevalence, however, there was no change. However, increased school restrictions and social distancing were found to be associated with small increases in mild anxiety and depression but not in severe levels. These findings support the importance of strong governance when implementing periodic and robust restriction measures to combat the spread of COVID-19.
Registration and protocol
The study protocol has been registered and can be accessed on PROSPERO, with registration number CRD42022343130.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1192/j.eurpsy.2023.2467.
Acknowledgments
We would like to acknowledge all data providers who have not been listed as co-authors, for contributing data to this work. These include Sarah Butter and Richard Bentall from the COVID-19 Psychological Research Consortium (C19PRC); Christoph Pieh from the Department of Psychosomatic Medicine, University of Continuing Education Krems; Mark Ward from the Irish longitudinal study on Ageing, Trinity College, Dublin, Ireland; Violetta Parutis from the UK Understanding Society COVID-19 study, University of Essex, United Kingdom; Elvira Lara from the Department of Psychiatry, Hospital Universitario de La Princesa, Madrid, Spain; Mark Shevlin from the Department of Psychology, Ulster University, Ireland; Peter van der Velden from the Tilburg School of Social and Behavioral Sciences, Tilburg University, the Netherlands; Søren Dinesen Østergaard from the Department of Clinical Medicine, Affective Disorders, Aarhus University, Denmark; Andrew Jones from the Department of Economics and Related Studies, University of York, United Kingdom; Matthias Pierce from the Division of Psychology and Mental Health, University of Manchester, United Kingdom; and Eugenio Proto form the Adam Smith Business School, University of Glasgow, United Kingdom, Rory O’Connor form the School of Health and Wellbeing, University of Glasgow, United Kingdom; Daisy Fancourt and Bu Feifei from the Institute of Epidemiology and Health, University College London, United Kingdom; and Peter Winkler and Marie Kuklova from the National Institute of Mental Health, Czech Republic. This project was part of the European Commission Horizon 2020-funded project “a Pan-European Response to the ImpactS of COVID-19 and future Pandemics and Epidemics” - Periscope.
Author contribution
Conceptualization: C.D., P.F., M.N., A.S.; Data curation: V.L., M.N., P.F.; Formal analysis: V.L., H.S., M.N.; Funding acquisition: C.D., M.N., W.O.; Investigation: V.L., M.N., P.F.; Methodology: A.S., H.S., P.F., M.N., M.D., P.H., L.H.A., PFallesen, M.C.C., A.K.S.K., K.W., E.W., J.M.G., C.A.; Project administration: A.-C.H., C.D., W.O., M.N.; Resources: C.D., M.N., W.O.; Supervision: A.-C.H., C.D., P.F., M.N.; Writing – original draft: V.L., M.N.; Writing – review and editing: All authors.
Financial support
Funding for this research was provided through the Horizon 2020 research and innovation program (V.L, P.F., C.D., A-C.H., W.O., M.N., grant number 101016233), Nuffield Foundation; UK Research and Innovation; Wellcome Trust (D.F. F.B.); ROCKWOOL Foundation (L.H.A., PFallesen, M.C.C., grant number 1227); Swedish Research Council for Health, Working Life and Welfare (PFallesen, grant number 2016-07099), and NIHR School for Public Health Research (EW grant reference number PD-SPH-2015). The funder had no role in the design, completion, or writing up of the study.
Competing interest
None declared.








Comments
No Comments have been published for this article.