Introduction
It remains unclear whether the coronavirus disease 2019 (COVID-19) pandemic is having an impact on suicide rates (SR). Some predict that SR will rise, since actions to contain COVID-19, such as social distancing, economic lockdown or the temporary restructuring of the health system, could cause risk factors for suicide to increase (Fitzpatrick et al., Reference Fitzpatrick, Harris and Drawve2020; Kawohl and Nordt, Reference Kawohl and Nordt2020; Wand et al., Reference Wand, Zhong, Chiu, Draper and de Leo2020; McIntyre and Lee, Reference McIntyre and Lee2020a, Reference McIntyre and Lee2020b). Indeed, analyses of previous economic crises have shown that an increase in unemployment was associated with an increase in SR (Nordt et al., Reference Nordt, Warnke, Seifritz and Kawohl2015; Oyesanya et al., Reference Oyesanya, Lopez-Morinigo and Dutta2015; Rachiotis et al., Reference Rachiotis, Stuckler, McKee and Hadjichristodoulou2015; Alicandro et al., Reference Alicandro, Malvezzi, Gallus, La Vecchia, Negri and Bertuccio2019; Huikari et al., Reference Huikari, Miettunen and Korhonen2019). According to leading theories of suicide prevention, the loss of social inclusion is a major risk factor for suicide (van Orden et al., Reference van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010). However, it has not yet been clarified whether social cohesion decreased during the pandemic as a result of physical distance or increased, as has been observed during other existential threat scenarios (Durkheim, Reference Durkheim1867/1951; Wasserman, Reference Wasserman1992; Wasserman et al., Reference Wasserman, van der Gaag and Wise2020).
While some studies on previous epidemics found an increase in SR in particular age groups (Wasserman, Reference Wasserman1992; Cheung et al., Reference Cheung, Chau and Yip2008; Chang et al., Reference Chang, Chang, Hsu and Gunnell2020; Leaune et al., Reference Leaune, Samuel, Oh, Poulet and Brunelin2020; Zortea et al., Reference Zortea, Brenna, Joyce, McClelland, Tippett, Maxwell, Arensman, Corcoran, Hatcher, Heise, Links, O'Connor, Edgar, Cha, Guaiana, Williamson, Sinvor and Platt2020), the evidence base for suicide risk during the COVID-19 pandemic is very limited (Niederkrotenthaler et al., Reference Niederkrotenthaler, Gunnell, Arensman, Pirkis, Appleby, Hawton, John, Kapur, Khan, O'Connor and Platt2020). An initial high-quality study showed no indications of an increase in SR in the early phase of the COVID-19 pandemic in Australia (Leske et al., Reference Leske, Kõlves, Crompton, Arensman and de Leo2020) and a study analysing state-level data from Connecticut found a higher proportion of ethnic minorities among suicide cases during the COVID-19 lock-down compared to preceding years (Mitchell and Li, Reference Mitchell and Li2020). Studies using indirect measures for suicide risk during the pandemic provided inhomogeneous results (Gratz et al., Reference Gratz, Tull, Richmond, Edmonds, Scamaldo and Rose2020; Halford et al., Reference Halford, Lake and Gould2020; Knipe et al., Reference Knipe, Evans, Marchant, Gunnell and John2020; Patsali et al., Reference Patsali, Mousa, Papadopoulou, Konstantina, Kaparounaki, Diakogiannis and Konstantinos2020; Sinyor et al., Reference Sinyor, Spittal and Niederkrotenthaler2020).
In Germany, as in other countries, significant restrictions were imposed to contain the COVID-19 pandemic with the strongest restrictions coming into force between 22 March and 5 June.
German borders were virtually closed for travel from 16 March onwards (Federal Ministry of the Interior, 2020a, 2020b, 2020c). On 22 March 2020, the German Federal Government and the Länder agreed on a comprehensive restriction of social contacts, which required people to reduce contacts with others (except for members of one's own household) to an absolute minimum (German Federal Government, 2020a). By closing educational and child care facilities, religious sites, all cultural facilities, sports and leisure facilities, hotels, gastronomic establishments and most shops, as well as by prohibiting private gatherings, public and social life was shut down (Free State of Saxony, 2020; German Federal Government, 2020b). Between 4 May and 5 June, contact restrictions were extended to persons from two households.
From 6 June 2020 on, the severe restrictions on going out were eased (Sächsische Staatskanzlei, 2020) and as June progressed, extensive freedom of movement within the EU's Schengen Area was gradually restored, but differentiated travel warnings and quarantine regulations following travel remained in place for parts of it until the end of September 2020 (Federal Foreign Office, 2020).
This study investigated suicide trends during the COVID-19 pandemic and the influence of social distancing during the COVID-19 restrictions on SR. We addressed the following hypotheses:
SR increased in the total population under severe COVID-19 restrictions of social contact compared to periods without or with moderate restrictions.
An interrupted time series analysis shows an increase of suicide risk during the COVID-19 pandemic compared with the time period before onset of the pandemic.
Methods
Sample and data acquisition
The data on suicides in this study are based on the City of Leipzig's cause of death statistics, and were provided by the responsible health authority for the years 2010−2020. Annual population statistics were provided by the residents' registration office of Leipzig (https://statistik.leipzig.de/statcity/).
In Germany, physicians determine the cause of death and, if it is uncertain, a medical autopsy may be conducted. The health authorities receive the death certificate and the results of potential autopsies in order to compile statistics on the causes of death. At the time of the investigation, all autopsies had been completed and the causes of death for the cases included had been conclusively determined. However, the total number of suicides may change slightly, e.g. if currently missing persons are found dead at a later date.
Analytical strategy
Data were analysed using the R software version 3.3.1 (R Core Team, 2016), IBM SPSS 25.0 (IBM Corp., 2019) and Microsoft Excel.
The analysis includes all suicides between January 2010 and September 2020.
For the year 2020, days without restrictions on freedom of movement or social contact were aggregated as period nR_2020 (1 January−16 March), those with moderate restrictions as period R1_2020 (travel restrictions; 17−21 March and 6 June−30 September), and those with severe restrictions as period R2_2020 (restrictions on travel, going out and social contact; 22 March−5 June). To compare suicide mortality in 2020 before and during the COVID-19 restrictions, suicide cases were assigned to groups nR_2020, R1_2020 and R2_2020. Corresponding life years (LY) were calculated, according to the length of the periods examined.
LY and suicide events were used to calculate the risk ratios (RR). Differences in suicide risk among groups nR_2020, R1_2020 and R2_2020 were conducted using chi-square tests.
The suicide risk during the COVID-19 pandemic (March 2020−September 2020) was compared with the suicide risk of the pre-COVID-19 period (January 2010−February 2020). Since the SRs in Germany have been declining in recent years (Alicandro et al., Reference Alicandro, Malvezzi, Gallus, La Vecchia, Negri and Bertuccio2019), an interrupted time series analysis was performed to control for underlying linear trends and seasonal fluctuations. This approach has been used in previous publications (Chang et al., Reference Chang, Chang, Hsu and Gunnell2020).
Due to overdispersion in the data, we performed a negative binomial regression analysis to identify suicide trends in the pre-COVID-19 period, with annual log-transformed population sizes as offset variable. Seasonal effects were adjusted by defining dummy variables for each calendar month. In a second step, expected suicides for each month of the COVID-19 period were calculated based on the identified time trends.
To examine whether SR during the COVID-19 pandemic were out of line with the time trend of previous years, expected and observed suicides of the COVID-19 period were compared by calculating incidence rate ratios and 95% confidence intervals.
Ethical considerations
The study was approved by the ethics committee of the medical faculty of the University Hospital Leipzig, Germany (study ID: 272/20-ek) and conducted in accordance with the Declaration of Helsinki. This epidemiological cohort study is based on the death statistics. For methodological reasons, no informed consent can be obtained.
Results
A total of 6 032 690 LY were spent and 643 suicides were registered during the periods studied. In 2020, 21 suicides (LY: 124 937) were attributed to nR_2020, 23 (LY: 200 556) to R1_2020 and 9 (LY: 124 937) to R2_2020. The SR within the individual periods were 16.8, 11.5, 7.2 in nR_2020, R1_2020, and R2_2020, respectively.
The suicide risk in 2020 was found to be different between nR_2020 and R2_2020 (χ 2 [1; N = 249 903] = 4.033, p = 0.045). Comparisons of nR_2020 with R1_2020 (χ 2 [1; N = 325 537] = 1.253, p = 0.263) and R1_2020 and R2_2020 (χ 2 [1; N = 325 525] = 1.023, p = 0.312) were not significant (see Table 1).
Table 1. Suicide risk before and during COVID-19 restrictions

Suicide numbers, person years (LY) and suicide rates (SR, suicides per 100 000 LY) during investigated periods of 2020 without, with moderate and severe COVID-19 restrictions.
The time series analysis showed that monthly suicide numbers in the pre-COVID-19 period decreased by 0.3% per month (IRR = 0.997, p = 0.028) and the calendar months modulated this linear time trend with an IRR between 0.922 and 1.275 (see Figs 1, 2a). According to the extrapolation of the time trend in 2020, 32.3 expected suicides were calculated for the COVID-19 period March−September 2020 and 35 suicides were observed. The observed versus expected differences were not significant (IRR = 1.084, CI 95% = [0.665, 1.766], p = 0.682). Expected and observed suicides of the individual months in 2020 are shown in Fig. 2b.
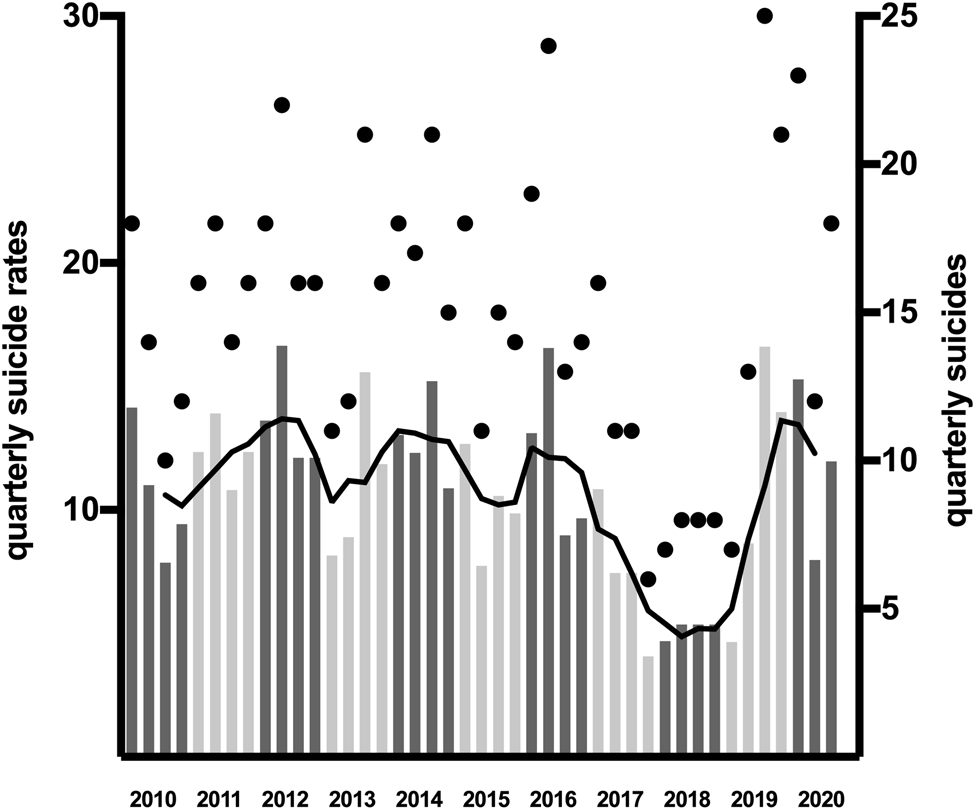
Fig. 1. Quarterly suicides and suicide rates from 2010 to 2020. For each quarter of the years 2010 to 2020, the suicide rate (barchart), 12-month moving average (black line) and the number of suicides (black dots) are shown.
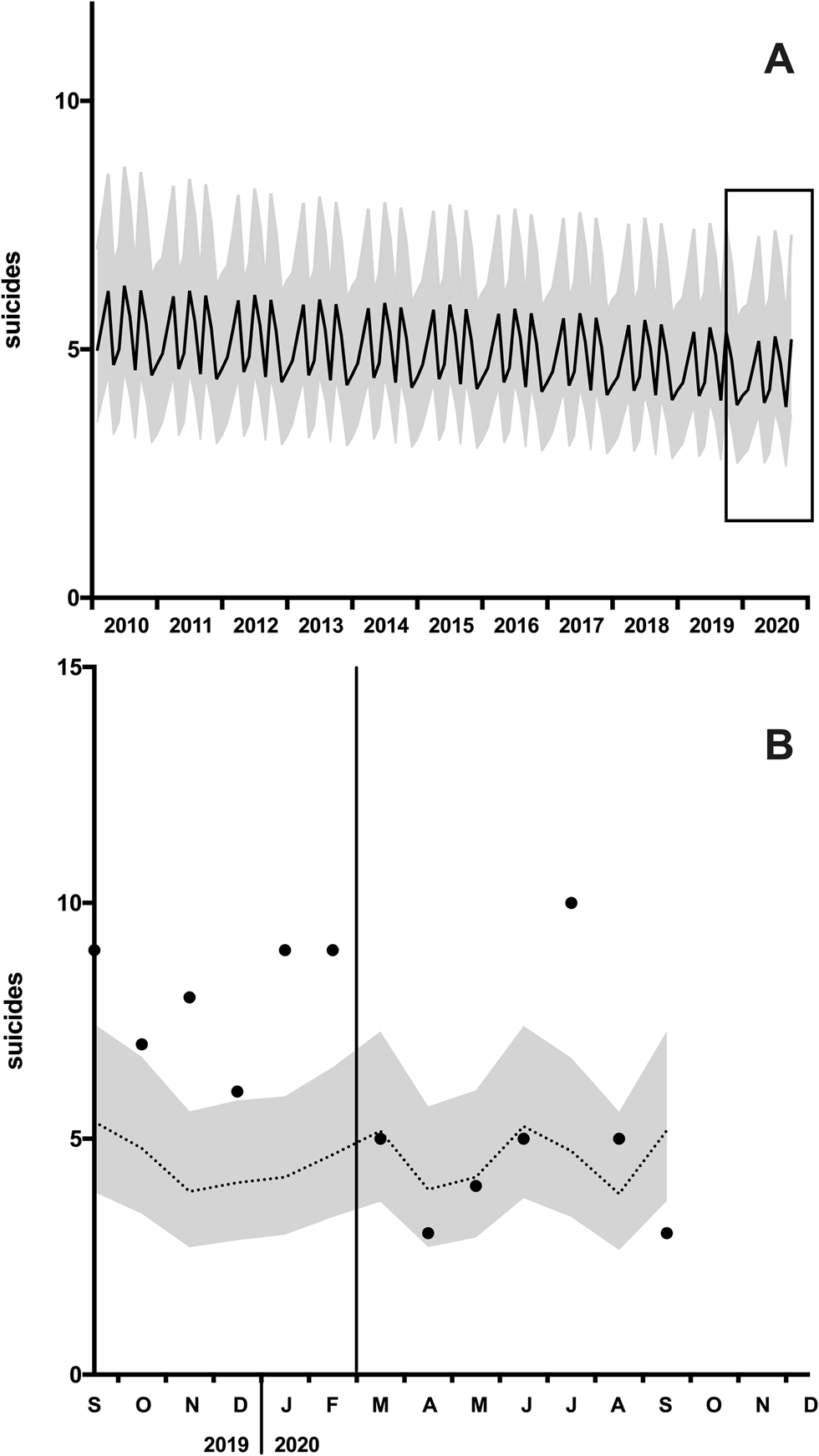
Fig. 2. Suicide time trends. (A) Expected suicides (black line) and the 95% confidence interval (95% CI, grey corridor) based on the time series analysis of suicides in 2010 to 2019. The rectangle indicates the section shown below. (B) Projection of expected suicides (doted line), 95%CI and observed suicides (dots) of the individual months.
Discussion
Our hypotheses regarding SR increasing during COVID-19 restrictions could not be confirmed. The time series analysis revealed that SR during the restrictions were in line with the trend in previous years. In 2020, lower SR were found during severe restrictions compared to the time interval before the restrictions, but this difference was due to unexpectedly high SR in January and February.
The results represent local suicide trends during the COVID-19 pandemic in a major city in Saxony with about 600 000 inhabitants. In Saxony, as in most regions of Germany, the prevalence and mortality rates of COVID-19 were comparatively low during the first wave of the pandemic, with 135.8 and 251.0 cases per 100 000 inhabitants, respectively (Robert Koch Institut, 2020). The regional shut-down was much less restrictive than in other European countries, e.g. United Kingdom, France, Spain and Italy. At an early stage of the pandemic, the German government committed to supporting measures to prevent insolvencies and unemployment. Accordingly, results should be evaluated under these external conditions. Regional differences in the COVID-19 pandemic may produce regional differences in the mental health situation, economic crises and SR. The findings of this study should not, therefore, be extrapolated uncritically to other regions or countries. It should not be assumed either that the trend described will remain stable. This study only provides a first regional snapshot.
The unexpectedly high SR in January and February 2020 are probably unrelated to the pandemic, as they represent a continuation of high SR in 2019 (see Fig. 1). SRs were lowest during the most severe restrictions. Restrictions on going out may act as barriers to outdoor suicide methods, and a person's physical presence at home could strengthen family members' awareness of one another.
Although contact restrictions may contribute to loneliness and a reduced sense of belonging in the medium term, it is suggested that during external threat scenarios, such as war or terrorist attacks, the feeling of social cohesion increases temporarily, and may lead to reduced SR (Durkheim, Reference Durkheim1867/1951; Claassen et al., Reference Claassen, Carmody, Stewart, Bossarte, Larkin, Woodward and Trivedi2010). A heightened sense of social cohesion was also registered at the beginning of the COVID-19 pandemic, which found expression in public concern for at-risk groups and the question of how to maintain social inclusion despite the imperative of physical distance (Wasserman et al., Reference Wasserman, van der Gaag and Wise2020). However, the study design did not allow us to examine which influencing factors were effective during the restrictions. Future studies are needed to examine how restrictions affect individual risk factors for suicide.
Some studies investigated the association between infectious diseases and suicide risk (Wasserman, Reference Wasserman1992; Cheung et al., Reference Cheung, Chau and Yip2008; Chang et al., Reference Chang, Chang, Hsu and Gunnell2020; Leaune et al., Reference Leaune, Samuel, Oh, Poulet and Brunelin2020; Zortea et al., Reference Zortea, Brenna, Joyce, McClelland, Tippett, Maxwell, Arensman, Corcoran, Hatcher, Heise, Links, O'Connor, Edgar, Cha, Guaiana, Williamson, Sinvor and Platt2020). Two studies focused on the impact of severe acute respiratory syndrome on SR in Hong Kong and found higher SR in the elderly (Chan et al., Reference Chan, Chiu, Lam, Leung and Conwell2006; Cheung et al., Reference Cheung, Chau and Yip2008). Two studies found an increase of SR during the influenza pandemic of 1918–1920 in the United States (Wasserman, Reference Wasserman1992) and in Taiwan (Chang et al., Reference Chang, Chang, Hsu and Gunnell2020).
There is little evidence of suicide risk during the COVID-19 pandemic. Only one study reports data on SR during the COVID-19 pandemic based on a time series analysis of 3793 suicides in Australia, without any evidence of an increase of suicide risks (Leske et al., Reference Leske, Kõlves, Crompton, Arensman and de Leo2020). A second study analysing state-level data on suicide mortality from Connecticut reported decreasing SR and overrepresentation of ethnic minorities among suicide cases during the COVID 19 quarantine conditions compared with preceding years (Mitchell and Li, Reference Mitchell and Li2020).
Projections based on underlying risk factors for suicide, such as unemployment, indicate rising SR during the COVID-19 pandemic (McIntyre and Lee, Reference McIntyre and Lee2020a, Reference McIntyre and Lee2020b). This does not contradict our findings of our study, since although unemployment rose during the COVID-19 pandemic, it remained at a low level during the first months of the pandemic in the region studied (Bundesagentur für Arbeit und Stadt Leipzig, 2020). Our results are consistent with studies reporting no increase in suicidal behaviour, which is used as an indirect measure for suicide risk (Halford et al., Reference Halford, Lake and Gould2020; Hamm et al., Reference Hamm, Brown, Karp, Lenard, Cameron, Dawdani, Lavretsky, Miller, Mulsant, Pham, Reynolds, Roose and Lenze2020; Jacobson et al., Reference Jacobson, Lekkas, Price, Heinz, Song, O'Malley and Barr2020; Knipe et al., Reference Knipe, Evans, Marchant, Gunnell and John2020; Sakelliadis et al., Reference Sakelliadis, Katsos, Zouzia, Spiliopoulou and Tsiodras2020; Sinyor et al., Reference Sinyor, Spittal and Niederkrotenthaler2020; Smalley et al., Reference Smalley, Malone, Meldon, Borden, Simon, Muir and Fertel2020). For instance, online surveys showed a decrease in suicidal thoughts and intention during the pandemic; presentation at emergency departments due to suicidal ideation decreased (Smalley et al., Reference Smalley, Malone, Meldon, Borden, Simon, Muir and Fertel2020), suicides in selective autopsy samples remained low (Sakelliadis et al., Reference Sakelliadis, Katsos, Zouzia, Spiliopoulou and Tsiodras2020), and search engine users entered suicide-related terms less frequently (Halford et al., Reference Halford, Lake and Gould2020; Jacobson et al., Reference Jacobson, Lekkas, Price, Heinz, Song, O'Malley and Barr2020; Knipe et al., Reference Knipe, Evans, Marchant, Gunnell and John2020; Sinyor et al., Reference Sinyor, Spittal and Niederkrotenthaler2020). However, the overall results are inhomogeneous, since other surveys indicate a high prevalence of suicidal thoughts during the pandemic, in particular under quarantine conditions (Fitzpatrick et al., Reference Fitzpatrick, Harris and Drawve2020; Gratz et al., Reference Gratz, Tull, Richmond, Edmonds, Scamaldo and Rose2020; Patsali et al., Reference Patsali, Mousa, Papadopoulou, Konstantina, Kaparounaki, Diakogiannis and Konstantinos2020).
Overall, there is limited evidence on suicide risk during the COVID-19 pandemic. In many countries, including Germany, national cause-of-death statistics are published with a time lag of several months. During the COVID-19 pandemic, however, up-to-date data are needed to adapt prevention strategies. To facilitate this, the more rapidly available regional data should be published and evaluated in meta-analytical approaches. A platform for this is for example provided by the International COVID-19 suicide prevention research collaboration (ICSPRC) (Gunnell et al., Reference Appleby, Arensman, Hawton, John, Kapur, Khan, O'Connor, Pirkis, Caine, Chan, Chang, Chen, Christensen, Dandona, Eddleston, Erlangsen, Harkavy-Friedman, Kirtley, Knipe, Konradsen, Liu, McManus, Mehlum, Miller, Moran, Morrissey, Moutier, Niederkrotenthaler, Nordentoft, O'Neill, Page, Phillips, Platt, Pompili, Qin, Rezaeian, Silverman, Sinyor, Stack, Townsend, Turecki, Vijayakumar and Yip2020; International Association for Suicide Prevention; Niederkrotenthaler et al., 2020).
Conclusion
In the population studied, SR were elevated before onset of COVID-19 restrictions, but there was no increase in SR during restrictions. Careful monitoring of SR as the COVID-19 crisis progresses is essential to establish an evidence base for further prevention approaches. The available results represent a step in this direction.
Limitations and strengths
This study reports first data on SR during the COVID-19 pandemic in Germany. The study period in 2020 covers nine months and the population studied is relatively small with 0.6 M persons resulting in low suicides numbers. This may result in differences remaining unidentified due to insufficient statistical power.
These findings allow conclusions to be drawn for the region and time period investigated. The results do not allow a supra-regional evaluation or assessment of medium-term trends in SR.
Data
The paper is based on data provided by the Leipzig Health Authority. These case-related data cannot be published for reasons of data protection. On request, the corresponding author will make aggregated data available to other scientists.
Acknowledgements
We would like to thank the Leipzig Health Authority for their support and fast provision of relevant data sets. We acknowledge support from Leipzig University for Open Access Publishing. We would also like to thank Monica Buckland for her valuable support in proofreading.
Financial support
This study was conducted without external funding.
Conflict of interest
None.





