The ‘ultra-high risk’ (UHR), ‘clinical high risk’ (CHR) or simply the ‘at-risk’ criteria were developed as a useful paradigm for investigating antecedents of the onset of psychosis, specifically schizophrenia. This ‘close-in’ strategy identifies young people who might be in the prodromal phase of a psychotic illness by combining known state and trait risk factors for psychotic illness (Yung & McGorry, Reference Yung and McGorry1996). Since these criteria were first operationalized at the Personal Assessment and Crisis Evaluation (PACE) clinic in Melbourne, centres worldwide have adopted similar criteria, with some variation [e.g. Scheduled Interview for Prodromal Symptoms/Scale of Prodromal Symptoms (SIPS/SOPS) Miller et al. 2003], in an attempt to better predict the onset of psychosis. At PACE, the Comprehensive Assessment of At-Risk Mental States (CAARMS; Yung et al. Reference Yung, Yuen, McGorry, Phillips, Kelly, Dell'Olio, Francey, Cosgrave, Killackey, Stanford, Godfrey and Buckby2005) is used to rate the UHR status of young people at the age of peak risk for psychosis based on the criteria of: (1) attenuated psychotic symptoms; (2) brief limited intermittent psychotic symptoms (BLIPS); and/or (3) trait vulnerability for psychotic illness (schizotypal personality disorder or a history of psychosis in a first-degree relative), and deterioration in functioning or chronic low functioning.
The at-risk criteria predict the onset of frank psychotic disorder at a rate that is several hundred times higher than that of the general population (Yung et al. Reference Yung, Phillips, Yuen, Francey, McFarlane, Hallgren and McGorry2003, Reference Yung, Phillips, Yuen and McGorry2004). This group therefore represents an excellent population in which to study psychological, neurocognitive, neurobiological and genetic risk factors for psychotic illness. However, not all young people identified as being at-risk will develop psychotic disorder. Early findings from centres around the world showed that the transition rate from at-risk state to frank psychosis over a 1-year period was ~ 36% (Ruhrmann et al. Reference Ruhrmann, Schultze-Lutter and Klosterkötter2003). This has been declining in recent years, a phenomenon documented at the PACE clinic (Yung et al. Reference Yung, Yuen, Berger, Francey, Hung, Nelson, Phillips and McGorry2007) and recently verified in a review (Simon et al. Reference Simon, Velthorst, Nieman, Linszen, Umbricht and de Haan2011) and a meta-analysis (Fusar-Poli et al. Reference Fusar-Poli, Bonoldi, Yung, Borgwardt, Kempton, Valmaggia, Barale, Caverzasi and McGuire2012). Fusar-Poli et al. (Reference Fusar-Poli, Bonoldi, Yung, Borgwardt, Kempton, Valmaggia, Barale, Caverzasi and McGuire2012) found that the average transition rate is now ~ 22% at 1-year post-identification as at-risk, 29% at 2 years and 36% at 3 years. This means that about two-thirds of young people meeting at-risk criteria do not develop frank psychotic illness in the medium term, but very little is known about the outcome of this group of ‘non-transitioned’ cases.
Defining the psychosis threshold
The relative outcomes of transitioned and non-transitioned cases must be considered with the understanding that the threshold at which psychotic symptoms progress from attenuated to frank ‘psychotic disorder’ is arbitrary. That is, it was originally based on the level of positive symptoms at which clinicians felt anti-psychotic medication was indicated. This highlights the subjective clinical judgement involved in determining the point at which the prodrome ends and frank psychosis begins. The progression to psychotic disorder may not be smooth; symptoms may fluctuate in intensity and frequency in the progression towards psychosis. Degree of insight may also fluctuate, as could the patient's attribution of the source of the experiences (Yung & McGorry, Reference Yung and McGorry1996). The arbitrary nature of the psychosis threshold is clearly reflected in the different levels of symptoms (and interpretation of those symptoms) that constitute the threshold for psychosis on the CAARMS and on the SIPS/SOPS. According to CAARMS criteria, a person must experience at least one fully positive psychotic symptom for over 1 week to be deemed as having transitioned to psychosis (Yung et al. Reference Yung, Yuen, McGorry, Phillips, Kelly, Dell'Olio, Francey, Cosgrave, Killackey, Stanford, Godfrey and Buckby2005). ‘Schizophrenic psychosis’ is defined on the SIPS/SOPS as at least one fully positive psychotic symptom four times a week for at least 1 month or at least one fully psychotic symptom for at least 1 day if the symptom is seriously disorganizing or dangerous (Miller et al. Reference Miller, McGlashan, Rosen, Cadenhead, Ventura, McFarlane, Perkins, Pearlson and Woods2003). On the one hand, the SIPS/SOPS threshold for psychosis onset is higher than the CAARMS. However, if a judgement is made by the clinician that a symptom is dangerous or disorganizing, then the threshold is far lower. This highlights the arbitrary nature of the point at which a patient is deemed as having progressed from an at-risk to a frankly psychotic state.
This arbitrary threshold has been the primary or target outcome in at-risk research. That is, researchers have been interested in whether a person is psychotic or not by the time of follow-up assessment. Specifically, at-risk groups have been divided by the level of the positive psychotic symptoms that they develop in the search for markers of schizophrenia. However, it is possible that the current threshold is meaningless in terms of the functional and neurobiological changes associated with psychosis (Yung et al. Reference Yung, Nelson, Thompson and Wood2010). Although there are some neurobiological data suggesting that the threshold may be approximately correct (for a review, see Correll et al. Reference Correll, Hauser, Auther and Cornblatt2010), it is possible that a different threshold could be ‘more correct’. It is also possible that the dichotomous approach to the onset of psychosis may have little validity at all. There appears to have been a premature acceptance of the validity of the psychosis threshold as operationalized to date and as a result, these questions have not been investigated.
Another problem associated with the use of this arbitrary division is that assumptions are made about the similarity or dissimilarity of various trajectories of positive symptoms. For example, dividing at-risk patients into two groups (psychotic/not psychotic) essentially assumes that a person who experiences a brief prodrome, short psychotic episode, and quick symptomatic and functional recovery is the same as the person with an extended prodrome and chronic schizophrenia characterized by negative symptoms, cognitive impairment and functional disability (see Fig. 1). Similarly, using the current model, a young person who has never had any psychotic experiences is assumed to be equivalent to another who continues to present with attenuated psychotic symptoms and functional impairment, but who never progresses over the threshold of frank psychosis (see Fig. 1). Clearly, this is not correct. We know that many young people who transition to psychosis experience a rapid symptomatic and functional recovery, which Yung et al. (Reference Yung, Nelson, Thompson and Wood2010) termed ‘trivial transitions’. In fact, we have found that a significant proportion of at-risk young people who developed psychosis and received a diagnosis of schizophrenia did not meet the diagnostic criteria for a psychotic disorder when asked to report on their symptoms since treatment at the PACE clinic (a median of 6.7 years previously). There is also evidence that many who never transition continue to experience functional impairment, negative symptoms (and possibly attenuated positive psychotic symptoms) many years after being identified as at-risk (Lin et al. Reference Lin, Wood, Nelson, Brewer, Spiliotacopoulos, Bruxner, Broussard, Pantelis and Yung2011). It is currently unclear which of these presentations is most representative of ‘true schizophrenia’, but this has major implications for the search for vulnerability markers of the illness. These data argue for an alternative perspective on outcome, which includes other psychopathology, functional disability and negative symptoms, rather than relying solely on the intensity/frequency of positive symptoms defined at the arbitrary level.
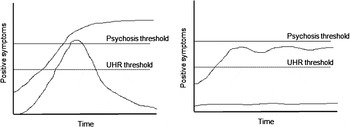
Fig. 1. Trajectories of positive psychotic symptoms over time.
Other outcomes of interest
Non-psychotic disorders
There is a dearth of research on diagnostic outcomes other than psychotic disorder in the at-risk population. We know that a majority of young people who meet at-risk criteria also meet criteria for non-psychotic disorders (e.g. Velthorst et al. Reference Velthorst, Nieman, Becker, van de Fliert, Dingemans, Klaassen, de Haan, van Amelsvoort and Linszen2009; Woods et al. Reference Woods, Addington, Cadenhead, Cannon, Cornblatt, Heinssen, Perkins, Seidman, Tsuang, Walker and McGlashan2009). However, there are only a few reports on the rates of non-psychotic disorders in patients who have not developed psychosis by follow-up assessment (McGorry et al. Reference McGorry, Yung, Phillips, Yuen, Francey, Cosgrave, Germano, Bravin, McDonald, Blair, Adlard and Jackson2002; Haroun et al. Reference Haroun, Dunn, Haroun and Cadenhead2006; Lam et al. Reference Lam, Hung and Chen2006; Addington et al. Reference Addington, Cornblatt, Cadenhead, Cannon, McGlashan, Perkins, Seidman, Tsuang, Walker, Woods and Heinssen2011). These studies show that depression and anxiety are common outcomes. Only the North American Prodrome Longitudinal Study (NAPLS) Consortium has published on the prevalence of non-psychotic diagnostic outcomes from a large sample over medium-term follow-up (Addington et al. Reference Addington, Cornblatt, Cadenhead, Cannon, McGlashan, Perkins, Seidman, Tsuang, Walker, Woods and Heinssen2011). They demonstrated a significant decrease in the prevalence of these disorders from baseline to 1-year and to 2-year follow-up. Nevertheless, at 2-year follow-up, 31% of the non-transitioned cases still met criteria for an anxiety disorder and 14% met criteria for depression. This finding suggests that those who do not develop psychosis continue to experience significant mental health problems. Long-term findings from the PACE clinic are similar (paper in preparation). Two-thirds of the non-transitioned sample met criteria for at least one disorder during the follow-up period, with significant comorbidity. In a majority of cases, these young people already had the diagnosis at baseline, meaning the incidence of new non-psychotic disorder was low, while chronicity/recurrence was high. The at-risk criteria may therefore be useful for detecting young people who are at heightened risk for chronic non-psychotic psychopathology, which could be targeted in clinical care. Such outcomes should also be targeted in research. These could include Axis II diagnoses. Importantly, it is likely that predictors of chronic non-psychotic disorders and personality disorders are different to predictors of psychosis, and these variables need to be built into research protocols.
Functional outcome
There is a growing appreciation of the importance of the functional outcome of at-risk samples. Deteriorating or chronically low functioning are now a criterion for at-risk status, and impaired functioning, in particular social functioning, has been found to predict the transition to psychosis (Velthorst et al. Reference Velthorst, Nieman, Linszen, Becker, de Haan, Dingemans, Birchwood, Patterson, Salokangas, Heinimaa, Heinz, Juckel, von Reventlow, French, Stevens, Schultze-Lutter, Klosterkötter and Ruhrmann2010; Cornblatt et al. Reference Cornblatt, Carrión, Addington, Seidman, Walker, Cannon, Cadenhead, McGlashan, Perkins, Tsuang, Woods, Heinssen and Lencz2011). We have recently shown that about 20% of a large at-risk sample from the PACE clinic was functioning very poorly at follow-up, between 2 and 13 years after identification of risk. Of the group with poor outcome, only 17% had a full-time occupation, 35% had completed high school and 19% were in a romantic relationship (Lin et al. Reference Lin, Wood, Nelson, Brewer, Spiliotacopoulos, Bruxner, Broussard, Pantelis and Yung2011). The social and role functioning of at-risk patients who transition to psychosis has been shown to be stable over time compared with the improvement evident in those who do not develop psychosis by follow-up (Addington et al. Reference Addington, Cornblatt, Cadenhead, Cannon, McGlashan, Perkins, Seidman, Tsuang, Walker, Woods and Heinssen2011; Cornblatt et al. Reference Cornblatt, Carrión, Addington, Seidman, Walker, Cannon, Cadenhead, McGlashan, Perkins, Tsuang, Woods, Heinssen and Lencz2011). However, in the PACE sample, 50% of the group with the worst functional outcome had never experienced a frank psychotic episode (Lin et al. Reference Lin, Wood, Nelson, Brewer, Spiliotacopoulos, Bruxner, Broussard, Pantelis and Yung2011), suggesting that even though there may be an overall functional improvement for non-transitioned patients, a significant proportion do not achieve functional recovery. This is consistent with other evidence that the functioning of at-risk individuals may be relatively independent of positive psychotic symptoms (Cornblatt et al. Reference Cornblatt, Carrión, Addington, Seidman, Walker, Cannon, Cadenhead, McGlashan, Perkins, Tsuang, Woods, Heinssen and Lencz2011), such as delusional ideation, grandiosity and perceptual abnormalities (Velthorst et al. Reference Velthorst, Nieman, Linszen, Becker, de Haan, Dingemans, Birchwood, Patterson, Salokangas, Heinimaa, Heinz, Juckel, von Reventlow, French, Stevens, Schultze-Lutter, Klosterkötter and Ruhrmann2010). Together these recent findings provide a strong rationale for considering long-term functioning as an important target outcome in at-risk research.
Negative symptoms
Although functioning may be relatively independent of positive psychotic symptoms, there is evidence that it is closely linked with negative symptoms (Velthorst et al. Reference Velthorst, Nieman, Linszen, Becker, de Haan, Dingemans, Birchwood, Patterson, Salokangas, Heinimaa, Heinz, Juckel, von Reventlow, French, Stevens, Schultze-Lutter, Klosterkötter and Ruhrmann2010; Corcoran et al. Reference Corcoran, Kimhy, Parrilla-Escobar, Cressman, Stanford, Thompson, David, Crumbley, Schobel, Moore and Malaspina2011; Cornblatt et al. Reference Cornblatt, Carrión, Addington, Seidman, Walker, Cannon, Cadenhead, McGlashan, Perkins, Tsuang, Woods, Heinssen and Lencz2011). Despite this, the role of negative symptoms in the at-risk phase has not received adequate attention. The exception here is the RAP programme in New York, in which a clinical high-risk negative state is identified based on these symptoms (Cornblatt et al. Reference Cornblatt, Lencz, Smith, Correll, Auther and Nakayama2003; Lencz et al. Reference Lencz, Smith, Auther, Correll and Cornblatt2004). The lack of research interest in negative symptoms is surprising since these symptoms are described as part of the prodrome (Yung & McGorry, Reference Yung and McGorry1996; Häfner et al. Reference Häfner, Löffler, Maurer, Hambrecht and an der Heiden1999) and social isolation/withdrawal has been shown to be a more common presenting symptom in at-risk samples than attenuated positive symptoms (Lencz et al. Reference Lencz, Smith, Auther, Correll and Cornblatt2004; Iyer et al. Reference Iyer, Boekestyn, Cassidy, King, Joober and Malla2008). Moreover, higher levels of negative symptoms at baseline, such as anhedonia, asociality and withdrawal, have been shown to predict transition to psychotic disorder (Yung et al. Reference Yung, McGorry, McFarlane, Jackson, Patton and Rakkar1996; Mason et al. Reference Mason, Startup, Halpin, Schall, Conrad and Carr2004; Riecher-Rössler et al. Reference Riecher-Rössler, Gschwandtner, Aston, Borgwardt, Drewe, Fuhr, Pflüger, Radü, Schindler and Stieglitz2007; Velthorst et al. Reference Velthorst, Nieman, Becker, van de Fliert, Dingemans, Klaassen, de Haan, van Amelsvoort and Linszen2009; Piskulic et al. Reference Piskulic, Addington, Cadenhead, Cannon, Cornblatt, Heinssen, Perkins, Seidman, Tsuang, Walker, Woods and McGlashan2012). The problem here is that, once again, the primary outcome is the development of (arbitrarily defined) psychosis, and negative symptoms are viewed as predictors. To our knowledge, the presence of negative symptoms at follow-up has never been treated as a specific outcome in at-risk research, even though their presence in established schizophrenia is associated with poorer prognosis (e.g. Fenton & McGlashan, Reference Fenton and McGlashan1994). What we would like to know is whether we can identify which at-risk patients are likely to develop or show persistent negative symptoms and functional disability, regardless of the trajectory of positive symptoms.
Incorporating other outcomes into research
A useful framework for considering functional outcome and negative symptoms in at-risk samples is the CASIS model proposed by Cornblatt et al. (Reference Cornblatt, Lencz, Smith, Correll, Auther and Nakayama2003). In this model, the prodromal period of illness comprises two distinct dimensions. The first is a vulnerability dimension caused by early insult which impacts brain pathology and manifests in adolescence as cognitive deficits, affective disturbances, social isolation, neurocognitive impairment and school failure (CASIS). This vulnerability dimension is stable, viewed as the underlying cause of functional disability and is necessary, but not sufficient, for the development of schizophrenia. The second dimension is positive psychotic symptomatology, which develops in some, but not all, individuals who display signs of CASIS vulnerability. Those who do not become frankly psychotic may continue to demonstrate neurocognitive and functional impairment with poor prognosis. This presentation is hypothesized to represent a schizophrenia subtype that closely resembles other conditions. Cornblatt et al. (Reference Cornblatt, Lencz, Smith, Correll, Auther and Nakayama2003) highlighted similarity to the ICD-10 diagnosis of simple schizophrenia (World Health Organization, 1994) and the concept of schizotaxia as described by Tsuang et al. (Reference Tsuang, Stone, Tarbox and Faraone2002a). It is also consistent with Raine's (Reference Raine2006) hypothesized neurodevelopmental subtype of schizotypal personality disorder or schizotypal disorder as described in the ICD-10 (which is a psychotic disorder rather than a personality disorder). These conditions capture the symptoms of social and physical anhedonia and withdrawal, functional disability, mild positive psychotic symptoms and (in some of these conditions) neurocognitive impairment.
The traditional focus on the development of frank psychosis, regardless of functioning, needs to be reconsidered. With the CASIS model in mind, we suggest the need to consider poor functional outcome, even in the absence of exacerbation of positive psychotic symptoms. Figure 2 shows the level of positive symptoms in relation to level of functioning. There is a large body of literature on those with poor outcome and transition (Area B), who might be viewed as having ‘deficit schizophrenia’ (Carpenter et al. Reference Carpenter, Heinrichs and Wagman1988). However, little is known about the people who transition but experience a good outcome (trivial transitions; Area A), and about those who never cross the psychosis threshold but experience poor outcome (Area C). These groups may be very important, not only from a clinical perspective but also for our understanding of the aetiology of schizophrenia. Investigating trivial transitions (Area A) may be useful for our understanding of recovery and good treatment response. An alternative possibility is that these young people actually represent a different underlying disease process (or aetiological pathway) to those in Area B, who also transition but experience poor functional outcome. It is also possible that young people who never transition but have poor outcome (Area C) may be endophenotypically more closely related to true schizophrenia than the trivial transitions (Area A). It is important to note here that Fig. 2 also uses arbitrary cut-offs for the onset of frank psychosis and functional outcome for the purpose of illustration. A dimensional view may indeed be a more accurate reflection of all these clinical outcomes.
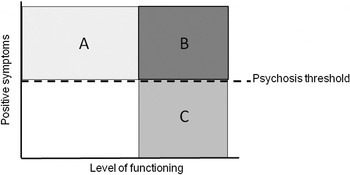
Fig. 2. Positive psychotic symptoms relative to functioning.
If individuals in Areas B and C of Fig. 2 represent a similar aetiological pathway, then at-risk individuals with an outcome consistent with that represented in Area C cannot be viewed as false positives, as they currently are. They are not considered to be unwell and are unlikely to receive ongoing treatment. If, however, they do have a clinically meaningful syndrome, intervention may be beneficial, particularly in reducing their negative symptoms and improving quality of life. There is evidence for the efficacy of low-dose anti-psychotic medication in reducing negative symptoms and improving the quality of life and neurocognitive functioning of people defined as having schizotaxia (Tsuang et al. Reference Tsuang, Stone, Seidman, Faraone, Zimmet, Wojcik, Kelleher and Green1999, Reference Tsuang, Stone, Tarbox and Faraone2002b). Theoretically, psychological interventions, such as teaching coping strategies, cognitive remediation or social cognitive intervention training, should also assist in symptomatic and functional improvement, although trials have not been reported. Intervention of this kind would not take the prevention of psychosis as a primary target but aim to address current functional impairment and negative symptoms, and facilitate compensatory strategies for neurocognitive and social cognitive impairments. The prevention of psychosis may be a secondary outcome. This line of reasoning suggests the need to shift the traditional notion of outcome in at-risk research.
In what direction is at-risk research heading? Predicting psychotic disorder remains an important outcome. However, the at-risk paradigm is proving to be useful in identifying young people who may never develop frank psychotic disorder but are nevertheless very unwell. In this regard, at-risk clinical services provide the perfect opportunity for intervention because the patients are already within the mental health system. Treatment should be broad so as to incorporate poor functioning, negative symptoms and current psychopathology, with awareness that not developing a psychotic disorder does not mean recovery and good outcome. Research should focus on better understanding the antecedents and predictors of these other outcomes.
Answering the call for researchers to consider outcomes other than psychosis raises many questions. What does the psychosis threshold actually mean? How does it relate to prognosis and functional outcome? Should negative symptoms also be considered in the at-risk criteria and in the diagnosis of schizophrenia? Do young people who experience good outcome simply respond better to treatment than those who experience poor outcome? Or does each group represent different underlying disease processes? We believe that these are central questions in the next decade of at-risk research.
Declaration of Interests
Professor Yung has received honoraria and travel support from AstraZeneca, Eli-Lilly, Bristol Meyer Squibb and Janssen-Cilag. Drs Lin and Nelson have nothing to disclose.




