Background
Due to the COVID-19 pandemic, different countries implemented different laws in 2020 to limit people's contacts and therefore COVID-19 transmission [1]. In the UK, the first lockdown implemented on 23/03/2020 legally restricted the movement of people from their place of residence, with movement only being permittable when seeking healthcare, to exercise (alone/with household members), to purchase necessities or to assist vulnerable persons. Subsequently, the laws were eased from 01/06/2020 [2]. However, on 14/09/2020, the guidance was again tightened and then England entered a second lockdown on 05/11/2020, which involved shutting down non-essential shops, working from home where possible, restricting gatherings to two people meeting outside in a public place, but with schools and universities remaining open [3]. Before the second lockdown, some UK areas had restrictions tightened above the national guidance due to higher transmission rates through the implementation of tiers or legislation in devolved nations. However, Bristol and the Southwest of England remained in the lowest tier throughout this period due to the low overall COVID-19 transmission rate [4], meaning that mixing may have been higher throughout the summer and autumn than in other areas of the country.
The first lockdown forced universities to move teaching online [5], including the University of Bristol (UoB). Universities began the 2020/21 term in the autumn, when reported daily COVID-19 cases were rising nationally [6]. Students migrated from around the UK and abroad to attend the new term. Although university students are mostly young and are therefore less likely to be severely affected by COVID-19 morbidity and mortality than other groups, some may still be medically vulnerable [Reference Felsenstein and Hedrich7]. Meanwhile, university staff are more representative of the working-age general population and tend to be older and are therefore more likely to be affected by COVID-19 morbidity and mortality.
For UoB's 2020/21 term, students returned towards the end of September for the first teaching block which ran from 5 October to 15 January. The UoB adopted a ‘blended’ teaching approach, including a mixture of face-to-face and online teaching. To reduce contact numbers, online teaching was offered for lectures across most courses, except those where face-to-face teaching was deemed necessary (e.g. dentistry). Face-to-face teaching was offered for small-group practicals, for which the number of students taught in each session was reduced to protect both students and staff. Students living in university halls of residence were divided into households (‘living circles’) and were instructed not to host non-residents in their flat but government social distancing guidelines applied outside the flat [8]. Students that test positive are required to isolate along with their household [8].
Despite COVID-19 restrictions, outbreaks of COVID-19 occurred across many UK universities during autumn 2020 [Reference Adams, Weale and Pidd9]. For UoB, there were outbreaks among students but few cases amongst staff: UoB reported 1722 positive tests among students from 14/10/2020 to 01/11/2020, roughly 7% of students, compared with 48 positive tests among staff (<1%) [8]. Hundreds of students (mostly first-year undergraduates) in university-owned halls of residence were told to self-isolate during the beginning of term.
There is little evidence to quantify the effect that the various COVID-19 restrictions in the UK have had on the number of contacts of individuals: a key driver of COVID-19 transmission. On 23/06/2020, we launched an online survey detailing the contacts and behaviours of staff and students at the UoB, with the survey continuing into the autumn term. We aimed to investigate whether there were differences in contact patterns for UoB staff and students between the periods before and during the autumn 2020 COVID-19 lockdown, and to quantify these differences.
Methods
CONQUEST (COroNavirus QUESTionnaire) is a survey that started on 23/06/2020 asking about contacts, behaviour and potential SARS-Cov-2 symptoms for staff and students at UoB. Survey participants complete an initial questionnaire including questions on background demographics and then have the option to fill out a shorter, recurring version of the questionnaire on contacts, symptoms and whether they have had COVID-19. The recurring questionnaire was initially every 14 days and then every 8 days as of 13/09/2020 (see Supplementary material for details). It was not possible to advertise the survey to students at the end of the 2019/2020 academic year via direct email and only light touch promotion was granted for social media. The survey was advertised to staff via email and newsletters during June and July 2020. Approval was granted for a larger targeting campaign for students when they returned to the university for the 2020/2021 academic year in September. Here, we present the data up to 25/11/2020.
Survey
Survey data were collected using UoB's REDCap Electronic Data Capture [Reference Harris10, Reference Harris11]. The initial survey (see Supplementary materials) captured demographic information on participants and asked about symptoms in the last 7 days, whether they had sought medical attention for these symptoms, whether they had been self-isolating in the last 7 days, and their COVID-19 status.
Participants were asked about contacts they had had on the previous day, which were split into three types:
1. Individual contacts: those who they spoke to in person one-on-one, including those in their household and support bubble.
2. Other contacts: if they spoke in person to many people one-on-one in the same setting (but they did not have the opportunity to speak to each other), for example, as part of working in a customer service role in a shop.
3. Group contacts: large groups of individuals in the same setting (e.g. sports teams, tutorials, lectures, religious services, large gatherings with friends and family).
Further information on the questions asked about each of these contact types is given in the Supplementary materials along with the full questionnaire. On 13/09/2020, amendments were made to the questionnaire (see Supplementary material).
We excluded responses where the survey was incomplete. We only include respondents that live in the Southwest of England as this region (including Bristol) remained in the UK government COVID-19 tier-1 throughout the existence of these tiers during the study period.
COVID-19 guidance periods
Table 1 presents key COVID-19 guidance implementation dates and dates relating to the CON-QUEST survey. The periods of COVID-19 restrictions were stratified as follows:
• Post-first lockdown: Survey start (23/06/2020) to the day before the second, more lenient set of COVID-19 regulations were implemented (03/07/2020).
• Relaxed period: second COVID-19 regulations implementation (04/07/2020) to the day before the fourth set of COVID-19 laws were implemented (13/09/2020).
• ‘Rule-of-six’ period: fourth COVID-19 regulations (14/09/2020) to the day before the second lockdown (04/11/2020).
• Second lockdown: second lockdown start (05/11/2020) to data cut-off (25/11/2020).
Table 1. List of key events relating to COVID-19 restrictions and the CON-QUEST survey around the study period [24]

Analyses
To make the dataset more representative of UoB's staff and student populations, weighting was used, described further in the Supplementary materials.
We investigated the associations between the overall number of contacts on the previous day with demographics and behaviours using univariable and multivariable negative binomial regression modelling, stratified for staff and students. All variables included in these models are presented in the relevant results tables, with variables chosen a priori. Note that cardinal symptoms are defined as loss of taste or smell, fever, persistent cough [12] and all postgraduates were assigned to the 4+ year group to differentiate them from undergraduates in their first year of study.
Analyses were performed in Stata version 16.1.
Ethical approval
Ethical approval was granted on the 14/05/2020 by the Health Sciences University Research Ethics Committee at the UoB (ID 104903), with four amendment requests approved on the 22/05/2020, 09/06/2020, 27/08/2020 and 07/09/2020 to update the relevance of the questions or to make the survey faster and easier to complete. All research was performed in accordance with the University of Bristol Ethics of Research Policy and Procedure (http://www.bristol.ac.uk/media-library/sites/red/documents/research-governance/Ethics_Policy_v8_03-07-19.pdf). Participants were aged ≥18, voluntarily opted-in to the study and were required to give their informed consent before starting the survey.
Data availability
Pseudonymised data will be made available from the corresponding author upon request.
Results
Included over the entire survey period were 722 staff, with repeat questionnaires leading to 4199 responses, whilst for students there were 738 participants and 1906 questionnaire responses. The median ages of the staff and students were 42 (interquartile range (IQR): 34–51) and 22 (IQR: 19–25), respectively. The median household size for staff was 2 (IQR: 1–3; mean: 2.6) and 3 for students (IQR: 2–5; mean: 4.5). Most staff participants were recruited between 23/06/2020 and 13/09/2020 (95.3%), whilst 20.7% of students were recruited between these dates (Table 2). Due to the communications campaign, most students (78.0%) were recruited between 14/09/2020 and 04/11/2020, whilst 4.3% of staff were recruited during this period. In the weighted analyses, there were 1623 staff responses between 14/09/2020 and 04/11/2020 and 628 from 05/11/2020 to 24/11/2020. For the students, these numbers were 1314 and 333, respectively.
Table 2. Characteristics of survey participants and responses (unweighted and weighted)

Variation in contacts over time
Figure 1 shows the mean, median and IQR of the number of contacts reported on the previous day, stratified by week. For staff, among whom there were high response numbers throughout the entire analysis period, the median number of contacts rose from 2 during the post-first lockdown period to 3 during the relaxed guidance and ‘rule-of-six’ periods and reduced to 2 during the second lockdown period. Similarly, the mean number of daily contacts for staff rose from 3.2 (95% confidence interval (95% CI) 2.8–3.5) during the post-first lockdown period to 4.4 (95% CI 3.9–4.9) during the relaxed guidance period, 5.4 (95% CI 4.6–6.1) during the ‘rule-of-six’ period and dropped to 3.3 (95% CI 2.8–3.8) during the second lockdown period.
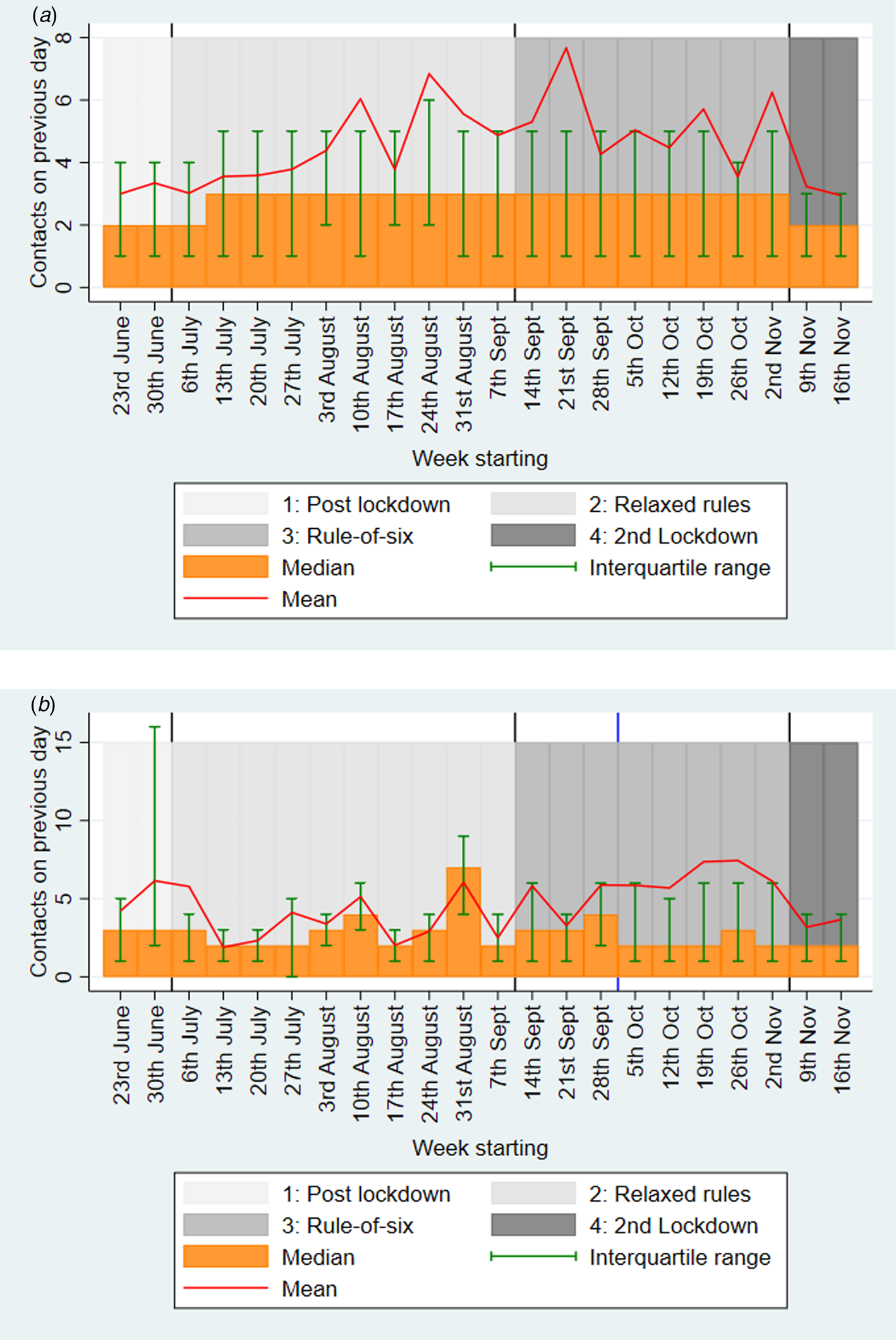
Fig. 1. Weighted mean and median (with interquartile ranges) number of contacts for the previous day, stratified by week for (a) staff; and (b) students. For students, the blue line indicates the start of the mass communications campaign*. *Mass communications campaign for students began the week of 5 October and ended in November.
For students, after 05/10/2020, when there were high numbers of responses leading to clearer interpretation, the median daily contacts was 2 and the mean was around 6.2 (95% CI 5.5–6.9), until the introduction of the second lockdown when it dropped to 4.0 (95% CI 3.3–4.7).
For both staff and students, there was a large difference in the mean and median contacts, as some individuals had large numbers of contacts (see Fig. 2). Supplementary Table S2 shows that there were lower numbers of survey responses at the weekend, but the reported number of contacts was similar for each day. Supplementary Figure S1 shows a histogram of contacts, stratified by staff and students.

Fig. 2. Weighted histograms of the number of contacts on the previous day for staff in (a) the ‘rule-of-six’ period (14 September–4 November) before the second lockdown; and (b) for the second lockdown period (5 November–25 November); and the same graphs, respectively for students: (c) and (d). *There were 60/1659 records for staff in the ‘rule-of-six’ period with more than 20 contacts, 11/635 in the second lockdown period, whilst for students, there were 78/1171 in the ‘rule-of-six’ period, and 6/363 in the second lockdown period.
Contacts in ‘rule-of-six’ period vs. second lockdown
Figure 2 shows that there was a shift towards higher proportions of both staff and students having lower contacts in the second lockdown period than in the ‘rule-of-six’ period. Table 3 compares the number of contacts and types of these contacts for staff and students during the ‘rule-of-six’ and second lockdown periods. For staff, the mean overall contacts dropped from 5.4 to 3.3, with a large part of this drop being driven by group contacts falling from a mean of 2.1 to 0.7 (this includes those with 0 group contacts). The mean individual contacts of staff dropped from 2.8 to 2.3, but there was a similar number of these contacts involving touch in both periods (1.4 and 1.3), similar mean numbers of household member contacts (1.4 and 1.4), frequent contacts (1.5 and 1.5) and contacts made at home (1.6 and 1.7). Staff had similar numbers of contacts made at the university over both periods (means 0.5 and 0.5) and similar numbers of UoB contacts (0.8 and 0.7). The mean number of contacts made at locations other than home and university dropped for staff between the two periods, from 2.9 to 1.2.
Table 3. Overall weighted number of contacts on the previous day and types of contacts for ‘rule-of-six’ and second lockdown COVID-19 restriction guidance periods, stratified by staff and students

a This question asks whether the majority of the group work or study at the University of Bristol. If this was answered ‘yes’, then we assume here that all members of the group are University of Bristol contacts, if not then we assume that none are.
*‘Individual’ contacts were the people that the participant spoke to in person one-on-one, including those in the participant's household and support bubble. ‘Group’ contacts were the contacts that the participant had with large groups of individuals in the same setting (e.g. sports teams, tutorials, lectures, religious services, large gatherings with friends and family). ‘Other’ contacts were the many people participants spoke to one-on-one in the same setting where the contacts did not have the opportunity to speak to each other (e.g. as part of a customer service role in a shop). Not all of the contact types were asked for each category of contacts, so are only comparable to the associated categories indicated here.
For students, the mean overall number of contacts dropped from 6.2 during the ‘rule-of-six’ period to 4.0 during the second lockdown. Between these two periods, mean individual contacts dropped slightly from 2.3 to 2.0, group contacts dropped from 2.6 to 1.3 and other contacts dropped from 1.3 to 0.6. The mean number of student contacts involving touch was lower than for staff but was consistent across both periods (0.8 and 0.8). Students reported a similar mean number of household member contacts over both periods (1.5 and 1.4) as staff, as well as similar numbers of frequent contacts (1.5 and 1.4), and contacts made at home (1.7 and 1.6). Students had higher mean numbers of contacts made at the university across the two periods than staff (1.1 and 1.0). Students also had higher mean numbers of UoB contacts than staff; however, these dropped between the two periods from 3.5 to 2.5, whilst contacts at locations other than home or university were lower than for staff and dropped between the two periods from 2.2 to 0.9.
Groups larger than six
Figure 3 shows the proportion of respondents that met with groups larger than six on the previous day for each guidance period. For staff, the proportion was lowest in the post-first lockdown period (0.01; 95% CI 0.00–0.02) and then rose in the relaxed guidance period (0.03; 95% CI 0.02–0.04) and again in the ‘rule-of-six’ period (0.06; 95% CI 0.05–0.07), before falling during the second lockdown (0.03; 95% CI 0.01–0.04). For students, there is large uncertainty in the first two periods due to a lack of responses, but the proportion reporting meeting with groups larger than six dropped between the ‘rule-of-six’ period (0.12; 95% CI 0.10–0.14) and the second lockdown period (0.07; 95% CI 0.04–0.10), although this was higher than for staff.

Fig. 3. Weighted proportion of respondents that met with groups larger than six on the previous day, stratified by staff and students, and by COVID-19 guidance period*. *Defined as group contacts of more than six for a single group.
Regression of daily contact numbers
Table 4a contains the results of the regression analyses on the number of contacts on the previous day for staff. In multivariable analysis, the number of contacts was higher in the ‘rule-of-six’ period than in the other periods. Being aged ≥65 was associated with a lower number of contacts in comparison with the 25–44 age group, whilst males reported lower numbers of contacts than females (adjusted incidence rate ratio (aIRR) 0.91; 95% CI 0.85–0.98). Staff reporting symptoms during the previous week had a higher number of contacts on the previous day than those without symptoms, aIRR 1.20 (95% CI 1.10–1.30), whilst those with cardinal symptoms had fewer contacts, aIRR 0.65 (95% CI 0.47–0.90). Staff that had been isolating during the previous week had lower contacts on the previous day, aIRR 0.49 (95% CI 0.38–0.63), whilst staff that were in high-risk health status groups had higher contacts, aIRR 1.29 (95% CI 1.11–1.50). Compared with staff living in a household of 2–3 people, staff with a household size of one had fewer contacts, aIRR 0.68 (95% CI 0.62–0.74), whilst staff with a household of 4–5 people had more contacts, aIRR 1.35 (95% CI 1.24–1.48). Compared with staff that had never tested positive or thought they had never been positive, staff that had previously tested positive more than 2 weeks before the survey had lower numbers of contacts on the previous day, aIRR 0.43 (95% CI 0.24–0.77).
Table 4. Weighted univariable and multivariable regression of the number of contacts on the previous day for (a) staff and (b) students

IRR, incidence rate ratio; s.d., standard deviation; CI, confidence interval.
For students, the regression analysis results are shown in Table 4b. Similarly to staff, the ‘rule-of-six’ period was associated with a higher number of contacts on the previous day than the other periods in the multivariable analysis. Higher age was associated with a lower number of contacts on the previous day. Unlike for staff, males had a higher number of contacts on the previous day than females, aIRR 1.14 (95% CI 1.02–1.27). Postgraduates reported a lower number of contacts than undergrads, aIRR 0.56 (95% CI 0.45–0.71), whilst students in study year 1 had lower numbers of contacts than students in other years. As with staff, students reporting symptoms during the last week had higher numbers of contacts on the previous day than those not reporting symptoms, aIRR 1.23 (95% CI 1.09–1.38), and those isolating during the last week had fewer contacts than those that had not been isolating, aIRR 0.62 (95% CI 0.51–0.74). For students, there was no difference in daily contacts by household size. Students living in catered halls reported fewer contacts on the previous day than those living in a shared house/flat, aIRR 0.65 (95% CI 0.45–0.95), whilst those living with their family had higher contacts than those in shared houses/flats, aIRR 1.36 (95% CI 1.10–1.67). Students living alone had lower numbers of contacts than those living in a shared house/flat, aIRR 0.42 (0.31–0.56). Students that previously suspected themselves to be positive more than 2 weeks before taking the survey reported higher numbers of contacts on the previous day than those that had never tested positive nor suspected themselves of having COVID-19, aIRR 1.38 (95% CI 1.18–1.60).
Discussion
For both the university staff and students, the number of contacts on the previous day was higher in the ‘rule-of-six’ period than in the post-first lockdown period, the relaxed guidance period and the second lockdown.
For staff, contacts remained low throughout the analysis period, rising between the post-first lockdown period (median: 2, mean: 3.2), the relaxed guidance period (median: 3, mean: 4.4), the ‘rule-of-six’ period (median: 3, mean: 5.4), and dropping during the second lockdown (median: 2, mean: 3.3). The difference between the median and means is due to some individuals reporting many contacts. The drop in mean contacts between the last two periods for staff was mostly driven by a mean reduction in contacts in locations other than home or university (from 2.9 to 1.2), including group contacts (from 2.1 to 0.7), whilst there was a similar number of household member contacts between both periods (1.4 and 1.4) and those made at the university (0.5 and 0.5). This indicates that staff members reduced their numbers of social contacts and mostly remained in contact with their household members.
For students, there were few responses until October when a mass communications campaign was launched, after which, the number of contacts on the previous day remained low, the median was 2 and the mean was 6.2 during the ‘rule-of-six’ period, dropping to 4.0 in the second lockdown. It is possible that student contact numbers before and during the autumn will have been affected by their return to university when their social patterns and activities would likely have been different and teaching resumed.
The lower median contacts during the early weeks of term for students than staff was perhaps due to a high percentage of students having to isolate: both students and staff that were isolating had lower numbers of contacts than those not isolating. The drop in mean number of contacts for students between the last two periods was driven by a reduction in all contact types except for those made at home (1.7 to 1.6), which, similarly to staff, indicated a reduction in social contacts. Students also had higher mean numbers of UoB contacts than staff; however, for students, these dropped between the two last periods from 3.5 to 2.5.
For both staff and students, the proportion meeting with groups larger than six dropped between the ‘rule-of-six’ period and the second lockdown period, although was higher for students than for staff. A study [Reference Williams13] suggests that in the COVID-19 pandemic, in contrast to previous research on adherence to non-pharmaceutical interventions in a pandemic [Reference Teasdale14], that there have been high levels of adherence even when individuals believe themselves to be at comparatively low risk from the disease to other groups. This is seen in our study where students were highly compliant with the regulations during various COVID-19 regulation periods, despite most students being in a low-risk age group. Where students were meeting with groups larger than six during the rule-of-six period, this could have been due to exemptions for sports groups, teaching group sizes or students living in large households. Alternatively, these could reflect non-adherence to regulations, with the main barriers to adherence in students having been previously identified as a fear of mental health impacts and loneliness [Reference Blake15]. It must be noted that compliance related to hygiene has been found to be uniformly distinct from compliance related to social distancing behaviours and that treating public health compliance as one construct can lead to poorer prediction of compliance behaviour and poorer production of effective recommendations for public health [Reference Williams13]. Therefore, the compliance to social distancing regulations we found here may not indicate that there has been similar compliance to hygiene practices in staff and students during the COVID-19 pandemic.
The regression models also found that contacts for both staff and students were highest in the rule-of-six period, but other interesting multivariable associations were noted. Among staff, the number of contacts appeared to decrease with age, possibly due to those in older age groups being more cautious as they would likely be at higher risk. However, staff in high-risk groups due to comorbidities had higher numbers of contacts than those not in high-risk groups, although the actual difference was not large (5.1 vs. 4.5), suggesting that more study of this is required. Larger household sizes appeared to correlate with higher contacts for the well-populated household size groups, showing the outsized role that household contacts play in the overall contact numbers. Male staff had lower contact numbers than female staff, which could be due to a variety of reasons including female staff being more likely to work in fields with more face-to-face contact. Staff reporting any COVID-19 symptoms in the previous week had higher contacts than those not reporting symptoms, whilst those reporting cardinal symptoms had fewer contacts, which possibly reflects the pattern of events leading to self-isolation – those isolating within the previous week also had lower contacts. The results regarding those previously or recently testing positive for COVID-19 are difficult to interpret due to low numbers.
Among students, males had higher numbers of contacts than females, possibly reflecting different levels of caution between the genders, although contacts were lower for males among staff. Postgraduates had lower contact numbers than undergraduates, although contact numbers appeared the lowest for first years – possibly due to the high prevalence of self-isolation in halls where most first-year students reside. The same patterns seen in staff regarding symptoms and isolating were seen among students. However, there was some weak evidence that those with cardinal symptoms in the previous week had higher contacts. There appeared to be little evidence of differences in contact numbers between household sizes for students, perhaps indicative of different social mixing patterns for households of different sizes. For the residence type variable, students living alone reported the lowest numbers of contacts, whilst the responses from students living in catered halls suggested they had lower numbers of contacts than those in other residence types. This may be explained by high numbers of students self-isolating in halls of residence at this time. In the multivariable regression model, students living with their family or in self-catered halls appeared to have higher numbers of contacts than those living in a shared house/flat, but the actual differences in the means were small (shared house/flat: 5.9; live with family: 5.7; self-catered halls: 6.2).
Comparison with other literature
For each guidance period studied, we found a lower mean number of daily contacts among our staff and student populations than was found in the pre-COVID-19 era Warwick social contacts survey from 2009 [Reference Danon16, Reference Danon17], either among their entire sample (26.8) or the students in that sample (29.9). The students in the Warwick survey had more home contacts (3.5) than other participants (2.3), whilst most contacts for students (82%, 95% CI 79–86%) were either at home or university-related. Students reported 20 (95% CI 14.1–28.8) university-related contacts. Similarly, we found that a high percentage of the contacts of students were either at home or university (~72%) and that our staff (comparing with the Warwick survey's ‘other participants’) had 1.6 home contacts. However, we found that students had a daily mean of 1.7 contacts at home and 2.5 university contacts, possibly indicating that the national and university guidance was successful in reducing contacts. Meanwhile, the POLYMOD social contacts survey [Reference Mossong18] found a lower mean than Warwick social contacts survey (11.7) in their Great Britain sample (average age ~30), but still much higher than the mean values we recorded for either staff or students. The BBC Pandemic project reported the number of daily contacts from a national study in 2018, with a mean of 10.5 [Reference Klepac19], also much higher than we reported.
The CoMix study found during the first COVID-19 lockdown 24–29 March that mean contacts were 2.8 among their general population participants [Reference Jarvis20], comparable to the 3.0 contacts among staff during the second lockdown period in our study. The COVID-19 Contact Network (CoCoNet) Study was conducted between 28 July and 14 August in the general population, with preliminary findings suggesting a mean of 2.9 daily non-household contacts per person [21]. Similarly, we report 0.5 contacts in the university among staff and 2.9 in non-home, non-university settings in the ‘rule-of-six’ period.
Strengths and limitations
The strengths of this survey include the sample size, longitudinal format and anonymous nature that enabled us to capture self-reported contact patterns of a large number of staff and students during a key period in the UK's COVID-19 pandemic. It provides a unique data source on student and staff behaviour during the pandemic for informing public health action and mathematical models. Results for students are likely generalisable to other UK city-based universities, and to some city-based universities in other countries. Meanwhile, the staff results are likely generalisable to a working cohort of the general population, due to their age profile. Survey questions were designed to be comparable to existing contact surveys [Reference Danon16–Reference Mossong18].
However, the survey started after the first lockdown period, so we are unable to compare whether contacts during the second lockdown were higher than in the first. Also, we cannot ascertain what caused the changes in numbers of contacts. We lack student data for the early period of the survey, as data collection could not be scaled up until October; therefore, we only have robust data on students from October onwards. Additionally, those with many contacts or with little available time may have been deterred from completing it, which may mean it is not representative. There were 7683 responses in dataset, 529 were dropped due to having an incomplete background questionnaire, with 613 responses dropped due to having an incomplete questionnaire on COVID-19 and contacts. Of these 613, 540 filled out the question regarding whether they felt they had had COVID-19, but only 120 of these included information on contacts, which indicated that the majority stopped filling the survey out during the section on COVID-19 symptoms and behaviours. We included clear instructions defining ‘contacts’ in the survey; however, people may have interpreted the instructions differently leading to variation in what people considered a contact to be.
Selection bias for people particularly engaged in health-seeking behaviours may have occurred. However, we did capture individuals reporting large numbers of contacts. There will inevitably be issues regarding recall bias, and issues with response bias, leading to inaccurate or false responses. The implementation of different tiers throughout England (and differing COVID-19 guidance in Scotland, Wales and Northern Ireland) may affect the generalisability of these results, as Bristol and the Southwest remained in the lowest restriction tier 1 throughout this period, so mixing may have been higher than in other areas of the country where stricter guidance was in place.
Implications
This study comes at a unique time when a lockdown has been implemented to reduce contacts between individuals. However, the number of reported daily cases of COVID-19 is still high [6]. Bristol went into the second lockdown covered by this study in the lowest tier of COVID-19 restrictions and came out (as with much of the country) in the highest tier, with a third lockdown then implemented in 2021 [4]. UoB, as with many other UK universities, is preparing to manage a possible mass migration event of its students back to university when the current lockdown is relaxed, with the potential for COVID-19 transmission to escalate due to enhanced population mixing [Reference Brooks-Pollock22]. The setting is important due to its uniqueness, as universities were allowed to carry on teaching throughout the lockdown, meaning that some mixing between households still occurred [3], whilst the setting is also generalisable, as university staff are likely relatively representative of many working-age populations in age structure, enabling us to estimate the difference in contacts between students and the general population. It is important to be able to understand the effect of the COVID-19 guidance changes, particularly lockdowns, on people's behaviour for any future pandemics that could occur. We show that on average there was high adherence to the guidance throughout the survey period for both staff and students, despite students receiving negative media coverage during the pandemic [Reference Ng23]. The average number of contacts remained low throughout the study and few people were meeting groups larger than six, despite many students living in large households and attending lectures. Students had slightly higher numbers of overall contacts than staff during the ‘rule-of-six period’; however, there was a reduction in the number of contacts during the second lockdown for both groups, returning them to levels in the periods after the first UK lockdown. This was primarily driven by a reduction in social contacts, whilst daily household contact numbers remained steady between these two periods.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0950268821001618
Acknowledgements
We would like to thank the Elizabeth Blackwell Institute for funding this research, our RedCap data manager Alison Horne and our PPI group for their feedback during the development of the survey. We would also like to thank all the participants who have taken part in this study.
Author contributions
AT and EN wrote the first draft of the manuscript. EN and EBP organised data collection, whilst AT analysed the data. HC, AF, ATh, CR, CM, GH, JM, JGW, KT, RK, SS, EBP and LD designed analyses, interpreted the results and critically reviewed the manuscript.
Financial support
This study was funded and supported by the Elizabeth Blackwell Institute. HC, AF, KT and EBP would like to acknowledge support from the National Institute for Health Research (NIHR) Health Protection Research Unit (HPRU) in Behavioural Science and Evaluation at the University of Bristol. HC is additionally funded through an NIHR Career Development Fellowship (CDF-2018-11-ST2-015). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. CR is a member of the MRC Integrative Epidemiology Unit and receives support from the MRC (MC_UU_00011/5) and the University of Bristol. ATh is supported by Wellcome (217509/Z/19/Z). EBP, EN and LD are supported by UKRI through the JUNIPER consortium (grant number MR/V038613/1). LD and EBP are further supported by MRC (grant number MC/PC/19067). LD acknowledges funding from EPSRC (EP/V051555/1 and The Alan Turing Institute, grant EP/N510129/1).
Conflict of interest
HC has received research funding from Sanofi Pasteur, IMS Health, AstraZeneca and GSK unrelated to this research. JGW has received research funding from Gilead Sciences unrelated to this research. All other authors declare no competing interests.










