INTRODUCTION
Hungarian obstetrician Dr Ignaz Phillip Semmelweis (1 July 1818–13 August 1865) was the first to identify the mode of transmission of puerperal sepsis (childbed fever). Although Semmelweis's troubled history has been detailed by Nuland [Reference Nuland and Semmelweiss1], Carter [Reference Carter and Codell2], Loudon [Reference Loudon3, Reference Loudon4] and Waller [Reference Waller5, Reference Nuland6], to our knowledge, no one has attempted an appropriate statistical analysis of Semmelweis's data available since 1861 [Reference Semmelweis7, Reference Semmelweis8]. Here we attempt to correct this.
From those data, analysed with standard statistical methods (see Appendix 1), we have created Figures 1–3 which track the changes in annual maternal mortality between 1784 and 1858 in the Maternity Hospital in Vienna, the Allgemeines Krankenhaus (AKH), at which Semmelweis studied and worked, first as a medical student from 1837 until April 1844; then from 1 August 1844 until 27 February 1846 as aspirant Assistant to the Professor of Obstetrics Johann Klein. Subsequently he worked as Provisional Assistant to Professor Klein until 1 July 1846 whereafter he was appointed Assistant in Obstetrics to Professor Klein on a 2-year contract. This was withdrawn temporarily between 20 October 1846 and 20 March 1847, prior to his reinstatement for a further year.

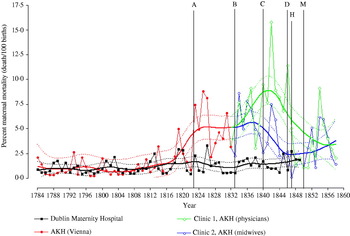
Fig. 1. Percent maternal mortality in the Dublin Maternity Hospital (1784–1849) and in the Allgemeines Krankenhaus (AKH) (Vienna) (1784–1848). A, January 1823, Appointment of Professor Johann Klein as Professor of Obstetrics in charge of the AKH. B, January 1833, Obstetric services at the AKH split into Clinics 1 and 2. 95% confidence band, smoothing parameter=0·35.
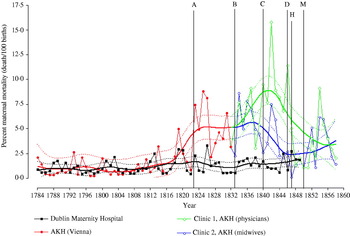
Fig. 2. Percent maternal mortality in the Dublin Maternity Hospital (1784–1848) and in the Allgemeines Krankenhaus (AKH) (Vienna) (1784–1858). A, January 1823, Appointment of Professor Johann Klein as Professor of Obstetrics in charge of the AKH. B, January 1833, Obstetric services at the AKH split into Clinics 1 and 2. C, 19 October 1840, Staffing at the AKH split by gender with males (physicians) in Clinic 1 and females (midwives) in Clinic 2. D, 27 February 1846, Semmelweis promoted to provisional Assistant in Clinic 1. H, Late May, Semmelweis introduces chlorine washings to Clinic 1. M, 15 October, Semmelweis leaves Vienna for Budapest. Appointed honorary Senior Physician at St Rochus Hospital. 95% confidence band, smoothing parameter=0·35.

Fig. 3. Monthly maternal mortalities in Clinics 1 and 2 at the Allgemeines Krankenhaus (AKH) between January 1846 and December 1852. D, 27 February 1846, Semmelweis promoted to provisional Assistant in Clinic 1. E, 1 July, Semmelweis promoted to Assistant in Clinic 1. F, 20 October, Semmelweis replaced by Dr Franz Breit who ‘seldom visited the morgue’. G, March, Death of Professor Jacob Kolletschka from septicaemia. 20 March, Reappointment of Semmelweis as Assistant in Clinic 1. H, Late May, Semmelweis introduces chlorine washings to Clinic 1. I, October, Patient with medullary carcinoma of the uterus treated in Clinic 1. J, November, Patient with ‘carious knee’ treated in Clinic 1. K, March, Height of uprising against the Hapsburg Monarchy spreads to Vienna. Clinical teaching at the AKH is suspended. For the first month ever, no mother dies of puerperal sepsis. L, March, Semmelweis's contract expires. Dr Carl Braun appointed as Aspirant to Professor Klein in Clinic 1. M, 15 October, Semmelweis leaves Vienna for Budapest. Appointed honorary Senior Physician at St Rochus Hospital.
At the termination of his contract in March 1849, Semmelweis's application for reappointment was denied causing him to leave for Budapest on 15 October 1850. On 21 May 1851 Semmelweis was appointed Honorary Senior Physician in the Obstetrics Division at St Rochus Hospital in Budapest where he worked until July 1855. Thereafter he was appointed Professor of Theoretical and Practical Midwifery at the University of Pest, a position he held until July 1865 when his deteriorating mental state caused his institutionalization.
Semmelweis died on 13 August 1865, 2 weeks after his admission to the ward for maniacs at the Lower-Austrian Mental Home in Vienna. An extensive abscess in the anterior chest wall that perforated into the thoracic cavity, reaching the pericardium caused his death [Reference Nuland6]. The source of the infection were ‘wounds inflicted when he was forcibly restrained by the attendants at the mental home – that he was, in effect, beaten to death’ [Reference Semmelweis8, p. 58]. His immediate family was party to this tragedy: ‘the fact that Semmelweis was ill-treated despite his social standing, strongly suggests that his death was welcomed, if not prearranged’ [Reference Waller5, p. 157].
MATERIAL AND METHODS
Mean annual percent maternal mortality data were sourced from two publications, Semmelweis I., The Etiology, Concept and Prophylaxis of Childbed Fever (translated by K. Codell Carter) [Reference Semmelweis8], and Semmelweis I., The Etiology, the Concept and the Prophylaxis of Childbed Fever (translated by F. P. Murphy) [Reference Semmelweis7]. Mortality rates, as they appear in the former [Reference Semmelweis8] in tables 1–8 and 11–14 on pages 64, 68, 72, 78, 85, 90, 91, 96, 131, 132, 142 and 143 respectively, were used in statistical comparisons (Appendix 1) between the Dublin Maternity Hospital, the AKH (before and after its division into two clinics), and the University of Pest.
RESULTS
Maternal mortality at the AKH compared to equivalent European institutions
In addition to mortality data from the Obstetric Clinics at the AKH between 1784 and 1858, Figures 1 and 2 include data for the Dublin Maternity Hospital for the same years, used as ‘control’ data since mortality rates did not differ significantly during this time. Obstetricians in Dublin Maternity Hospital did not perform autopsies before entering the labour wards. In addition they washed their hands and had some understanding that disease could be contagious, although they considered other possibilities as well. Data from the obstetrical clinics in Budapest, managed by Semmelweis between 1851 and 1859, were also analysed. Earlier data from Hungarian clinics were destroyed in the abortive Hungarian uprising, crushed in early 1849, against the absolutist rule of the Hapsburg monarchy [Reference Waller5].
1784–1822: Baseline data
The mortality in the maternity hospitals in Vienna and Dublin was the same for the years 1784–1822 (Fig. 1). Furthermore, the maternal mortality exceeded 2% in only four of those 39 years in Dublin and in only seven of those years in Vienna (Fig. 1).
1823–1847: The effect of the replacement of Professor Lucas Boër by Professor Johann Klein and the introduction of teaching in Pathological Anatomy
In January 1823 (Figs 1 and 2, line A) Professor Lucas Boër, who had trained in England and subscribed to the theory that puerperal sepsis was a contagious condition that could be spread from infected patients, and for which transmission could be reduced by general hygienic principles, was ousted as Director of the AKH on ‘the pretext of insubordination’ [Reference Slaughter9, p. 17]. He refused to use cadavers in the teaching of obstetrics to Viennese students. Instead he instructed students using a ‘phantom’ or mechanical mother. His refusal was seen as resistance to the developing trend to increase the ‘anatomical’ basis of medical teaching in Vienna.
Boër was replaced by his former assistant Professor Johann Klein, who opposed the contagion theory. In the same year the post-mortem dissection of the deceased and the formal study of their diseased organs, Pathological Anatomy, was introduced into the teaching curriculum for (male) Viennese medical students. As the first Professor of Pathological Anatomy at the University of Vienna between 1844 and 1875 Karl (von) Rokitansky would become one of the outstanding pathological anatomists of the 19th century and would perform in excess of 30000 autopsies during this period [Reference Semmelweis8, p. 95].
Therefore, beginning in 1823, when Klein became professor, male doctors and male medical students at the University of Vienna were exposed for the first time to post-mortem dissections, including those mothers who had died from puerperal sepsis. In addition male students of obstetrics practiced vaginal examinations on recently deceased mothers. They would also perform those same examinations on healthy mothers in labour in the AKH, often going directly from the morgue to the maternity ward.
Mortality increased significantly in the AKH compared to Dublin Maternity Hospital following the appointment of Johann Klein as Professor of Obstetrics in 1823 (Figs 1 and 2); and rose still further and remained higher than in Dublin until 1846.
1833–1840: The effect of the division of obstetrical services at the AKH into Clinics 1 and 2, both staffed by (male) medical students and (female) midwives
After January 1833 (Figs 1 and 2, line B), an increasing workload at the AKH required that the work be shared between two clinics, subsequently known as Clinic 1 and Clinic 2, which rotated the admission of expectant mothers every 24 hours. The maternal mortality for both clinics combined for the years 1833–1840 was not different from the rate between 1823 and 1832 but was significantly higher than the rate prior to the appointment of Professor Klein in 1823 (Fig. 1). Mortality was also higher in both clinics than in the Dublin Maternity Hospital during the same period (Fig. 1). However, mortality in Clinic 1 was not different from Clinic 2 during those years (1833–1840) (Fig. 2).
1840–1846: The effect of staffing Clinic 1 exclusively with male medical students and male obstetricians and Clinic 2 with female midwives
By Imperial Decree of 19 October 1840 (Fig. 2, line C), the staffing of Clinics 1 and 2 was arranged according to gender (and hence medical speciality) since gender determined the medical speciality to which students could aspire at the University of Vienna. As a result, female midwives and female students in midwifery were assigned to Clinic 2 whereas male obstetricians and male medical students were allocated to Clinic 1. The mortality in Clinic 1 was significantly higher than in Clinic 2 for the years 1841–1846 (Fig. 2). Admission to Clinics 1 and 2 was assigned by rotation and changed every 24 hours, except on weekends when all admissions were to Clinic 1. In his book Nuland [Reference Nuland6, pp. 20–21] describes the following fictional interaction between a pregnant mother and a medical student controlling admissions to Clinic 1: ‘Please pay attention, young miss! Patients are divided equally and alternately by the days on which they come to us. From Friday afternoon until Sunday afternoon we admit to the First Division. You must go to the doctors!’ The additional point of course was that the higher death rate in Clinic 1 was apparently an open secret amongst the women in Vienna; ‘women particularly dreaded the first clinic and tried desperately to avoid being admitted there’ [Reference Carter and Codell2, p. 17]. Whilst this might have produced bias, it seems improbable that women at lower risk of puerperal sepsis (for whatever reason) could have willingly delayed the onset of labour for up to 24 hours (weekdays) or 48 hours (weekends).
Thus, as described by Semmelweis [Reference Carter and Codell2, p. 64], admissions to the first clinic began at 4 o'clock on Mondays and ended at 4 o'clock on Tuesdays, at which time admission to Clinic 2 began. Then at 4 o'clock on Wednesdays admission to Clinic 2 halted, and resumed in Clinic 1. This alternation of admission to each of the clinics continued on a 24-hour basis except between 4 o'clock on Friday afternoons and 4 o'clock on Sundays when admission was exclusively to Clinic 1. From Sunday afternoon to Monday at 4 o'clock admissions to Clinic 2 resumed. Thus, Clinic 1 received mothers 4 days a week and Clinic 2, 3 days a week. Mortality in both clinics was also significantly higher than in Vienna prior to 1823 and in Dublin in 1841–1846. This indicates that a unique factor (or factors) was present in Clinic 1 explaining the higher maternal mortality than in Clinic 2 whereas additional common factor(s) present in both clinics, and introduced only after 1823, explain their higher mortalities than in the Dublin Maternity Hospital.
1846–May 1847: The appointment of Semmelweis as Assistant to Professor Klein in Clinic 1 and the effect of the death of Professor Jakob Kolletschka on Semmelweis's evolving hypothesis
On 1 August 1844 Semmelweis began his appointment as aspirant Assistant to Professor Klein in Clinic 1 at the AKH. On 27 February 1846 (Figs 2 and 3, line D) Semmelweis was appointed provisional Assistant in Clinic 1. Then on 1 July 1846 Semmelweis was promoted to Assistant (Fig. 3, line E) to replace Dr Franz Breit whose 2-year contract had expired. Figure 3 (line F) indicates the date (20 October 1846) on which Semmelweis's position was withdrawn in favour of Dr Breit who was offered a 2-year extension to his previous contract as Assistant. As a result, Semmelweis spent the period studying obstetrical practices in England and Ireland. Semmelweis recorded that Breit ‘seldom visited the morgue in the months of December 1846 and January, February, and March 1847. The Austrian students … followed his example’ [Reference Semmelweis8, p. 102]. It will become apparent why the absence of the less conscientious Breit and his students from the morgue led to a dramatic fall in maternal mortality (Fig. 3, line 1) during those months.
Figure 3 (line G) indicates the death of Semmelweis's friend Jakob Kolletschka, the Professor of Forensic Medicine, from disseminated sepsis in March 1847. Kolletschka's death was caused by a scalpel wound received whilst conducting an autopsy on a mother who had recently died from puerperal sepsis. The autopsy findings on Kolletschka provided the moment of discovery after which Semmelweis understood how puerperal sepsis was transmitted: ‘Day and night I was haunted by the image of Kolletschka's disease and was forced to recognise … that the disease from which Kolletschka died was identical to that from which so many maternity patients died’ [Reference Semmelweis8, p. 19].
To arrive at this conclusion, Semmelweis had to discount at least two entrenched dogmas of the time; that puerperal sepsis was a disease affecting exclusively women and that this disease, like all others, had multiple (atmospheric-cosmic-terrestrial) or ‘telluric’ causes [Reference Semmelweis8, p. 65].
Discarding these dogmas, Semmelweis concluded that: ‘I was forced to admit that if [Kolletschka's] disease was identical to the disease that killed so many maternity patients, then it must have originated from the same causes that brought it on in Kolletschka’ [Reference Semmelweis8, p. 19]. Next he realized that as the scalpel had introduced ‘decaying matter’ into the blood of Kolletschka, so the hands of the obstetricians and students, soiled by their contact with the tissues of the recently diseased, were passing the same material to the birth canals of the mothers in labour. Semmelweis identified his own deadly contribution: ‘only God knows the number of patients who went prematurely to their graves because of me. I have examined corpses to an extent equalled by few other obstetricians’ [Reference Semmelweis8, p. 98]. Thus Semmelweis ‘identified the contaminated hands of the examining physicians as the source of the decaying matter that spread the same disease [that had killed Kolletschka] among the patients’ [Reference Semmelweis8, p. 20].
Hence, Semmelweis correctly deduced that the cause of the excess mortality from puerperal sepsis in Clinic 1 was the transfer of some agent, present in and on the bodies of the deceased mothers, from the autopsy room to the vaginas of the mothers in labour, on the hands of the obstetricians and students assigned to Clinic 1, thereby sustaining the infectious cycle since labelled ‘The Doctor's Plague’ [Reference Nuland6]. Since Semmelweis was not at that time working in the AKH, he was temporarily powerless either to test his novel hypothesis or to transfer ‘cadaverous particles’ from the morgue to the maternity wards.
Dr Franz Breit was appointed to the Chair of Obstetrics at Tubingen University on 20 March 1847 (Fig. 3, line G), allowing Semmelweis to be reappointed in his stead as Assistant in Clinic 1 at the AKH. The dramatic changes in mortality when Semmelweis was first replaced and then reinstated in Clinic 1 can now be explained. The steeply falling mortality in the period when Semmelweis was replaced by Breit in Clinic 1, November 1846 to March 1847 (Fig. 3, line 1, combined data for Clinics 1 and 2) can be explained by Breit's disinterest in performing autopsies. As a result, neither he nor his students carried ‘cadaverous particles’ to the mothers in Clinic 1 during those months. Conversely the immediate increase in mortality after Semmelweis’ reinstatement as Aspirant in Clinic 1 in March 1847 (Fig. 3, line 2, combined data for Clinics 1 and 2) was due to the resumption of his autopsy duties, after which he returned to Clinic 1 to fulfil his obstetrical duties including examining, with soiled hands, mothers in labour.
May 1847–1849: The effect of the introduction by Semmelweis of handwashing with chlorine in Clinic 1
Realizing that his proposed cycle of infection would be broken if all obstetricians and medical students in Clinic 1 washed their hands with chlorine (chlorina liquida) before examining the mothers in labour, Semmelweis introduced chlorine handwashing into Clinic 1 in late May 1847 (Figs 2 and 3, line H). Semmelweis also introduced a policy of public shaming in which the names of the midwife and student assigned to each mother in labour were displayed above her bed ‘for all to see’ [Reference Waller5, p. 140]. Should the mother die from puerperal sepsis those responsible for her death were immediately identifiable.
Following the introduction of the chlorine washings the mortality in Clinic 1 fell sharply, so that between 1847 and 1849 mortality rates in Clinics 1 and 2 were no longer different (Fig. 2). Furthermore, mortality in Clinic 1 in those years was not different from the mortality in the AKH in the years before the appointment of Professor Klein and the introduction of an ‘anatomically based’ education in 1823 (Fig. 2). However, mortality in Clinic 1 was higher than in the Dublin Maternity Hospital during the same years (Fig. 2).
Semmelweis concluded that
the cadaveric material adhering to the examining hand of the accoucheur is the cause of the greater mortality in the First Obstetrical Clinic; I have eliminated this factor by the introduction of the chlorine washings. The result was that the mortality in the first clinic was confined within the limits of that in the second. … The conclusion, therefore, that the cadaveric particles adhering to the hand had in reality caused the preponderant mortality in the first clinic, was also the correct one [Reference Semmelweis7, p. 395].
Further support for Semmelweis' theory arose in March 1848 (Fig. 3, line K). As widespread civil uprising against the rule of the Hapsburgs reached Vienna in that month [Reference Waller5], clinical teaching of medical students at the AKH was suspended and Semmelweis himself was ‘unusually absent from work’ [Reference Nuland6, p. 122]. As a result, not one of 276 mothers who gave birth in either clinic during that month developed puerperal sepsis [Reference Semmelweis7, p. 536]. A similar result was achieved in August the same year. Never before had this occurred.
But other clinical experiences had taught Semmelweis that his initial explanation for the spread of puerperal sepsis was too restrictive. Since he had already concluded that there must be only one singular cause for puerperal sepsis, Semmelweis assumed there had to be a logical explanation for the increased mortality that he observed in Clinic 1 in October and November 1847 and which caused the increased mortality in the combined data for Clinics 1 and 2 (Fig. 3, line 4). The increased mortality in October (Fig. 3, line I) was traced to the presence of a patient in Clinic 1 with a discharging medullary carcinoma of the uterus occupying the bed at which the ward rounds always began. Since doctors washed their hands with chlorina liquida only before they examined the first patient on the ward round and then used only soap and water between the internal examination of subsequent patients, Semmelweis noted that:
of 12 patients then delivering, 11 died. The ichor from the discharging medullary carcinoma was not destroyed by soap and water. In the examinations, ichor was transferred to the remaining patients and so childbed fever multiplied. Thus, childbed fever is caused not only by cadaverous particles adhering to hands but also by ichor from living organisms. It is necessary to clean the hands with chlorine water, not only when one has been handling cadavers but also after examinations in which the hands could become contaminated with ichor [Reference Semmelweis8, p. 93].
In November 1847 (Fig. 3, line J) a patient with a discharging ‘carious’ knee was admitted to the ward. As a result, according to Semmelweis:
the ichorous exhalations of the carious knee completely saturated the air in the ward. In this way the other patients were exposed and nearly all the patients in the room died. … These deaths were largely due to ichorous exhalations from this individual. The ichorous particles that saturated the air in the maternity ward penetrated the uteruses already lacerated in the birth process. The particles were resorbed, and childbed fever resulted. Thereafter, such individuals were isolated to prevent similar tragedies [Reference Semmelweis8, p. 93].
Unexplained by Semmelweis's theory was why these two mothers had not themselves succumbed to puerperal sepsis.
As a result of these additional experiences, Semmelweis concluded that:
I regard the disease, without a single exception, as a resorption fever dependent on the resorption of decaying animal-organic matter. … In the overwhelming majority of cases the decaying animal-organic matter is conveyed to the individual from external sources. The source of decaying animal-organic matter can be a corpse of any age, of either sex, regardless of the preceding disease, regardless whether the corpse is a pregnant woman or not … whether the individual suffers from childbed fever … Decaying animal-organic matter is carried by examining fingers, operating hands, instruments, bed linen, the atmosphere, sponges, basins, hands of midwives and attendants. … In other words, anything that is contaminated by decaying animal-organic material and comes into contact with the genitals of patients [Reference Semmelweis8, pp. 114–115].
To explain why this explanation was not immediately embraced, Waller [Reference Waller5] points out that, at least in Britain and France, morgues were seldom located in the maternity hospitals. Thus Semmelweis's theory appeared to explain a special case, specific only to the AKH. In particular, Semmelweis's theory could not explain why mothers in Clinic 2 continued to die, or why puerperal sepsis also occurred in mothers delivering outside hospital. The germ theory of infection explained the universal applicability of Semmelweis's theory [Reference Waller5].
After 1850: The effect of the termination of Semmelweis's contract as Assistant to Professor Klein in Clinic 1 and his replacement by Dr Carl Braun
Figure 3 (line L) records when Semmelweis's contract in Clinic 1 was terminated (March 1849). He was replaced by Dr Carl Braun who would later succeed Klein as Professor of Obstetrics at the University of Vienna. Braun did not accept Semmelweis's theory. As a result, once Semmelweis had left Vienna, Braun did not enforce the prophylactic measures introduced between 1847 and 1849.
On 15 October 1850 Semmelweis left for Budapest (Figs 2 and 3, line M) where he was appointed honorary Senior Physician in the Obstetrics Division at St Rochus Hospital in Budapest and in July 1855 as Professor of Theoretical and Practical Midwifery at the University of Pest.
Waller [Reference Waller5] offers the novel explanation for why Semmelweis left Vienna even though a group of outstanding young professors at the University of Vienna supported his revolutionary ideas. He argues that Semmelweis actively identified with the republican forces wishing to overthrow the Hapsburg monarchy whereas Klein was an ardent monarchist. Klein saw Semmelweis's theory as a revolutionary threat to that hierarchy and so it had to be suppressed. According to Waller, Semmelweis had no option but to leave Vienna ‘a belated casualty of the year of revolutions’ [Reference Waller5, p. 148].
Following the appointment of Carl Braun, mortality in both clinics at the AKH began to rise (Figs 2 and 3, line M). Thus mortality was significantly greater in both clinics than prior to 1823, although not statistically higher than the mortality between 1847 and 1849 when chlorine washing was in vogue (Fig. 2). Later Semmelweis would calculate that during Braun's 12-year tenure an excess of 1035 deaths occurred because the practice of chlorine washings was not promoted [Reference Semmelweis7, p. 856].
1850–1858: Maternal mortality rates in the Budapest Maternity Hospital directed by Semmelweis
In contrast, in his new position in the maternity hospitals in Budapest, Semmelweis initially maintained a low mortality in Budapest until 1857 and 1858. Semmelweis explained the greater mortality in those 2 years on soiled bed linen that was not changed between deliveries nor properly sterilized because the hospital outsourced the cleaning of linen to the cheapest contractor [Reference Semmelweis7, pp. 424–427]. As a result, the mortality in the Budapest hospitals during the years of Semmelweis's direction (1850–1858) (range 0·39–4·01) were not significantly different from Clinic 2 of the AKH (range 1·06–6·18) during the same time (P=0·09). However, for 8 out of the 9 years Clinic 1 of the AKH had a higher mortality rate (range 1·07–9·10) than the Budapest hospitals (range 0·39–4·01) (P=0·02) indicating a substantial saving of maternal lives in Budapest compared to Vienna. Interestingly the mortality rate in Clinic 1 remained lower than in Clinic 2 between 1849 and 1852 even though Semmelweis was no longer present. This suggests some residual effect of his teachings.
SUMMARY
Appropriate statistical analyses, not available to Semmelweis, establish that maternal mortality was not different in the maternity hospitals of Vienna and Dublin between 1784 and 1822. Mortality rose significantly after the introduction of Anatomical Pathology to the Vienna Medical School in 1823 whereas it remained unchanged and lower in the Dublin Maternity Hospital. The division of obstetric services between Clinics 1 and 2 at the AKH in 1833 did not alter the mortality, which remained significantly higher in both clinics than (i) in Dublin during the same period and (ii) compared to the mortality in the AKH before 1823. The splitting of services by gender between the two clinics after 1840 caused mortality in Clinic 1, staffed by physicians (obstetricians and doctors in training) to be significantly higher until 1847 than the mortality in Clinic 2, staffed by midwives. The introduction of chlorine washings of the physicians' hands in Clinic 1 caused a significant reduction in mortality such that the mortality in Clinic 1 was no longer different from the mortality in the AKH prior to 1823. The succession of Semmelweis by Braun in Clinic 1 caused the mortality in both clinics to rise, albeit not significantly, than before the introduction of Pathological Anatomy at the University of Vienna in 1823.
This retrospective statistical analysis of these data establish that, according to modern criteria, Semmelweis provided sufficient evidence to confirm his hypothesis that the excess mortality in Clinic 1 at the AKH was due to the transfer of an infective agent on the hands of doctors and medical students from deceased mothers to those in labour. It is acknowledged that better evidence may have been provided by a case-control study in which individual data are analysed. However, within the limits of the data available, the case is clearly convincing. The creation of the germ theory of infection allowed the global relevance of Semmelweis's discovery to be understood, namely that the infective agent was a specific bacterium that exists ubiquitously in hospitals, not just on the bodies of those suffering from, or who have recently died from puerperal sepsis.
We trust that our paper will serve as another lasting tribute to a man who might be considered as one of the great minds in the history of medicine, but in whom, personality [Reference Nuland6], democratic political beliefs [Reference Waller5] and the onset of premature senility [Reference Nuland6] sadly conspired to conceal his genius [Reference Nuland and Semmelweiss1].
ACKNOWLEDGEMENTS
The research undertaken in the Unit is funded by the Harry Crossley and Nellie Atkinson Staff Research Funds of the University of Cape Town, the Medical Research Council of South Africa, Discovery Health, Bromor Foods, and the National Research Foundation of South Africa through the THRIP initiative.
APPENDIX 1. Statistical analysis
The response variable maternal mortality was measured every year from 1784 to 1858. Since no assumption could be made about the regression function, local polynomial smoothing, which is a method for non-parametric function estimation, was used [Reference Cleveland10]. The underlying idea is to take advantage of the fact that arbitrary smooth functions are well approximated by polynomials, but this property is only used locally. The estimator of the function at a point is the value of a polynomial fitted in a neighbourhood around the point. For the current analysis, we want to smooth the response variable as a function of year, for which the number of maternal deaths was measured equally distant from 1784 to 1858. Quadratic local polynomials were used for the local least squares fitting [Reference Cleveland and Grosse11]. The bias corrected Akaike Information Criteria was used for choosing the smoothing parameter that minimizes both the tightness of the fit and the model complexity (balance between bias and variance). This resulted in a value of 0·35 for the smoothing parameter. In the presence of some outliers, a robust fitting method (iterative reweighting) was used. Because of heteroscedastic residuals, a priori weights were assigned before the 95% confidence limits were added to the model predictions. For comparisons of mortality rates in the maternity hospitals in Budapest with the AKH Clinics 1 and 2 for the period 1850–1858, the Cox and Stuart Test [Reference Cox and Stuart12] (simple sign test) was used, testing the null hypothesis that the rate in Clinic 1 is the same as the rate in St Rochus, against the alternative that the rate in Clinic 1 is higher than the rate in St Rochus.
NOTE
Supplementary information (the raw data used to produce Figs 1–3) accompanies this paper on the Journal's website (http://journals.cambridge.org).
DECLARATION OF INTEREST
None.