Introduction
Measles is a highly infectious viral disease that rapidly spreads in susceptible populations. It can be associated with serious complications such as pneumonia, encephalitis, death and rarely subacute sclerosing panencephalitis. Measles is a vaccine-preventable disease. The measles mumps rubella (MMR) vaccine was introduced to the UK childhood immunisation schedule in 1988, and since 1996 has been offered as two doses, the first at 12–13 months of age and the second preschool, given from 3 years 4 months of age [1]. MMR is considered a highly effective vaccine for preventing measles with one dose conferring protection from developing clinical measles in 95% of individuals [Reference Demicheli2].
MMR uptake in children in Scotland is high with 93% of children receiving two doses by the age of 5 years [3]. Due to this, measles is rare in Scotland (population 5 404 700) and an average of 23 confirmed cases of measles have been notified annually over the past 5 years [4, 5]. Scotland has not had large outbreaks of measles recently unlike other urban centres in the UK [Reference Pegorie6, Reference Wise7]. Meanwhile, Europe has seen a number of countries affected by large national outbreaks that have spread to thousands of people and resulted in a number of deaths [8–10].
Edinburgh, the capital of Scotland, has a large and diverse student population of over 60 000 in four universities, the largest of which attracted more than 10 000 international students in 2015/2016 [11]. There have not been significant measles outbreaks in universities in Edinburgh before, although there have been large outbreaks of mumps [Reference Willocks12].
In September 2016, an imported case of measles in Edinburgh in a university student resulted in a further 17 confirmed cases during October and November 2016. All cases were confirmed as having measles genotype D8 with a virus strain most commonly seen in South East Asia. Most of the cases were in university staff and students, and despite hundreds of staff and students being exposed, the outbreak was successfully contained due to the rapid notification and diagnosis of cases, follow-up of contacts, the high background vaccination rates in Edinburgh and the deployment of mass vaccination clinics in areas affected by the outbreak.
We describe the epidemiology of these measles cases and detail the multifaceted response that successfully contained this outbreak.
Methods
Reporting of measles cases
Measles is a statutory notifiable disease in Scotland, and all clinically suspected and laboratory-confirmed cases must be reported to public health departments [13]. In Edinburgh, the local public health department is notified via health practitioners or laboratories of all suspected and confirmed measles cases. Cases of measles are excluded from work and educational settings for the duration of their infectious periods. Contact tracing is undertaken for all cases of measles and post-exposure prophylaxis for contacts with MMR vaccine or human normal immunoglobulin is organised as required according to national guidance [14].
Case definitions
Case definitions for the outbreak were defined as per Table 1. Suspected cases were discussed between clinicians, virology and health protection professionals and assigned to the relevant category.
Table 1. Case definitions used throughout the outbreak of measles in Edinburgh from September 2016 onwards
Case finding
All possible, probable and confirmed cases of measles during the outbreak were reported to and collated by the local public health department. Epidemiological data included the patient's demographic details, occupation, student status and location of studies, date of presentation, date of rash onset, symptoms, MMR status, contact with healthcare services, results of virology testing and current case definition.
Communications were sent out to all primary and secondary care providers in the region to increase awareness of the outbreak and encourage reporting of suspected cases meeting the case definitions.
An enhanced surveillance form was completed for all probable and confirmed cases, in which were details on all contacts of cases within their infectious period. Cases’ infectious period was defined as between 5 days before and 4 days after rash onset. Contacts were defined as those who had direct face-to-face contact or spent 15 min or more in the same room while an infectious case was present, as defined in national guidance [14]. For the purposes of this outbreak, a room was defined as any confined place and therefore included lecture halls and event venues. Epidemiological case and contact data were collected and compiled using Microsoft Excel.
Virology testing
All possible or probable cases of measles were tested by PCR on pharyngeal swab at the East of Scotland Specialist Virology Laboratory at the Royal Infirmary of Edinburgh. Two hundred and sixty-three PCR tests were carried out on possible and probable cases of measles throughout the duration of the outbreak from the end of September 2016 to the end of December 2016. Ninety-seven per cent of these PCR tests were carried out within 12 hours of receipt at the laboratory. These pharyngeal swab samples were taken as soon as possible after presentation with rash and fever to health services.
All possible and probable cases were sent self-collection saliva kits to their home address if they tested negative initially via PCR. When returned, these saliva samples underwent testing at the Public Health England Reference Laboratories, Colindale, to repeat PCR testing and to undergo serology testing for measles IgM.
PCR-positive throat swabs were sent for confirmatory testing at the Public Health England Reference Laboratories, Colindale. At these laboratories, PCR tests were repeated, and genotyping was undertaken. The strain of measles in this outbreak was compared with the worldwide database of measles nucleotide sequences to identify if it matched other strains with the same sequence circulating worldwide [15].
Results
Index case
The public health department in Edinburgh was informed of a suspected case of measles in a university student at the start of the academic year at the end of September 2016. Measles was confirmed via PCR testing of a pharyngeal swab after admission of the case to hospital.
The index case was notified shortly after admission to hospital and an interview was conducted by the local public health department to identify contacts. The index case had been in South East Asia just prior to the onset of their symptoms and the start of the academic year at the university. During their infectious period, they attended multiple lectures, student induction events, an event in Edinburgh out with the university, an out-of-hours primary care service and an open hospital ward before being diagnosed and isolated. In this short period, several hundred people, mostly university students, were potentially exposed to measles. Over 300 contacts of the index case were identified and contacted by the local public health department. These contacts were given written information on measles and offered the opportunity to attend an ad hoc MMR vaccination clinic hosted at the affected university.
Outbreak description
During October and November 2016, a further 17 confirmed cases of measles were notified to the public health department in Edinburgh. An initial peak in secondary cases began on day 12 of the outbreak when nine cases were notified within the period of one week. A further peak of cases occurred on day 22 of the outbreak with seven cases notified within the following week. The outbreak was declared over two incubation periods (42 days) after the end of the last case's infectious period at the end of December 2016. Figure 1 shows the epidemic curve.
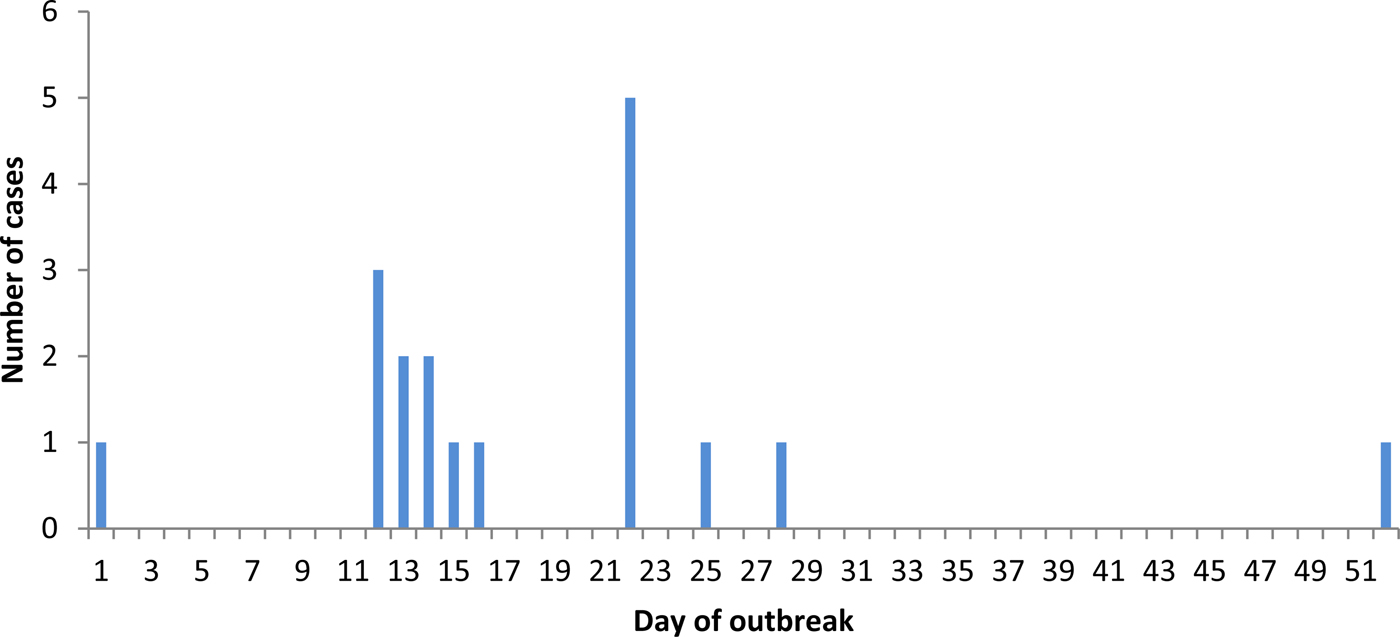
Fig. 1. Epidemic curve of measles outbreak by notification date in Edinburgh 2016.
Ten of the 18 confirmed cases were aged between 15 and 24 years old (Fig. 2). Ten cases were male and eight were female. MMR status was ascertained via an interview for 13 of the 18 cases. In addition to the interview, MMR vaccinations were verified by general practitioner (GP) records, the Scottish Immunisation Recall System or physical documentation in six cases. Five cases were unable to recall their MMR status and did not have local records to confirm their vaccination status. Having been confirmed by local records, one case had previously received two doses of MMR and one case had received one dose. Of the 11 cases who were unvaccinated, one was too young to have received any MMR vaccine.
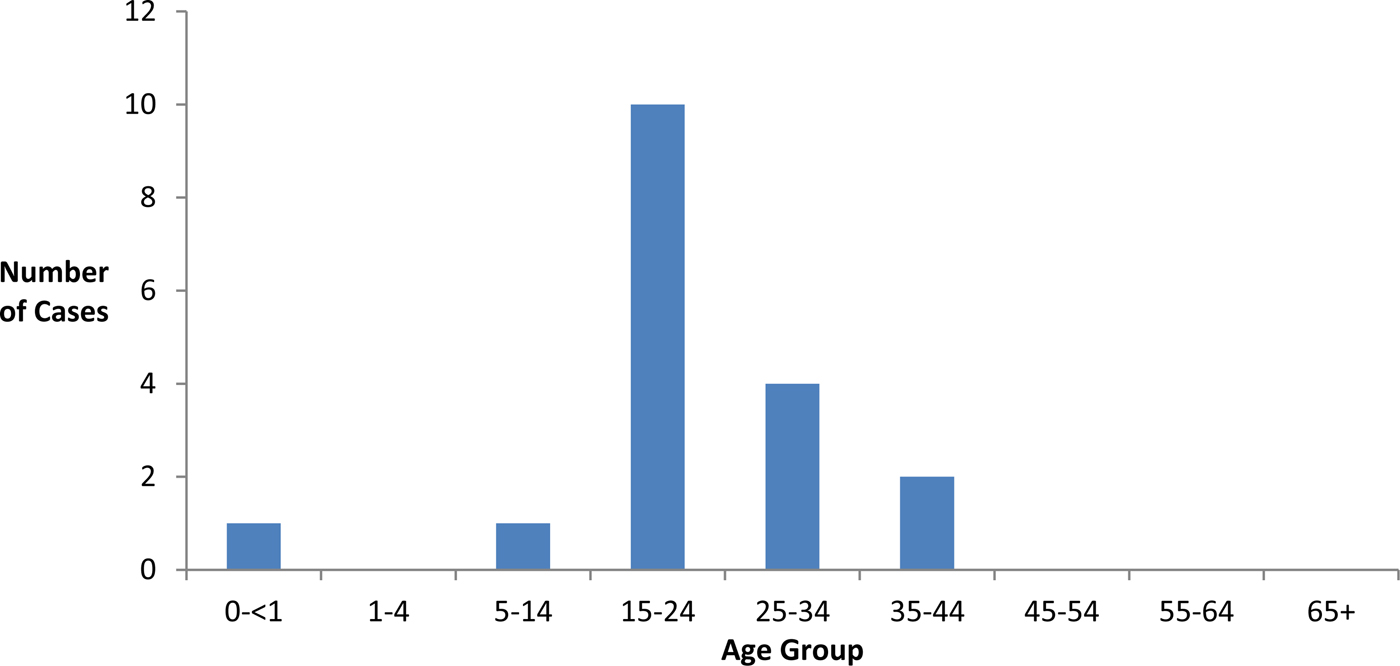
Fig. 2. Age groups of confirmed cases of measles during the outbreak in Edinburgh 2016.
Figure 3 describes the epidemiological links between cases. The university affected was the main focus of the outbreak with a total (including the index case) of 12 confirmed cases (10 university students and two university staff). Secondary spread resulted in nine cases with identifiable epidemiological links to the index case. Five were students based at the same university campus and one was a household contact (also a university student). Three cases attended an event in Edinburgh out with the university, which the index case had also attended. Of these three cases, two were also university students and one was an infant.
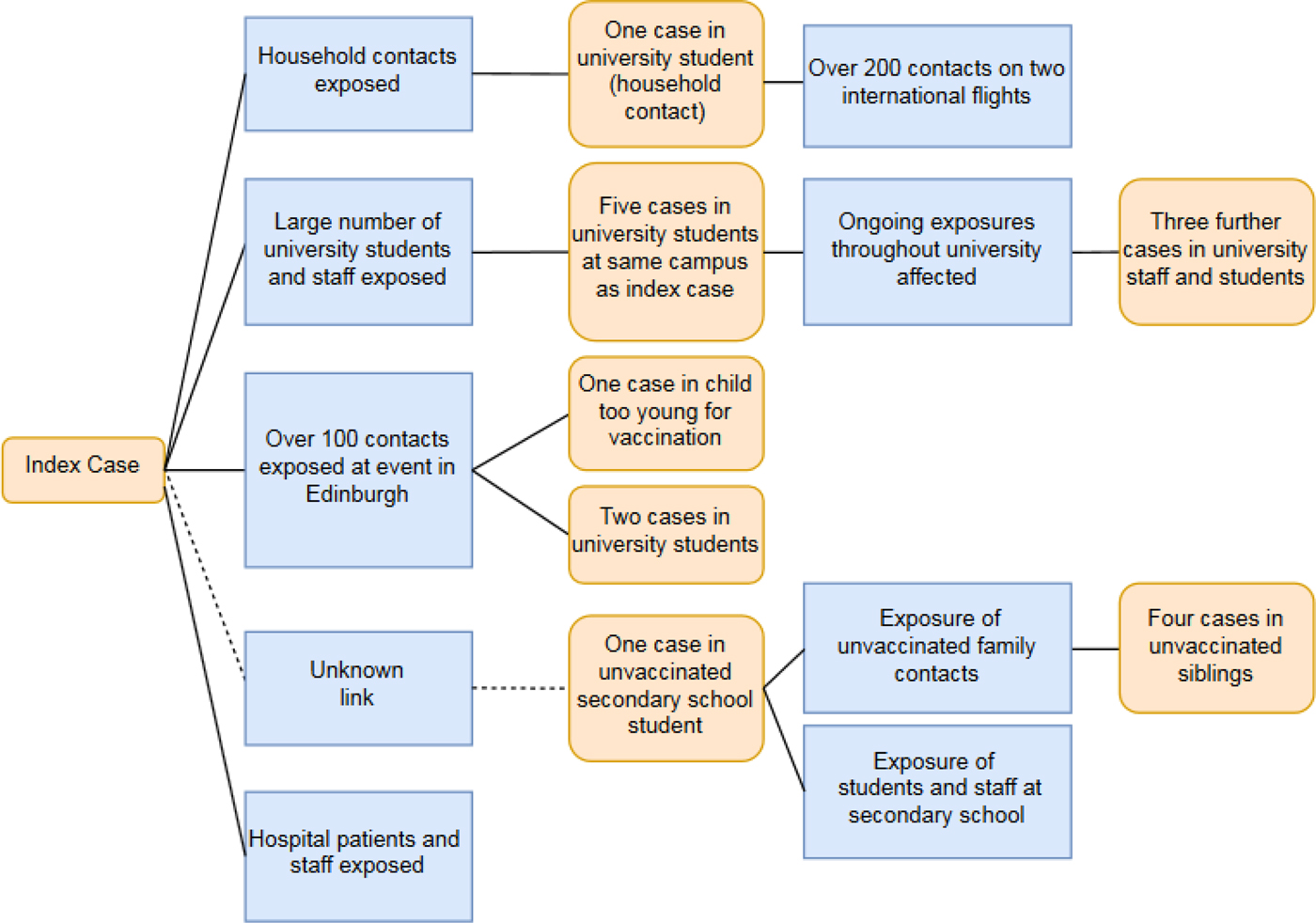
Fig. 3. Epidemiological links between 18 confirmed cases of measles and groups exposed to cases.
One unvaccinated child at an Edinburgh secondary school developed measles with the same outbreak strain within two weeks of the index case being notified. They however did not have an identifiable epidemiological link to the index case. The secondary school affected was in an area of Edinburgh where uptake of MMR had previously been identified as being lower than the surrounding areas. Four unvaccinated siblings were household contacts of the secondary school child. These unvaccinated siblings were excluded from the educational settings they attended under the Public Health, etc. (Scotland) Act 2008 as they were deemed to be at high risk of developing measles [13]. All four siblings went on to develop confirmed measles after having been excluded.
A further three cases in university staff and students later in the outbreak were notified to the local public health department and were likely due to tertiary spread within the university.
One of the secondary cases, a household contact, developed measles while abroad. While infectious, this case boarded two flights on return to Edinburgh exposing hundreds of international passengers to measles.
Laboratory findings
Twenty-one samples initially tested positive by measles PCR at the local laboratory. All positive PCR samples on throat swab were sent to the reference laboratory where 18 of the samples were confirmed to be of the same virus type and strain in this outbreak. The three other samples that tested positive initially were due to recent administration of the MMR vaccine. Those who had negative PCR tests were sent self-collection saliva kits. There was a 35% return rate from these samples. Of those cases that submitted further saliva samples, all were negative when retested for measles IgM. However, due to the poor return from self-collection saliva kits, the majority of possible cases were discarded on the basis of negative PCR results and clinical assessment. Discarded cases comprised of those presenting with other illnesses causing fever and rash.
The outbreak virus strain was genotype D8, which is one of the most common circulating types in the world [Reference Rota16]. It had the closest match to a measles genotype D8 strain currently circulating in South East Asia [15]. It did not match measles genotype D8 strains currently circulating in the rest of the UK and indicates that the origin of this measles outbreak was an imported strain.
Public health response
The public health response involved extensive contact tracing and follow-up of over 1500 individuals who were identified as having had contact with confirmed cases of measles. All confirmed and probable cases were contacted directly and interviewed over the phone or in person by the local public health department.
Drop in MMR vaccination clinics were set up promptly and ran throughout the outbreak at several campuses at the university affected, the secondary school where one case had attended and a different university in Edinburgh where one of the confirmed cases had also attended.
Mass communications were sent throughout the university affected via e-mails, e-posters, posters and flyer handouts by the local public health department in communal university areas to inform staff and students of the risk of measles and advertise drop in vaccination clinics for MMR. Members of the public health department also attended these vaccination clinics to discuss vaccination with staff and students in person. During the outbreak, 22 vaccination clinics were held administering over 1200 doses of MMR vaccine.
The public health response also involved immediate isolation of suspected cases of measles once notified for the remaining duration of their anticipated infectious period. For probable and confirmed cases, extensive contact tracing by phone was undertaken and management of contacts exposed to measles included information and advice as well as post-exposure prophylaxis with MMR vaccine or human normal immunoglobulin when required as per national guidance [4].
The exposure of a large number of people on two international flights prompted a large follow-up exercise based on guidance from the European Centre for Disease Prevention and Control [17]. The national health protection body for Scotland, Health Protection Scotland, was informed and gathered information on all those who were on board the flight inbound for Edinburgh using flight manifests. Passengers on the inbound flight were subsequently contacted. Public health authorities abroad were contacted regarding the exposure of passengers at an international airport out with Scotland.
Healthcare response
Five of the cases were admitted to hospital for supportive treatment, all of whom were discharged promptly. Eight of the other cases attended primary or secondary care services in some form. Patients exposed in hospital settings were followed up by hospital infection and prevention control teams as per national guidance [4]. Primary care and emergency departments were given advice to identify suspected measles cases at reception and avoid exposing others in waiting rooms.
Staff who had come into contact with a case of measles were followed up by local occupational health services. A large number of frontline staff had uncertain MMR status or no evidence of measles immunity. MMR vaccination was given to those who required it and three healthcare workers required formal exclusion from work under the Public Health, etc. (Scotland) Act 2008 [13].
Discussion
We report an imported case of measles in a university setting, which led to an outbreak of measles with a total of 18 cases. Several factors contributed to the success in containing this outbreak and preventing spread to others. These included the prompt detection and confirmation of cases, immediate isolation of cases and their unvaccinated contacts as well as a co-ordinated whole health systems response. There is currently no specific data on vaccination rates of university students in Edinburgh; however, the over 1200 doses of MMR given mostly to university students and staff indicate an undervaccinated population. The high background MMR vaccination rates in Edinburgh may have prevented this outbreak spreading to the wider population regardless of these interventions. However, single cases of measles in the UK have led to large national outbreaks, and therefore prompt public health actions such as those described here are pragmatic when new cases or clusters of measles cases occur [Reference Wise7]. Joint working with the affected university enabled widespread communications about measles to be sent to students and staff and facilitated the prompt arrangement of accessible MMR vaccination clinics. Public health departments should put in place plans for the rapid deployment of clinics for mass vaccination in the event of an outbreak.
Ten cases were university students, two cases were university staff and two cases were secondary school students. This outbreak illustrates the ease by which measles infection can spread within higher educational settings. Seventeen of the 18 cases were either undervaccinated, unvaccinated or uncertain of their MMR vaccination status. There is currently an age cohort of measles-susceptible individuals in UK educational settings, including universities and secondary schools, who were unvaccinated as children during the MMR scare which incorrectly linked the MMR vaccine with the development of autism [Reference Godlee18, Reference Wakefield19]. Other universities similar to those in Edinburgh will also host a large number of international students who may have grown up in countries with suboptimal rates of MMR vaccination. Within the university affected, hundreds of people were exposed within a short space of time following only one imported case. The potential exposure of hundreds of people on flights at international airports also demonstrates the ease by which the virus can travel across continents in highly mobile university staff and student populations.
Despite the university affected advising that all students should be fully vaccinated with two doses of MMR before matriculation, it would appear that many are either undervaccinated or unsure of their status. This was demonstrated by the high uptake of MMR vaccines at drop in vaccination clinics set up at the university during the outbreak. Closer working between universities and public health authorities will assist with prevention and preparedness for future measles outbreaks. Universities and university health services should make special efforts, particularly at the beginning of the academic year, to offer and promote the uptake of MMR in students to prevent similar outbreaks occurring. Evidence of MMR vaccination should be considered as a compulsory prerequisite to enrolment at academic institutions in combination with other approaches to promote uptake in current students.
The frontline healthcare workforce in Edinburgh was not fully aware of their vaccination status with MMR or their immune status to measles prior to this outbreak. A large-scale occupational health response, including MMR vaccinations for frontline staff, was therefore required during the outbreak. Three frontline staff were exposed to cases of measles and required exclusion from work for significant periods of time. Health systems should be prepared for measles, and therefore have a fully vaccinated workforce prior to the emergence of measles outbreaks. Other measles outbreaks have highlighted the risks to unvaccinated healthcare workers and the risk of nosocomial transmission in propagating an outbreak [Reference Porretta20]. This may warrant occupational health teams requesting compulsory evidence of complete MMR, equivalent vaccination or immune status before staff start work in a health care environment and up-to-date accurate recording of vaccinations for current staff.
After the initial cluster of cases between days 29 and 51 of the outbreak, there were no probable or confirmed cases of measles identified across NHS Lothian. The 22 days before the final case of measles in this outbreak was identified is at the upper end of the reported incubation period for measles (21 days). However, due to the significant period between these cases, it is possible that other cases in this time were not identified or had subclinical features, which did not result in them presenting to healthcare facilities. The use of PCR as the main diagnostic tool in this study also presents some limitations as this is not the current WHO standard [21]. There was a poor return rate of self-collection saliva kits testing measles IgM that had been sent out to PCR-negative cases. It is therefore possible that negative PCR cases were misclassified or discarded incorrectly. However, possible and probable cases were isolated for the duration of their anticipated infectious periods regardless of PCR results and were only discarded after accounting for clinical presentation in combination with PCR results. As discussed, 97% of tests were reported within 12 hours of receipt at local laboratories, whereas serology has a significantly longer turnaround time. The rapid reporting of PCR results in this outbreak assisted in the prompt public health response described. We recommend that the use of PCR should be considered alongside serology in other outbreak situations to facilitate a rapid response to confirmed cases of measles. The wide case definition of possible cases (Table 1) meant that the majority of those tested were those with other viral illnesses causing rash. This was likely due to the increased awareness of GPs and hospital services to the ongoing outbreak of measles.
Several ongoing measles outbreaks in Europe have spread rapidly amongst vulnerable or undervaccinated populations [8–10]. As discussed above, the relative contribution of the public health measures described in preventing the further propagation of this outbreak is not possible to quantify. However, despite secondary and tertiary spread to another 17 cases, given that over 1500 contacts were identified, this outbreak demonstrates how the prompt detection and response to single confirmed cases of measles can successfully limit onward spread and prevent large national outbreaks. This requires systems in primary and secondary care to rapidly alert public health authorities, diagnostics that can confirm suspected cases of measles rapidly and the ability to provide post-exposure prophylaxis for contacts of cases of measles where indicated.
Conclusions
The MMR vaccine should be widely promoted and easily accessible throughout higher educational and university settings for both domestic and international students early in the academic year. Wide and clear communications in outbreak settings, high background vaccination rates, rapid diagnostics and prompt vaccination clinics in the event of a measles outbreak can effectively control an outbreak in higher educational institutions and other settings. The continuing measles outbreaks currently affecting Europe should prompt close working between public health authorities and higher educational settings to mitigate this risk.
Acknowledgements
The authors would like to acknowledge the contributions of all members of the Incident Management Team; NHS Lothian's Directorate of Public Health and Health Policy; NHS Lothian's Communications team; NHS Lothian Virology services; Lothian Acute hospital services; Lothian Unscheduled Primary Care services and General Practitioners in the affected area; NHS Lothian, Lothian Occupational Health; Health Protection Scotland. This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of Interest
None.







