INTRODUCTION
Non-typhoidal (NT) Salmonella infections remain an important public health problem in Canada and worldwide [Reference Majowicz1]. In Canada, NT Salmonella is one of the leading bacterial causes of enteric illness with more than 100 000 domestically acquired estimated cases each year [Reference Thomas2]. Of these, 80% are estimated to be of foodborne origin. NT Salmonella is also the leading pathogen for the estimated annual cost of illness and quality-adjusted life years (QALY) loss in the United States, with an estimated cost of 3·3 billion and 17 000 QALYs [Reference Hoffmann, Batz and Morris3]. Although most cases of NT Salmonella are self-limiting, some will lead to severe symptoms and sometimes to severe invasive infections, including bacteraemia and arthritis [Reference Threlfall, Wain, Lane and Palmer4]. The economic burden of NT Salmonella is substantial and hospitalizations and deaths associated with severe infections account for much of this cost [Reference Hoffmann, Batz and Morris3]. Some groups of individuals are considered more at risk of severe NT Salmonella infection, including young children, pregnant woman, immunocompromised individuals and seniors [Reference Gerba, Rose and Haas5]. Among those groups, seniors are one sub-population that is expected to change significantly in the next decade. With increasing life-span and a demographic shift towards a larger proportion of seniors, Statistics Canada expects that people over 60, who represented 20% of the Canadian population in 2011, will increase to 30% by 2035 – an increase of 56% for this age group or more than 5 million people [6]. Moreover, the proportion of people over 80 will also increase over time, meaning that they will come to represent a larger percentage of the senior population. This is noteworthy since in Canada the health-adjusted life expectancy – the average number of healthy years that a person lives – is <72 years [7], which means that even if people live longer, they are not necessarily living healthy.
In older people several factors can contribute to more severe consequences following infection by enteric pathogens, including NT Salmonella. Aging is associated with changes and deterioration of the immune system. In older adults, adaptive immune function decreases as functional alterations in macrophages and granulocytes occur [Reference Khanna and Markham8]. Moreover, a natural shift to memory T-cells reduces the efficiency of the cell-mediated response when new exposures to pathogens occur [Reference Khanna and Markham8, Reference Castle9]. Various other factors may also influence immunity in older people, including therapies associated with chronic diseases (e.g. rheumatoid arthritis, cancer) and malnutrition [Reference Smith10–Reference Donskey12]. Aging is also associated with a higher chronic disease incidence and it has been reported that hospitalized salmonellosis patients with chronic diseases may be at increased risk for adverse outcomes, including death and longer length of stay [Reference Cummings13].
The growth of the senior population represents an important challenge for the health care system in terms of capacity and expenditures. The incidence of reported cases of NT Salmonella in Canada is approximately 18/100 000 and 20% comes from seniors, but higher hospitalization and death rates have been reported for this age group [14, Reference Kennedy15]. Better understanding of the actual burden of NT Salmonella-related hospitalizations in seniors is essential to be able to anticipate future burden. Therefore, the objectives of this study were to describe NT Salmonella-related hospitalization in seniors from 2000 to 2010 in Canada and generate estimates of hospitalizations associated with domestically acquired foodborne NT Salmonella in that vulnerable population.
METHODS
The numbers of NT Salmonella-related hospitalized cases were extracted from the Hospital Morbidity Database (HMDB) of the Canadian Institute for Health Information (CIHI) from 1 April 2000 to 31 March 2010. This database contains national discharge statistics from all acute care facilities across Canada; however, it does not include discharge data from chronic care, rehabilitation, psychiatric facilities, and emergency department visits [16, 17]. The HMDB contains clinical and demographic information on inpatients. Key variables include patient sex, patient age, province of residency, date of admission, date of discharge, discharge disposition (includes death outcomes), and length of stay. It also contains diagnosis codes from the International Statistical Classification of Diseases and Related Health Problems (ICD-9-CM and ICD-10) published by the WHO (World Health Organization). For each discharge, 16–25 diagnostic codes were captured depending on the year. To ensure consistency in this study, a case was defined as a patient listed in the HMDB for whom one of the diagnosis codes associated with NT Salmonella (Table 1) had been recorded anywhere in the first 16 diagnostic code categories. The database also contains the variable ‘most responsible diagnosis’ for hospitalization, which is defined by the diagnosis or condition that can be described as being most responsible for the patient's stay in hospital. To be consistent with another Canadian study on hospitalizations, repeat visits with a diagnostic of NT Salmonella within 30 days were excluded as they were considered to be associated with the same episode [Reference Thomas18]. Only patients for whom a Canadian province or territory was recorded as a place of residency were kept, thus excluding non-Canadian travelers hospitalized in Canada during the study period.
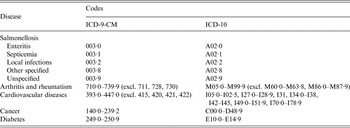
Table 1. ICD-10 and ICD-9-CM codes for salmonellosis and selected chronic diseases
Total and annual numbers of hospitalizations were compiled for the 10 years of the study. The mean and annual hospitalization rates per 100 000 were calculated for three age groups of adults: 20–59 years old, 60–79 years old, and 80 years and over. Population estimates from Statistics Canada for 2000–2010 were used for rate calculations [19]. The estimated percentage of reported cases hospitalized was calculated by dividing the numbers of hospitalized cases by the number of reported cases of Salmonella obtained from the Canadian Notifiable Disease Surveillance System [14]. Descriptive analyses (percentages, means, and medians) were performed on variables associated with the burden of hospitalization: length of stay and death. The discharge disposition variable in the database was used to identify deaths, meaning that all patients hospitalized with a diagnosis of NT Salmonella and who died at the hospital were recorded, reflecting both underlying and contributing causes of death. Medians were used when variable distributions were skewed. Descriptive analyses were also performed on comorbidity recorded according to the four most prevalent chronic diseases affecting seniors in Canada: arthritis and rheumatism, cardiovascular diseases, cancer, and diabetes [20] (Table 1). Diagnostic codes associated with these chronic diseases are presented in Table 1. Death outcomes and chronic disease status for hospitalizations with salmonellosis as the most responsible diagnosis (or the main reason for hospital stay) were also described. Statistical tests were used to test significance – the χ2 test was used for comparing proportions among age groups and the Wilcoxon rank-sum and Kruskal–Wallis tests were used to test differences between medians. Data analyses were performed by using SAS statistical software version 9.3 [21].
Estimates of hospitalizations and deaths associated with total and domestically acquired foodborne NT Salmonella were calculated from the modeling approach used for the estimation of foodborne illness-related hospitalizations and deaths in Canada described in Thomas et al. [Reference Thomas18]. This analysis accounted for under-reporting and under-diagnosis (adjusting for a multiplier of 1·8). The proportion of salmonellosis cases caused by foodborne transmission (80%) was assumed to be the same as in Thomas et al., and an age-specific proportion of travel-related illnesses was applied using data from FoodNet Canada (2005–2013), Canada's integrated enteric disease surveillance system based on sentinel sites [22] (Table 4). Monte Carlo simulations were performed to account for uncertainty generating mean estimates and 90% probability intervals (PI).
RESULTS
Number of hospitalizations and rates
From April 2000 to March 2010, 6148 NT Salmonella-related hospital admissions were recorded in adults aged 20 years and over. Although seniors (60+) represented 23% of reported NT Salmonella cases in adults in Canada during this time period, almost 50% (2995) of NT Salmonella-related hospitalizations occurred in this age group. In seniors, NT Salmonella-related hospital admissions represent an estimated 32% (2995/9634) of nationally reported cases, compared with 10% (3153/32 173) in other adults. Annual numbers and hospitalization rates are presented in Table 2. For each age group, hospitalization rates in men and women were not significantly different from each other. The diagnostic code Salmonella enteritis was the most recorded for each age group, followed by Salmonella sepsis and localized Salmonella infections when type of infection was specified (Table 3). Unspecified infections represented about 7% of hospitalizations in each age group. Proportions of hospitalizations where NT Salmonella diagnostic codes were captured as the most responsible diagnosis for hospitalization were the same (68%), regardless of age group.
Table 2. Annual numbers and hospitalization rates for salmonellosis (2000–2010)

* Percentage of the Canadian adult (20+) population.
Table 3. Percentages of hospitalizations, deaths and length of stay according to NT Salmonella as the most responsible diagnostic codes (2000–2010)
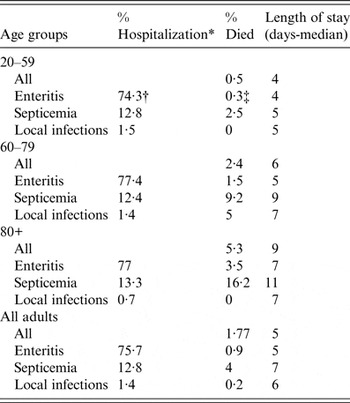
* Total not equal to 100 because unspecified and other infections not included.
† Enteritis represents 74·3% of NT Salmonella-related hospitalization among the 20–59 age group.
‡ The 0·3% of patients with identified enteritis has the most responsible diagnostic in this age group who died at the hospital.
Length of stay and outcome
The median length of stay for NT Salmonella-related hospitalization in seniors was 7 days compared with 4 days for other adults. The length of stay also increased (P < 0·05) with age with a median length of stay of 6 days for people aged 60–79 years and 9 days for people aged 80 years and over. Moreover, median days in hospital varied depending on type of infections contracted, with longer stays associated with sepsis (Table 3).
When looking at hospitalizations when NT Salmonella was identified as one of the diagnostic codes, deaths within hospital increased with age (P < 0·05) for seniors. Deaths occurred in 4·3% of patients aged 60–79 years and in 7·4% of patients aged 80 years and over, for a mean percentage of deaths of 5·2% in seniors, representing 82% of the deaths recorded in the adult population. In other adults, 1·1% of patients with salmonellosis died at the hospital. Similarly, deaths at the hospital increased with age (P < 0·05) when NT Salmonella was recorded as the most responsible diagnosis; death occurred in 2·4% of patients aged 60–79 years and in 5·3% of patients aged 80 years and over. In comparison, 0·5% of other adults died at the hospital when NT Salmonella was identified as the most responsible diagnosis for hospitalization (Table 3).
Chronic diseases
Among seniors (60+) hospitalized with NT Salmonella as the most responsible diagnosis, 60% were also diagnosed with at least one of the four most prevalent chronic diseases in seniors in Canada, namely cardiovascular diseases, diabetes, arthritis and rheumatism, and cancer (Fig. 1). Among those with at least one chronic disease, 36% were affected by two or more. Table 1 shows ICD diagnostic codes associated with chronic diseases. Among patients with only one chronic disease recorded, 45% of them recorded cardiovascular diseases. No statistically significant differences among these proportions were observed when looking at the two age groups among seniors (60–79 and 80+). When two or more chronic diseases were recorded, the most frequent combination was cardiovascular disease and diabetes, with 19% of patients affected with this combination of diseases.
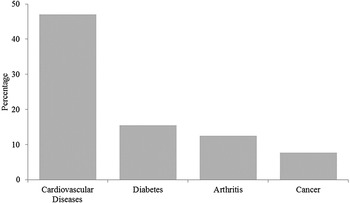
Fig. 1. Percentage of seniors diagnosed with chronic diseases and Salmonella as the most responsible diagnosis for hospitalization.
Estimates of domestic foodborne hospitalizations and deaths
After accounting for under-reporting and under-diagnosis, the annual estimate of total NT Salmonella-related hospitalizations in seniors in Canada is 534 (90% PI 375–733) hospitalizations (Table 4), for an annual incidence of 11·2 hospitalizations per 100 000 people, representing about 35% of Salmonella-related hospitalizations for all age groups [Reference Thomas18]. A breakdown of the 60–79 and 80 and over age groups can be found in Table 4. When also accounting for the proportion of foodborne and travel-related infections (based on this age group), we estimated that each year, 336 (90% PI 251–433) hospitalizations are related to domestically acquired foodborne NT Salmonella in seniors for an annual incidence of 5·7 hospitalizations per 100 000. The annual estimate of total NT Salmonella-related deaths in seniors is 27 (90% PI 18–42) deaths; this includes both underlying and contributing causes of death, representing more than 90% of deaths estimated for all age groups. We also estimated that each year there are 17 (90% PI 10–26) deaths related to domestically acquired foodborne NT Salmonella in seniors for an annual incidence of 0·29 deaths per 100 000.
Table 4. Annual estimate of NT Salmonella-related hospitalizations and deaths (2000–2010)
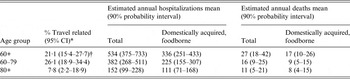
* Unpublished data FoodNet 2005–2013.
† Not used in calculation of domestically acquired, foodborne result for the 60+ age group (results for 60-79 and 80+ age group models were added to account for distribution of hospitalizations between the two age groups).
DISCUSSION
Findings from this study showed that half of the NT Salmonella-related hospitalizations and most of the deaths recorded in the Canadian adult population occurred in seniors, even though they represent only a quarter of the adult population during the 10 years of the study. These proportions are of particular concern because they are expected to increase as the population aged 60 years and over is expected to increase by more than 56% by 2035 [6]. It is also important to mention that the hospitalization rate and the percentage of deaths within the hospital increased with age almost twofold among individuals aged 80 years and over compared with individuals aged between 60 and 79 years. This is noteworthy knowing that the proportion of people aged over 80 in the Canadian senior population is expected to increase over time. According to Statistics Canada, people aged over 80–20% of the Canadian senior population in 2011 – will increase to more than 25% of the seniors by 2035, representing an increase of 1·8 million people for this age group. A similar finding was also identified in the USA, with higher proportions of the 80+ age group hospitalized with NT Salmonella than the 65–79 age group [Reference Scallan23].
This study also revealed that the burden associated with NT Salmonella-related hospitalization is greater as people get older. Seniors tend to stay longer in the hospital with a median length of stay that is 2–3 days longer than other adults. This prolonged stay, especially of older people who tend to be affected by more than one medical condition, may contribute to an increased cost to the health care system. Results also showed that hospitalized seniors with NT Salmonella infection are more at risk of death than other adults hospitalized for the same condition. This was a similar finding identified in the USA for NT Salmonella, with a 2·4% case fatality rate for the 65+ age group compared with 0·3% for 5–64 years [Reference Scallan23]. Of the estimated annual costs attributed to Salmonella infections, fatal cases have been reported to have the highest cost per case in terms of medical care and loss of productivity [Reference Frenzen24].
Chronic dehydration, impaired immune function, existing chronic diseases and medication may make older people more vulnerable to infection and to more severe disease and health outcomes [Reference Gavazzi and Kraus25, Reference Warren26].
A non-negligible proportion of seniors hospitalized with a NT Salmonella diagnosis as the most responsible diagnosis also had one or more underlying chronic diseases. Therefore, people affected by chronic disease may be more likely to seek medical care and be hospitalized when they have enteric symptoms. An American study also found a positive association between a higher number of chronic conditions in hospitalized salmonellosis patients and both disease severity and length of stay at the hospital [Reference Cummings13]. Other studies have shown that chronic diseases influence the immune system in various ways that may lead to more severe illness for people suffering from bacterial infections, including salmonellosis [Reference Lund and O'Brien27, Reference Kirkwood, Ebrahim and Kalache28]. These results on chronic diseases in patients hospitalized with NT Salmonella remind us that elderly people afflicted with chronic diseases are functionally impaired and rely regularly on medication, which can make them even more susceptible to developing severe enteric diseases such as salmonellosis. This should be considered when prevention programs are developed and targeted to this sub-population.
Previous analyses of hospitalization data in Canada for all age groups revealed that Salmonella infections accounted for more hospitalizations than infections with any other bacterial foodborne pathogens during 2000–2010 [Reference Thomas18]. Moreover, NT Salmonella was the second bacteria of importance when looking at the numbers of deaths. Of the total annual estimate of total domestically acquired Salmonella-related hospitalizations and deaths for all age groups in Canada, seniors represent about 35% of hospitalizations and more than 90% of deaths, highlighting the significant impact of the senior population on the burden of salmonellosis in Canada. These proportions are of particular concern as they are likely to be even greater in the future with the expected demographical shift towards a larger proportion of seniors and older seniors in the Canadian population in the coming decades [19]. Using a similar model, the USA estimated 5100 hospitalizations and 220 deaths each year related to NT Salmonella among adults aged 65+ [Reference Scallan23]. This reflects a higher rate (13·7) per 100 000 people than in Canada, which may reflect illness rates as well as their use of surveillance program data compared with the use of hospital administrative data to inform estimates. The use of linked surveillance data may capture more data on hospitalization outcomes for all laboratory-confirmed Salmonella cases, while administrative data may capture hospitalizations related to Salmonella that are first diagnosed at the hospital only.
Some limitations should be taken into account when looking at the results of this study. Hospitalization data are limited or not available through national surveillance programs. National level data for Canada is available through the databases of CIHI, however, NT Salmonella hospitalizations could have been under- or over-identified in those databases. According to a data quality analysis conducted by CIHI in 2009–2010 comparing the database and patient charts, 70% of admissions associated with intestinal infectious and parasitic diseases that were recorded in patient charts were identified in the database and 9% of hospitalizations associated with those diseases identified in the database were not identified in the medical charts of the patients [Reference Thomas18, 29]. Because of under-reporting and under-diagnosis, numbers of hospitalizations are certainly underestimated. This is why calculated estimates presented in this study are important to integrate to better understand the true burden of hospitalization associated with salmonellosis in seniors. Limitations of the model to estimate domestically acquired hospitalizations and deaths are described in detail elsewhere [Reference Thomas18], however, one additional limitation to note is the use of FoodNet Canada data for the age-specific proportion of travel-related illness that may not be fully representative of the Canadian population [22]. Understanding cause of death is complex, especially when taking into account comorbidities; these results describe deaths of people who died after being infected with Salmonella and the resulting illness may be either the cause or the contributing cause of death.
This study describes specific characteristics of NT Salmonella-related hospitalization in seniors and therefore increases our understanding of the severity and health care use by age group. For the first time, age group-specific estimates of NT Salmonella-related hospitalizations and deaths in Canada were calculated, highlighting the importance of the senior population in the over-all burden estimates. This should be considered when developing direct and indirect medical costs to estimate total economic cost of the illness in Canada. NT Salmonella continues to be a common pathogen causing illness and older people are considered a vulnerable population to these infections and especially to severe outcomes. Because of their vulnerable status, identification of unique risk factors and targeted prevention with seniors should be pursued to reduce the number of salmonellosis cases and to reduce hospitalizations and deaths associated with this disease.
ACKNOWLEDGEMENTS
This study used data and information provided by the Canadian Institute for Health Information. However, the analyses, conclusions, opinions and statements expressed herein are those of the authors and not necessarily those of the Canadian Institute for Health Information. The authors thank the Data Coordination and Access Program of the Public Health Agency of Canada for their support with the database.
DECLARATION OF INTEREST
None.








